
Video-Vetted Vs. Non-Video-Vetted Vs. Subjectivity
To the endometriosis community,
Over the past several months, we have had some questions regarding iCarebetter and the legitimacy of our expert lists. We have seen several posts, comments, and threads sharing various information and questions about iCarebetter and the vetting platform. We thought it might be helpful to clear the air and provide answers in case anyone has been confused. Specifically, we are here to answer these questions:
- Are all of the surgeons on iCareBetter video vetted?
- Do doctors have to pay iCarebetter to be added to the expert list on the website?
- Is the vetting process for iCarebetter regulated?
We fully understand and appreciate the concerns about the quality of an excision surgeon and the complexity of assessing a surgeon’s skill for a patient.
Before diving into the Video-Vetting and iCareBetter list, let’s review other options. There have been several recommendations, which include:
- Review the surgeon’s social media profile and their surgical videos
- Use Google to search for nearby doctors and their reviews
- Ask surgeons how many complex surgeries they have done
- Look at their publications
- Lists
While many of those with endometriosis have had to do this for many years, It is obvious that these solutions are not practical or helpful for many patients, and they lack objectivity.
For example, reading in detail about someone’s experience can be helpful. However, reading a list of Google reviews will often be one-sided or only demonstrate extreme views—those with extremely positive or negative experiences.
Having scientific publications doesn’t mean a surgeon is good. Most people have been informed that funding sources, conflicts of interest, and the quality of research are important to understand. Without having a background in healthcare or research, this can be hard for patients to understand how to do or what to look for. There are also publications that say the right things, but their intentions are not in the right place and there may be secondary gain. Many surgeons in the endo space may demonstrate a good understanding of endo, but this does not always extend in their surgical skills.
Knowing the power dynamic between patients and surgeons, it is almost impossible to get a clear answer about how many endo surgeries a surgeon has performed. Logically, it makes sense that if a doctor is only performing a few surgeries per month compared to someone doing a few surgeries per week, the physician performing more has more practice. That being said, there are other considerations that are beyond the control of the physician.
We can go on, but you get the idea. The bottom line is that everyone has their own subjective perspective, which is based on past experiences, their own research, and oftentimes others’ influence and experiences. And we all know each individual is different and what worked for me might not work for you.
In contrast to all these methodologies, iCareBetter has only applied objective processes. We have only examined evidence to see what works.
A study in the New England Journal of Medicine used actual data to show that video-based surgical skill scores were correlated with Complications. https://www.nejm.org/doi/full/10.1056/NEJMsa1300625
iCareBetter then applied this Journal Article methodology to endometriosis surgery. We created the list of Video-Vetted surgeons after vetting their surgeries. iCareBetter started by only listing surgeons who passed video vetting. This process requires surgeons to submit three videos with specific criteria, which are then peer-reviewed by other experts in this field. The entire process is double-blinded.
As iCareBetter is relatively new to the endo space, it took some time to build up our resources. Unfortunately, the number of surgeons submitting videos and the number of surgeons who passed was very low. Additionally, reviewing a surgeon’s videos is very long and usually takes three months on average. At the same time, 90% of patients who used iCareBetter could not find a surgeon based on their criteria and location. In order to serve the needs of those utilizing iCareBetter to find care, we had to make a change so patients could still find a doctor who could still provide some surgical care. Therefore, we made the decision to add a second group of surgeons who are non-video-vetted. These surgeons are added based on their peers’ recommendations and their personal interests. Patients can review them on their iCareBetter profile, and we publish the reviews without filters.
We hope that these non-video-vetted surgeons will take the steps to pass the video-vetting in the future. Meanwhile, the Video-Vetted designation is explicitly stated on the profile of the Video-Vetted surgeon, there is no fine print.
In regards to the questions about surgeons paying to be on iCareBetter, we did begin this process by charging doctors a subscription fee to be on iCareBetter. But since over a year ago, we have given the option for a 100% discount, and surgeons can choose to be on iCareBetter for zero subscription fee. To keep the lights on, we only charge doctors if we help them with promotion or management services such as training their staff to offer better care to patients and giving them marketing strategies, all of which are optional. That said, for video vetting, the only required fee for surgeons is a one-time review fee of $400 that pays for reviewers and the cost of the review.
Currently, we have 222 providers, including surgeons on iCareBetter, and we are seeing constant interest and growth. We will continue to do video-vetting and hope that more surgeons will become Video-Vetted. We continue Video-Vetting for patients’ interest and for the purpose of transparency.
We would love to hear your thoughts and concerns here.

Can Minimal Endometriosis Cause Infertility
Endometriosis, a common gynecological condition, has been frequently associated with infertility. However, the question remains: can minimal endometriosis cause infertility? This comprehensive article aims to delve into the connection between endometriosis, particularly in its minimal stage, and fertility issues.
Defining Endometriosis
Endometriosis is a medical condition characterized by the growth of endometrium-like tissues outside the uterus. These tissues can adhere to various pelvic structures like the ovaries, fallopian tubes, and even the intestines and bladder, causing irritation, inflammation, and scar tissue formation.
Stages of Endometriosis
Endometriosis is categorized into four stages:
- Stage I (Minimal): Small endometriotic implants with no scar tissue.
- Stage II (Mild): More extensive implants, involving less than 2 inches of the abdomen, without scar tissue.
- Stage III (Moderate): Severe endometriosis with deep implants and possible formation of endometriotic cysts or ‘chocolate cysts’ in the ovaries.
- Stage IV (Severe): Numerous endometriotic implants, possibly large endometriotic cysts in the ovaries, and scar tissue formation around the reproductive organs.
Read More: Understanding How Endometriosis Can Cause
The Connection Between Endometriosis and Infertility
It’s estimated that 30% to 50% of women with endometriosis may experience infertility. Even in cases of minimal or mild endometriosis, the disease may still impact fertility in numerous ways, including:
- Distorted pelvic anatomy due to scar tissue and adhesions
- Inflammatory response causing a hostile environment for eggs, sperm, and embryos
- Altered immune system functionality
- Changes in the hormonal environment affecting egg quality and embryo implantation
However, it’s essential to note that endometriosis does not necessarily equate to infertility. Many women with endometriosis, even in severe stages, can conceive naturally or with fertility treatments.
Exploring the Question: Can Minimal Endometriosis Cause Infertility?
The impact of minimal endometriosis on fertility is a contentious subject. The disease, even at its earliest stage, can cause inflammation and subtle changes in the pelvic environment, potentially affecting fertility. However, many women with minimal endometriosis conceive without issues, leading some researchers to suspect that other factors, possibly genetic or immunological, might be at play in cases of endometriosis-associated infertility.
Diagnosing Endometriosis
Diagnosing endometriosis can be challenging, as many women with infertility migh experience no symptoms. The gold standard for diagnosis is a surgical procedure known as laparoscopy, allowing the doctor to visually inspect the pelvic organs for endometriotic lesions and scar tissue, and take samples for histopathology.
Read More: Life After Endometriosis Surgery: A Comprehensive Guide
Evaluating Fertility
Before initiating any fertility treatment, a comprehensive fertility evaluation is recommended. This includes hormonal and blood tests, an assessment of ovarian reserve, a sperm analysis for the male partner, and possibly a laparoscopy to confirm the presence and extent of endometriosis.
Read More: Pelvic Floor Physical Therapy: What you Need to Know
Treatment Options for Endometriosis-Related Infertility
The treatment approach for endometriosis-related infertility is multifaceted, depending on the stage of endometriosis, the woman’s age, and the presence of other fertility factors.
Surgical Treatment
For women with Stage I or II endometriosis, surgical removal of endometriotic tissue may improve pregnancy rates. However, for women aged 35 or older, other fertility treatments might be recommended in addition to surgery.
Medical Treatment
Medical treatments aim to suppress endometriosis growth by reducing estrogen levels. However, these treatments, including hormonal contraceptives and Gonadotropin-Releasing Hormone (GnRH) agonists, prevent pregnancy during use.
Assisted Reproductive Technology (ART)
In cases where pregnancy does not occur naturally or following surgery, ART methods such as Intrauterine Insemination (IUI) or In Vitro Fertilization (IVF) may be recommended. The success rates of these treatments vary depending on the woman’s age, ovarian reserve, and specific fertility issues.
Conclusion: Can Minimal Endometriosis Cause Infertility?
While minimal endometriosis can potentially affect fertility, it does not guarantee infertility. A comprehensive evaluation and personalized treatment plan can help women with endometriosis, even at minimal stages, to conceive successfully. However, further research is needed to fully understand the complex relationship between endometriosis and fertility.
References:
https://www.uptodate.com/contents/endometriosis-treatment-of-infertility-in-females

Can Endometriosis Spread to Your Diaphragm: An In-Depth Analysis
Endometriosis is a chronic health condition that manifests when tissues akin to the endometrial lining start to grow outside the uterus. This exogenous growth of endometrial-like tissue can be found in various areas such as the ovaries, fallopian tubes, and bladder. However, endometriosis can also occur in less common areas like the diaphragm, organs in the upper abdomen, like the stomach, in the retroperitoneum like the lymph nodes and kidneys, and so on. Of these uncommon findings, finding some amount of endo on the diaphragm is perhaps most common.
Understanding the Diaphragm
The diaphragm is a large, dome-shaped muscle located beneath the lungs, responsible for the crucial function of respiration. Acting as a separation between the abdominal and thoracic (chest) cavities, its involuntary contraction and relaxation facilitate the breathing process. The diaphragm also has openings that allow important structures such as the esophagus and major blood vessels to pass through.
Endometriosis in the Diaphragm
In most cases, diaphragmatic endometriosis affects the right side of the diaphragm. The endometrium-like tissue that builds up on the peritoneal surface of the diaphragm reacts to the menstrual cycle’s hormones in the same way it does in the uterus, which can cause a range of symptoms in the affected individuals.
Read More: Understanding How Endometriosis Can Cause
Symptoms of Diaphragmatic Endometriosis
The most common symptoms of diaphragmatic endometriosis include pain in the chest, upper abdomen, right shoulder, and arm. This pain typically occurs around the time of your period and may get worse when you take deep breaths or cough. In rare cases, if it grows through the diaphragm and involves the lungs, it can lead to a collapsed lung. This is known as catamenial pneumothorax. However, diaphragmatic endometriosis can often be asymptomatic while only small superficial implants are present. Hence, surgery usually involves at least looking at the diaphragms to document if there are any endo implants even if there are no symptoms in that area.
Causes of Diaphragmatic Endometriosis
The exact causes of diaphragmatic or other types of endometriosis remain unknown. However, it is plausible that endo cells from the pelvis can travel throughout the abdomen and up into the diaphragm. What makes them implant and grow there is unknown. Alternatively, there are other possible etiologies, such as lymphatic or blood stream spread to this area or direct transformation of stem cells or growth of embryologic remnants into endometriosis implants. This is all likely facilitated or repressed by genetic and genomic molecular signalling that is only now coming to be appreciated and unraveled.
Read More: What Does Bowel Endometriosis Feel Like? Understanding the Pain and Symptoms
Diagnosis of Diaphragmatic Endometriosis
Diagnosing diaphragmatic endometriosis can be challenging. Diagnosis often involves a combination of medical history, physical examination, and imaging tests such as a CT (computed tomography) scan or MRI (magnetic resonance imaging).
The most reliable way to diagnose diaphragmatic endometriosis is via minimally invasive laparoscopic or robotic surgery. Ideally, the surgeon who is excising endo in the pelvis can also remove diaphragmatic implants or have a surgeon available as part of the team, who can do so. In the much rarer event that endo is suspected to be inside the chest and/or growing on or in the lungs, a thoracic surgeon should be consulted.
Treatment of Diaphragmatic Endometriosis
Surgery is the main treatment for diaphragmatic endometriosis and this can usually be accomplished using minimally invasive laparoscopic or robotic surgery. Again, the excision surgeon or surgical team should be capable of removing endo from the diaphragms.
In some cases, endo is not suspected to be growing on the diaphragm. In that case, if the surgery cannot be safely accomplished by the surgeon or surgeons on the team, it is best to back out and not cause more harm than good. The diaphragm is very thin and it is rather easy to enter the chest as part of the excision. In expert hands, that is not a problem. However, going one step beyond diaphragmatic endo, if it is unclear whether or not the endo may be crossing into the chest cavity it is best to back out, re-evaluate with proper imaging and consultation and perform the surgery with a thoracic surgeon at a later date.
Complications of Diaphragmatic Endometriosis
In relatively rare cases, endometriosis of the diaphragm can lead to defects or holes forming in the diaphragm. Endo can then grow into the chest cavity and possibly involve the lungs. This can lead to life-threatening complications such as a collapsed lung during your period (catamenial pneumothorax) or significant bleeding into the chest, also compressing the lung.
Read More: Can Endometriosis on Ureter Cause Kidney Shooting Back Pain?
Conclusion
In conclusion, while it is relatively uncommon, endometriosis can indeed spread to your diaphragm. Under more rare circumstances it can even grow into the chest and lungs. Expert endometriosis consultation and care is always prudent. But if you are experiencing upper abdominal or chest symptoms as discussed this this article, it become crucial.
References
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6018178/

Can Endometriosis on Ureter Cause Kidney Shooting Back Pain?
Endometriosis is a common gynecological condition that affects many women during their reproductive years. While it typically manifests in the pelvic region, in some instances, it may invade other organs, including the urinary system. This article explores the question: Can endometriosis on the ureter cause kidney shooting back pain?
About Endometriosis
Endometriosis is a chronic disease characterized by the presence of endometrial-like tissue outside the womb. This could include the ovaries, fallopian tubes, and the lining of the pelvic cavity. In some extreme cases, endometrial tissue may also affect organs outside the pelvic cavity, such as the bladder, bowel, or kidneys.
Read More: Understanding Endometriosis: Unveiling the Common Symptoms and Their Impact
Understanding Ureteral Endometriosis
Ureteral endometriosis is an uncommon manifestation of the disease, accounting for about 1% of all endometriosis cases. It involves the ureters, the tubes that transport urine from the kidneys to the bladder. This condition can lead to urinary tract obstruction, resulting in hydronephrosis, which is the swelling of a kidney due to a build-up of urine.
The Kidney-Endometriosis Connection
The kidneys can be impacted when one or both of the ureters become affected by endometriosis. The section of the ureter that is usually affected sits below the pelvic area.
Symptoms of Kidney Endometriosis
Kidney endometriosis can be asymptomatic for several years. If a person who has undergone surgery to treat endometriosis has ongoing urinary problems such as pain and infections, it may suggest the presence of urinary tract or kidney endometriosis. Symptoms may include:
- Pain in the lower back that gets worse with a monthly menstrual cycle. That pain can also extend down through the legs.
- Blood in the urine that can co-occur with the menstrual cycle
- Difficulty urinating
- Recurrent urinary tract infections
Read More: Understanding How Endometriosis Can Cause
Diagnosis of Kidney Endometriosis
The diagnosis of ureteral endometriosis relies heavily on clinical suspicion. As a result, they often misdiagnose patients with kidney cancer. This can lead to patients not receiving treatment on time, or receiving the wrong kind of treatment.
Read More: Life After Endometriosis Surgery: A Comprehensive Guide
Treatment Options
Kidney endometriosis can lead to kidney damage and even kidney failure if left untreated. However, the best approach is to treat the condition by removing endometriosis lesions with minimally invasive laparoscopic surgery.
The Silent Threat of Kidney Failure
One of the most concerning aspects of ureteral endometriosis is the silent threat of kidney failure. It is estimated that as many as 25% to 50% of nephrons are lost when there is evidence of ureteral endometriosis, and 30% of patients will have reduced kidney function at the time of diagnosis.
Impact on Kidney Health
The good news is that if one kidney isn’t functioning due to endometriosis, you can survive on the other kidney. So, if you find out you only have one fully-functioning kidney, it’s essential to take care of it.
Conclusion
In conclusion, while endometriosis is typically a pelvic condition, it can venture beyond and affect the urinary system, including the kidneys. This can lead to severe complications, including kidney failure. Therefore, it’s crucial for women with endometriosis to be aware of the potential symptoms and seek medical advice if they experience any signs of kidney problems. The early detection and treatment of ureteral endometriosis are crucial to preserving kidney function and overall health.
References:
https://drseckin.com/kidney-endometriosis/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3535807/
Endometriosis: Perilous impact on kidneys
https://endometriosis.net/clinical/silent-kidney-failure

iCareBetter Launches Endometriosis Center For Long-Term Care
iCareBetter Launches Endometriosis Center For Long-Term Care
“
Based on patients’ needs and considering the lack of appropriate endometriosis care, iCareBetter launches Endometriosis Centers for long-term care. The centers’ focus will be long-term endometriosis care before and after excision surgery. We will collaborate closely with excision surgeons, physical therapists, and other providers on iCareBetter to offer long-term multidisciplinary care to endometriosis patients. We believe that excision surgery is the gold standard of treatment for endometriosis, and we also believe that patients need an ongoing care plan and monitoring after excision surgery, even if the best surgeons in the world do it.
”
This is Dr. Saeid Gholami, the founder of iCareBetter. I have an important announcement to make today. But first, let me take you on a journey with me through the last three and a half years.
Phase I – it starts with surgery.
In my exposure to endometriosis patients as a medical student and then as a primary care doctor, I have always tried to find a solution to identify trusted resources for patients. A few years ago, right at the beginning of the pandemic, while the world was going upside down, I started working with a team of the best endometriosis surgeons and advocates to create a vetting system to find and introduce skilled excision surgeons. The vetting was based on a New England Journal of Medicine article and assessed surgical videos in a double-blind process.
This vetting made some people uncomfortable. However, the vetting confirmed the skills of the best surgeons in the world and introduced some new excision surgeons with a limited chance to prove themselves in a space where everyone claimed expertise without proof. This led to a transparent process that let patients make informed decisions about their excision surgeons. This innovation put us on the map and made us a significant platform in the endometriosis world.
Phase II – add multiple disciplines
After successfully launching video vetting for surgeons, we sought other opportunities to support endo patients. Our conversations with patients taught us that the community needs vetted physical therapists (PT) who understand endometriosis and its complex care requirements. Therefore, we introduced the iCareBetter Physical Therapy vetting and built a network of PTs. Our list of PTs kept growing, and after two years, many advocates and patients are using it daily and promoting the importance of physical therapy for endometriosis patients. The PT directory has been very helpful for patients, and we have over 120 physical therapists in almost all the US states. And thousands of patients have used iCareBetter to find a PT to help with their endometriosis.
Similarly, we added urologists, dietitians, and pain specialists so patients can use iCareBetter for most of their endo-related issues.
Phase III – Artificial Intelligence for endometriosis
Right after the launch of Chat-GPT and the excitement around artificial intelligence (AI), we launched an AI-powered chat tool called endometriosis.AI. This created massive excitement, and many patients started using it. As a result, we ran out of server capacity within three days after launch and had to shut it down to avoid going into debt for server costs. As I am speaking with you, thousands of patients have used it and keep using it to acquire information about endometriosis. With the launch of endometriosis.ai, we made endometriosis the first disease community to have its specialized AI discussion. This was in sharp contrast with the history of endometriosis, which is always among the last diseases to be considered in other situations, such as surgical tools, medications, and others.
Moreover, we have published hundreds of articles and interviews to create an education hub for endometriosis.
We currently have over 200 providers in our network, and 30,000 patients use our services each month.
I am incredibly proud of what we have achieved.

Phase VI – Begins iCareBetter Centers for Long-Term Care.
One question that patients commonly asked us was, “Where can I go before surgery or after surgery for long-term care?”
We searched the medical community for the right centers to help with this long-term care. Our non-negotiable criteria were simple: These centers should not dismiss patients and avoid putting endo patients on hormones as “the cure for endo.”
To my frustration and shock, no center expressed interest in seeing more endometriosis patients. We even purchased the emails of ten thousand OBGYNs in the US and invited them to join our network and support endo patients. Not even one ObGyn responded positively to the invite to see more endometriosis patients. Except for our excision surgeons, no one wanted to deal with endometriosis patients in their practice. It was a heartbreaking realization for all of us.
From a patient’s perspective, they need a care team that is in their corner and does not get tired of them after four or five visits because the pain is still there. A team that sits and thinks with the patient and tries to problem-solve with the patients as a team member. This team should map out the options, what has been tried, and what is left to be tested. A team that patients can go to four weeks, four months, or four years after surgery to complain that the pain is back.” This team, instead, thoroughly evaluates patients for other pain generators or a recurrence of endometriosis. A care team that believes in patients and helps them connect with the right specialist for their gastrointestinal, urinary, neurological, and other symptoms.
We tried several solutions to create this care team with other centers and groups, but there was a complete lack of interest and empathy, as it has always been with endometriosis. Therefore, we decided to build these centers ourselves. With that, I am proud to announce that we are launching the first iCareBetter Endometriosis Center in sunny California. It will be at 6621 Bay Laurel Place, Suite A, Avila Beach, CA 93424. We plan to open the next centers in CA and other states.
The centers’ focus will be long-term endometriosis care, so we will collaborate closely with excision surgeons, physical therapists, and other providers on iCareBetter to offer long-term multidisciplinary care to endometriosis patients. We believe that excision surgery is the gold standard of treatment for endometriosis, and we also believe that patients need an ongoing care plan and monitoring after excision surgery, even if the best surgeons in the world do it. iCareBetter centers will be the long-term care center for patients before and after excision surgery.
Our first center in Central California will be ready to see patients on February 20th, and we will offer in-person and virtual services. The next ones are being prepared, and we will announce their launch soon. If you want to ensure you secure your place before we run out of space, join the waitlist by filling out the form below. Also, if you want to be among the first ones to know about iCareBetter centers when we come to your area, please use the link below to add your name to the waitlist.

What Does Bowel Endometriosis Feel Like? Understanding the Pain and Symptoms
Endometriosis is a condition affecting roughly 11% of women worldwide, predominantly those of reproductive age. An even more specific form of this ailment is bowel endometriosis, which impacts around 5% to 12% of those diagnosed with endometriosis. In this comprehensive guide, we delve into the intricacies of bowel endometriosis, exploring what it feels like, the symptoms, causes, diagnosis, and treatment options.
What is Bowel Endometriosis?
Bowel endometriosis occurs when endometrial-like tissue, which typically grows inside the uterus, begins to develop on or inside the bowel walls. This can lead to a range of gastrointestinal symptoms, often causing significant discomfort and negatively impacting the quality of life.
Read More: Understanding Bowel Endometriosis
Where Does Bowel Endometriosis Occur?
The condition predominantly affects the rectum and sigmoid colon, with approximately 90% of bowel endometriosis cases directly involving these regions. However, the appendix, small intestine, stomach, and other parts of the large intestine can also be affected. In many cases, bowel symptoms occur because of the mere presence of intensely inflammatory endo lesions on the peritoneum in the pelvis and abdomen and not even involving the bowel directly with implants.
Symptoms of Bowel Endometriosis
The symptoms of bowel endometriosis often mimic common gastrointestinal disorders, including small intestinal bacterial overgrowth (SIBO), making it difficult to diagnose. They can range from mild to severe, and often fluctuate depending on the menstrual cycle.
Common Symptoms
Common symptoms may include:
- Abdominal pain, particularly in the lower quadrants
- Bloating, often referred to as “endo belly”
- Changes in bowel movements, including constipation or diarrhea
- Nausea and vomiting
- Pain during bowel movements, which might increase during menstruation
- Rectal bleeding
Non-Bowel Symptoms
In addition to bowel symptoms, individuals with endometriosis might experience:
- Chronic pelvic pain
- Difficulties with fertility
- Painful sexual intercourse
- Pain during urination
- Pelvic heaviness
- Fatigue
- Impaired psychological well-being
Causes of Bowel Endometriosis
The exact cause of bowel endometriosis remains unknown. However, Mullerianosis of embryogenic origin and retrograde menstruation are two often-quoted theories. Mullerianosis of embryogenic origin suggests that developmental abnormalities lead to cells being present in atypical locations which later turn into endometriosis. This includes potential genetic, genomic and immunologic influencing factors. Retrograde menstruation proposes that period blood flows upward towards the Fallopian tubes and into the pelvis instead of out through the vagina, potentially leading to endometriosis. Given that most women experience retrograde menstruation, and only 10% or so experience endometriosis, this theory is antiquated and has been challenged because of this disconnect. Far more likely, some combination of embryologic, molecular, immunologic and genetic factors are in play and this can vary between individuals.
Read More: Can Endometriosis Cause Bowel Issues?
Diagnosis of Bowel Endometriosis
Diagnosing bowel endometriosis is a complex process. It often requires a combination of a good evaluation of symptoms history, physical examination, imaging techniques like ultrasound or MRI, and sometimes minimally invasive laparoscopic or robotic surgery. However, diagnosis could be delayed due to its symptom similarity with other gastrointestinal diseases. Imaging can only help with diagnosis and potential mapping for surgery. It is absolutely not reliable enough to exclude the diagnosis of endo.
Misdiagnosis
Misdiagnosis is common in bowel endometriosis, with many patients being misdiagnosed with irritable bowel syndrome (IBS) or other gastrointestinal disorders. Therefore, a high index of suspicion is necessary for diagnosis, and any bowel symptoms correlated with the menstrual cycle should be critically evaluated.
The Role of Minimally Invasive Surgery
Surgery with biopsy is considered the “gold standard” in diagnosing endometriosis, including bowel endometriosis. It provides a more accurate diagnosis and gives healthcare providers an exact idea of how much scar tissue and endometrial-like tissue they’re dealing with. Ideally, the surgeon should be prepared to perform a therapeutic surgery at the same time as a diagnosis. However, a bad surgery is worse than no surgery if the surgeon is unprepared and performs some variation of fulguration (burning) of endometriosis lesions as opposed to proper excision of the lesions or implants. If diagnostic surgery uncovers a situation where the surgeon is unprepared to properly perform therapeutic excision it is better to back out and refer to an appropriate surgeon.
Treatment of Bowel Endometriosis
Treatment for bowel endometriosis often involves surgery, as medical management has generally been deemed ineffective for these specific lesions. The chosen surgical method depends on the extent of the condition. In many cases, hormonal options may also be recommended after surgery to reduce recurrence risk. The better the surgery the less likely this would be required but there are exceptions.
Surgical Treatment
The surgical treatment of endo usually involves removing all of the peritoneal lesions by an excisional technique. In deeply infiltrating endometriosis, the approach may vary based on the involvement of the rectal wall or the mesentery, which is where the blood vessels to the rectum are located. The treatments for bowel endometriosis include shaving, nodulectomy, disc resection, and bowel resection. The surgeon should be capable of performing any of these procedures as needed at the time. In some cases this may be the main excision surgeon, if they have bowel surgery training and hospital prvileges, and in other cases, this may be another surgeon who is part of the backup team. In the latter situation, it is best if the possibility of bowel surgery and options are addressed before surgery and not as an emergency during surgery, when appropriate surgeons may not be readily available.
Lifestyle Changes
Alongside medical treatment, lifestyle changes can aid in managing bowel endometriosis symptoms. Some patients find that certain foods or lifestyle habits, such as stress or irregular sleep, may trigger their symptoms. Keeping a journal to track triggers and consulting with a healthcare provider or nutritionist when making dietary changes can be beneficial.
Read More: How to Treat Bowel Endometriosis: A Comprehensive Guide
Coping with Bowel Endometriosis
Living with bowel endometriosis can be challenging, but with the right diagnosis, treatment, and management, individuals can lead fulfilling lives. It’s essential to communicate openly with healthcare providers about symptoms and concerns, as this can aid in diagnosis and treatment planning.
In conclusion, bowel endometriosis is a painful and often misunderstood condition. Increased awareness and understanding of the disease can help in early diagnosis, effective treatment, and improved quality of life for those affected. If you suspect you might have bowel endometriosis or are experiencing any of the symptoms mentioned, do not hesitate to seek medical advice.
References:
Surgical Outcomes after Colorectal Surgery for Endometriosis: A Systematic Review and Meta-analysis

Can Endometriosis Cause Bowel Issues?
Endometriosis is a common but often under-recognized condition, primarily affecting women between 15-50. It results from the growth of tissue similar to the endometrium (the lining of the uterus) outside the uterus. This article explores the question: Can endometriosis cause bowel issues?
Understanding Endometriosis
Endometriosis is a condition where tissue, similar to the kind that lines the uterus (the endometrium), grows outside the uterus. This condition usually affects the ovaries, fallopian tubes, and the tissue lining the pelvis. However, in some cases, it can also affect other organs, including the bowel.
Endometriosis and Bowel Involvement
When endometriosis affects the bowels, it typically occurs in two forms:
- Superficial: The endometriosis tissue is located on the surface of the bowel.
- Deep: The endometriosis tissue passes through the bowel wall.
In both cases, doctors usually find a small mass of tissue, known as a lesion, on the bowel wall. More rarely, these lesions can penetrate into the muscular layer of the bowel.
Read More: Endometriosis and Inflammatory Bowel Disease: Distinguishing the Differences
Causes of Endometriosis
While the definitive cause of endometriosis remains unknown, several contributing factors have been identified. These include hormonal imbalances, immune system problems, and genetic factors.
Symptoms of Bowel Endometriosis
The symptoms of bowel endometriosis can vary, depending on the location and size of the lesion, and how deep it is within the bowel wall. These symptoms often mimic those of irritable bowel syndrome (IBS), but there are key differences.
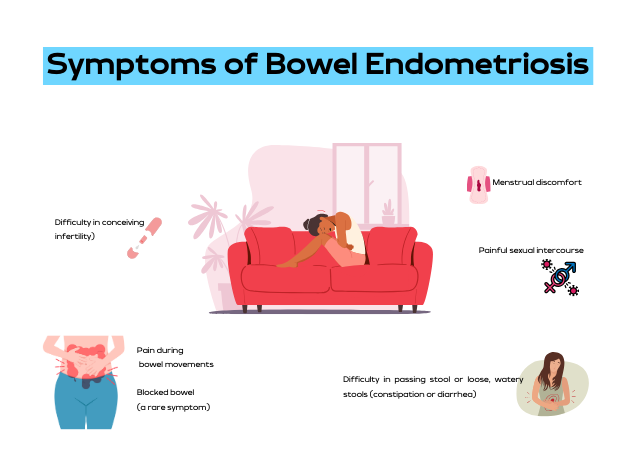
Some of the common symptoms include:
- Trouble pooping or loose, watery stools (constipation or diarrhea)
- Pain during bowel movements
- Menstrual discomfort
- Painful sex
- Difficulty getting pregnant (infertility)
- Blocked bowel (this is a rare symptom)
Diagnosing Bowel Endometriosis
Diagnosing bowel endometriosis can be challenging due to its similarities with other conditions. However, if you have other endometriosis symptoms, such as painful periods, painful sex, lower back pain, or abdominal bloating and discomfort, it’s critical to talk to your doctor.
Read More: Understanding Bowel Endometriosis
Misdiagnosis of Bowel Endometriosis
Unfortunately, bowel endometriosis is often misdiagnosed as irritable bowel syndrome or other gastrointestinal diseases. This is because the symptoms of bowel endometriosis can mirror those of IBS, Crohn’s disease, and appendicitis.
Read More: Finding an Excision Specialist: What you Need to Know
Treatment for Bowel Endometriosis
Treatment for bowel endometriosis is usually tailored to the patient’s symptoms and medical history. The most common treatments include surgery, hormone treatments, and counseling.
Coping with Bowel Endometriosis
Bowel endometriosis is a challenging condition to live with. It not only affects your physical health but also your mental well-being. Many patients have found some symptom relief through lifestyle changes, including dietary adjustments and regular exercise.
The Importance of Early Detection
Given the potential complications of bowel endometriosis, early detection and treatment are crucial. If you experience bowel issues alongside painful menstruation, it’s essential to consult with a healthcare professional.
Conclusion
The question, “Can endometriosis cause bowel issues?” is undoubtedly answered with a resounding yes. However, with timely detection, appropriate treatment, and necessary lifestyle changes, it’s possible to manage the symptoms and lead a healthy life.
Additional Information
This article is a comprehensive exploration of how endometriosis can impact bowel health. It’s essential to remember that while this condition can cause significant discomfort and health issues, effective treatments are available. If you suspect you have endometriosis, don’t hesitate to reach out to a healthcare provider.
References:
https://www.webmd.com/women/endometriosis/bowel-endometriosis
https://www.endofound.org/gastrointestinal-distress
https://maidenlanemedical.com/endometriosis/endometriosis-and-constipation/
https://drseckin.com/bowel-endometriosis/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4604671/
Understanding How Endometriosis Can Cause
Bowel Problems
Endometriosis, a common health concern among women, can manifest itself in various ways, one of them being bowel problems. But how exactly can endometriosis cause bowel problems? This article will take you through the intricate connection between endometriosis and bowel problems, the symptoms to look out for, diagnostic procedures, and potential treatments.
What is Endometriosis?
Endometriosis is a health condition where the tissue similar to the type that lines the uterus, known as the endometrium, grows outside the uterus. This condition predominantly affects the reproductive organs such as the ovaries, fallopian tubes, and the external part of the uterus. However, it can also extend to other parts of the body including the bowels, rectum, and other pelvic organs.
Understanding Bowel Endometriosis
Bowel endometriosis is a form of endometriosis that affects the gastrointestinal tract, specifically the bowels. It can appear in two forms: superficial (on the surface of the bowel) and deep (penetrating the bowel wall).
Read More: Understanding Bowel Endometriosis
Symptoms of Bowel Endometriosis
The symptoms of bowel endometriosis can vary widely depending on the location of the lesion, its size, and how deep it is in the bowel wall. Some women may experience no symptoms. However, common symptoms include:
- Difficulty in passing stool or loose, watery stools (constipation or diarrhea)
- Pain during bowel movements
- Menstrual discomfort
- Painful sexual intercourse
- Difficulty in conceiving (infertility)
- Blocked bowel (a rare symptom)
It is noteworthy that these symptoms can often mimic other conditions like irritable bowel syndrome (IBS), but the two conditions are distinct. One distinguishing factor is that with bowel endometriosis, symptoms often worsen before and during the menstrual period.
Read More: Endometriosis and Painful Intercourse: Is it Really Just Endometriosis?
Causes of Bowel Endometriosis
The exact cause of bowel endometriosis is still under study. However, several factors have been linked to its occurrence. These include genetic predisposition, inflammation, and levels of estrogen, a female sex hormone.
The Prevalence of Endometriosis
Endometriosis affects approximately 10%-12% of women of childbearing age. The condition is often diagnosed in women who are in their 30s, although it can occur at any age.
Diagnosing Bowel Endometriosis
The diagnosis of bowel endometriosis starts with the doctor asking about your symptoms and medical history, followed by a physical examination of your pelvic area. The doctor may also recommend imaging tests to get more information on the location and size of any cysts or tissue damage related to endometriosis. These tests include:
- Transvaginal or transrectal ultrasound: This procedure involves the insertion of a wand-like device into your vagina or rectum. This device releases sound waves that create images of your organs.
- Magnetic resonance imaging (MRI): An MRI test provides detailed images of your organs and tissues using a magnetic field and radio waves.
- Laparoscopy: This surgical procedure involves making a small incision near your belly button and inserting a thin viewing tool called a laparoscope.
- Barium enema: This type of X-ray is used to see changes or defects in your large intestine (colon).
- Colonoscopy: They pass a tube with a camera on its tip through the anus into the colon to directly visualize the wall and take samples from inside the colon.
Read More: Colon Chronicles: Delving into Bowel Endometriosis
Treating Bowel Endometriosis
The treatment plan for bowel endometriosis will be personalized, taking into account your symptoms, medical history, age, and reproductive plans. Treatments can include:
- Surgery: The aim of surgery is to remove as many lesions as possible while preserving your organs and overall health.
- Hormone treatments: These medications control estrogen levels which can worsen the symptoms of bowel endometriosis.
- Counseling: Given the ongoing nature of bowel endometriosis and its impact on both physical and mental health, counseling may be recommended to provide emotional support.
The Prognosis for Bowel Endometriosis
There is currently no cure for endometriosis. However, treatments like surgery and hormone therapy can help manage the symptoms. It is also important to note that symptoms could return if treatment is halted, or they could recur on their own, especially in cases with deep lesions.
Endometriosis is a complex condition that can cause bowel problems and other health issues. If you suspect you have endometriosis and are experiencing bowel problems, it’s important to consult with a healthcare provider. Early diagnosis and treatment can help manage symptoms and improve your quality of life.
References:
https://www.webmd.com/women/endometriosis/bowel-endometriosis
https://www.endometriosis-uk.org/endometriosis-and-bowel
https://www.endofound.org/gastrointestinal-distress
ENDOMETRIOSIS AND CONSTIPATION

Anti-Mullerian Hormone & Endometriosis – What’s The Connection?
Endometriosis has been associated with a marker called Antimullerian hormone (AMH), which is a pivotal marker of ovarian reserve, and is commonly measured in women with endometriosis specifically in relation to fertility. There is debate among the community that your AMH level is what it is and it cannot change. I would challenge this notion though as I have seen people with endometriosis have significant increases after proper excision surgery, which is a point of debate. Recently, I had another patient send me lab work that demonstrated what some may call a low AMH, has confirmed endometriosis, but likely a surgery that was incomplete and is continuing to suffer ongoing symptoms. Though I have seen this change in my patients, I recognize this is only a small fraction of the people suffering, so it was time to review what the research says. This article aims to provide a review of the various studies conducted on this critical subject, exploring how endometriosis and AMH interact, the effect of surgical intervention on AMH levels, and the subsequent impact on fertility.
The Antimullerian Hormone (AMH): A Brief Overview
AMH, a hormone playing diverse roles during embryonic development and puberty, is produced by ovarian follicles smaller than 8 mm, hence linking ovarian reserve to AMH levels in the blood. The normal range for AMH hovers between 1 and 4 ng/mL. However, women’s AMH levels greatly vary based on factors like age, ethnic background, lifestyle, and genetics. Additionally, someone at the low end of range may still suffer problems despite them being “in range.”
AMH Testing in Reproductive Health
AMH testing is a crucial tool for evaluating female fertility. It can assist in:
- Assisting with understanding the prognosis of a woman’s response to assisted reproduction techniques (ART) such as in vitro fertilization (IVF)
- Confirming other markers of menopause
- Providing a more comprehensive evaluation when certain conditions are confirmed or suspected such as polycystic ovarian syndrome (PCOS), premature ovarian failure, and endometriosis
Endometriosis and AMH Levels
Endometriosis is a common culprit behind infertility, affecting nearly half of the women suffering from this ailment. This infertility arises from various factors, including inflammation in the reproductive tract, scar tissue-induced decreased blood supply to the ovaries, and pelvic anatomical distortions. Research reveals a significant correlation between endometriosis and lower than average AMH levels.
Some argue that surgical intervention of endometriosis often leads to a reduction in AMH levels, though many of us in the community may argue that this is a more nuanced topic and this highly depends on the skill of the surgeon, something that is often overlooked in endometriosis research. Various studies have attempted to decipher the impact of endometriosis surgery on AMH levels and fertility outcomes. A retrospective study conducted in 2016 found that preoperative AMH levels did not influence pregnancy rates after surgery. This is consistent with the literature we have on surgical impact, and thus the need for better research in the future. In my experience, this is the opposite of what I have seen, as many of us have seen when people get to the right surgeon.
Laparoscopic Cystectomy on AMH Levels
Laparoscopic ovarian cystectomy, a common surgical procedure to treat endometriomas, has been associated with decreased ovarian reserve. A study in 2019 demonstrated significantly lower AMH levels in women who underwent laparoscopic endometrioma cystectomy, especially in cases with bilateral cysts larger than 7 cm and stage 4 endometriosis.
Considerations: I want to highlight that we do not know the skill of the surgeon, but we do know that the skill of the surgeon matters. That being said, large endometriomas can often overtake ovarian tissue which is what happened to Christina. Hear her story here. This is why it is extremely important to find a knowledgeable surgeon that you feel comfortable with. If you need help finding a surgeon, you can start here.
Laparoscopic Endometriosis Surgery on AMH Levels
A literature review and meta-analysis of 19 studies conducted between 2010 and 2019 on the impact of laparoscopic endometriosis surgery on AMH levels post-surgery revealed a decline in AMH levels, extending beyond six months post-surgery. This decline was more pronounced in cases where surgery was performed on both sides of the body, compared to a single side.
Again, I would argue that we consider the quality of the research and the skill of the surgeon. Remember, ablation is different from excision and this may be another factor that is skewing results. I repeat this because, like many of us in the community, this is not our experience, thus I often read research with these things in mind. If many others in the community are also seeing this, there must be more to consider than what is presented. The bottom line is that we need better research.
AMH Levels Post-Surgery for Endometrioma
Several studies have observed that laparoscopic ovarian cystectomy results in a significant and progressive decrease in AMH levels post-surgery. However, other studies have noted that this decrease may only be temporary, with levels potentially returning to normal within a year. Another factor to consider is when the AMH was measured post-surgery and what other factors may have impacted the levels!
Certain studies have observed a temporary decrease in AMH levels following endometrioma ablation. However, this decrease did not persist beyond six months in most cases, suggesting a potential recovery of ovarian reserves.
Several studies have compared the decrease in AMH levels following ovarian cystectomy and endometrioma vaporization. The general consensus suggests a higher postoperative decline in AMH levels following cystectomy compared to vaporization, particularly in bilateral endometrioma cases.
This caught my attention and highlights my thoughts on how the surgery (excision) is being performed as to not compromise ovarian tissue. Using ablation, which is what the CO2 laser is referring to, may not compromise the ovarian tissue, but it also may not treat the disease. Paul Tyan, MD discusses this complex topic in our interview which you can find here.
The combined technique, involving partial cystectomy and ablation, has been shown to have less detrimental effects on the ovary, resulting in a lesser decline in AMH levels post-surgery.
The role of endometriosis surgery in improving pregnancy rates remains a topic of debate. Some studies suggest that surgery might improve the success rates of fertility treatment, while others highlight the risk of ovarian damage due to surgical intervention.
In conclusion, the Antimullerian hormone is a vital marker for assessing the impact of endometriosis and its surgical intervention on ovarian reserve and fertility. Understanding the complex relationship between AMH levels, endometriosis, and surgical intervention along with identifying gaps in the research can help medical professionals devise more effective treatment strategies, improve the quality of research studies which ultimately improves patient outcomes.
IRelated Reading:
- Does Endometriosis Cause Infertility? Covering the Basics
- Endometriosis and Pregnancy: Natural, Medical, & Surgical Options
References:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6603105/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7865255/
- https://drseckin.com/endometriosis-surgery-and-amh-levels/
Endometriosis and Inflammatory Bowel Disease: Distinguishing the Differences
Exploring the complex world of health and medical conditions can sometimes feel like navigating through a labyrinth. The similarities between certain conditions often blur the lines, making it challenging for individuals and even healthcare professionals to differentiate between them. This is notably true in the case of endometriosis and inflammatory bowel disease (IBD), two disorders that share several overlapping symptoms and characteristics. We’ve recently been discussing endometriosis and the bowel, this article aims to shed light on these conditions, highlighting the differences, similarities, and the challenges faced in their diagnosis.
ICYMI: Colon Chronicles: Delving Into Bowel Endometriosis
Symptoms of Endometriosis
The signs and symptoms of endometriosis can vary greatly, making it a complex disease to diagnose. Some of the most common symptoms include dysmenorrhea (painful periods), dyspareunia (painful intercourse), chronic pelvic pain, and gastrointestinal symptoms like diarrhea, constipation, and abdominal pain. Because endometriosis symptoms often overlap with GI symptoms, getting a diagnosis in general can be tricky, but especially if it may be impacting the bowels which is estimated in about 5-12% of cases, whereas approximately 90% of those with endometriosis suffer from gastrointestinal symptoms. In many cases, these symptoms can be mistaken for other conditions, leading to delays in diagnosis.
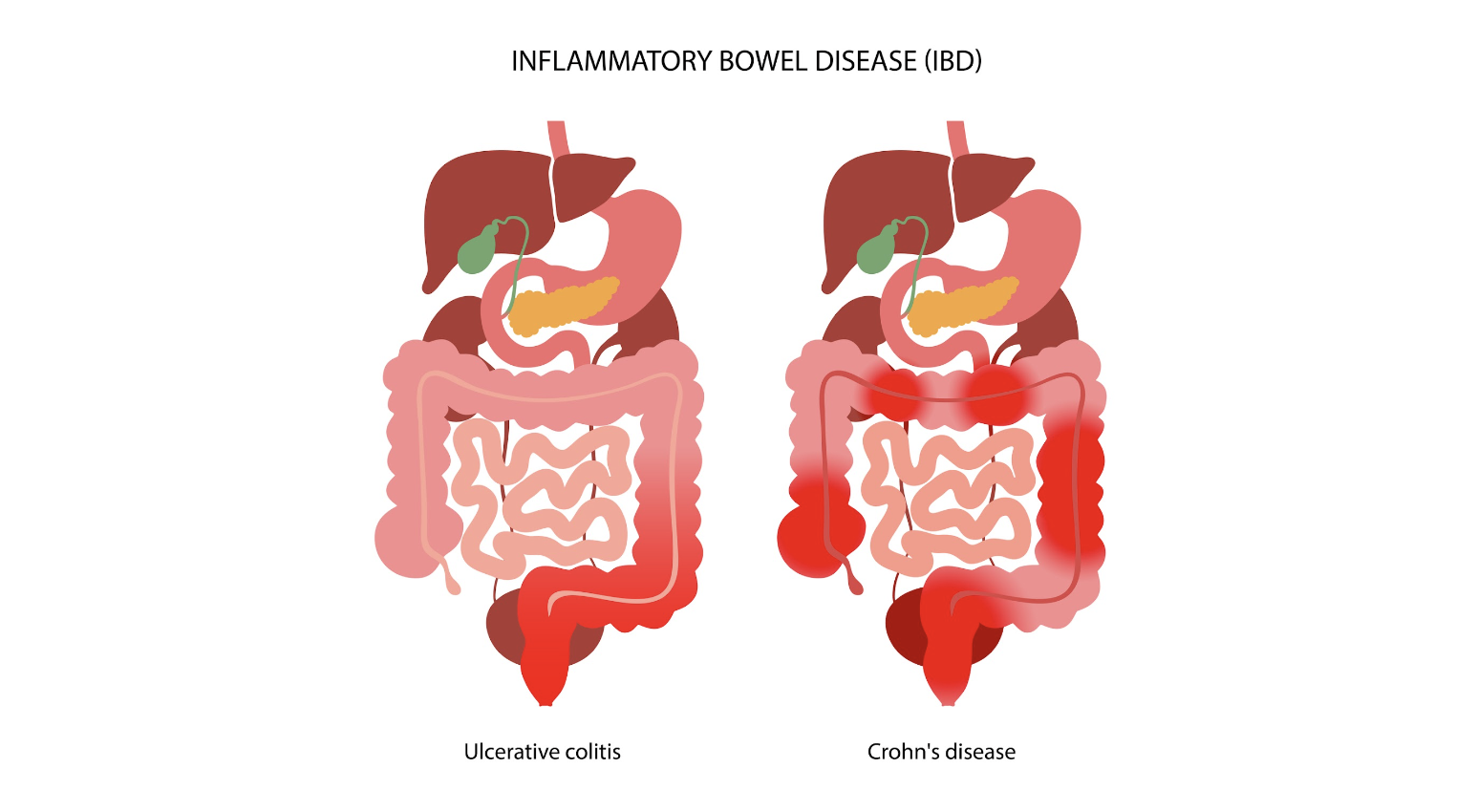
Inflammatory Bowel Disease: An Overview
Inflammatory bowel disease (IBD) is an umbrella term that encompasses two chronic autoimmune disorders: ulcerative colitis (UC) and Crohn’s disease (CD). These conditions are characterized by the chronic inflammation of the gastrointestinal tract, which can lead to a wide range of symptoms, including abdominal pain, diarrhea, weight loss, and fatigue.
The prevalence of IBD is highest in Europe, with reported cases reaching up to 505 per 100,000 for UC in Norway and 322 per 100,000 for CD in Italy. Like endometriosis, IBD can significantly impact an individual’s quality of life, necessitating long-term management strategies to control symptoms and prevent complications.
The Overlap: Endometriosis and IBD
Interestingly, endometriosis and IBD share several common traits, including immune dysregulation and overlapping clinical manifestations like abdominal pain and bowel-related symptoms. This overlap often poses a significant diagnostic challenge, as endometriosis can mimic IBD or vice versa, leading to delays or indeterminate diagnosis.
In fact, endometriosis has often been termed as having “IBD-like” features due to the similarities in symptoms and underlying pathophysiology. This has led to substantial interest in the potential link between these conditions, with several studies investigating the co-occurrence of endometriosis and IBD.
Investigating the Link: Endometriosis and IBD
To understand the potential link between endometriosis and IBD, numerous studies have been conducted, ranging from case reports and clinical series to epidemiological research. These studies have reported varying results, further highlighting the complexity of these conditions and the challenges associated with their diagnosis and management.
Case Reports and Clinical Series
Many case reports have been published that highlight the diagnostic challenges associated with endometriosis and IBD. For instance, several cases have been reported where an initial diagnosis of CD was later revised to intestinal endometriosis upon histopathological examination. Similarly, other case reports have documented instances where an initial diagnosis of UC was later confirmed to be appendiceal endometriosis.
Conversely, there have also been cases where an initial diagnosis of endometriosis was later revised to be CD upon histopathological examination. Additionally, several case reports have documented instances where both CD and endometriosis were diagnosed in the same patient.
Epidemiological Studies
In addition to case reports and clinical series, several epidemiological studies have investigated the co-occurrence of endometriosis and IBD. One such study, a nationwide Danish cohort study, reported a 50% increase in the risk of IBD in women with endometriosis compared to the general population. This increased risk persisted even more than 20 years after a diagnosis of endometriosis, suggesting a genuine association between the two conditions..
Another study, a retrospective cross-sectional study conducted in Israel, found that 2.5% of patients with endometriosis also had a diagnosis of IBD, compared to 1% in the general population. A recent Italian case-control study found that among 148 women with endometriosis, five had IBD, although this did not reach statistical significance.
The Challenge of Temporality
One of the critical aspects of evaluating the association between endometriosis and IBD is the issue of temporality, or the order in which the conditions are diagnosed. Many studies do not provide information on the temporal sequence of endometriosis and IBD, which poses a significant challenge in determining a cause-effect relationship between the two conditions.
Furthermore, the diagnosis of endometriosis often faces delays, with an average delay of seven years estimated between the onset of symptoms and definitive diagnosis. This delay further complicates the evaluation of the temporal relationship between endometriosis and IBD.
Distinguishing Between Endometriosis and IBD
Given the overlapping symptoms and shared characteristics of endometriosis and IBD, distinguishing between these conditions can be challenging. Both conditions can result in similar symptoms, such as abdominal pain and bowel-related symptoms, which can lead to misdiagnosis or delayed diagnosis.
In cases where endometriosis and IBD coexist, the symptoms can be atypical and cyclic, and fibrosis caused by chronic inflammation can lead to obstruction of the intestinal lumen. Therefore, it’s essential for healthcare professionals to consider both conditions when evaluating patients with such symptoms.
In cases of intestinal endometriosis, endoscopic biopsies may reveal IBD-like lesions. However, these lesions may represent an epiphenomenon of endometriosis rather than a true IBD. Hence, patients with concurrent IBD and endometriosis should be adequately followed up for the reassessment of IBD diagnosis over time.
Related Reading: Understanding Bowel Endometriosis
The Role of Treatment in the Risk of IBD
The treatment of endometriosis could potentially influence the risk of developing IBD. For instance, oral contraceptives are a common treatment for endometriosis, and a meta-analysis of 14 studies suggested an increased risk of IBD among users of oral contraceptives. Additionally, non-steroidal anti-inflammatory drugs (NSAIDs), often used for pain relief in endometriosis, have been reported to increase the risk of IBD.
The Need for Further Research
Though existing research has shed some light on the association between endometriosis and IBD, there is still much to uncover. Further research is needed to better understand the temporal relationship between endometriosis and IBD in cases of co-occurrence and identify predictors that could be useful for evaluation and management of these patients.
Understanding these conditions and their potential links can not only improve diagnostic accuracy but also inform treatment strategies and improve the quality of life for those affected.
Distinguishing between endometriosis and inflammatory bowel disease can be a challenging task due to the overlapping symptoms and shared characteristics of these conditions. However, understanding the nuances of these conditions and the potential links between them can lead to improved diagnostic accuracy and more effective treatment strategies. As research progresses in this area, we hope to gain a better understanding of these complex conditions and continue to improve the lives of those affected.
Related Reading:
- Finding an Endometriosis Specialist: Your Guide to Effective Treatment
- Unraveling the Connection Between Endometriosis and Autoimmune Diseases
References:
- Parazzini F, Luchini L, Vezzoli F, Mezzanotte C, Vercellini P. Gruppo italiano perlo studio dell’endometriosi. Prevalence and anatomical distribution of endometriosisin women with selected gynaecological conditions: results from amulticentric Italian study. Hum Reprod 1994;9:1158–62.
- Bulun SE. Endometriosis. N Engl J Med 2009;360:268–79.
- Weed JC, Ray JE. Endometriosis of the bowel. Obstet Gynecol 1987;69:727–30.
- Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology 2012;142:46–54.
- Nielsen NM, Jorgensen KT, Pedersen BV, Rostgaard K, Frisch M. The co-occurrence of endometriosis with multiple sclerosis, systemic lupus erythematosus and Sjogren syndrome. Hum Reprod 2011;26:1555–9.

Life After Endometriosis Surgery: A Comprehensive Guide
Endometriosis, a chronic and often debilitating condition, affects numerous women worldwide. Surgery, specifically laparoscopic excision, is considered the gold standard for treatment. However, what is life like after endometriosis surgery? This comprehensive guide explores various aspects of life after endometriosis surgery, including recovery, physical and mental health, fertility, and the overall quality of life.
Understanding Endometriosis and Its Surgical Treatment
Endometriosis is a condition where tissue similar to the lining of the uterus grows outside the uterus, causing adhesions, fibrosis, and lesions in organs such as the intestines or bladder. The symptoms can be severe, including pelvic pain, dysmenorrhea, and even infertility.
Laparoscopic excision surgery is currently deemed the most effective method for diagnosing and treating endometriosis. In this procedure, endometriosis lesions and their surrounding tissue are cut out and removed. Despite its efficacy, access to endometriosis excision specialists can be limited, expensive, and frequently not covered by insurance.
Read More: Endometriosis Surgery Costs: Everything You Need to Know
The Post-Surgery Recovery Period
Recovery from endometriosis surgery largely depends on the extent of the disease and the individual’s overall health. Most surgeries are minimally invasive, involving only a few small incisions and a laparoscope to guide the surgeon’s tools. Recovery might take several weeks to months, with patients often feeling more tired in the first week after surgery.
Patients are typically advised to consume soft, easily digestible foods, drink adequate fluids, and take fiber supplements and laxatives to prevent constipation, especially if they are on narcotic pain medication. Strenuous activities should be avoided, although short walks are encouraged.
How long should you take off work after endometriosis excision surgery?
How long you take off work after endometriosis excision surgery depends on your case and factors such as how much endometriosis is removed, how physical your job is, your pain levels and symptoms after surgery, and any complications. The recommended time could vary from one week to over one month. This is something you should discuss with your surgeon before excision surgery.
Read More: Physical therapy before excision surgery for endometriosis
Physical Health After Surgery
According to a study, the physical health component of quality of life (QoL) in women with endometriosis can be positively correlated with age. However, in a study, women with deep endometriosis haa worse physical and social functions compared to the norm in Spanish women.
The physical health component of QoL includes physical function, physical role, body pain, and general health. Bodily pain, especially, can significantly improve after surgery.
Read More: Endometriosis what to do after diagnosis
Mental Health After Surgery
Mental health is another crucial aspect to consider in life after endometriosis surgery. Emotional role, mental health, and vitality are areas that could improve significantly after surgery.
However, it is essential to note that the emotional strain of enduring a chronic disease like endometriosis can lead to mental health disorders like anxiety or depression in 60% of patients. Therefore, mental health support should be incorporated into post-surgery care.
Fertility and Family Planning After Surgery
Fertility and family planning are significant concerns for many women with endometriosis. Studies show that surgery could double the spontaneous pregnancy rate in people with mild endometriosis. Those with moderate to severe endometriosis also have improved spontaneous birth rates after the laparoscopic removal of endometrial-like lesions.
However, even after successful surgery, some women may struggle with fertility issues. It is essential to have a candid discussion about fertility and family planning with your healthcare provider before surgery.
Financial Implications of Endometriosis Surgery
Endometriosis surgery can be costly, and financial wellness can significantly impact the individual’s mental and physical wellness and quality of life. Many excision surgeons in the United States are not in-network with insurance, which may result in higher out-of-pocket rates.
Patients should discuss expected costs with their insurance company and surgeon’s office before surgery and develop a savings plan for future surgery if needed. For people who are uninsured or underinsured, some excision specialists may offer payment plans or connect patients with grants or donated surgeries.
Coping with the Potential Return of Endometriosis After Surgery
Despite the effectiveness of surgery in improving symptoms, endometriosis can reoccur. Studies have shown that over ten years, 51% of women needed another surgical intervention to treat a recurrence of endometriosis.
Risk factors for a follow-up procedure include being under age 30 at the time of the original surgery, endometriosis in the ovaries, endometriosis patches that were not entirely removed, certain subtypes of endometriosis, and the skill of the original surgeon in removing most endometriosis tissues.
Embracing a Healthy Lifestyle After Surgery
Well-being after endometriosis surgery is essential for physical and mental health. Patients are encouraged to lead a healthy lifestyle, which includes drinking plenty of fluids, exercising regularly, maintaining a healthy weight, and eating a diet rich in omega 3, vitamin E, vitamin C, and citrus. Smoking and excessive alcohol intake should be avoided.
In addition, patients should be watchful for signs of infection such as fever, shaking chills, and redness or oozing of the incision sites, and report these to their healthcare provider immediately.
A Final Note
Life after endometriosis surgery can be a journey of healing and rediscovery. While the journey may be challenging, it is essential to remember that you are not alone. Reach out to your healthcare provider, join support groups, and lean on your loved ones. Remember, every step you take towards recovery is a step towards a healthier, happier you.
References:
https://my.clevelandclinic.org/health/treatments/4620-endometriosis-surgery
https://www.verywellhealth.com/endometriosis-surgery-7377270
https://pacificendometriosis.com/postop-care-the-next-6-12-weeks/
https://www.verywellhealth.com/endometriosis-excision-surgery-6385621
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9605478/

Understanding Bowel Endometriosis
Bowel Endometriosis is a debilitating chronic health condition that affects a significant number of women worldwide. This disease is characterized by the growth of endometrial-like tissue outside the uterus, specifically on or inside the bowel walls. The condition often presents with varying gastrointestinal symptoms like painful bowel movements, constipation, and diarrhea, making it difficult to diagnose.
What is Bowel Endometriosis?
Bowel Endometriosis is a specific form of endometriosis that involves the intestines. In this condition, cells similar to those that line the uterus start growing on the bowel or even penetrate into the bowel wall. This growth can lead to painful and uncomfortable symptoms, particularly during a woman’s menstrual cycle.
Prevalence and Affected Areas
Bowel Endometriosis is a subset of a larger condition, endometriosis, affecting 1 in 5 endo patients. The most common sites for bowel involvement are the rectum, appendix, sigmoid, cecum, and distal ileum. It’s also worth noting that bowel endometriosis frequently co-exists with endometriosis in other areas, making it a multifaceted disease that requires comprehensive treatment.
Symptoms of Bowel Endometriosis
Understanding the symptoms of bowel endometriosis can help in early diagnosis and treatment. It’s essential to note that these symptoms often overlap with other gastrointestinal conditions, making it a challenging disorder to diagnose.
Common Symptoms
- Painful bowel movements: This is one of the most common symptoms of bowel endometriosis. The pain is often described as sharp or cramping and may worsen during menstruation.
- Constipation and Diarrhea: Changes in bowel habits are another common symptom. Some women may experience constipation, while others may have diarrhea. These symptoms may also worsen during menstruation.
- Rectal Bleeding: While not as common, some women may experience rectal bleeding, particularly during their menstrual period. A healthcare professional should always evaluate this symptom as it can also be a sign of other serious conditions.
- Abdominal Pain: Abdominal pain, often worsening during the menstrual cycle, is another common symptom. The pain can range from mild to severe and may be constant or intermittent.
- Dyspareunia: Dyspareunia, or painful sex, is another symptom that may indicate the presence of bowel endometriosis. This pain often stems from endometriosis lesions in the posterior pelvic compartment peritoneum, an area around the rectum that includes the surface peritoneum, commonly called the pouch of Douglas.
Diagnosing Bowel Endometriosis
Diagnosing bowel endometriosis can be challenging due to the overlap of symptoms with other gastrointestinal disorders. However, several diagnostic tools can aid in the identification of this condition.
Physical Examination and Patient History
A detailed patient history and a thorough physical examination are crucial first steps in diagnosing bowel endometriosis. The doctor will ask about the symptoms, their severity, and if they worsen during menstruation. A pelvic exam may also be performed to check for any abnormalities.
Imaging Tests
Imaging tests, such as transvaginal sonography (TVS) and magnetic resonance imaging (MRI), are commonly used to identify and characterize endometriosis lesions.
TVS is a first-line imaging technique providing detailed dynamic images of the pelvis with minimal patient discomfort. It helps identify all of the bowel’s layers and any potential endometriosis nodules.
MRI, on the other hand, is typically used as a second-line diagnostic tool. It excels in evaluating the extent of the disease and identifying any specific organ involvement and depth of infiltration.
Endoscopy and Biopsy
An endoscopy may also be performed to examine the bowel for any abnormalities. A biopsy can be taken during this procedure to check for the presence of endometriosis cells. However, this method has its limitations as it only provides a superficial sample, and endometriosis usually involves deeper layers of the bowel wall.
Laparoscopy
Laparoscopy is the gold standard for diagnosing endometriosis. This surgical procedure allows for visual inspection of the peritoneal cavity and can provide a definitive diagnosis. The surgeon can also assess the extent of the disease and its impact on other organs.
Misdiagnosis of Bowel Endometriosis
Bowel endometriosis is often misdiagnosed due to its similar symptoms to other gastrointestinal disorders. This condition is frequently mistaken for irritable bowel syndrome (IBS), Crohn’s disease, and even colon cancer.
It’s crucial for healthcare providers to consider a possible diagnosis of bowel endometriosis in women presenting with gastrointestinal symptoms, especially if these symptoms worsen around the menstrual cycle.
Treatment of Bowel Endometriosis
Treating bowel endometriosis is typically multidisciplinary, involving a team of specialists. It generally involves a combination of medical and surgical therapies.
Medical Therapy
Medical treatments aim to control the symptoms of bowel endometriosis and may include pain relievers, hormonal therapies like oral contraceptives or progestins, and gonadotropin-releasing hormone analogs. These treatments work by reducing inflammation and suppressing the growth of endometrial tissue.
Surgical Therapy
In more severe cases, or when medical therapy is ineffective, surgery may be necessary. The type of surgery will depend on the extent and location of the endometriosis. In some cases, a conservative approach may be used, where the surgeon attempts to remove the endometriosis while preserving as much of the bowel as possible. In other cases, a segment of the bowel may need to be removed.
Laparoscopic Surgery
Laparoscopic surgery is often the preferred method for treating bowel endometriosis. This minimally invasive procedure allows for precise removal of the endometriosis with less damage to surrounding tissue and quicker recovery times. However, it requires a skilled surgeon and may only be an option in some cases.
Read More: Why It’s Important Your OB-GYN Specializes in Endometriosis?
Bowel Endometriosis and Fertility
Research indicates that bowel endometriosis may have an impact on a woman’s fertility. This could be due to the inflammation and scarring caused by the disease, which can interfere with the normal function of the reproductive organs.
In cases where infertility is an issue, assisted reproductive technologies may be considered. However, surgery to remove the endometriosis is often recommended first to increase the chances of a successful pregnancy.
Read More: Does Endometriosis Cause Infertility?
Conclusion
Bowel endometriosis is a complex condition that can significantly impact a woman’s quality of life and fertility. Early diagnosis and effective treatment are crucial to managing this condition and minimizing its effects. Suppose you’re experiencing symptoms of bowel endometriosis. In that case, it’s important to consult with a healthcare provider who is knowledgeable about this condition and can guide you through the diagnosis and treatment process.
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6996110/
https://drseckin.com/bowel-endometriosis/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6397811/

Through the Looking Glass: Reflecting on 2023
Embarking on the journey of self-reflection is not just a personal endeavor; for us at iCareBetter, it’s a collective celebration of progress, community, and collaboration. As we bid farewell to 2023, a year marked by challenges and triumphs, it’s time to take a look into the past year and reflect on all that has been accomplished. Join us as we navigate through the areas of growth, community involvement, projects, and meaningful collaborations that shaped our year. In this special blog post, we’re excited to share the insights gained from our podcast endeavors and offer a sneak peek into the thrilling developments that await us in 2024. Let’s rewind, recap, and anticipate the exciting narrative that continues to unfold in the ever-evolving story of iCareBetter.
About iCareBetter
iCareBetter is an innovative platform dedicated to helping patients with endometriosis and chronic pelvic pain find compassionate and skilled experts. All experts on iCareBetter have shown knowledge and expertise in the treatment of endometriosis and chronic pelvic pain.
Vision
Our vision is to reduce the symptom-to-effective treatment of endometriosis to less than a year. Studies show that patients with endometriosis spend an average of 7.5 years to have an official diagnosis. Moreover, even after the diagnosis, patients will have to spend several years with multiple failed treatment attempts. After the long delays in diagnosis and treatment, they might be lucky enough to receive effective treatment from an expert.
Mission
Our mission is to improve access to high-quality specialized care for those with endometriosis. iCareBetter wants to combat the issue of patients living in confusion, pain, and isolation. To that end, we hope to connect as many patients to the right experts as early as possible. And we hope that this will ensure timely diagnosis and effective treatment.
To read more about why iCareBetter was built and the inspiration behind it, check out our blog here and listen to episode 1 of the podcast here, where Saeid and Jandra give you a behind the scenes look into what inspired them.
What happened in 2023?
In 2023, iCareBetter grew in many ways, including new avenues to provide education along with collaboration from the community. Here are some of the highlights!
- We started a podcast! iCareBetter: Endometriosis Unplugged is hosted by Jandra Mueller, DPT, MS a pelvic floor physical therapist and endometriosis patient. The podcast is available on Spotify, Apple Podcasts, and Youtube.
- We had 19 weekly episodes in season one
- Listeners joined from all over the world, reaching 22 countries
- We brought on a team to help with new content on social media creating a more visually appealing platform, community engagement, and followers.
- We now have 211 providers on our website available and ready to help those suffering from endometriosis and we are continuing to grow!
- Our blog content is now consistent with twice weekly posts bringing you updates on all things endometriosis.
What To Expect in 2024
While 2023 was a big year for iCareBetter, we hope to continue the growth and expand our providers across the globe. Our hope is to increase our collaboration with medical specialists, researchers, and advocates. There are some exciting things to come in 2024 including a new season of iCareBetter: Endometriosis Unplugged as well as some other projects that will be announced in 2024.
We hope you have found our resources helpful either for yourself or a loved one, and hope you continue to share the love and spread the word about Endometriosis. All of us here at iCareBetter wish you a safe and happy new year.

Cheers to 2024!
Do you or a loved one have Endometriosis? Here are some blogs that may help you get started on your journey.
- Endometriosis Signs and Symptoms: Everything You Need to Know
- Endometriosis Facts & Myths: Dispelling the Misconceptions

Women’s Health Research and the White House Initiative
Merry Christmas and Happy Holidays! It’s time for some good news when it comes to researching ‘women’s diseases.’
Women’s health has long been an area that has been overlooked and understudied in medical research. Despite making up more than half of the population, women have historically been underrepresented in clinical trials and medical studies, leading to significant gaps in knowledge and understanding of women’s health issues. However, recent developments, such as the establishment of the White House Initiative on Women’s Health Research, are changing the landscape and paving the way for a new era of research and innovation in women’s health.
The Historical Underrepresentation of Women in Research
For decades, women’s health needs were considered a low priority in the scientific and medical fields. During the 1970s, when the women’s health movement emerged as part of the larger women’s movement, it became apparent that women were significantly underrepresented in medical and scientific research. At that time, there were few women working in medicine and science, and the lack of representation had serious implications for the understanding and treatment of women’s health conditions.
One significant example of the cautious approach towards including women in research was the Food and Drug Administration’s policy in 1977, which recommended excluding women of childbearing potential from early-stage drug trials. This policy was a response to the tragic consequences of the drug thalidomide, which caused severe birth defects in thousands of babies born to women who had taken the drug during pregnancy. While the intention was to protect women from potential harm, it resulted in a lack of data on how drugs specifically affected women.
The Shift Towards Inclusion and Advocacy
As awareness grew about the exclusion of women from research studies, advocacy groups and activists began to protest for change. They argued that individual women should be allowed to make informed decisions about participating in research and that excluding women limited their access to potentially life-saving treatments. The Public Health Service Task Force on Women’s Health Issues, in their 1985 report, called for long-term research on how behavior, biology, and social factors affect women’s health, further highlighting the need for inclusion.
In response to these concerns, the National Institutes of Health (NIH) established a policy in 1986 that encouraged the inclusion of women in studies. This policy, published in the NIH Guide for Grants and Contracts in 1987, urged researchers to include women and minorities in their studies and provided guidelines for doing so. The policy was further reinforced in 1989 when NIH announced that research solicitations should prioritize the inclusion of women and minorities.
The Founding of the White House Initiative on Women’s Health Research
In 1990, the Congressional Caucus for Women’s Issues requested an investigation into NIH’s implementation of guidelines for the inclusion of women in research studies. The subsequent report by the General Accounting Office (now known as the Government Accountability Office) highlighted inconsistencies in applying the inclusion policy and the need for improved communication. As a result, the Office of Research on Women’s Health (ORWH) was established in 1991 to monitor and promote the inclusion of women in research.
Under the leadership of Dr. Bernadine Healy, the first female NIH Director, the Women’s Health Initiative was launched in 1991. This initiative consisted of clinical trials and an observational study involving over 150,000 postmenopausal women. The trials aimed to investigate the effects of hormone therapy but was stopped due to incorrect interpretation of the data resulting in the majority of women stopping their hormone therapy overnight, literally. We are still dealing with the consequences of this today.
Legislation and Policies to Ensure Inclusion
While the inclusion of women in research was initially an NIH policy, it became federal law in 1993 through the NIH Revitalization Act. This act included provisions requiring the inclusion of women and minorities in clinical research funded by NIH. The law mandated that NIH ensure the inclusion of women and minorities and that trials be designed to analyze whether variables affect women and minorities differently. It also emphasized that cost should not be a reason for exclusion and called for outreach efforts to recruit diverse populations for clinical studies.
Since the establishment of the ORWH, the office has monitored adherence to inclusion policies and guidelines. Researchers receiving NIH funding are required to report on the sex, race, and ethnicity of participants enrolled in clinical trials. These reports contribute to the ongoing efforts to promote inclusivity and address health disparities among different populations.
Improving Women’s Health Through Research
The White House Initiative on Women’s Health Research, announced by President Biden and led by First Lady Jill Biden, signifies a renewed commitment to advancing women’s health research. The initiative aims to galvanize the federal government, private sector, and philanthropic communities to close research gaps, address health disparities, and pioneer the next generation of discoveries in women’s health.
Under this initiative, concrete recommendations will be delivered to the Biden-Harris Administration within 45 days, outlining actions to improve research on women’s health and maximize investments in this field. Priority areas of focus will be identified to ensure transformative outcomes, ranging from heart attacks in women to menopause and beyond. The initiative also seeks to engage stakeholders from the scientific, private sector, and philanthropic communities to drive innovation and foster collaborative partnerships.
By prioritizing research on women’s health, we can gain a deeper understanding of conditions and diseases that predominantly affect women, such as endometriosis, cardiovascular disease, and Alzheimer’s disease. This knowledge will enable healthcare providers to better prevent, diagnose, and treat these conditions, ultimately improving the lives of millions of women.
The establishment of the White House Initiative on Women’s Health Research and the ongoing efforts to promote inclusion in medical research mark significant milestones in addressing the historical underrepresentation of women in studies. Through policies and legislation, initiatives like the Women’s Health Initiative, and the monitoring of adherence to inclusion guidelines, progress is being made to close research gaps and improve women’s health outcomes.
Research plays a crucial role in understanding the unique aspects of women’s health and developing effective treatments and interventions. By prioritizing and investing in research on women’s health, we can empower women, healthcare providers, and researchers to make informed decisions and advancements that will positively impact the health and well-being of women across the nation. The White House Initiative on Women’s Health Research is a vital step towards achieving this goal and creating a future where women’s health is fully understood, supported, and prioritized.
What you can do!
The Initiative is accepting written comments and input, we urge everyone to get involved.
You can send in either a word document or PDF file to WomensHealthResearch@who.eop.gov
Related reading:
- Endometriosis Signs and Symptoms: Everything You Need to Know
- Endometriosis Facts & Myths: Dispelling the Misconceptions
- Why was iCareBetter built?
References:
- https://www.whitehouse.gov/briefing-room/statements-releases/2023/11/13/fact-sheet-president-joe-biden-to-announce-first-ever-white-house-initiative-on-womens-health-research-an-effort-led-by-first-lady-jill-biden-and-the-white-house-gender-policy-council/
- https://www.whitehouse.gov/gpc/briefing-room/2023/11/17/launch-of-white-house-initiative-on-womens-health-research/
- https://www.whitehouse.gov/briefing-room/speeches-remarks/2023/11/13/remarks-by-president-biden-and-first-lady-jill-biden-establishing-the-first-ever-white-house-initiative-on-womens-health-research/
- https://orwh.od.nih.gov/toolkit/recruitment/history#:~:text=Inclusion%20Becomes%20Law&text=In%201993%2C%20Congress%20wrote%20the,as%20Subjects%20in%20Clinical%20Research.

Endometriosis: Is it a Disability?
Endometriosis, a debilitating condition affecting millions of women globally, often prompts questions about its influence on daily life and work ability. This article provides an in-depth analysis of endometriosis, how it affects women’s work ability, and the possibility of qualifying for disability benefits.
Endometriosis is a medical condition that primarily affects women during their reproductive years, and is very prevalent, with over 80 million women diagnosed worldwide, typically between the ages of 20 and 40. Treatments such as surgery and medical management as well as physical therapy can alleviate some symptoms, but there is currently no definitive cure for the disease.
Endometriosis and Disability: An Intricate Relationship
The symptoms of endometriosis vary greatly among individuals. The most common symptom is pelvic pain, particularly during menstruation, sexual intercourse, bowel movements, or urination. Other symptoms include abdominal bloating, nausea, as well as infertility, among other symptoms.
Endometriosis can significantly disrupt daily functioning due to associated symptoms such as pain, fatigue, and psychological distress especially during one’s menses (period) but is not always confined to that time of the month. Consequently, the disease might qualify as a disability under the Americans with Disabilities Act (ADA) in certain cases. However, it is important to know that the Social Security Administration (SSA) does not automatically classify endometriosis as a disability.
Endometriosis and Social Security Disability Benefits
Qualifying for Social Security disability benefits due to endometriosis is not straightforward. The SSA considers two primary factors when determining if an individual qualifies for SSDI (Social Security disability insurance) or SSI (Supplemental Security Income) disability benefits:
1. Does the individual’s condition meet (or equal) the requirements of a listed impairment?
2. If not, do the symptoms of endometriosis significantly interfere with the individual’s ability to function, to the point where they cannot perform any type of job safely?
Since endometriosis is not listed as a qualifying condition, sufferers cannot automatically meet the first criterion. However, they might still qualify for Social Security disability if their symptoms significantly impede their ability to work, what the SSA calls “substantial gainful activity,” or SGA.
How to Qualify for Social Security Disability for Endometriosis
To qualify for Social Security disability due to endometriosis, it must be demonstrated that the symptoms of the disease prevent the afflicted individual from performing their job. The SSA will then assess if there is any type of job that the individual can safely perform. This evaluation considers medical records, age, work experience and job skills, education, and residual functional capacity (the minimum work that can be expected from an individual).
Applying for Social Security Disability for Endometriosis
Applications for Social Security disability benefits can be made online, through a phone call to the Social Security’s national office, or in person at a local Social Security field office. Winning a disability claim for endometriosis can be challenging, but applicants can seek assistance from an experienced disability attorney or non-attorney representative.
Endometriosis and Employment: A Complex Scenario
While endometriosis can significantly impact an individual’s ability to work, it does not automatically lead to unemployment or early retirement. In fact, many women suffering from endometriosis are able to maintain their employment status, albeit with certain adjustments to accommodate their symptoms.
Work Ability and Endometriosis
A woman’s ability to work can be severely compromised by endometriosis, with the disease often linked to poor work ability at age 46. This decreased work ability can lead to increased absence from work due to health issues. However, despite the increased absenteeism, women with endometriosis often maintain an employment rate comparable to women without the disease. It makes you question why?
Over the past few years, emphasis has been put on staying home if you are sick, as a safety measure for spreading disease, though many with endometriosis may not be able to afford days off of work either because financially they are unable, or there is worry about saying PTO for an unexpected turn of event such as a necessary surgery, or increased symptoms causing debilitating pain. So we suffer through expecting there to be worse days. Women in general, tend to minimize their own symptoms or question if they are “really that bad” as a result of societal influences.
Disability Retirement and Endometriosis
The emergence of disability retirement due to endometriosis is not common. Despite the debilitating symptoms of the disease, the risk of early retirement is not significantly higher for women with endometriosis compared to those without the condition. This finding is encouraging and demonstrates the resilience and determination of women battling this condition. Or, is it that those with endometriosis stay working longer because of the financial need and medical bills?
Conclusion
Endometriosis is a complex and debilitating condition that can significantly impact a woman’s ability to work. However, it does not inevitably lead to unemployment or early retirement per the literature, though that does not mean that those living with the condition are able to work feeling well or without worry about consequences of not working. With appropriate medical treatment and workplace accommodations, we hope that not only can those with endometriosis keep working, but with a higher quality of life while working.
Related Reading:
- Endometriosis Facts & Myths: Dispelling the Misconceptions
- Endometriosis Signs and Symptoms: Everything You Need to Know
- Endometriosis Signs and Symptoms: Everything You Need to Know
References:
- The Americans with Disabilities Act www.ada.gov
- Rossi, H., Uimari, O., Arffman, R., Vaaramo, E., Kujanpää, L., Ala‐Mursula, L., Piltonen, T.T., 2021. The association of endometriosis with work ability and work life participation in late forties and lifelong disability retirement up till age 52: A Northern Finland Birth Cohort 1966 study. Acta Obstetricia et Gynecologica Scandinavica 100, 1822–1829.

Your Guide to Supporting a Loved One Through the Holidays: The Ultimate Endometriosis Resource List Updated and Revised
The holiday season can be a joyous time filled with festivities, but for individuals navigating the challenges of endometriosis, it can also present unique hurdles. Supporting a loved one with endometriosis during this time involves not only empathy but also understanding the complexities of the disease. To aid both those directly affected and their support systems, a plethora of resources are available, ranging from insightful blogs and informative books to engaging movies and podcasts. These tools not only offer a wealth of knowledge about endometriosis but also provide a platform for individuals seeking a better understanding of the condition or those desiring to support their loved ones effectively.
In this guide, we will explore a curated selection of resources, offering both emotional support, educational insights, and even some ideas for your holiday shopping list to help individuals navigate the holiday season with a heightened awareness of endometriosis and a supportive approach to those impacted by this often misunderstood condition.
Understanding Endometriosis
For those of you unfamiliar with our blog, endometriosis is a chronic disease that primarily affects women (XX) of reproductive age. It involves the growth of endometrial-like tissue (the tissue that lines the inside of the uterus) outside of the uterus, leading to inflammation and pain, particularly during menstruation, though many other symptoms may be present.
For more information on symptoms of endometriosis, read our blog 20 Signs and Symptoms of Endometriosis.
Despite being a common condition, endometriosis is often misdiagnosed or overlooked, leading to many women suffering in silence. However, with the right information, supportive community, and access to informed medical providers, it is possible to manage the condition and lead a fulfilling life.
Podcasts on Endometriosis
Podcasts are an excellent way of gaining insights and information about endometriosis in a convenient and accessible format. Here are some podcasts that delve into various aspects of the disease, from personal stories to expert opinions:
- “iCareBetter: Endometriosis Unplugged”: Hosted by yours truly, is a video podcast (Spotify & Youtube) that focuses on expert interviews and patient stories with a few bonus episodes of specialists who treat conditions that often coexist with those with endometriosis. We have completed season 1 and hope to have season 2 coming in 2024!
- “In Sixteen Years of Endometriosis”: Hosted by two witty best friends who share their personal journey with the disease, this podcast offers a blend of humor, vulnerability, and accurate information.
- “The Cycle”: This podcast features stories of people living with endometriosis from around the world, providing practical ways to cope with the disease.
For more podcasts about endo, check out our previous blog here.
Books about Endometriosis
Reading about endometriosis can provide a comprehensive understanding of the disease. Here are some books written by medical experts and those living with the condition:
- “Beating Endo: How to Reclaim Your Life from Endometriosis”: Written by Iris Kerin Orbuch, MD, and Amy Stein, DPT, this book provides actionable insights into understanding and managing the disease.
- “Heal Endo”: By Katie Edmonds, (F)NTP provides a book that is patient focused with a more indepth understanding of the science balanced by actionable items that range from surgery to dietary and lifestyle changes.
- “The Endometriosis Health and Diet Program”: Authored by Dr. Andrew S. Cook, MD, FACOG, and Danielle Cook, MS, RD, CDE, this book focuses on treating endometriosis holistically, offering a comprehensive program tailored to individual needs.
- “Know Your Endo: An Empowering Guide to Health and Hope With Endometriosis”: Authored by Jessica Murnane, this book provides tools and strategies to manage chronic pain associated with endometriosis.
- “The Endo Patient’s Survival Guide: A Patient’s Guide to Endometriosis & Chronic Pelvic Pain”: This book by Andrew S. Cook, MD, FACOG, Libby Hopton, MS, and Danielle Cook, MS, RD, CDE, is a companion guide for patients, offering insights into diagnosis, treatment options, and achieving optimal relief.
Videos and Documentaries about Endometriosis
Visual content can help in understanding complex information about endometriosis. Several documentaries and movies have been produced to increase awareness about the disease.
- “Below the Belt”: A documentary from Shannon Cohn who created “Endo What?” focuses on the journey of several women seeking an endometriosis diagnosis and the challenges they face. “Below the belt” is not only an empowering film for educating the masses, it has become a tool for legislative change. A must see for everyone.
- “All about NINA”: A drama highlighting the experience of a woman, Nina Geld, managing her life with endometriosis.
- “Endo what?”: A documentary featuring women living with endometriosis and experts discussing treatment options.
- “The painful truth”: This film focuses on endometriosis and adenomyosis, another related condition.
- “A thousand needles”: A short documentary about the impact of endometriosis on a woman’s life.
- “End-o”: A short film showcasing the life of a young woman, Jaq, living with endometriosis.
- “The resilience of women in pain”: This short film focuses on Rose, a woman suffering from endometriosis and chronic illness, and her journey towards resilience.
Your Endo Shopping List: Comfort Tools for Loved Ones
In case you need to do some last minute shopping and want to show your loved ones you understand, here are some essential items that have proven useful for many. While these tools may not be able to stop this awful disease, they may provide some degree of comfort and relief when things get bad. Whether you are prepping for surgery, or just need some handy tools, here are some of my favorite items.
- Wedge Pillow. This is a must for those preparing for surgery during recovery. I only found this at my 3rd (and hopefully last) surgery and it was a game changer. When your belly is full of air, tender, and you don’t feel like moving (or sitting up at the very least), this helps to provide relief for recovering in bed or on the couch and is great if you are a side or back sleeper.
- Heating pads. This is probably the number one item most endo warriors have – likely at home and work. They are always handy to have wherever you are, and for a more personalized gift, ETSY.COM has some amazing endo swag (including heating pads).
- My Obi Apollo. This is a TENS unit with heat and multiple programs to help with cramps and reduce pain. To learn more about how TENS may be helpful, check out our blog here.
- Squatty Potty. Everyone should have one. This is the gift that no one really wants, but secretly is so happy when they get one. It is essential for optimal toileting for everyone, but especially if you have endometriosis. Constipation and pelvic floor dysfunction are two issues the majority of those with endometriosis suffer from and this tool can make a world of a difference for toileting….
Until recently, endometriosis was not a term most people were familiar with, unless you are suffering. It is amazing how this is shifting and so many more people are familiar with the term, but may not understand how impactful this disease is to one’s life. Finding the right surgeon is key to address the lesions, but having tools to help in the meantime is crucial. More importantly, your loved one will most appreciate the effort you made to educate yourself about their disease, especially during the stress the holidays may bring. Give them the gift of understanding and empathy this year, and maybe something to help their pain in the meantime.
Please note: We do not have financial affiliations with any of these products listed above.
Related Reading:
- Find an Endometriosis Specialist for Diagnosis, Treatment, & Surgery
- Endometriosis Facts & Myths: Dispelling the Misconceptions
- What You Need to Know About Endometriosis Excision Surgery
- Managing Endometriosis: What You Need to Know.

Preparing for the Holidays: Tips for Managing Flares
As the holiday season approaches, individuals grappling with endometriosis or other chronic illnesses are contemplating how to sidestep discomfort and flare-ups. Despite our concerted efforts to prevent or mitigate the frequency and intensity of flares associated with endometriosis, the truth remains that flare-ups are inevitable.
The holiday season holds the promise of joy, connections, and quality time with loved ones for many, but for others, it may bring stress, indulgence, worry, temptation, or even apprehension. The prospect of navigating gatherings, grappling with uncomfortable inquiries, or being compelled to make challenging food choices after diligently avoiding certain items for an extended period can be disheartening. Although flares may be an inherent part of the journey at any given time, holidays are no exception. The good news is that there are strategies available to effectively manage or minimize flares during these festive times!
Managing endometriosis or any chronic illness during the holiday season can present unique challenges, but there are strategies to help minimize flares and make the most of the festive season. Here are some tips:
Plan and Pace Yourself:
- Plan your activities and commitments wisely. Don’t overcommit to events or tasks.
- Prioritize what’s most important to you and conserve your energy for those activities.
Communicate Openly:
- Communicate with friends and family about your condition. Let them know your limitations and needs.
- Be open about your health concerns, so they can better understand and support you during gatherings.
- Or have a script of what you may want to say to those you do not want to share this information with such as: “Thank you for asking, though I’d prefer not to share those details right now, thank you for understanding.”
For a list of resources for yourself or others, check these out:
Choose Your Events:
- Select events that align with your energy levels and health status.
- It’s okay to decline invitations or leave early if you’re not feeling well.
Mindful Eating:
- Food is more than just its ingredients and nutrients, food is a major part of many of our cultures, enjoy it!
- Remember, stressing about trigger foods may be just as triggering as enjoying some of your favorite dishes.
- Consider bringing a dish that aligns with your dietary restrictions to ensure there’s something you can comfortably eat.
- Eat prior to going to events to avoid overindulging in foods that may be a trigger for your symptoms.
Rest and Relaxation:
- Schedule breaks for rest and relaxation. Give yourself permission to step away from activities and take time for self-care.
- Incorporate relaxation techniques such as deep breathing or meditation to manage stress.
Create a Comfortable Space:
- If attending gatherings, find a comfortable spot to rest if needed.
- Consider bringing a cushion, heating pad, or any other items that provide comfort during flare-ups.
Be Kind to Yourself:
- Understand that flares may still happen despite your best efforts. Be kind to yourself and acknowledge that it’s okay to take a step back when needed.
Stay Connected:
- Stay connected with supportive friends or online communities. Sharing experiences and tips with others who understand what you’re going through can be comforting.
Use your toolbox!
- For many, you have gathered your individual tools that have worked well for you in the past, don’t forget about these!
- Connect with your providers, if you haven’t seen your providers in a while, it may be helpful to touch base with your mental health therapist, nutritionist, or physical therapist.
- Maybe you opt for that less intense workout to give your body a break.
Remember, everyone’s experience with endometriosis is unique, so tailor these tips to your specific needs and preferences. It’s essential to prioritize your well-being and enjoy the holiday season in a way that works best for you.
For more on this topic, check out our blog Managing Endometriosis: What You Need to Know.
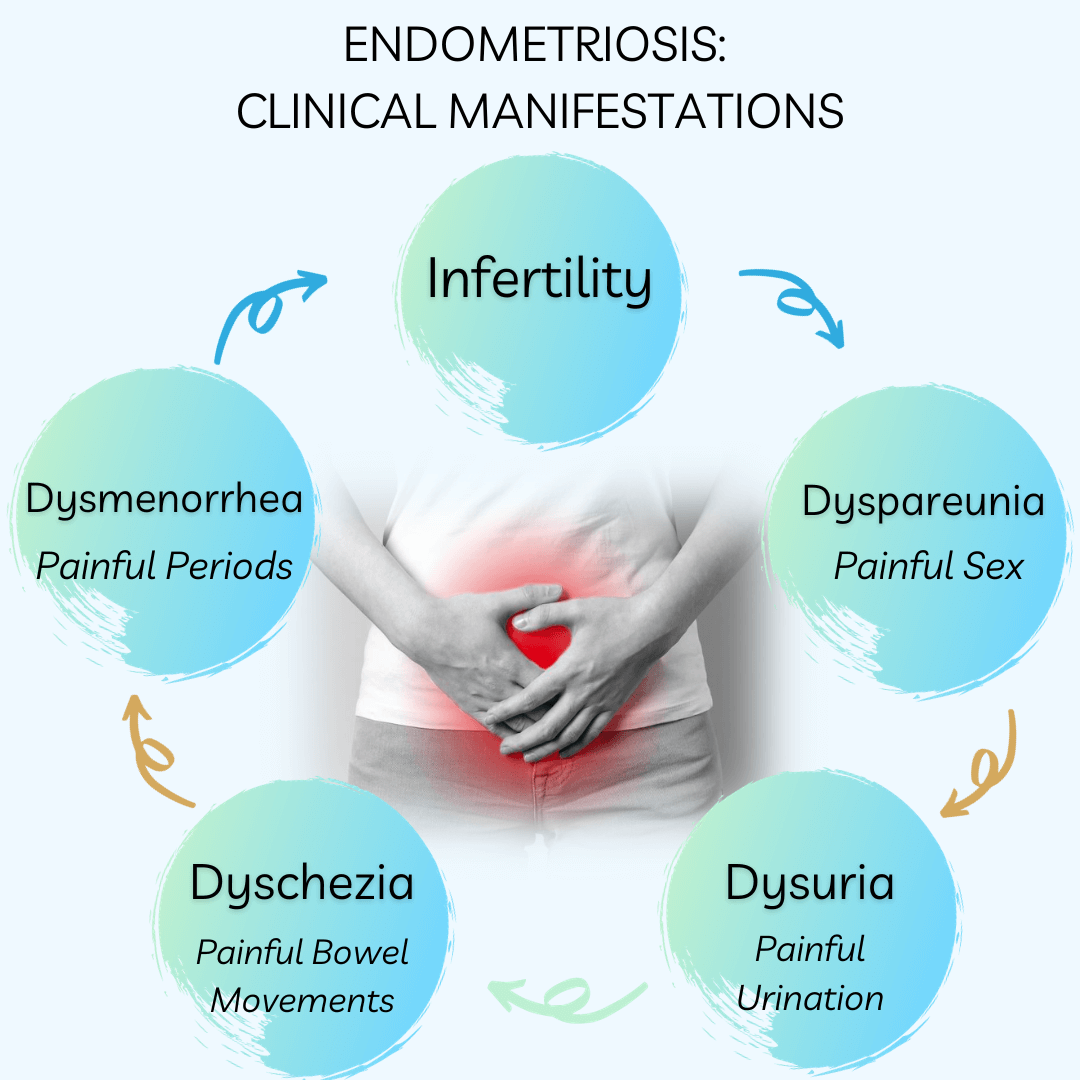
Understanding Endometriosis: Unveiling the Common Symptoms and Their Impact
A recent article from Australia on common symptoms and endometriosis was released recently that followed several thousand women that were both surgically and clinically diagnosed (evaluated separately) with endometriosis and their symptoms to look at associations. There are minimal longitudinal studies available, so this article can be very impactful in raising awareness of the variable, but common, symptoms those with endometriosis experience.
Endometriosis, a chronic gynecologic disorder, is characterized by the presence of endometrium-like tissue outside the uterus. This condition has a profound impact on women’s (XX) lives, often leading to increased hospitalizations, diminished work productivity, and a reduced quality of life. While menstrual symptoms are the most commonly associated with endometriosis, an array of other symptoms can significantly affect the physical and mental wellbeing of women diagnosed with this condition. This article aims to provide an in-depth understanding of the common symptoms associated with endometriosis and their impact on women’s health.
The Prevalence of Endometriosis
Endometriosis is a prevalent health condition affecting approximately 1 in 9 women (11.4%) in Australia by the age of 44 years and in the US the estimation is 1 in 10, though this may be inaccurate due to the significant delay or issues with misdiagnosis. The nonspecific nature and normalization of the symptoms often lead to a significant delay in the diagnosis of endometriosis, with several studies reporting an average delay of 7 to 11 years. This delay in diagnosis results in untreated endometriosis-related symptoms, increased hospitalizations, higher healthcare resource utilization, and potentially reduced success using assisted reproductive technologies. Additionally, some of the overlapping symptoms may be due to the “treatments” offered for symptom management such as hormonal supressive therapies.
Endometriosis and Menstrual Symptoms
Women diagnosed with endometriosis frequently report an array of menstrual symptoms. These may include severe period pain (dysmenorrhea), heavy menstrual bleeding, irregular periods, and premenstrual tension. The association between endometriosis and these symptoms is strong, with the odds ratio for severe period pain being as high as 3.61.
Endometriosis and Mental Health Problems
Apart from physical discomfort, endometriosis can significantly affect a woman’s mental health. Studies reveal a higher incidence of mental health problems, including depression, anxiety, and other mental health disorders, in women with endometriosis. The adjusted odds ratios for depression and anxiety are 1.67 and 1.59, respectively.
Endometriosis and Bowel Symptoms
Bowel symptoms are another common complaint among women with endometriosis. These may include constipation, hemorrhoids or piles, indigestion, or heartburn, bloating, diarrhea, or a combination of these. Additionally, one of the clinical manifestations is dyschezia, or discomfort/pain associated with bowel movements. The adjusted odds ratio for constipation is 1.67, indicating a significant association between endometriosis and bowel symptoms. Additional studies have demonstrated that approximately 90% of those with endometriosis have IBS-like symptoms.
Endometriosis and Urinary Symptoms
Urinary symptoms, such as burning with urination (dysuria) and vaginal discharge or irritation, are also more prevalent in women with endometriosis. The increased odds of urinary symptoms suggest a possible alteration in the pelvic innervation caused by endometriotic lesions.
Endometriosis and Pain Symptoms
Endometriosis is often associated with other forms of pain, including back pain, headaches or migraines, and stiff or painful joints. The adjusted odds ratios for these pain symptoms range from 1.50 to 1.76, further emphasizing the multifaceted impact of endometriosis on women’s health.
Endometriosis and Nonspecific Symptoms
In addition to the symptoms described above, endometriosis is also linked to various nonspecific symptoms. These may include severe tiredness, difficulty sleeping, palpitations, and allergies or hay fever or sinusitis. The association between endometriosis and these symptoms underlines the complex nature of this condition and its wide-ranging effects on women’s health.We need more understanding whether these symptoms are a direct result of the endometriosis, the side effects of treatments, or another related issue.
The Importance of Early Diagnosis
Given the wide array of symptoms associated with endometriosis and their significant impact on a woman’s quality of life, the importance of early diagnosis and treatment cannot be overstated. Early intervention can not only alleviate the physical discomfort associated with the disease but also significantly improve mental health outcomes. Furthermore, it can potentially prevent the development of chronic pain conditions and other long-term health complications.
Conclusion
Endometriosis is a complex condition that affects multiple aspects of a woman’s health. It is associated with a wide range of symptoms, extending beyond menstrual problems to include mental health issues, bowel and urinary symptoms, pain, and other nonspecific symptoms. Understanding these symptoms and their impact on women’s lives is crucial for providing comprehensive care to those diagnosed with this condition. While further research is needed to elucidate the specific mechanisms underlying these associations, the current evidence underscores the importance of early diagnosis and intervention in improving health outcomes for women with endometriosis.
Related reading:
- Understanding fatigue and endometriosis: A Practical No-Nonsense Guide
- Interstitial Cystitis and Endometriosis: Unraveling the “Evil Twins” Syndrome of Chronic Pelvic Pain
- Endometriosis Signs and Symptoms: Everything You Need to Know
References:
- Gete DG, Doust J, Mortlock S, et al. Associations between endometriosis and common symptoms: findings from the Australian Longitudinal Study on Women’s Health. Am J Obstet Gynecol 2023;229:536.e1-20.
Remembering David Redwine: A Modern Hero in Endometriosis Research and Excision Surgery
The recent death of David Redwine has undoubtedly left many with sadness and devastation. Our thoughts are with his friends, family, colleagues, and the endometriosis community as a whole. The world of gynecology has been significantly influenced and transformed by the groundbreaking work of Dr. David Redwine, a significant contributor to those suffering from this disease. A modern hero in this community in his contributions to endometriosis research, excision surgery, and fighting alongside patients and advocating for better answers and better care. His innovative approaches and relentless pursuit of knowledge have positioned him as a leading advocate for patients with endometriosis, a debilitating condition that affects millions of women worldwide.
Who is David Redwine?
A formidable figure in the medical community, Dr. David Redwine has devoted his career to understanding and treating endometriosis. His profound commitment to research and patient care has made him a renowned authority in the field.
Redwine’s Contribution to the Understanding of Endometriosis
Endometriosis is a complex and often misunderstood condition. Dr. Redwine’s research has been instrumental in challenging established theories and introducing new perspectives on the origins and treatment of the disease.
Challenging Sampson’s Theory
One of the most significant contributions of Dr. Redwine has been his challenge to the widely accepted Sampson’s Theory of endometriosis. The theory, proposed by Dr. John Sampson in the 1920s, suggests that endometriosis is caused by retrograde menstruation, where menstrual blood containing endometrial cells flows back through the fallopian tubes and into the pelvic cavity. Redwine questioned the validity of this theory, arguing that if retrograde menstruation were indeed the cause of endometriosis, there should be ample microscopic evidence of refluxed endometrial cells attaching to the pelvic lining and subsequently proliferating. Yet, such evidence is conspicuously lacking. While modern day understanding by experts support alternative theories and are moving toward more plausible explanations, Dr. Redwine is largely to thank for this movement.
Proposing an Embryonic Origin
In place of Sampson’s Theory, Redwine proposed that endometriosis originates from an embryonic source. He argued that endometriosis is derived from mesoderm, the middle layer of the three embryonic layers, and is a result of abnormal differentiation and migration of cells during embryonic formation of the female reproductive tract. This theory suggests that endometriosis is a congenital condition that can manifest later in life under the influence of hormones and other factors.
The Concept of Mulleriosis
To further elucidate the embryonic origin of endometriosis, Redwine introduced the concept of ‘Mulleriosis.’ This term embraces a wider perspective, encompassing all pathologies associated with abnormal development of the Mullerian ducts, the precursor structures to the female reproductive organs.
Redwine’s Innovations in Endometriosis Surgery
Dr. Redwine has not only helped reshape our understanding of endometriosis but also revolutionized its treatment. He is a staunch advocate for excision surgery, a procedure that aims to completely remove endometriosis lesions. While early surgeries also focused on excision surgery, though lacking the precision and advanced technology we have today, the introduction of ablation surgery in the 70’s has complicated research findings, surgical outcomes, and the overall role of surgery in the treatment of this disease resulting in a further push towards hormonal suppression and the fight against Big Pharma.
The Importance of Excision Surgery
Whereas traditional first-line therapies often rely on hormonal therapy or less thorough surgical methods, Redwine emphasizes the importance of excision surgery in effectively treating endometriosis. Through extensive research and practice, he has demonstrated that excision surgery can significantly alleviate symptoms and improve the quality of life for patients with endometriosis.
The Concept of Cure
Contrary to the prevalent belief that endometriosis is incurable, Redwine insists that the disease can be effectively treated through excision surgery. He defines ‘cure’ as the complete absence of the disease, as proven by follow-up laparoscopy. While this topic may be nuanced to a degree and there are cases of regrowth, those of who have undergone a true excision surgery, and those that perform skilled excision surgery understand the difference of persistent pain vs. incomplete technique.
Redwine’s Advocacy for Patients with Endometriosis
In addition to his clinical and research work, Dr. David Redwine is a passionate advocate for patients with endometriosis. He strongly believes in empowering patients with knowledge about their condition and available treatment options.
Redwine is committed to educating both the medical community and the public about endometriosis. He regularly delivers lectures and presentations, sharing his insights and the latest research findings. His dedication to education aims to foster a more informed and empathetic understanding of endometriosis.
As a fervent advocate for patient-centered care, Redwine emphasizes the need to listen to patients’ experiences and concerns. He argues that an effective treatment approach should consider not only the physical manifestations of the disease but also its impact on a patient’s mental and emotional well-being.
You Will Be Missed!
Dr. David Redwine’s pioneering work in endometriosis research, excision surgery, and patient advocacy has had a profound impact on the understanding and treatment of the disease. His unwavering dedication to advancing knowledge and improving patient care serves as an inspiration for both medical professionals and patients alike. Dr. Redwine’s contributions will undoubtedly continue to shape the future of endometriosis care and research, despite his recent passing. His name will always be known in this community for the significant contributions he has made and the patients whom he has helped whether directly, or indirectly.
Rest in peace Dr. Redwine, you will be missed.
Related reading:
- The History of Endometriosis: Unraveling the Theories and Advances [or lack thereof]
- What You Need to Know About Endometriosis Excision Surgery
- Laparoscopy: A Common Treatment for Endometriosis
TENS Therapy: A Non-invasive Pain Relief Option for Dysmenorrhea
Dysmenorrhea and endometriosis are two common health issues that many women face. These conditions often cause severe pelvic pain, disrupting everyday life. Pain relief for these conditions traditionally involves medication whether it be oral contraceptive pills or other hormonal suppressive medications or non-steroidal anti-inflammatory medications, which can sometimes lead to unwanted side effects. In many cases, those with endometriosis need additional support as these are not always effective. While excision surgery should be discussed, even those who have had successful surgeries continue to have persistent pain. Conditions such as dysmenorrhea, adenomyosis, and endometriosis can all contribute to persistent pain. Our blog titled Endometriosis and Adenomyosis: Decoding Their Contribution To Pelvic Pain helps explain these connections.
Modalities do exist that can be helpful for some, with a low side-effect profile. One particular modality of interest has been various Transcutaneous Electrical Nerve Stimulation (TENS) devices, and there have been improvements in these devices especially for those with dysmenorrhea also known as painful periods. One device that we are fond of is the Apollo from My Obi.
What is TENS Therapy?
TENS therapy is a pain management technique that uses low-voltage electrical currents to alleviate pain. It’s a non-invasive treatment that doesn’t involve medication, making it an attractive option for those who experience side effects from traditional pain relief methods.
How Does TENS Therapy Work?
TENS therapy functions by sending electrical currents through the skin to stimulate the nerves. These currents trigger the production of endorphins, the body’s natural painkillers, and block the pain signals from reaching the brain. The intensity and duration of the current can be adjusted to suit individual needs and pain tolerance.
Operation of TENS Devices
TENS devices, such as the Apollo belt and the OVA device, are designed to be user-friendly. They are lightweight and can be clipped onto clothing, allowing users to continue with their daily activities while receiving treatment. The devices come with preset programmes, which the user can select and adjust according to their comfort level.
Benefits of TENS Therapy
TENS therapy offers numerous benefits, especially for women suffering from dysmenorrhea and endometriosis. They are often readily available and affordable, some devices offer a heating option as well!
Non-pharmacological Treatment Option
One of the main advantages of TENS therapy is that it’s a non-pharmacological treatment. It doesn’t involve medication, reducing the risk of side effects or interactions with other drugs.
Increased Blood Flow
TENS therapy can also increase blood flow to the abdomen. This improved circulation helps to reduce inflammation and swelling, further relieving pelvic pain.
User-Controlled
TENS therapy is controlled by the user. This means the intensity and duration of treatment can be adjusted to suit individual needs and pain levels.
Effectiveness of TENS Therapy for Period Pain and Endometriosis
Several studies support the use of TENS therapy for period pain and endometriosis. A review of these studies found TENS therapy to be effective in reducing pain in women with primary and secondary dysmenorrhea. In terms of endometriosis, TENS therapy may offer a viable treatment option, although more research is needed in this area.
Side Effects and Contraindications
TENS therapy is generally safe with few side effects. However, it may not be suitable for everyone. For instance, people with heart conditions or those with a pacemaker should avoid TENS therapy. It’s always best to consult with a healthcare professional before starting any new treatment.
Summary
TENS therapy provides a non-invasive, user-controlled, and effective pain relief solution for dysmenorrhea and endometriosis. It increases blood flow and stimulates the production of endorphins. Moreover, it’s a non-pharmacological treatment, making it an attractive option for those who experience side effects from traditional pain relief methods. However, it’s always best to consult with a healthcare professional before starting any new treatment.
The potential of TENS therapy is promising, and further research could unlock more benefits for women suffering from pelvic pain. By exploring alternative treatments like TENS therapy, we can continue to improve the quality of life for those affected by conditions like dysmenorrhea and endometriosis. If you suffer from pelvic pain or dysmenorrhea you may want to seek help from a specialist, not sure? Read about the signs and symptoms that warrant help here!
References:
Schiotz, H. A., Jettestad, M., & Al-Heeti, D. (2007). Treatment of dysmenorrhoea with a new TENS device (OVA). J Obstet Gynaecol, 27(7), 726-728.
The History of Endometriosis: Unraveling the Theories and Advances [or lack thereof]
Endometriosis is a complex condition that affects a significant number of women (XX) and on average takes 7-10 years for a diagnosis. The majority of people date their symptoms back to adolescence though go years seeking answers. Throughout their journey, many people receive either a wrong diagnosis or were simply dismissed altogether. In recent years, there has been a marked improvement in the recognition of the word ‘endometriosis’ but why does this disease remain such an enigma to so many healthcare professionals? Furthermore, endometriosis has been a subject of medical investigation for over a century with debates about how to approach treatment, understanding of the pathogenesis, clinical manifestations, and treatment methods.
Research in this field has evolved over time, but are we really that much further along than we were a century ago? One of the most frustrating concepts for those of us who truly understand endo, is the regurgitation of the theory of retrograde menstruation postulated in the 1920’s by Dr. John A. Sampson. The theory that endometriosis is derived from retrograde menstruation is an incomplete understanding of this original theory, that has perpetuated misinformation and our current recommended treatments – hormonal suppression and hysterectomies. Sampon’s original theory was more involved, but future research into alternative theories seems much more promising. Even so, our current “validated or trusted treatments” are still rooted in early understanding. This article delves into the intricate history of endometriosis, tracing its theories and advances, or lack thereof, to provide a comprehensive overview of this complex condition.
The Early Recognition of Endometriosis
Initial Observations and Descriptions
The first description of a disease resembling endometriosis can be attributed to Thomas Cullen in the early 20th century.1 Cullen identified endometriosis and adenomyosis as a single disease, characterized by the presence of endometrium-like tissue outside the uterine cavity.2 This breakthrough laid the foundation for future research and understanding of endometriosis.
Sampson’s Theory of Retrograde Menstruation
The term “endometriosis” was coined by John A. Sampson in the late 1920s.3 Sampson proposed the theory of retrograde menstruation as the primary cause of endometriosis, due to the observation during surgery of the similarity in endometriosis lesions and the endometrium, suggesting that endometrial cells are transported to ectopic locations via menstrual flow. This theory gained widespread acceptance and significantly influenced the direction of endometriosis research. Though he did note early on that there were additional factors to allow the growth of these lesions to transform, similar to more current theories and the immune system involvement.
Advances in Diagnosing Endometriosis
The Advent of Laparoscopy
The introduction of laparoscopy in the 1960s revolutionized the diagnosis of endometriosis.4 This minimally invasive surgical procedure allowed physicians to visually identify and classify endometriosis lesions, leading to a significant increase in the diagnosis of the disease.
Differentiating Clinical Presentations
With the advent of laparoscopy, three distinct clinical presentations of endometriosis were identified: peritoneal, deep adenomyotic, and cystic ovarian.5 These classifications, along with advances in imaging techniques such as ultrasound and magnetic resonance imaging (MRI), have improved the precision of endometriosis diagnosis.
Development of Medical Therapies for Endometriosis
Early Interventions
The first attempts at treating endometriosis with synthetic steroids began in the 1940s.6 Initially, androgenic substances were used, but their side effects led to a search for more effective and tolerable treatments. Fun fact: testosterone was actually the first hormone used in attempts to “treat” the disease.
The Pseudo-pregnancy Regimen
The 1950s saw the advent of the “pseudo-pregnancy” regimen, where hormones were used to mimic the hormonal environment of pregnancy, thereby suppressing ovulation and endometrial growth.7 During this time, there were limited options and this suggestions came from the observation that symptoms were improved when pregnancy occurred. This approach utilized a combination of estrogen and progestin medications and marked a significant advance in the medical management of endometriosis. At this time, birth control was becoming more widespread and more options were being developed. The myth that is still perpetuated today by uninformed practitioners and society of “just get pregnant, it will cure your endo” or “just have a baby” stems from this belief. In 1953 a physician legitimized the limited options and made recommendations suggesting that frequent and often pregnancy was one of the only options and “subsidize your children” was the solution for the increased financial burden. There are so many infuriating suggestions at this recommendation, but the 50’s were a different time, with limited research and options.
Gonadotropin-Releasing Hormone (GnRH) Agonists
Gonadotropin-releasing hormone (GnRH) agonists emerged as a primary medical therapy for endometriosis in the late 20th century.8 These drugs work by reducing the production of estrogen, thereby limiting the growth of endometriotic tissue, at least in theory. However, the side effects of hypoestrogenism led to the development of ‘add-back’ therapies to mitigate these effects.Not to mention poor regulation and research practices present in the 1990’s including falsified data on the true impact of these drugs.
Evolution of Surgical Treatments
Conservative Surgery & Advancements in Endoscopic Surgery
The development of laparoscopy also transformed the surgical management of endometriosis. Conservative surgical techniques, including the excision of visible endometriosis lesions and adhesion lysis, became feasible.9 These procedures aimed to preserve fertility while effectively managing the disease. The late 20th century saw further advancements (again, in theory) in laparoscopic surgery for endometriosis. Techniques such as CO2 laser vaporization and the use of circular staplers for bowel resection improved the effectiveness and safety of surgery.10
Unraveling the Pathogenesis of Endometriosis
The Role of the Peritoneal Environment
Research in the 1980s began to focus on the peritoneal environment’s role in endometriosis. Studies found evidence of a local peritoneal inflammatory process, including increased activation of peritoneal macrophages and elevated cytokine and growth factor concentrations.11
Endometrial Dysfunctions
Investigations also revealed biochemical differences between eutopic and ectopic endometrium in women with endometriosis. These differences suggested that endometriosis might be associated with endometrial dysfunction, contributing to both the pathogenesis and sequelae of the disorder.12 While research exists that shows differences in BOTH the endometriosis lesions and the endometrial environment, this is correlational research, and does not imply causation.
Immunological Factors
The involvement of the immune system in the pathogenesis of endometriosis was another significant discovery. Altered immune responses, including decreased T-cell and natural killer cell cytotoxicities, were observed in those with endometriosis.13
The Connection Between Endometriosis and Adenomyosis
In the late 20th century, researchers revisited the connection between endometriosis and adenomyosis, suggesting that the two conditions might represent different phenotypes of the same disorder.14 This theory proposed that both endometriosis and adenomyosis are primarily diseases of the junctional zone myometrium.
Modern Approaches to Endometriosis Treatment
Use of Gonadotropin-Releasing Hormone Agonist and Levonorgestrel-Releasing Intrauterine System
In more recent years, GnRHa therapy, often combined with ‘add-back’ therapy, has become a popular “treatment” for endometriosis.15 The levonorgestrel-releasing intrauterine system (LNG-IUS), which releases a progestin hormone into the uterus, has also shown promise in the management of endometriosis-associated chronic pelvic pain.16 In reality, this may be more true for adenomyosis and further research is needed. Research with less bias seems to oppose these claims stating that “GnRH drugs show marginal improvement over no active treatment” when compared with other hormonal suppression medications. Thanks to marketing, this is not well known among consumers. 19 Not to mention the significant side effects that further contribute to the various chronic overlapping pain syndromes associated with endometriosis.
The Future of Endometriosis Research and Treatment
The evolution of endometriosis theories and advances underscores the complexity of this condition. As we continue to unravel the mysteries of endometriosis, there is an ongoing need for research into its pathogenesis, diagnosis, and treatment. The future of endometriosis research and treatment lies in a deeper exploration of its genetic-epigenetic aspects, the role of oxidative stress, and the impact of the peritoneal and upper genital tract microbiomes.18
Conclusion
The history of endometriosis is marked by a continual evolution of theories, advancements in diagnostic and therapeutic approaches, and an expanding understanding of the disease’s complex pathogenesis. From the initial descriptions by Thomas Cullen to the modern laparoscopic techniques and hormonal therapies, the journey of understanding and treating endometriosis has indeed been a frustrating one.
One of the most frustrating aspects is that when we really understand the first observations of endometriosis in the 1800’s into the early 1900’s, it is not far from where we are today. This demonstrates the serious need for more research, better research, and more in depth understanding of the pathogenesis and treatment approaches for endometriosis. While this has improved in the last five years, it is not enough. We need to do more, and we need to do better. Healthcare policy change is an extremely slow process and in my personal observation, decided among individuals who show less understanding than those with the disease.
10. References
Disclaimer: This article is intended to provide general information on the topic and should not be used as a substitute for professional medical advice. Always consult with your healthcare provider for personal medical advice.
- Cullen, T. (1920). Adenomyoma of the Uterus. WB Saunders.
- Sampson, J.A. (1927). Metastatic or Embolic Endometriosis, due to the Menstrual Dissemination of Endometrial Tissue into the Venous Circulation. American Journal of Pathology, 3(2), 93–110.
- Sampson, J.A. (1927). Peritoneal endometriosis due to menstrual dissemination of endometrial tissue into the peritoneal cavity. American Journal of Obstetrics & Gynecology, 14, 422–469.
- Brosens, I., & Benagiano, G. (2011). Endometriosis, a modern syndrome. Indian Journal of Medical Research, 133(6), 581–593.
- Amro, B., et al. (2022). New Understanding of Diagnosis, Treatment and Prevention of Endometriosis. International Journal of Environmental Research and Public Health, 19(11), 6725.
- Miller, E.J. (1944). The use of testosterone propionate in the treatment of endometriosis. American Journal of Obstetrics & Gynecology, 48(2), 181–184.
- Kistner, R.W. (1958). The use of newer progestins in the treatment of endometriosis. American Journal of Obstetrics & Gynecology, 75(2), 264–278.
- Hughes, E., et al. (2007). Ovulation suppression for endometriosis for women with subfertility. Cochrane Database of Systematic Reviews, (3), CD000155.
- Brosens, I., et al. (2022). New Understanding of Diagnosis, Treatment and Prevention of Endometriosis. International Journal of Environmental Research and Public Health, 19(11), 6725.
- Keckstein, J., & Becker, C.M. (2020). Endometriosis and adenomyosis: Clinical implications and challenges. Best Practice & Research Clinical Obstetrics & Gynaecology, 69, 92–104.
- Dmowski, W.P., & Braun, D.P. (1997). Immunology of endometriosis. Best Practice & Research Clinical Obstetrics & Gynaecology, 11(3), 365–378.
- Lebovic, D.I., et al. (2001). Eutopic endometrium in women with endometriosis: ground zero for the study of implantation defects. Seminars in Reproductive Medicine, 19(2), 105–112.
- Dmowski, W.P., & Braun, D.P. (1997). Immunology of endometriosis. Best Practice & Research Clinical Obstetrics & Gynaecology, 11(3), 365–378.
- Leyendecker, G., et al. (2009). Endometriosis results from the dislocation of basal endometrium. Human Reproduction, 24(9), 2130–2137.
- Surrey, E.S., & Soliman, A.M. (2019). Endometriosis and fertility: A review of the evidence and an approach to management. Journal of the Society of Laparoendoscopic Surgeons, 23(2), e2018.00087.
- Vercellini, P., et al. (2003). Endometriosis and pelvic pain: relation to disease stage and localization. Fertility and Sterility, 79(2), 156–160.
- Sutton, C.J., et al. (1994). Laser laparoscopy in the treatment of endometriosis: a 5 year study. British Journal of Obstetrics and Gynaecology, 101(3), 216–220.
- Brosens, I., & Benagiano, G. (2011). Endometriosis, a modern syndrome. Indian Journal of Medical Research, 133(6), 581–593.
- Johnson, N. P., Hummelshoj, L., & World Endometriosis Society Montpellier, C. (2013). Consensus on current management of endometriosis. Hum Reprod, 28(6), 1552-1568.

Navigating the Path to Your Endometriosis Specialist
The journey towards resolving endometriosis involves an important decision – selecting the right surgeon. Leveraging expert resources like Nancy’s Nook and iCareBetter can be instrumental in this process.
Find an endometriosis specialist
Determining Your Needs in a Surgeon
Being aware of your specific requirements can help you make an informed choice. Here are a few considerations you should keep in mind:
Training and Experience
A surgeon’s training, notably in Minimally Invasive Gynecologic Surgery (MIGS) or Fellowship in Minimally Invasive Gynecologic Surgery (FMIGS) is crucial. Such surgeons have spent more time in operation theaters, honing their skills through extensive practice.
Ensure your surgeon is board-certified and inquire about their experience, including the number of surgeries they’ve performed, complications they’ve encountered, and outcomes.
Surgical Support Team
The surgeon’s team is equally important. Ask about their procedure in case of bowel, bladder, ureter, or diaphragmatic involvement. Inquire if everything can be done during a single procedure.
Approach to Excision
Surgeons may have different opinions on excision versus ablation. Find out their thoughts on the subject and where and when they excise or ablate.
Post-Surgery Care
Ask if the surgeon routinely prescribes suppressive medications pre and post-surgery. Understand their reasons if they do.
Costs
Don’t hesitate to inquire about costs, insurance acceptance, payment policies, and any hidden charges.
Comfort Level
Ensure you feel comfortable conversing with your surgeon and that your queries are answered satisfactorily.
Find an endometriosis specialist
Factors That May Not Influence Your Decision
Certain aspects may not influence the quality of surgical care:
- Gender: The surgeon’s gender does not impact their surgical ability.
- Preferred Tools: The surgical tool used is less important than the surgeon’s skill.
- Bowel Prep: Surgeons may have different preferences for bowel prep before surgery, but it doesn’t seem to influence the outcome.
Factors That Might Influence Your Decision
Some factors might play a role in your decision-making process:
- Reputation: Be cautious while considering a surgeon’s reputation. Some may get media coverage or have excellent bedside manners, but that doesn’t necessarily make them a skilled surgeon.
- Office Management: A well-managed front office can make your experience smoother.
- Location: Depending on your comfort and ability to travel, location might influence your decision.
- Timing: The availability of the surgeon and your urgency might also play a role.
The Most Important Factor
Patients often report being most satisfied with surgeons who actively listen to them. Your surgeon should respect your knowledge and experiences without objection to being recorded or having someone with you during consultations.
Leading Endometriosis Specialists
iCareBetter has a list of endometriosis specialists and surgeons vetted for their surgical skills. Nancy’s Nook on Facebook also provides a list of providers.
Managing Your Relationship with Your Current Doctor
Dealing with a current doctor who might not be capable of handling your endometriosis can be challenging. Here are some tips:
- Think long-term, maintain a cordial relationship, and educate your doctor about your condition without alienating them.
- Be respectful and considerate of your doctor’s opinions.
- Try to keep your doctor on your side by asking for their support.
- Remain calm and collected during discussions.
- If you choose to seek surgery elsewhere and decide not to return to your current physician, send a copy of the operative and pathology reports with a note of gratitude.
- If your doctor dismisses you as a patient, consider it as a sign that it wasn’t a good fit.
- Routine care can be handled by a GP or Family Doctor, a Nurse Practitioner, or a Physician’s Assistant.
Find an endometriosis specialist
Remember, in addition to iCareBetter, which has a peer-reviewed video vetted group of endometriosis surgeons, Nancy’s Nook also provides a list of providers to help you navigate this journey.
Conclusion
Choosing an endometriosis specialist is a significant step on your health journey. Leveraging resources like Nancy’s Nook and iCareBetter can provide valuable insights to guide your decision. Always remember, your comfort and trust in your healthcare provider are paramount.

Acupuncture: An Underexplored Solution for Endometriosis Pain
Endometriosis is a complex, multifaceted health condition that predominantly affects women of reproductive age. Characterized by the growth of endometrial-like tissue outside the uterus, this condition can lead to chronic pelvic pain, dysmenorrhea, and infertility, significantly impacting the quality of life. Today’s treatment is limited to expert surgical excision and hormonal manipulation, with variable success. In recent years, acupuncture has gained attention as a potential complementary treatment for endometriosis-related pain. This ancient Chinese technique may hold promise for providing effective pain relief and enhancing overall well-being.
Understanding Endometriosis
Endometriosis is an estrogen-dependent, inflammatory gynecological disorder that can lead to chronic visceral pelvic pain and infertility. This condition is believed to affect approximately 10% to 15% of women during their reproductive years, causing symptoms such as chronic pelvic pain, deep dyspareunia, dysmenorrhea, dyschezia, dysuria, and more. It is theorized that endometriosis-related changes might be a result of alterations in the peripheral and central nervous systems, predisposing affected individuals to other long-lasting pain conditions.
Despite the availability of hormonal, pharmacological and surgical treatments, many of these interventions fail to sufficiently address the perceived pain. Moreover, they often come with significant side effects, presenting an additional burden of symptoms and potential for harm.
Read more: 20 Signs and Symptoms of Endometriosis.
Read more: What causes endometriosis?
The Science of Acupuncture:
Acupuncture is a traditional Chinese medicine technique that involves inserting thin needles into specific points on the body to balance the flow of energy or “Qi”. It has been used for centuries to treat various conditions, including pain and inflammation. The modern science corollary is that acupuncture may work by stimulating nerves, muscles, and connective tissues, which increases blood flow and activates the body’s natural painkillers. While this modern evidence supports the use of acupuncture it is important to keep in mind that energy medicine is quite poorly understood. Acupuncture is an ancient form of energy medicine. A lot more research is mandated to understand how this truly works and how it might be improved or adjusted on an individual basis.
Acupuncture and Endometriosis:
Pain Relief:
For endometriosis sufferers, the most significant benefit of acupuncture is pain relief. A study by Wayne et al. (2008) revealed that acupuncture significantly reduces pelvic pain, dysmenorrhea, and discomfort associated with endometriosis, enhancing the quality of life. The modern medicine mechanisms underlying this pain relief are thought to be related to the release of endorphins, the body’s natural painkillers, and the reduction of inflammatory markers.
Hormonal Balance:
Endometriosis is often associated with hormonal imbalances, particularly an excess of estrogen. Acupuncture is believed to modulate hormonal levels by impacting the hypothalamus-pituitary-ovarian (HPO) axis, which plays a crucial role in regulating reproductive hormones. A harmonious hormonal balance can help in managing endometriosis symptoms and reducing the progression of endometrial lesions. However, most studies show that acupuncture increases estrogen levels. So, this is a bit contradictory other than to say that other acupuncture-induced mechanisms influencing hormonal balance and homeostasis may be in play.
Improved Blood Flow:
Acupuncture is known to enhance blood circulation to the pelvic area, which can be beneficial for endometriosis patients. Improved blood flow can help reduce inflammation and promote the healing of endometrial lesions. This enhanced circulation can also alleviate the ischemia and hypoxia conditions commonly found in endometriotic tissues, potentially reducing the development of new lesions.
Reduced Stress and Anxiety:
Living with chronic pain and other symptoms of endometriosis can lead to increased stress and anxiety. Acupuncture is reputed to mitigate stress and anxiety by modulating the activity of the amygdala and other brain regions associated with emotion regulation, promoting relaxation and mental well-being.
Empirical Evidence:
Several studies and clinical trials have substantiated the efficacy of acupuncture in managing endometriosis symptoms. A systematic review by Zhu et al. (2011) concluded that acupuncture could be considered an effective and safe alternative for relieving endometriosis-related pain. Another study by Rubi-Klein et al. (2010) demonstrated that acupuncture reduces the severity and duration of pain during menstruation in women with endometriosis.
Integration with Conventional Treatment:
While acupuncture demonstrates the potential to alleviate endometriosis symptoms, it is crucial to view it as a complementary therapy. It is not a standalone treatment option for endo. Integrating acupuncture with conventional medical treatments, such as hormonal therapy, non-narcotic pharmaceuticals, and excisional surgery, can offer a holistic approach to managing endometriosis. This integrative approach can address both the physiological symptoms and the psychological stress associated with the condition, improving the overall quality of life for patients.
Read more: Integrative Therapies for Endometriosis
Limitations and Considerations:
While acupuncture offers promising benefits for endometriosis, limitations exist, including the variability in acupuncture techniques and the lack of standardized treatment protocols. Moreover, the effectiveness of acupuncture may be influenced by individual differences, necessitating personalized treatment plans. It is essential for patients to consult with experts in this field to determine the appropriateness of acupuncture based on their medical history and specific circumstances.
Conclusions:
Acupuncture emerges as a valuable complementary therapy for endometriosis, offering relief from pain, hormonal balance, improved blood flow, and reduced stress and anxiety. Empirical evidence substantiates its efficacy, and integrating it with conventional treatments can provide a comprehensive approach to managing endometriosis. However, individual variability and the lack of standardized protocols necessitate personalized treatment plans and consultation with experts in acupuncture as well as endo specialists. As research continues to unravel the mechanisms underlying acupuncture’s therapeutic effects, it holds the promise of enhancing the quality of life for individuals grappling with endometriosis.
References:
Wayne, P.M., et al. (2008). Acupuncture for pelvic and back pain in pregnancy: a systematic review. American Journal of Obstetrics & Gynecology, 198(3), 254-259.
Zhu, X., et al. (2011). Acupuncture for pain in endometriosis. Cochrane Database of Systematic Reviews, (9), CD007864.
Rubi-Klein, K., et al. (2010). Is acupuncture in addition to conventional medicine effective as pain treatment for endometriosis? A randomised controlled cross-over trial. European Journal of Obstetrics & Gynecology and Reproductive Biology, 153(1), 90-93.
Lund I, Lundeberg T (2016). Is acupuncture effective in the treatment of pain in endometriosis? J Pain Res; 9: 157–165.
Endometriosis and Its Implications on Early Menopause: A Comprehensive Insight
Endometriosis, a chronic inflammatory condition, has been studied for its severe impact on women’s reproductive health in some aspects more than others. One area that has been relatively understudied is the connection between endometriosis and early menopause. This article will delve into the intricate relationship between endometriosis and early menopause, exploring the latest research studies, the associated risk factors, and the potential implications for women’s health.
I. Understanding Endometriosis
Endometriosis is an often painful condition in which tissue similar to the one lining the inside of the uterus — the endometrium — grows outside the uterus, typically on the ovaries, Fallopian tubes, and the tissue lining the pelvis. In some cases, it can spread beyond the pelvic area. Endo mostly affects women during their childbearing years and may also lead to fertility problems.
Read more: What causes endometriosis?
II. The Enigma of Early Menopause
Early menopause, also known as premature menopause or early natural menopause (ENM), is defined as the cessation of menstrual periods before the age of 45. This condition can have a profound impact on a woman’s life, affecting her fertility, cardiovascular health, cognitive function, and overall mortality rate. The main driver is premature ovarian failure (POF) or insufficiency (POI). Without proper levels of estrogen and progesterone, among other hormones, and highly coordinated hormonal fluctuations, menses cease. Menses can also cease due to direct damage to the uterine endometrial lining, but that is far less common. In this latter situation, in contrast to ovarian insufficiency, there are no symptoms of hot flashes or mood swings and the like.
Read more: Endometriosis And Menopause: Everything You Need To Know
III. The Intersection of Endometriosis and Early Menopause
The potential implications of endometriosis on early menopause have not been extensively researched. There is a need for more comprehensive studies to understand the intricate associations and mechanisms linking these two conditions.
IV. Recent Studies on Endometriosis and Early Menopause
Recent investigations have shed light on the possible association between endometriosis and early menopause. These studies suggest that women with endometriosis may be at a higher risk of experiencing early menopause, even after adjusting for various demographic, behavioral, and reproductive factors.
V. Key Findings From the Studies
The studies indicate a statistically significant association between endometriosis and early menopause. Women with endometriosis, particularly those who never used oral contraceptives and are nulliparous, may have a heightened risk of experiencing a shortened reproductive lifespan.
Studies focusing on premature ovarian failure (POF) or insufficiency (POI) suggest that this, in and of itself, is highly heterogeneous and related to mutations in more than 75 genes. Some of these mutations overlap with those associated with endometriosis, particularly in the range of inflammatory autoimmune disorders.
VI. Factors Influencing the Association
Multiple shared clinical factors may influence the association between endometriosis and early menopause, including body mass index (BMI), cigarette smoking, oral contraceptive use, parity, and history of infertility attributed to ovulatory disorder.
Given the genetic overlap of autoimmune and other disorders that influence POI and POF, it is quite probable that this is the root cause of the association between endometriosis and early menopause. However, this remains to be scientifically validated.
In those patients with advanced endo, where ovaries are partially removed or badly, as in the case of large endometriomas, there may be a direct anatomic cause for POI and POF.
VII. Implications of the Findings
The findings of these studies have important implications for women’s health. They suggest that women with endometriosis may need to consider the potential risk of early menopause in their reproductive planning. Additionally, healthcare providers may need to consider these findings when developing individualized treatment plans for women with endometriosis. A full evaluation should include screening for autoimmune disorders and possible genetic analysis for associated conditions.
VIII. Limitations and Future Research
While these findings are significant, they are also limited by certain factors, including the reliance on self-reported data and the lack of racial and ethnic diversity in the study populations. Future research should aim to address these limitations and further explore the clinical and genetic or molecular association between endometriosis and early menopause.
IX. Coping With Endometriosis and Early Menopause
Living with endometriosis and dealing with early menopause can be challenging. However, understanding the connection between these conditions and seeking timely medical advice can help women manage their symptoms and maintain their quality of life. The first step is evaluation and management by providers who have specific and focused expertise in managing endometriosis.
Read more: Navigating HRT for Menopause in Women with Endometriosis
X. Conclusion
The association between endometriosis and early menopause is a significant area of women’s health that mandates further exploration. While recent studies suggest a potential link, more comprehensive research is needed to fully understand the implications of this association. In the meantime, it is crucial for women with endometriosis to be aware of the potential risk of early menopause and to seek expert consultation with endometriosis specialists.
References:
https://pubmed.ncbi.nlm.nih.gov/35061039/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5327623/

Postmenopausal Malignant Transformation of Endometriosis
Endometriosis is a pain and infertility producing condition which predominantly affects premenopausal women. Estimates suggest that up to 10% of women worldwide suffer from the condition during their reproductive years. While the incidence of postmenopausal endometriosis is considerably lower, studies have suggested that this may still be in the neighborhood of 2.5%. So it is a misconception that endo is exclusively a disease of younger women.
Further, although endometriosis is a benign disorder, there lies a risk of malignant transformation, at all ages. This article delves into the potential for malignant transformation of postmenopausal endometriosis.
Understanding Endometriosis and Menopause
Postmenopausal endometriosis refers to the occurrence or continuation of endometriosis symptoms after menopause, which typically occurs around age 50. This is defined as the cessation of menstrual cycles for twelve consecutive months. After this point, the ovaries produce minimal estrogen, a hormone which is generally considered essential for endo growth. So, without this hormone, or lowered levels, most cases of endometriosis naturally diminish. Yet, for some postmenopausal women, endometriosis can persist or even manifest anew.
The cause or causes of endometriosis in younger women are controversial and incompletely defined. Through uncertain but likely multifactorial mechanisms, endometriosis is characterized by the presence and growth of ectopic endometrial-like tissue outside the uterus. While one might assume that a hypoestrogenic state associated with menopause would alleviate endometriosis, this isn’t always the case.
In postmenopausal women, the causes of endometriosis are less clear. Some contributing factors include:
- Residual Disease: Endometriosis that began before menopause may continue after menopause due to residual disease and growth stimulated by factors other than estrogen or high sensitivity to low estrogen levels.
- Exogenous Estrogen: Hormone replacement therapy (HRT) can potentially stimulate the growth of endometrial cells. This may be particularly relevant for postmenopausal women who take estrogen-only HRT, which can reactivate endometrial implants or even initiate new growths.
- Endogenous Estrogen Conversion: Adipose (fat) tissue can produce estrogen by converting it from other hormones. Postmenopausal women with higher amounts of adipose tissue might produce enough estrogen to promote the growth of endo. Fat can also store xeno-estrogens from certain toxins and then slowly release them into circulation. The tissue microenvironment around endometriosis lesions also contributes to local estrogen production.
Read more: Endometriosis And Menopause: Everything You Need To Know
Malignant Transformation: A Rare but Possible Event
While endometriosis is overwhelmingly benign, studies have indicated that women with endometriosis have an increased risk of developing certain types of ovarian cancers, specifically clear cell and endometrioid carcinomas.
Some factors that might increase the risk include:
- Duration of Endometriosis: Prolonged presence of endometriosis lesions might increase the risk of malignant transformation. In general, cancer risk increases with age and it is well known that chronic inflammation contributes to formation of cancer. Endo is inflammatory in nature. Thus, if endo is still growing after menopause this means more time in an inflammatory state, hypothetically contributing to the risk.
- HRT Use: As mentioned, exogenous estrogen can stimulate endometriosis growth, potentially increasing the risk of malignant changes in existing lesions. This is not proven but may be a contributory factor which is very complicated due to individual variations in receptor activity and levels of estrogen.
- Genetic Factors: Some genetic mutations might predispose women to both deeply invasive endometriosis and ovarian cancer, and there is overlap. Epigenetic factors regulate which genes turn on an off during life and are influenced by environmental factors. There is also a potential cumulative effect in the number of active mutated genes over the years. Some of the key genetic factors include:
- PTEN: PTEN is a tumor suppressor gene. Its mutations have been identified in both endometriosis and endometrioid and clear cell ovarian cancers. Loss of PTEN function can lead to uncontrolled cell growth and might play a role in the malignant transformation of endometriosis.
- ARID1A: ARID1A mutations are frequently seen in endometriosis-associated ovarian cancers. This gene is involved in chromatin remodeling, and its mutation can lead to disruptions in DNA repair and subsequent malignant transformation.
- KRAS and BRAF: Mutations in these genes are known to play roles in the pathogenesis of various cancers. They’ve been identified in benign endometriotic lesions and might contribute to the early stages of malignant transformation.
- Inherited Genetic Mutations: Women with inherited mutations in BRCA1 and BRCA2 genes, known for their association with breast and ovarian cancers, might also have an increased risk of developing endometriosis and its subsequent malignant transformation.
Read more: Understanding the Connection between Endometriosis and Cancer
Conclusions
Postmenopausal endometriosis, although less common than its premenopausal counterpart, cannot be overlooked. The absolute risk of malignant transformation, albeit very low, emphasizes the importance of regular monitoring and endo specialist consultations for postmenopausal women with endometriosis or its symptoms. When postmenopausal endometriosis is suspected or diagnosed, especially if it is invasive and there are unusual symptoms or pelvic masses, a consultation with a gynecologic oncologist is also prudent.
References
Bulun SE. Endometriosis. N Engl J Med. 2009;360(3):268-279.
Pearce CL, Templeman C, Rossing MA, et al. Association between endometriosis and risk of histological subtypes of ovarian cancer: a pooled analysis of case-control studies. Lancet Oncol. 2012;13(4):385-394.
Luca Giannella, Chiara Marconi, Jacopo Di Giuseppe, et al. Malignant Transformation of Postmenopausal Endometriosis: A Systematic Review of the Literature. Cancers (Basel) 2021 Aug 10;13(16):4026.
Luca Giannella, Chiara Marconi, Jacopo Di Giuseppe, et al. The association between endometriosis and gynecological cancers and breast cancer: a review of epidemiological data. Gynecol Oncol. 2011;123(1):157-163.
Sato N, Tsunoda H, Nishida M, et al. Loss of heterozygosity on 10q23.3 and mutation of the tumor suppressor gene PTEN in benign endometrial cyst of the ovary: possible sequence progression from benign endometrial cyst to endometrioid carcinoma and clear cell carcinoma of the ovary. Cancer Res. 2000;60(24):7052-7056.
Wiegand KC, Shah SP, Al-Agha OM, et al. ARID1A mutations in endometriosis-associated ovarian carcinomas. N Engl J Med. 2010;363(16):1532-1543.
Dinulescu DM, Ince TA, Quade BJ, Shafer SA, Crowley D, Jacks T. Role of K-ras and Pten in the development of mouse models of endometriosis and endometrioid ovarian cancer. Nat Med. 2005;11(1):63-70.
Saha R, Pettersson H, Svedberg P, et al. Endometriosis and the risk of ovarian and endometrial adenocarcinomas: a meta-analysis. BMJ Open. 2020;10(4):e034760.

Can Endometriosis Become Malignant After Menopause?
Endometriosis, a condition commonly affecting women of reproductive age, doesn’t just vanish in menopause. In fact, an estimated 2-4% of postmenopausal women suffer from symptomatic endometriosis. Although endometriosis is generally benign, there lies a risk of malignant transformation. This article delves into the malignant transformation of postmenopausal endometriosis, presenting a comprehensive analysis of the topic.
Understanding Endometriosis and Menopause
Endometriosis is a complex clinical syndrome characterized by the presence of ectopic endometrial-like tissue. This pathological condition primarily affects women of reproductive age, often causing infertility and chronic pelvic pain leading to severe functional limitations.
While one might assume that the cessation of menstruation and the hypoestrogenic state associated with menopause would alleviate endometriosis, this isn’t always the case. Postmenopausal endometriosis can affect up to 4% of women. Recurrences or malignant transformations, although rare, are possible events.
Read more: Endometriosis And Menopause: Everything You Need To Know
Malignant Transformation: A Rare but Possible Event
While endometriosis is a benign condition, it carries a risk of malignant transformation. Approximately 1% of ovarian endometriosis can turn into cancer. However, a prospective study found a standardized incidence ratio of malignant transformation of 8.95, indicating that malignant transformation, while rare, is a serious concern.
In the case of postmenopausal endometriosis, malignant transformation is even rarer. There are no definitive percentages about its prevalence, with data derived from studies, including case reports and case series. This scarcity of data highlights the need for further research into this topic.
Read more: Understanding the Connection between Endometriosis and Cancer
Recurring Clinical Conditions
In the malignant transformation of postmenopausal endometriosis, some clinical conditions tend to recur:
- History of endometriosis
- Definitive gynecological surgery before menopause
- Estrogen-only hormone replacement therapy (HRT) for a relatively long time
These conditions, however, have shown a significant decrease in recent years. This decrease could be due to changes in the attitudes and management of gynecologists, influenced by up-to-date scientific evidence about the use of major surgery in gynecological pathologies.
The Role of Hormone Replacement Therapy (HRT)
HRT plays a significant role in postmenopausal endometriosis. Among the women who used HRT, estrogen-only therapy was taken by approximately 75% of women. The duration of treatment had a median of 11 years, with the course of treatment exceeding five years in most women.
Current recommendations on HRT include continuous combination formulations or Tibolone for women with previous endometriosis. However, these recommendations are based on limited data, emphasizing the need for more extensive studies on this topic.
Read more: Navigating HRT for Menopause in Women with Endometriosis
Cancer Lesion Characteristics and Treatment
The malignant transformation of endometriosis can present with varying characteristics and may require different treatment approaches. Approximately 70% of cases had histology of endometrioid adenocarcinoma or clear cell carcinoma. The most frequent localization of the lesions was at the level of the pelvis, ovary, and vagina.
Most women underwent surgical treatment, with procedures including excision of the mass, hysterectomy with bilateral salpingo-oophorectomy, and surgical debulking. Adjuvant medical treatment was performed in about 60% of cases.
Read more: How to tell the difference between endometriosis and ovarian cancer.
Patient Outcomes and Follow-up
The outcomes for patients with malignant transformation of postmenopausal endometriosis are generally favorable. The survival rate is approximately 80% in 12 months, with a recurrence rate of 9.8% and a death rate of 11.5%.
The duration of follow-up had a median of 12 months. However, follow-up data is still too incomplete to provide adequate information on the prognosis, highlighting the need for further research in this area.
Conclusions
The malignant transformation of postmenopausal endometriosis presents a clinical challenge that requires further exploration. As gynecologists’ attitudes and management strategies evolve, it’s crucial to continue research into this area, to provide accurate and individualized evaluation and information for patients.
While endometriosis is generally a benign condition, the risk of malignant transformation, particularly in postmenopausal women, should not be overlooked. Comprehensive understanding and timely management of this condition are crucial to improving patient outcomes.
Reference:
https://pubmed.ncbi.nlm.nih.gov/34439184/

The Hidden Connection Between Endometriosis and Systemic Lupus Erythematosus
Based on possible shared characteristics and pathogenesis the interconnectedness of various ailments becomes a focal point of research. Such is the relationship between endometriosis and lupus, two seemingly unrelated conditions that share intriguing parallels. This article aims to shed light on the increased risk of being diagnosed with endometriosis in patients suffering from Systemic Lupus Erythematosus or SLE. The purpose of unraveling connections is that this may lead to treatment discoveries.
Understanding Endometriosis
Endometriosis is a multifaceted disease that primarily affects women in their reproductive years. It is characterized by the abnormal growth of endometrial-like tissue outside the uterus, leading to chronic pelvic pain, and potential infertility.
The pathophysiology of endometriosis involves a systemic inflammatory response, influenced by female sex hormones that may subtly affect the maintenance of immunity or the development of autoimmune diseases.
Getting to Know Systemic Lupus Erythematosus (SLE)
SLE is a chronic, autoimmune disease that can affect various parts of the body, including the skin, joints, kidneys, heart, and lungs. It involves the immune system attacking the body’s own tissues, leading to inflammation and damage. Women, especially of childbearing age, are more frequently diagnosed with SLE than men. Other factors such as ethnicity, age of onset, and socioeconomic class significantly influence SLE incidence, with notable geographic differences observed.
Endometriosis and SLE: The Intriguing Association
Epidemiological studies suggest a solid link between endometriosis and female-dominant autoimmune diseases. However, not all studies support a significant association between endometriosis and SLE. The potential for spurious associations due to small study sizes and suboptimal control selection is high.
Unraveling the Connection: A Comprehensive Study
Given these inconsistencies, and accepting that the findings may not be applicable to all geo-ethnic populations, a large nationwide retrospective cohort study was conducted to assess the risk of endometriosis in women diagnosed with SLE. The study analyzed data from the Taiwan Longitudinal Health Insurance Research Database 2000 (n = 958,349) over a 13-year follow-up period (2000–2013).
Study Design and Population
The study adopted a retrospective cohort design with primary data sourced from the Taiwan National Health Insurance Research Database (NHIRD). The study cohort included women diagnosed with SLE between 1997 and 2013, and the index date was defined as the first diagnosis of SLE.
Assessed Outcome
The primary outcome was defined as the diagnosis of endometriosis. Given the lack of non-invasive diagnostic tools for endometriosis, the disease’s diagnosis was derived from clinical evidence or surgical intervention. Every effort was made to optimize parameters of non-surgical diagnosis of endo but surgical validation was lacking in a large number of subjects, representing a significant study weakness.
Results and Implications
The study, within stated limitations, found a statistically significant association between SLE and endometriosis, after controlling for age.
Read more: Unraveling the Connection Between Endometriosis and Autoimmune Diseases.
Conclusion: A Call for Further Research
The risk of endometriosis was found to be significantly higher in SLE patients compared to the general population in this study. This adds substantially to the overall body of evidence supporting an association. However, more research is needed to fully understand this association and to determine if it can be generalized across different geo-ethnic populations. Clearly, more basic science research is also critically needed to support epidemiologic associations.
Reference:
https://pubmed.ncbi.nlm.nih.gov/35922461/

Can endometriosis cause miscarriage? Understanding Endometriosis and Its Impact on Miscarriage
Endometriosis is a prevalent health condition, affecting approximately 10% of women worldwide. It is often associated with chronic pain and infertility, but its potential connection to miscarriage is not as widely recognized. This article aims to shed light on the link between endometriosis and miscarriage, drawing on recent scientific research and expert insights.
What is Endometriosis?
Endometriosis is a chronic condition where tissue similar to the lining of the uterus, known as endometrium, grows outside the uterus. This tissue can grow on the ovaries, fallopian tubes, or the lining of the pelvic cavity. Just as the inner lining of the uterus thickens, breaks down, and bleeds with each menstrual cycle, so too does the endometrial-like tissue outside the uterus. However, this displaced tissue has no way to exit the body, leading to various problems.
Read More: What causes endometriosis?
Pathogenesis of Endometriosis
Endometriosis develops in stages, with severity ranging from minimal to severe. The American Society for Reproductive Medicine groups endometriosis into four stages: minimal (Stage I), mild (Stage II), moderate (Stage III), and severe (Stage IV). The stages reflect the extent, location, and depth of endometrial-like tissue growth, as well as the presence and severity of adhesions and the presence and size of ovarian endometriomas.
Symptoms of Endometriosis
While some women with endometriosis may have no symptoms, others may experience:
- Painful periods
- Pain during intercourse
- Pain with bowel movements or urination
- Excessive bleeding
- Infertility
- Other signs and symptoms such as fatigue, diarrhea, constipation, bloating, or nausea
Read more: 20 Signs and Symptoms of Endometriosis
Endometriosis and Pregnancy Complications
Endometriosis has long been associated with infertility, with studies indicating that up to 50% of women with infertility have the condition. However, less is known about its impact on women who do conceive. Emerging research suggests that endometriosis may increase the risk of several pregnancy complications, including preterm birth, cesarean delivery, and miscarriage.
Read More: How Does Endometriosis Cause Infertility?
Endometriosis and Miscarriage: Understanding the Connection
Recent research has begun to explore the potential link between endometriosis and miscarriage. Miscarriage, also known as spontaneous abortion, is defined as the loss of a pregnancy before 20 weeks of gestation. It is estimated that about 10-20% of known pregnancies end in miscarriage. The actual number is likely higher, as many miscarriages happen so early in pregnancy that a woman might not even know she’s pregnant.
The Role of Inflammation
One theory proposes that the inflammation associated with endometriosis could interfere with the early stages of pregnancy. Endometriosis is characterized by chronic pelvic inflammation, which could potentially disrupt the implantation of the embryo or the development of the placenta.
The Impact of Surgical Treatment
Another factor to consider is the potential impact of surgical treatment for endometriosis. There have only been a few clinical trials and they do not indicate that surgical excision reduces the risk of miscarriage. However, there are two very large databases from Sweden and Scotland that suggest a benefit to removing known endometriosis to lower pregnancy loss risk. More research is required.
Hormonal Factors
Endometriosis can alter the hormonal environment of the uterus, which could potentially impact early pregnancy. More research is needed to fully understand how these hormonal changes might contribute to miscarriage risk.
Research Insights: Endometriosis and Miscarriage Risk
Several studies have investigated the link between endometriosis and miscarriage. A meta-analysis published in 2020 in the journal BioMed Research International found that women with endometriosis had a significantly higher risk of miscarriage compared to women without the condition. This risk was particularly pronounced in women who conceived naturally, rather than those with tubal infertility who conceived through assisted reproductive technology (ART).
Coping with Endometriosis and Miscarriage
The potential link between endometriosis and miscarriage can come as distressing news. However, it’s important to remember that many women with endometriosis have successful pregnancies. So, counseling and intervention really depend on the individual situation. With repeat losses, there are many potential reasons but it appears that endo can be one of them.
Read more: Find an Endometriosis Specialist for Diagnosis, Treatment, & Surgery.
Conclusion
Endometriosis is a complex condition that can impact various aspects of a woman’s health, including her fertility and pregnancy outcomes. While research suggests a potential link between endometriosis and miscarriage, many women with the condition have successful pregnancies. If you have endometriosis or suspect you have endo, and having difficulty conceiving or experiencing pregnancy losses, it’s crucial to seek consultation with an endometriosis specialist.
Reference:
https://pubmed.ncbi.nlm.nih.gov/33490243/

Genetics and Epigenetics of Endometriosis: Unraveling the Complex Web of Hereditary Implications
Endometriosis, a medical condition afflicting numerous women worldwide, continues to puzzle medical researchers due to its complex nature and the myriad of genetic and environmental factors contributing to its development. This article aims to dissect the convoluted genetic aspect of endometriosis, providing a comprehensive understanding of its hereditary implications.
1. Introduction to Endometriosis
Endometriosis is a condition characterized by the growth of endometrium-like tissue outside the uterus. This disease exhibits significant diversity in its manifestation, with the tissue appearing in various forms and locations. It has a significant impact on the quality of life of the affected individual, often causing pain, infertility, and other related complications.
2. The Genetic Puzzle of Endometriosis
2.1 Hereditary Factors in Endometriosis
Endometriosis has been confirmed as a hereditary disease, with the risk of developing the condition significantly higher in first-degree relatives of affected women. Twin studies further corroborate this, showing a similar prevalence and age of onset in twins. Despite this, the exact genetic mechanisms contributing to endometriosis remain elusive and likely presents with an inheritance pattern that is multifactorial.
2.2 Genetic and Epigenetic Incidents in Endometriosis
Genetic and epigenetic incidents, both inherited and acquired, significantly contribute to the development of endometriosis. These incidents, which can cause changes in gene expression, are often triggered by environmental factors such as oxidative stress and inflammation. Familial clustering of endometriosis has been shown in an array of studies with similar findings. First-degree relatives are 5 to 7 times more likely to have surgically confirmed disease.
Familial endometriosis may be more severe than sporadic cases. This also supports the multifactorial inheritance of endometriosis and a genetic propensity as it may spread more severely to offspring or siblings. These women with familial inheritance may also have earlier age of onset and symptoms.
3. Theories on the Pathogenesis of Endometriosis
3.1 The Implantation Theory
The implantation theory, popularized by Sampson in 1927, suggests that endometriosis is caused by the implantation of endometrial cells in locations outside the uterus. This theory, while reasonable, fails to explain certain observations, such as the occurrence of endometriosis in men and women without endometrium.
3.2 The Metaplasia Theory
The metaplasia theory postulates that endometriosis is a result of metaplastic changes, a process where one type of cell changes into another type due to environmental stress. This theory, while accounting for some observations, is limited by the varying definitions of “metaplasia” and the disregard for genetic or epigenetic changes.
3.3 The Genetic/Epigenetic Theory
The genetic/epigenetic theory proposes that endometriosis results from a series of genetic and epigenetic incidents, both hereditary and acquired. This theory is compatible with all known observations of endometriosis, providing a comprehensive understanding of the disease’s pathogenesis.
4. The Genetic/Epigenetic Theory: A Closer Look
4.1 Genetic and Epigenetic Incidents: The Triggers of Endometriosis
According to the genetic/epigenetic theory, endometriosis is triggered by a series of genetic and epigenetic incidents. These incidents can be hereditary, transmitted at birth, or acquired later in life due to environmental factors such as oxidative stress and inflammation.
4.2 The Role of Redundancy in the Development of Endometriosis
Redundancy, where a task can be accomplished by multiple pathways, plays a significant role in the development of endometriosis. This redundancy can mask the effects of minor genetic and epigenetic changes, causing them to become visible only when a higher capacity is needed.
4.3 The Genetic/Epigenetic Theory and Endometriosis Lesions
Endometriosis lesions are clonal, meaning they originate from a single cell that has undergone genetic or epigenetic changes. The genetic/epigenetic theory proposes that these lesions can remain dormant for extended periods, similar to uterine myomas, and may only be reactivated by certain triggers such as trauma.
5. Clinical Implications of the Genetic/Epigenetic Theory
5.1 Understanding the Nature of Endometriosis Lesions
According to the genetic/epigenetic theory, most subtle or microscopic lesions are normal endometrium-like cells that would likely resolve without intervention. In contrast, typical, cystic, and deep lesions are benign tumors that do not recur after complete excision but may progress slowly or remain dormant for an extended period.
5.2 The Role of Hereditary Factors in Endometriosis
The genetic/epigenetic theory suggests that genetic and epigenetic defects inherited at birth may play a significant role in the development of endometriosis. These hereditary factors may not only contribute to the disease’s onset but also to associated conditions such as subfertility and pregnancy complications.
5.3 Variability in Endometriosis Lesions
The genetic/epigenetic theory explains that endometriosis lesions can vary significantly in their reaction to hormones and other environmental factors. This variability is due to the specific set of genetic and epigenetic changes present in each lesion.
6. Prevention and Treatment of Endometriosis: A Genetic/Epigenetic Perspective
6.1 Prevention of Genetic/Epigenetic Incidents
Preventing the genetic/epigenetic incidents that trigger endometriosis can be a complex task. However, reducing repetitive stress may be useful in this regard.
6.2 Treatment of Endometriosis
The genetic/epigenetic theory suggests that the treatment of endometriosis should focus on the complete excision of the lesions to prevent recurrence. However, it also proposes that less radical surgery may be sufficient in some cases where the surrounding fibrosis and outer cell layers are composed of normal cells with reversible changes.
7. Conclusion
While the genetic/epigenetic theory provides a comprehensive understanding of the pathogenesis of endometriosis, it remains a theory until disproven by new observations. Further research is needed to fully elucidate the genetic and epigenetic mechanisms contributing to endometriosis, paving the way for more effective prevention and treatment strategies. Despite the complexity and challenges, the pursuit of knowledge in this field continues, offering hope for a future where endometriosis can be effectively managed and potentially prevented.
Reference:
- Koninckx PR, Ussia A, Adamyan L, Wattiez A, Gomel V, Martin DC. Pathogenesis of endometriosis: the genetic/epigenetic theory. Fertil Steril. 2019 Feb;111(2):327-340. [PubMed]
- Simpson J, Elias S, Malinak L, et al. Heritable aspects of endometriosis: 1. Genetic studies. Am J Obstet Gynecol. 1980;137:327–331. [PubMed] [Google Scholar]
- Kennedy S, Hadfield R, Mardon H, Barlow D. Age of onset of pain symptoms in non-twin sisters concordant for endometriosis. Hum Reprod. 1996;11:403–405. [PubMed] [Google Scholar]
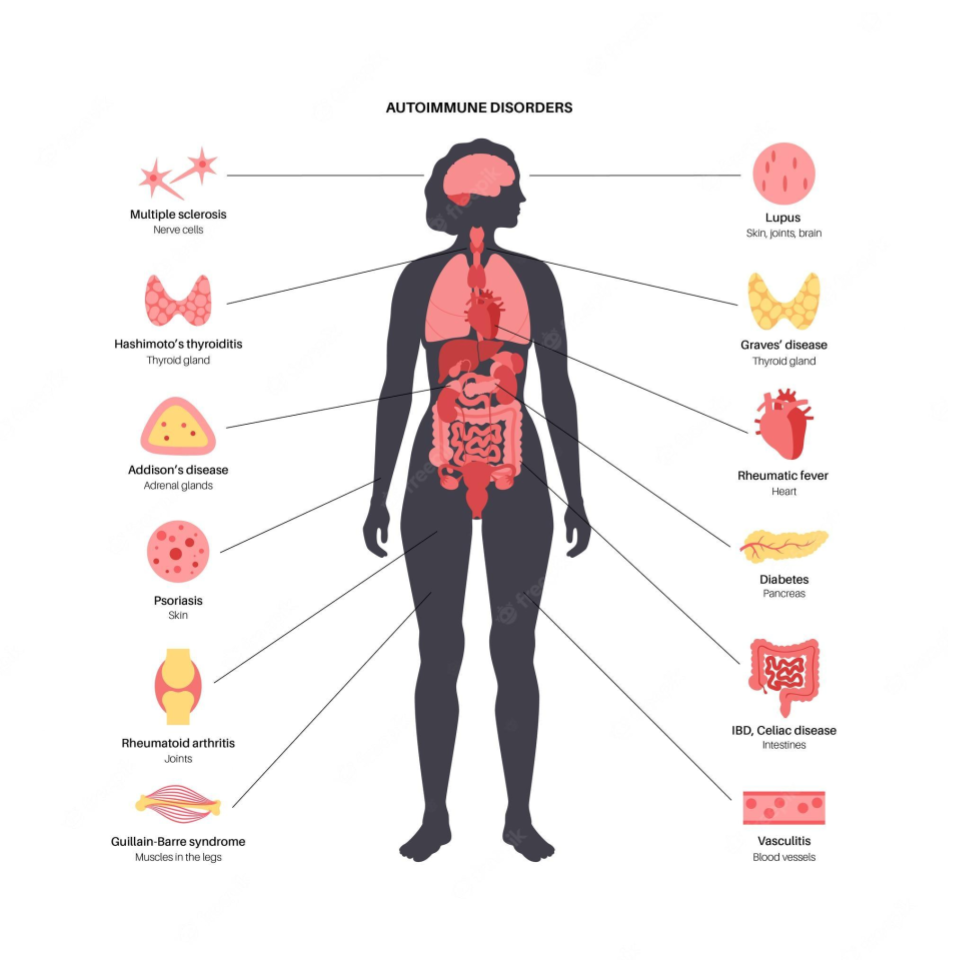
Unraveling the Connection Between Endometriosis and Autoimmune Diseases
Endometriosis causes pain, multiple bowel symptoms and infertility, among many other debilitating symptoms, in about 10% of women, mostly in the reproductive age range. Developing research has shown that there is a link to various autoimmune conditions.
Understanding Endometriosis
Endometriosis is a chronic gynecological disorder characterized by the presence of endometrial-like tissue growing outside the uterus. This means the cells look like those which line the inner part of the uterus but differ markedly in multiple ways at the molecular level. The more we find out the less it is clear what the origins are. However, they are likely partly genetic and partly based on other multiple influences of the environment on your body and genes.
Read more: What causes endometriosis?
The Immune System’s Role
Research suggests that abnormalities in the immune system may play a key role in the development of endometriosis. These abnormalities could prevent the immune system from effectively clearing ectopic endometrial cells, regardless of how they get there, allowing them to implant and grow outside the uterus. This hypothesis suggests that endometriosis might be, at least in part, an immunity-associated disorder.
Furthermore, endometriosis is often associated with a chronic inflammatory response, triggered by the presence of ectopic endometrial-like cells. This inflammation, coupled with the immune system’s inability to effectively remove ectopic cells, could partly explain the chronic pain often associated with endometriosis.
The Link to Autoimmune Diseases
Autoimmune diseases occur when the immune system mistakenly attacks the body’s own cells, viewing them as foreign invaders. The link between endometriosis and autoimmune diseases is still being explored, but multiple studies suggest that women with endometriosis may have a higher risk for certain autoimmune diseases. It is not clear if endo carries a risk of developing autoimmune diseases or if the reverse is true or if they simply share common molecular mechanisms which results in both potentially occurring in any given individual. At this point it is important to stress that an “association” does not mean “cause”.
This review aims to delve into the current state of research on the association between endometriosis and autoimmune diseases. It presents key findings from population-based studies, discusses the potential implications, and highlights areas for future research.
Systemic Lupus Erythematosus (SLE) and Endometriosis
Systemic Lupus Erythematosus (SLE) is an autoimmune disease characterized by inflammation and damage to various body tissues, including the skin, joints, kidneys, and heart. Some studies have suggested a positive association between endometriosis and SLE.
One study suggested a seven-fold increase in the odds of having SLE among women with endometriosis. However, the study relied on self-reported diagnoses, which may introduce bias. A more recent cohort study found a more modest but still significant elevation in SLE risk among women with endometriosis.
Read more: The Hidden Connection Between Endometriosis and Systemic Lupus Erythematosus
Sjögren’s Syndrome (SS) and Endometriosis
Sjögren’s Syndrome (SS) is an autoimmune disorder characterized by dry eyes and mouth, often accompanied by other systemic symptoms. Several studies have investigated the potential link between SS and endometriosis.
A meta-analysis of three case-control studies found a 76% higher odds of SS in women with endometriosis. However, these studies had small sample sizes and wide confidence intervals, indicating a need for further research. Confidence intervals describe the range of results around a measurement which indicate how accurate the conclusion might be. The tighter it is among measurements the better.
Rheumatoid Arthritis (RA) and Endometriosis
Rheumatoid Arthritis (RA) is a chronic inflammatory disorder affecting many joints, including those in the hands and feet. Some studies have suggested a link between endometriosis and an increased risk of developing RA.
One meta-analysis, for example, found a 50% increased risk of RA among women with endometriosis. Again, the studies included in the analysis had limitations, including small sample sizes and wide confidence intervals.
Autoimmune Thyroid Disorders (ATD) and Endometriosis
Autoimmune thyroid disorders (ATDs), including Graves’ disease and Hashimoto’s thyroiditis, occur when the immune system attacks the thyroid gland, leading to either overactivity (hyperthyroidism) or underactivity (hypothyroidism) of the gland.
A meta-analysis of three case-control studies suggested a non-significant increase in the odds of ATD in women with endometriosis. However, the studies had high heterogeneity and low-quality scores, suggesting that further research is needed.
Coeliac Disease (CLD) and Endometriosis
Coeliac disease (CLD) is an autoimmune disorder where ingestion of gluten leads to damage in the small intestine. Some studies have suggested a possible link between endometriosis and CLD.
A meta-analysis of two case-control studies found a four-fold increase in the odds of CLD among women with endometriosis. Again, these studies had small sample sizes and wide confidence intervals, indicating a need for further research.
Multiple Sclerosis (MS) and Endometriosis
Multiple Sclerosis (MS) is a chronic disease that attacks the central nervous system. Current research on the association between MS and endometriosis is limited and inconclusive, with some studies suggesting a possible link while others finding no significant association.
Inflammatory Bowel Disease (IBD) and Endometriosis
Inflammatory bowel disease (IBD), including Crohn’s disease and ulcerative colitis, is characterized by chronic inflammation of the gastrointestinal tract. Some studies indicate a possible association between IBD and endometriosis.
One study found a 50% increase in the risk of IBD among women with endometriosis. However, the study had a small sample size and the confidence interval was wide, indicating a need for further research.
Read more: Is Endometriosis Genetic? Understanding the Genetic Links in Endometriosis.
The Bigger Picture
While the evidence for an association between endometriosis and certain autoimmune diseases is compelling, it’s important to emphasize that correlation or association does not imply causation. Further research is needed to determine whether endometriosis actually increases the risk of developing autoimmune diseases or vice versa, or whether the two share common risk factors or underlying mechanisms.
The potential link between endometriosis and autoimmune diseases highlights the importance of a comprehensive approach to women’s health. For women with endometriosis, being aware of the potential increased risk of autoimmune diseases can inform their healthcare decisions and monitoring.
The Path Ahead
The intersection of endometriosis and autoimmune diseases is a complex and evolving field of research. Better understanding the relationship between these conditions could help improve diagnosis, treatment, and ultimately, the quality of life for patients with endometriosis.
By continuing to explore this connection, we are gaining new insights into the pathophysiology of endometriosis and autoimmune diseases, potentially leading to novel treatments and preventive strategies.
Reference:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6601386/

Navigating HRT for Menopause in Women with Endometriosis
Endometriosis, a chronic condition, is often associated with the fertile years of a woman’s life. But what happens when these women reach menopause? Can the symptoms of endometriosis persist, or even worsen, during this transition? This article aims to shed light on these questions and provide guidance for women with a history of endometriosis approaching menopause.
Understanding HRT and Endometriosis: A Quick Overview
Endometriosis is a medical condition characterized by the growth of endometrial-like tissue (the tissue that lines the uterus) outside the uterus. This condition, affecting approximately at least 10% of women in their reproductive years, can lead to debilitating pain, infertility, and other complications. However, the diagnosis of endometriosis often gets delayed due to the non-specific nature of its symptoms and the lack of reliable diagnostic tools.
The exact cause of endometriosis remains unclear, but estrogen dependence, progesterone resistance, inflammation, environmental factors and genetic predisposition are some of the known contributing factors. The primary treatment and support options for endometriosis include hormonal therapy, pain management, pelvic floor physical therapy and excisional surgery.
Read more: What causes endometriosis?
Endometriosis and Menopause: The Connection
Menopause, the cessation of menstruation, is a natural phase in a woman’s life. It is commonly believed that endometriosis, an estrogen-dependent condition, resolves after menopause due to the decline in estrogen levels. However, this belief is being challenged as more cases of postmenopausal endometriosis are reported.
The persistence or recurrence of endometriosis after menopause can be attributed to multiple factors. One factor may be persistent higher levels of estrogen in some women. One common estrogen source is Hormone Replacement Therapy (HRT) to manage menopausal symptoms. HRT, which usually includes estrogen, may reactivate endometriosis in some cases. However, it is a complex interplay of estrogen, progesterone or progestins if they are included, receptor sensitivity and number and other molecular signaling factors, including the presence or absence of genomic alterations. It’s also important to keep in mind that endometriosis cells and their surrounding support cells can locally produce estrogen. Estrogen can also be generated by the interconversion of other hormones in your fat cells. So, taking hormonal replacement is not the only potential source of estrogen after menopause.
Postmenopausal Endometriosis: Case Studies and Observations
Numerous case reports and series have documented the recurrence of endometriosis or malignant transformation of endometriotic foci in postmenopausal women. In these reports, the majority of women had undergone surgical menopause (ovaries were removed) due to severe premenopausal endometriosis.
Read more: What would happen to the signs and symptoms of endometriosis after menopause?
Recurrence of Endometriosis
In several case studies, postmenopausal women reported symptoms similar to those experienced during their premenopausal years. These symptoms included abnormal bleeding if the uterus was still intact and pain, often in the genitourinary system. Notably, all women who experienced recurrence were on some form of Hormone Replacement Therapy (HRT), particularly unopposed estrogen therapy.
Malignant Transformation of Endometriotic Foci
Case studies have also reported instances of malignant transformation of endometriotic foci in postmenopausal women on HRT. These cases highlight the potential risk of exogenous estrogen in stimulating malignant transformation in women with a history of endometriosis. It’s critical to point out that this is rare and that is why these are case reports rather than large studies. When these steps towards malignant transformation have been found they are usually associated with genetic alterations like PTEN, TP53 and ARID1A. These alterations are more often found in deep infiltrating and endometrioma types of endometriosis, which are less common than the superficial variant.
Read more: Understanding the Connection between Endometriosis and Cancer
Should HRT be Given to Women with Previous Endometriosis?
The decision to prescribe HRT to women with a history of endometriosis is complex and should be individualized on a holistic basis, looking at the risk and benefit overall. This includes risk and benefit for other symptoms and conditions like hot flashes, osteoporosis, heart disease, skin and vaginal changes, and more. While HRT is the most effective treatment for these menopausal symptoms, it may increase the risk of recurrence or, more rarely, malignant transformation of the endometriosis.
Several observational studies and clinical trials have sought to assess the risks of HRT in women with a history of endometriosis. Although these studies suggested a small association between HRT and endometriosis recurrence, the differences between treatment and control groups were not statistically significant. This means that for the vast majority, it is likely safe to take hormone replacement therapy, especially when considering the far more common benefits of such therapy.
Whether or not the uterus has been removed or not is another factor. HRT for those with an intact uterus usually includes estrogen and a progestational agent, most often a synthetic progestin. This is to protect against developing uterine endometrial cancer. If the uterus is surgically absent, then only estrogen is usually administered. There is a big reason for this. The large Women’s Health Initiative (WHI) study performed over twenty years ago revealed that the risk of breast cancer mainly increases with hormone therapy that contains a progestin (synthetic progestational agent). Estrogen alone does not increase this risk. This is because progestins act as growth factors (mitogens) in breast tissue. While natural progesterone was not evaluated in the WHI study, we know that it is not a mitogen from other studies. So, if your uterus has not been removed, from a breast risk perspective, it may be reasonable to inquire about natural progesterone rather than a synthetic progestin as part of hormonal replacement therapy.
It is also important to recognize that ectopic endometriosis cells are not as sensitive to progestational hormones as is eutopic endometrium, located in the uterine lining. So, the real benefit of adding progestin or progesterone may not be as significant as it is in theory. This requires more study, looking at the very complex molecular interplay of these hormones with their receptors located on and in endometriosis cells.
Should HRT be Given Immediately Following Surgical Menopause?
Another question that arises is whether HRT should be initiated immediately after surgical menopause. Delaying the start of HRT could potentially allow any residual endometriotic tissue to regress before introducing exogenous estrogen. However, current research is inconclusive, with studies showing mixed results.
Read more: Integrative Therapies for Endometriosis
What Menopausal Treatments are Most Appropriate for Women with Previous Endometriosis?
If a woman with a history of endometriosis decides to opt for HRT, choosing the most suitable preparation is crucial. Current research suggests that combined HRT, which includes both estrogen and progestin (or progesterone), may be a safer option for women with residual endometriosis. Keep in mind the caveat about breast tissue and synthetic vs natural progesterone. However, more research is needed to confirm these findings.
Read more: Postmenopausal Malignant Transformation of Endometriosis
Conclusions and Guidance
Navigating the transition to menopause can be challenging for women with a history of endometriosis. While HRT can be effective in managing menopausal symptoms, it may also increase the risk of endometriosis recurrence or malignant transformation.
Women with a history of endometriosis should have a thorough discussion with their healthcare providers about the overall potential risks and benefits of HRT. It is also important to explore the risk and benefit of synthetic vs natural progestational agents. Not all practitioners are well versed in this innuendo.
It’s also important to remember that each woman’s experience with endometriosis and menopause is unique. Therefore, individualized care that takes into account the symptoms, medical history, and personal preferences is crucial.
Ultimately, more high-quality research is needed to better understand the molecular relationship between endometriosis and menopause, and to guide the management of menopausal symptoms in women with a history of endometriosis.
Reference:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5850813/

What Causes Endometriosis?
Actionable Insights and Cause-Based Treatments on the Horizon
Most of what you read online and in books or articles says something like “The cause of endometriosis is unknown, but we have a number of theories, some of which are more likely than others.” But what does this practically mean for you as an individual? As someone who is looking for answers for pain relief or infertility solutions or a diagnosis or why your endo recurred, you probably want practical answers not abstract theories. Actionable answers seem remarkably elusive. To add to your frustration, you may also find yourself stumbling upon a storm of “controversies” regarding the best treatment options, further muddying the water in your personal quest for answers.
As a backgrounder for the problem, endometriosis is a chronic and often painful condition that affects at least 10% of women (XX) of reproductive age and significantly, but not entirely, fueled by sex hormones, mainly estrogen. It is exceedingly rare in men (XY), but has been reported with high doses of prolonged estrogen therapy for prostate cancer and similar conditions. Thus it may have increasing implications for trans women who might be prescribed prolonged estrogen therapy.
This article is an introductory overview of the most current research on the etiology, pathobiology, and potential therapeutic strategies for this extremely complex and prevalent condition. In other words, it attempts to connect what we know with some practical insights for you to base decisions on, including factoring in what may be coming as options down the road. This may or may not alter your decision-making in the here and now.
At the end of this article, we will introduce some practical tips and strategies for getting you to where you want to go. But you have to understand the basis for these first, or it won’t make sense.
What is Endometriosis?
Endometriosis is a medical condition characterized by the growth of endometrial-like tissue, similar to the internal lining of the uterus, outside the uterus. You see this a lot in print, but what does it mean exactly? It means that the cells look quite similar under the microscope, but molecularly they are very different.
Gene expression: Endometriotic cells often express genes associated with survival, inflammation, angiogenesis (blood vessel formation to have access to nutrients), and invasion more highly than typical endometrial cells. Major examples include genes coding for COX-2, VEGF, MMPs, and various cytokines, which are often upregulated. These all encode for aggressive epigenetics (something you will read about below): Epigenetic differences, including DNA methylation and histone modification differences, have been observed between endometriotic and endometrial cells. These changes can alter gene expression without changing the DNA sequence itself.
Hormonal responses: Endometriotic cells often show altered responses to hormones, including estrogen and progesterone. For example, they often contain higher levels of aromatase, an enzyme that produces estrogen and may be less responsive to progesterone due to changes in progesterone receptor expression.
Immune response: Endometriotic lesions often contain immune cells, such as macrophages and T cells, and produce pro-inflammatory cytokines. This is indicative of an ongoing inflammatory response, which may contribute to the symptoms of endometriosis and the survival of endometriotic cells outside the uterus.
The presence of these aberrant endometrial-like tissues in ectopic or unusual locations often results in chronic pelvic pain, intestinal symptoms like bloating, fertility problems, and a host of other symptoms that can significantly impact the quality of life.
The Prevalence and Impact of Endometriosis
Beyond affecting at least 10% of XX women and potentially an increasing number of XY trans-women, the condition is detected in up to 50% of women seeking treatment for fertility issues. Moreover, epidemiological studies suggest that women with endometriosis may be at a higher risk of developing other health conditions including, but not limited to, asthma, rheumatoid arthritis, intestinal dysbiosis, other immune dysfunction, cardiovascular disease and even cancers like ovarian, breast and melanoma. So, while endo cannot explain all symptoms, at the root, these symptoms and signs may still be very related and due to a common root cause. Too often, the diagnosis is extremely delayed, up to a decade, because medical evaluation and testing do not explore these connections. In other words, for example, intestinal complaints are looked at in isolation, and connections to painful periods, pain during sex, or infertility are overlooked.
Symptoms and Diagnosis of Endometriosis
While debate concerning possible causes of endometriosis may continue for some time and the etiologies may overlap or differ between individuals, the first step is to get a correct diagnosis. That leads to the best personalized and informed treatment plan.
The symptoms of endometriosis can vary greatly based on where it is located in your body, the inflammation it is causing and all of the related conditions. But, the most common symptoms include bloating, chronic pelvic pain (both cyclical and non-cyclical), painful periods, painful intercourse, and pain during bowel movements and urination. In addition to physical discomfort, endometriosis is often associated with fatigue and depression, further compounding the impact of the condition.
Diagnosing endometriosis is challenging due to the overlap of its symptoms with more common conditions. This can result in up to a decade of visiting emergency rooms and various specialists, who look at the symptoms through their specialty’s diagnostic lens with somewhat of a tunnel-vision result. So, a gastro will focus on the gut, a general gynecologist will focus on the uterus and ovaries, a neurologist will focus on nerves, a urologist will focus on the bladder, and so on, all looking for common diagnoses within their specialties. These more common diagnoses are usually not endometriosis. Further, there are no specific blood tests yet and imaging is not very accurate. However, inflammatory markers and other tests can help an endo specialist hone in on the diagnosis. Similarly, imaging via ultrasound or MRI may be helpful in finding obvious signs of endometriomas (ovarian cysts filled with old blood and endometriosis tissue) or deep infiltrating type of endometriosis. This simply helps preparation for surgery in the event of findings like disease near the sciatic nerve or growing into the bladder or rectum. However, if negative, the surgeon and/or team must expect and be ready to handle the unexpected.
Today, a definitive diagnosis of endometriosis can only be achieved by biopsy, usually during a diagnostic minimally invasive surgery. Ideally, the surgeon who is operating should be capable of removing any endo that is found by excising it, at that time and not at a subsequent surgery. This is where the diagnosis overlaps with an effective known treatment, excision surgery. The skill base for this is usually beyond most general gynecologists unless they have devoted extra time and training to acquire more advanced surgical skills. If at all possible, this diagnosis and possibly therapeutic surgery should be done correctly the first time in order to minimize misdiagnosis, complications and repeat surgeries.
Based on some of what you are about to read, diagnostics will likely soon be enhanced and accurate blood tests will become available for diagnosis and monitoring. These tests will be based on proteomics and miRNA signatures, which means that endometriosis is associated with various measurable proteins and ribonucleic acids (RNA) of a specific kind, circulating in the blood. A lot of research has already been done on this but it is a matter of finding a combination of these that is accurate.
Unraveling the Cause or Causes of Endometriosis
It is highly unlikely that there will be a discovery of “THE’ unifying cause of endometriosis any time soon, if ever. However, this is still possible on a gene level and is a focus of ongoing research. But when you are looking for actionable, practical answers, this uncertainty should be framed a little better. Far more likely than not, the causes (plural) of endometriosis are polygenic (multiple gene aberrations), multifactorial, and most likely differ between individuals. In general, this certainly affects choosing the best treatment plan for any disease, and the same situation exists in other diseases we treat. There is no single cause of cancer, blood pressure problems, different types of diabetes, and so on. Yet, treatment options are increasing because we are now searching for causative factors and targeted therapies at a molecular, genetic, epigenetic and genomic level. That is a mouthful, but these subcellular molecular factors control everything in your body, normal and abnormal. More on this below.
Theories
One of the most widely accepted theories for the origin of endometriosis is the very old concept of retrograde menstruation. It has been both overly glorified and vilified and certainly misunderstood often. This theory suggests that endometrial tissue fragments and cells escape from the uterus during menstruation, being forced backward through the Fallopian tubes, and implant in the pelvic cavity, directly forming endometriosis lesions. But since retrograde menstruation is very common (at least 70-90% of all women based on laparoscopy observational studies), why do most or all women with a uterus not have endo? Also, from a molecular point of view, eutopic endometrium and ectopic endometriosis cells differ in many respects. The answer to these disconnects is that perhaps this theory is indeed totally wrong and outdated. Or perhaps there are factors in most women that are able to bio-molecularly or immunologically repel the growth of spilled endometrial cells, while some can’t. Or perhaps, since we know somatic stem cells exist in the endometrium, only a fraction of a certain type of stem cell may grow and differentiate if dropped into the peritoneal cavity and not all endometrial cells. So, before completely retiring this theory, more sophisticated studies are required with today’s scientific tools. We have come a long way since the limited science that was available more than 100 years ago, when this was initially proposed.
One thing is for certain, in order for endo to grow and cause problems it has to get there somehow and take root first. Other than retrograde menstruation, how else might that happen?
Other theories as to how endo originates include:
1/ coelomic metaplasia: this theory suggests that peritoneal mesothelium (lining) could transform into endometrial-like tissue (also proposed about 100 years ago)
2/ endometrial somatic stem/progenitor cells may play a role in the formation of endometriosis lesions, getting to the peritoneum either by retrograde menstruation (a variation of the original theory) or via lymph or tiny vascular transport channels
3/ benign metastasis, meaning that endometrial cells are transported by the lymphatic system beyond the uterus
4/ bone marrow pluripotent stem cells (i.e. can turn into any cell imaginable), which we know circulate in the blood, can reach the pelvis or other areas directly, implant due to a favorable local growth environment and grow.
There are others, and variations of the above have also been proposed.
The truth, as almost always, is likely in between all of these theories and likely differs between individuals to some extent. Today, we have molecular evidence that supports most of the above in varying degrees and tends to overlap.
Endometriosis Growth and Progression
Finding out how endometriosis develops will eventually lead to prevention strategies, which may be highly individualized. But for now, the more actionable question is, once the initial cells are there, what causes them to grow and regrow, and at different rates? It is the growth that gets you into trouble with symptoms by triggering inflammation, fibrosis and pain. Keep in mind that there are three general types of endo: 1/ superficial 2/ deep infiltrating and 3/ endometrioma. These can overlap, or not. So, there will never be a one-size-fits-all solution in all likelihood.
However, what happens with progression, when it happens and why is happens is where the rubber meets the road. In answering these questions, insights and actionable strategies can be developed. The following are avenues or pathways by which endometriosis cells can be fueled to grow. Therefore, they present actionable intervention possibilities, now and into the future as we identify more targets.
So, the following is where we are going with all this, what is medically/surgically actionable now and what you can do proactively today that may influence your personal situation. The latter is in the realm of lifestyle and diet, but grounded in science. There is a lot of woo-woo “alternative” stuff out there but also quite a bit that is evidence-informed and that can be helpful.
Genetics and Genomics
From epidemiologic, twin, single gene, and genome-wide association studies (GWAS) there is little doubt that your risk for developing endo is largely grounded in multiple genes (polygenic) and their polymorphisms (alterations of various magnitudes). Further, genes can interact with each other, either amplifying or attenuating disease. But inheriting less desirable gene polymorphisms or mutations is not the be-all end-all because how these genes are activated or suppressed is dependent upon other multifactorial influences (e.g. your environment, including nutrition, toxins and lifestyle choices). In other words, you may inherit good cards or bad cards, but how they play out can be influenced. These influences are based on genomics and epigenetics and related sciences like proteomics, metabolomics, nutrigenomics, and so on, introduced below.
Read more: Is Endometriosis Genetic? Understanding the Genetic Links in Endometriosis.
Epigenetics
Epigenetics studies how genes are controlled or expressed without changing the inherited DNA sequence. “Epi-” means on top of the genes. These are modifications that attach to the DNA, like methyl groups (from diet and supplement sources), which can suppress or help activate genes. Environmental factors such as diet, hormones, stress, drugs, chemical toxin exposure alter methylation. Directly related to endo, alterations in DNA methylation patterns in endometriotic lesions have been described. The epigenome harbors other ways that this gene to environment interplay occurs. This includes histone modification, which is regulatory mechanism that controls unraveling of DNA so it can be read or transcribed. This is also subject to lifestyle and dietary influence today, and is a major potential therapeutic target for the future.
Hormonal imbalances
Endometriosis is often described as a “steroid-dependent” disorder, reflecting the significant role of steroid hormones, mainly estrogen, in its pathogenesis.
This is a VERY complex influence and defies logic in some cases. It is not as simple as therapeutically adding or taking away estrogen or progesterone. Rather, it depends on tissue levels of estrogen and progesterone as well as the number and sensitivity of estrogen and progesterone receptors. The hormones and their receptors work like a lock (receptor) and key (hormone). And that is just the beginning, because there are different components of receptors and additional molecular pathway influences, before and after estrogen binds to its receptor.
For example, there is more estrogen on board when someone is significantly overweight, because there is production from the ovaries AND estrogen from fat cell interconversion AND from environmental xenoestrogen endocrine disruptors that are stored in fat. So that would mean the people who are overweight are more likely to have endo, right? Wrong. Endo, is more common in women with a healthy BMI. Problematic deep infiltrating endo and endometrioma types, is more prevalent in those who are very thin (BMI less than 18.5). Why? This is unknown, but various homeostatic mechanisms like estrogen receptor upregulation can hypothetically lead to higher estrogen sensitivity. Also, hormonal signals are not the only molecular influence on endo.
As another example, after menopause, estrogen levels drop and endometriosis does tend to regress, but not in everyone. That is partly because endometriosis lesions can produce their own estrogen and there are likely other molecular growth factors in play. There are also more ERβ receptors on endometriosis cells, and this causes higher prostaglandin production (which contributes to pain at any point in life).
In general, lowering “estrogen-dominance” to some degree suppresses endometriosis, but ideally not using synthetic progestins to “balance” hormones. Progesterone (natural) and progestins (synthetic) do downregulate and limit the mitogenic (growth) influence of estrogen but progestins can be a mitogenic in some tissues (e.g. breast). Also, overall progesterone or progestins exert less of an effect on endometriosis than on eutopic endometrial tissue inside the uterus. Likewise, dropping estrogen levels radically via GnRH agents for a relatively short period of time does not achieve the desired result and causes side effects and harm. The risk vs benefit is particularly precarious here. Potentially, chronic gentle suppression might be more effective, and at least safer. This can be achieved by using progesterone. Synthetic progestins like norethindrone acetate can be used but with the caveats above. Alternatively, you can also help by consuming seaweed, regular exercising and other lifestyle choices, like active xenoestrogen toxin avoidance.
Read more: What would happen to the signs and symptoms of endometriosis after menopause?
Read more: Endometriosis And Menopause: Everything You Need To Know
Inflammation
Endometriosis may be partially a product of inflammation and is also characterized by generating an inflammatory response itself. So it can snowball and contribute to the development and persistence of symptoms. Immune cells, such as macrophages, NK and T cells, are found in abundance in endometriosis lesions, and their interactions with endometriosis cells can promote the formation and growth of these lesions. Additionally, the peritoneal fluid of women with endometriosis often exhibits an altered composition, with increased levels of pro-inflammatory cytokines and growth factors.
Inflammation can be from various sources, including infection which may be clinical (in other words you feel sick) or chronic subclinical. For example it is well established that chronic endometritis (infection inside the uterine lining) is present in endometriosis patients more often than those without endo. This is an association and the cause-effect is not well worked out, but more recently various bacteria have been implicated. At least in animal models, antibiotic treatment targeting those bacteria have produced regression of endometriosis lesions. Bacteria from the uterus or cervix can easily travel, either directly through the Fallopian tubes or via the bloodstream, to cause inflammation in the peritoneal cavity. This inflammatory response is postulated to lead to progression of endo.
Leaky gut, which may be related to an unhealthy low microbiome diversity, can lead to bacterial fragments, called lipopolysaccharides (LPS), seeding the peritoneal cavity as well. This in turn causes inflammation and the same potential effect on endo growth.
But inflammation can be due to a myriad of other non-infectious factors including stress, autoimmune disorders, obesity, systemic diseases like diabetes or pre-diabetes, mast cell activation, toxin exposure and so on.
Most of these inflammatory conditions are actionable. Failing that, general anti-inflammatory strategies may also be beneficial, both pharmacologic and integrative.
Dysbiosis
Dysbiosis of the gut has a direct negative effect on the gut-endocrine axis and can impact endometriosis growth. There are three significant ways this happens.
Estrobolome: This term refers to the fraction of gut microbiota capable of metabolizing estrogens. In healthy individuals, the estrobolome helps maintain a balance of estrogen levels by contributing to the enterohepatic circulation of estrogens, thereby affecting the overall circulating and excreted amounts of these hormones. Dysbiosis, however, can disrupt the functioning of the estrobolome, leading to alterations in the metabolism of estrogens. In the context of endometriosis, this dysbiosis may lead to excess circulating estrogen, which stimulates the growth and survival of endometrial cells outside the uterus, contributing to endometriosis.
Gut-Endocrine Axis: The gut microbiota also influences the gut-endocrine axis, which refers to the complex interplay between the gut microbiota, gut cells, and endocrine organs. Dysbiosis can result in changes in gut permeability (also known as “leaky gut” introduced above), leading to increased inflammation and immune dysregulation. This can, in turn, disrupt normal hormone regulation, potentially exacerbating conditions like endometriosis.
Gut-Brain Axis: Dysbiosis can also influence the gut-brain axis, a bi-directional communication system that links the central nervous system with the enteric nervous system. Changes in the gut microbiota can affect this axis and lead to altered pain perception and increased stress responses, both of which can affect the experience and progression of endometriosis.
Read more: Endo-Fighting Microbiome Optimization: Research-based Tips
Cancer molecular shared growth drivers
It’s important to note that a very small fraction of women with endometriosis might develop an endo-associated cancer (<1%), and gene mutations probably drive that. Having said that there is overlap of these genes with more aggressive variants of endo, like deep infiltrating and endometrioma. Meaning, they may not lead to cancer but may still fuel a more aggressive form of endometriosis. This has led some researchers to propose that endometriosis is a pre-cancerous condition in a small percentage of those with endo. The most studied gene in this regard is ARID1A, but the following have also been associated: KRAS, PTEN, HOXA10, VEGF, ESR1 and ESR2, and FN1. Since there is a lot of research on these in the cancer world, there may be targeted therapies for more aggressive variants of endometriosis arising from this research.
Read more: How to tell the difference between endometriosis and ovarian cancer.
Current Treatment Strategies for Endometriosis
Current effective treatment for most patients is built upon a personalized evaluation, correct diagnosis, and expert excision surgery to reduce the amount of inflammation and triggering of pain and other symptoms. This is followed by some degree of medical suppression in many patients, usually on a hormonal basis. Personalized guidance is key, which does not go overboard by either over or under-treating.
Excisional surgery is today’s cornerstone because it yields an accurate diagnosis and removes the visible disease if at all possible. But this should not be indiscriminate and should be done by an expert if the index of suspicion for endo justifies the surgical risks. It seems prudent to reserve consideration of medical suppressive treatments for use after an accurate diagnosis is made vs. use of potentially very dangerous hormonal therapies based on a suspicion of endo only.
Before and after surgery there are quite a few optimization strategies, including pelvic floor physical therapy (PFPT) and a pain management plan which take into account what the pain triggers are. These can differ between people. Both of these supportive therapies are complex but integral to treatment in the vast majority of cases. This helps you get ready for surgery and go through surgery more smoothly and then transition to a life without endo.
In addition, evaluation of the related conditions covered in this article, like dysbiosis and possible small bacterial overgrowth (SIBO) and leaky gut is mandatory. The symptoms can easily cross over from these conditions and endo so it helps to sort out other related causes of pain and bloating. Finally, evaluation should also consider mast cell activation, chronic inflammatory response syndrom (CIRS), autoimmune hypothyroidism, fibromyalgia, irritable bowel syndrome (IBS) or disorders of gut-brain interactions, interstitial cystitis (IS). There are also conditions not directly related to endo but often associated, like Lyme disease and mold. The latter two can accentuate inflammatory response and water logged buildings often have black mold. The CDC is also warning that tick-borne disease like Lyme and Babesiosis is on the rise.
Also, as you are now aware from reading this article, there are many other steps you can take to influence and limit the course of endo recurrence and progression. None of this is magic and none of it is a quick fix but when guided by an expert it is also generally pro-health, not dangerous and not expensive by and large. Again, best results are obtained with expert guidance.
Emerging Therapeutic Approaches
Although we have some options today, there is a pressing need for novel, effective therapies for endometriosis beyond surgery and variations of hormonal therapy. For instance, immunotherapies that target specific cytokines or immune cells involved in endometriosis are currently under investigation. Other promising areas of research include therapies targeting the altered metabolic environment of endometriosis lesions and neuromodulatory treatments aimed at disrupting pain pathways associated with the condition. This article is not intended to cover these future options in depth, but based on all of the potential causes and influencing factors it becomes easier to see what is coming sooner than later.
Some recent example animal studies and concepts which should get to human trials include: Targeted anti inflammatory therapy, antibiotic therapy targeting specific bacteria like Fusobacterium, antibody (AMY109) that binds IL-8, small interfering RNA for VEGF (siVEGF), epigenetic and histone modification targeting endo-related gene transcription including estogen and progesterone receptors, epigenetic modification of T-cell immune response in endo, ARID1A and related “cancer gene” targeting, and more. So, while we do not have these available in clinical practice yet, the research wheels are turning. Certainly that can be accelerated with more funding, but it is ongoing.
Holistic Proactive Principles
While we await mainstream targeted molecular therapies you should know that the same molecular pathway targets are also influenced by natural integrative approaches. They may not be laser targeted on a specific pathway but that can actually be a good thing. Abnormal cells like endo know how to work around blockades from therapy and the treatment can stop working. We know that from other diseases where molecular therapies are already quite common. Mother nature has actually considered that problem, so to speak, and a lot of nutrients can have a synergistic favorable effect on multiple molecular pathways at the same time.
Further, your microbiome, estrobolome, inflammation, oxidation, nutrition, stress, lack of exercise, and so much more, impacts your body on the basis of epigenetics that was introduced above and, more specifically, a significant part is related to nutrigenomic epigenetics.
It’s critical to note that this does not mean loading up on the weirdest supplements you never heard of that cost an arm and a leg. The 80/20 rule, which says that you get 80% of your result from 20% of an action, suggests that you can get pretty far with a personalized anti-oxidant anti-inflammatory diet and that is most often embodied by a whole food plan-based diet. Combine this with an exercise plan and stress management and you are 80% of the way there.
Read more: Integrative Therapies for Endometriosis
Conclusion
Endometriosis is a complex, multifaceted, polygenic and multifactorial disorder, and much remains to be understood about its causes and progression. As our understanding of endometriosis deepens, so too does our ability to develop accurate diagnostics and targeted, effective therapies. But for now, in expert hands and with your own proactive commitment to nutritional and lifestyle options, outcomes can be good to great. There is no disease or condition where everyone gets the benefit of a great outcome, but certainly in the case of endo it can be optimized by seeking out an endometriosis expert.
Read more: Breaking the Cycle: Understanding Endometrioma Recurrence After Surgery.
Read more: The Endometriosis Roller Coaster: Understanding Recurrence and How to Prevent It
References:
- Endometriosis: Etiology, pathobiology, and therapeutic prospects
- The Main Theories on the Pathogenesis of Endometriosis
- Nutrition in the prevention and treatment of endometriosis: A review
- Cancer-Associated Mutations in Endometriosis without Cancerf

Is Endometriosis Genetic? Understanding the Genetic Links in Endometriosis.
Endometriosis is a significant cause of discomfort and can greatly reduce the quality of life. Although the disease’s origin remains somewhat elusive, research indicates a potential familial pattern. This article delves into the possible genetic basis of endometriosis, exploring its genetic and genomic aspects and their implications for improved diagnosis and treatment.
The Enigma of Endometriosis
Endometriosis is a condition where tissue similar to the endometrium – the internal lining of the uterus – grows outside the uterus. This can occur on the ovaries, fallopian tubes,the tissue lining the pelvis, and beyond. In some cases it grows superficially, in others it can invade deeply into other tissues or affect the ovaries. Despite extensive research, the exact cause of endometriosis and the reason for these variants remains an enigma. However, an interesting pattern has emerged over time – the disease appears to cluster in families, suggesting a potential genetic link.
Is Endometriosis Genetic?
Familial predisposition suggests that endometriosis could be inherited in a polygenic or multifactorial manner. Polygenic or multifactorial inheritance refers to a condition that is affected by multiple genes (polygenic) and influenced by environmental factors (multifactorial). Since everyone is different, this may also help explain why some people get one variant of the disease and others do not.
Challenges in Understanding the Genetic Link
Several factors make it difficult to understand the genetic link in endometriosis. The foremost is the diagnostic method. Endometriosis can only be definitively diagnosed through invasive procedures like laparoscopy or laparotomy. This can often lead to under-reporting of the disease with many people walking around undiagnosed for years. Another factor is the disease’s heterogeneous nature mentioned above, as it can manifest in different variants and locations within the body, suggesting potentially diverse disease processes. Once these genetic links, which likely overlap, are unraveled and mapped then we will be able to diagnose endometriosis through blood tests rather than surgery. Each genetic link eventually leads to molecular signals which can be used for diagnosis, treatment and follow-up monitoring.
Familial Clustering and Evidence
Epidemiologic research has shown a familial clustering of endometriosis, meaning it appears more frequently within families. However, it does not seem to follow a simple Mendelian inheritance pattern. This observation supports multiple genetic factors contributing to the disease, consistent with polygenic/multifactorial inheritance and environmental impact.
Genetic Mapping and Endometriosis
Gene mapping is a technique used to investigate potential gene mutations or polymorphisms associated with diseases like endometriosis. This method involves looking at the genome for excess sharing of informative polymorphic microsatellite markers in affected siblings. Studies using this method have highlighted areas in chromosomes 10 and 20 that may be linked to endometriosis. Despite the identification of these risk loci, the exact mechanism by which these genes influence the development of endometriosis is not yet fully understood. So this association means someone may be at higher risk but does not guarantee that endometriosis will actually develop in any given individual.
Genome-Wide Association Studies
Genome-Wide Association Studies (GWAS) represent a very promising method used to identify differences in the genetic makeup of individuals that could be responsible for variations in disease susceptibility. Basically, they compare the genomes of people with a certain disease (like endometriosis) to healthy individuals to look for genetic differences.
GWAS scans the genome of individuals for small variations, called single nucleotide polymorphisms (SNPs), that occur more frequently in people with a particular disease than in people without the disease. Each study can look at hundreds or thousands of SNPs at the same time. Then statistical methods can help identify which SNPs are associated with the disease.
First, genetic markers identified through GWAS could potentially be used to develop a genetic test for endometriosis. This could enable earlier and more accurate diagnosis of the disease, which is often difficult to diagnose due to its nonspecific symptoms and the need for invasive procedures to confirm diagnosis.
Second, as an example of treatment potential, if a GWAS identifies a SNP in a gene involved in inflammation that is associated with endometriosis, researchers could develop a drug that targets this gene to reduce inflammation and treat endometriosis. There are many other potential molecular pathways that influence endo development and progression that can and will be targeted.
Genomics of Endometriosis
While genetics refers to the inheritance of a trait, genomics focuses on how genes are expressed, meaning how they are turned into structural proteins and signals and so forth. Genomics studies have identified significant alterations in gene expression in endometriosis, providing major insights into underlying biology. Genomic studies will likely lead to new noninvasive diagnostic strategies and possible new therapies.
So, deeper understanding of endometriosis genomics can provide insights into the biological pathways and processes involved in the disease. This can, in turn, inform diagnosis, treatment, and monitoring strategies.
Diagnosis:
When we better understand the genomics of endometriosis, we will be able to develop non-invasive non-surgical diagnostic tests. For example, if certain genetic variants are found to be associated with endometriosis, a simple blood test could be developed to look for these variants.
In addition to these genetic tests, understanding the molecular signaling pathways involved in endometriosis could potentially lead to the development of biomarker-based tests. Biomarkers are substances, such as proteins, that are indicative of certain biological conditions, like inflammation or fibrosis formation. If certain molecules are found to be elevated or decreased in women with endometriosis, these could be used as biomarkers for the disease.
Read more: The Different Tests Used to Diagnose Endometriosis
Treatment:
Current treatments for endometriosis are basically limited to hormonal-based therapy, pain management, and surgery. However, these approaches do not work for everyone and can have significant short and long-term side effects. Short of a complete excision surgery, which is the cornerstone of today’s therapy, these are not curative therapies. Despite world-class excision surgery microscopic invisible post-surgical residual remains a concern and we need better options to eliminate anything that might be left in order to minimize or eliminate risk of recurrence.
By understanding the genes and molecular pathways involved in endometriosis, we can identify new targets for biological drug development. For example, if a certain gene is found to be overactive in endometriosis, an agent could be developed to inhibit this gene. Similarly, some protein-based molecular pathways can be selectively inhibited. This is reality today in many diseases and there is no reason that endometriosis should not be amenable to similar options.
Read more: Why You Need an OB-GYN Who Specializes in Endometriosis
Monitoring:
Lastly, understanding the genomics of endometriosis could also improve disease monitoring. For example, if certain genetic variants or molecular signals are associated with disease progression, these could potentially be used to monitor disease progression or response to treatment. This could lead to more personalized treatment strategies and improve patient outcomes. To the point of microscopic residual after excision surgery, if none is likely present and no signals point to that, then no additional therapy would be required. On the other hand, if there is molecular evidence to support possible micro-residual then treatment might be initiated right away, or at least at the time of first molecular evidence of recurrence or progression.
The caveat here is that the translation of genomic and molecular research into clinical practice is a complex process that requires extensive further research and validation. It’s also worth noting that endometriosis is a complex disease likely influenced by a combination of genetic, environmental, and hormonal factors, and understanding these will be crucial for developing better diagnostic and treatment strategies.
Read more: Debunking the Myths About Endometriosis & Exploring the Facts
Concluding Thoughts
The notion of endometriosis being genetic is supported by a growing body of research, highlighting the disease’s intricate and multifaceted nature. While our understanding of the genetics and genomics of endometriosis is still evolving, it holds the promise of improved diagnosis and treatment methods in the future. By continuing to explore the genetic foundations of this disease, we move closer to empowering those affected by endometriosis with knowledge and more effective treatment options.
In the end, unlocking the genetic and genomic secrets of endometriosis will pave the way for a future where this enigmatic condition is better understood, diagnosed, and treated. While a lot of the above is in research or upcoming, some is available now. Seek out an endometriosis expert who can discuss these with you and individualize a treatment plan.
Reference:

How Does Endometriosis Cause Infertility?
Endometriosis, a complex and often misunderstood condition, can significantly impact a woman’s fertility. Understanding the intricacies of this condition, its causes, and its effects on fertility can be vital in paving the way for effective treatment strategies.
An Introduction to Endometriosis
Endometriosis is a benign, estrogen-dependent disorder primarily affecting approximately one in ten cisgender women in their reproductive years. It may also have an impact on transgender men, where the condition may be present in a higher percentage. While it has been reported in cisgender men, it is exceedingly rare. Thus the fertility impact discussed here is that which specifically affects the uterus, Fallopian tubes and ovaries.
Endometriosis is characterized by the abnormal presence of endometrial-like tissue outside the uterus. This abnormally growing tissue is often found in the pelvic region, such as on the ovaries, fallopian tubes, and the outer surface of the uterus. Still, in some cases, it can extend beyond the pelvic area.
While endometriosis affects approximately 10-15% of cisgender women in their reproductive years, the condition is more prevalent in those struggling with infertility, affecting up to 25%-50% of this demographic. The exact cause of endometriosis remains a subject of research and debate, and its impact on fertility is multi-faceted and complex.
Understanding The Pathogenesis of Endometriosis
While the precise cause of endometriosis is still under debate, several theories have emerged over the years, trying to explain the pathogenesis of this condition.
Retrograde Menstruation
The oldest theory is retrograde menstruation, which suggests that during menstruation, some of the endometrial tissue flows backward, through the fallopian tubes, into the pelvic cavity instead of leaving the body. These endometrial cells then attach to the peritoneal surfaces, proliferate, and form endometriosis implants.
Coelomic Metaplasia and Metastatic Spread
Other theories suggest that cells in the peritoneum can transform into endometrial cells, a process known as coelomic metaplasia. Alternatively, endometrial tissue may spread through the bloodstream or lymphatic system to other parts of the body, a process known as metastatic spread. Both these theories could explain how endometriosis implants can be found in areas outside the pelvic region.
Altered Immunity
Another theory proposes that women with endometriosis have a compromised immune system, which fails to eliminate the endometrial cells that have migrated to the peritoneal cavity. This immune dysfunction may also contribute to the progression of the disease, as the immune system’s reactions may inadvertently promote the growth and proliferation of endometrial implants.
Stem Cells and Genetics
Recent research also suggests that stem cells and genetic factors may play a role in the development of endometriosis. Bone marrow-derived stem cells may differentiate into endometriosis cells, contributing to the formation of ectopic endometrial-like tissue.
Additionally, genetic predisposition may play a significant role in the development of endometriosis. People with a first-degree relative affected by the disease have a seven times higher risk of developing endometriosis.
Learn More: Current Knowledge on Endometriosis Etiology: A Systematic Review
How Does Endometriosis Cause Infertility?
Endometriosis can affect fertility through various mechanisms:
Effect on Gametes and Embryo
Endometriosis can impact the production and quality of oocytes (eggs), as well as sperm function and embryo health. The presence of endometriomas (cysts caused by endometriosis) and the inflammatory environment they create can negatively affect both oocyte production and ovulation.
Effect on Fallopian Tubes and Embryo Transport
Endometriosis can disrupt the fallopian tubes’ normal functioning and impact the embryo’s transport. The inflammation caused by endometriosis can impair tubal motility and cause abnormal uterine contractions, which can hinder the transportation of gametes (eggs and sperm) and embryos.
Effect on the Endometrium
Endometriosis can also impact the uterine lining or endometrium, which can lead to implantation failure. Research suggests that endometriosis can alter the gene expression in the endometrium, affecting its receptivity to implantation.
Read More: Learn More About the Connections Between Endometriosis and Infertility
Current Treatment Options for Endometriosis-Associated Infertility
The treatment of endometriosis-associated infertility is multi-faceted and can include expectant management, medical treatment, surgical treatment, and assisted reproductive technologies.
Expectant Management
While endometriosis significantly lowers fertility rates, some women with mild to moderate endometriosis can still conceive without any medical or surgical intervention. However, this approach may be more suitable for younger women with mild endometriosis and no other fertility issues.
Surgical Treatment
Surgery can be both diagnostic and therapeutic in the context of endometriosis. The goal of surgical treatment is to remove or reduce endometriosis implants and restore normal pelvic anatomy and reduce the inflammatory impact. This could potentially improve fertility, particularly in women with severe endometriosis.
Assisted Reproductive Technology
In vitro fertilization (IVF) is currently the most effective treatment for endometriosis-associated infertility. IVF can be particularly beneficial for women with severe endometriosis or those for whom other treatments have failed.
Medical Treatment
Medical treatment for endometriosis primarily targets reducing the severity of the disease and relieving symptoms. Hormonal medications such as combined oral contraceptives, progestins, danazol, and gonadotropin-releasing hormone agonists or antagonists (GnRH analogs) are commonly used. However, these medications have not shown any significant benefit in treating endometriosis-associated infertility.
Read More: Natural, Medical & Surgical Treatment of Endometriosis Infertility
Looking Towards The Future: Potential Treatments
As our understanding of endometriosis deepens, new potential treatment options are emerging, such as therapies targeting the abnormal gene expression and inflammation caused by endometriosis. Furthermore, stem cell therapies and genetic interventions hold promise for treating endometriosis-associated infertility in the future. As research continues, the hope is that these advancements will lead to more effective strategies for managing this complex condition and improving fertility outcomes in those with endometriosis.
Read More: How Do Endo Fertility Issues Impact the Mental Health of a Person?
Reference: Macer ML, Taylor HS, Obstet Gynecol Clin North Am. 2012 Dec;39(4):535-49.

Interstitial Cystitis and Endometriosis: Unraveling the Evil Twins Syndrome of Chronic Pelvic Pain
Introduction
Chronic pelvic pain (CPP) is a health condition that burdens millions of women worldwide. The complexity of diagnosing and treating CPP is often overwhelming due to the multitude of potential underlying causes and associated conditions. Two such conditions, often called the “Evil Twins” syndrome, are Interstitial Cystitis (IC) and Endometriosis, both commonly found in patients suffering from CPP. This article will explore these conditions’ prevalence, diagnosis, and treatment in patients with CPP.
Understanding Chronic Pelvic Pain
Chronic Pelvic Pain (CPP) is a prevalent health condition affecting an estimated 9 million women in the United States alone. It accounts for up to 40% of laparoscopies and 10% to 12% of all hysterectomies, indicating its significant impact on women’s health. The annual expenditure on diagnosing and treating CPP is nearly $3 billion.
The “Evil Twins”: Interstitial Cystitis and Endometriosis
Two conditions frequently associated with CPP are Interstitial Cystitis (IC) and Endometriosis. These conditions can present similar symptoms and coexist in patients, making the diagnosis and management of CPP even more challenging.
Interstitial Cystitis (IC)
Interstitial Cystitis, or bladder-originated pelvic pain, is a significant disorder related to CPP. The etiology of IC is multifactorial and progressive, involving bladder epithelial dysfunction, mast cell activation, and bladder sensory nerve upregulation. The exact prevalence of IC in the United States varies, with estimates ranging from 10 to 510 per 100,000 normal population. However, current research suggests that IC might be more prevalent than previously estimated.
Endometriosis
Endometriosis is another common condition among women with CPP, affecting more than half of the patients diagnosed with CPP. Symptoms include pain during sexual intercourse (dyspareunia), cyclical perimenstrual lower abdominal pelvic pain, symptom flares after sexual intimacy, and irritative voiding in case of urinary tract involvement. A definitive diagnosis of endometriosis requires visual confirmation of the lesion during laparoscopy and histologic confirmation of the presence of both ectopic endometrial glands and stroma.
The Overlap Between Interstitial Cystitis and Endometriosis
Research has demonstrated a high rate of overlap between IC and endometriosis in patients with CPP. This overlap poses challenges in diagnosis and treatment, as the presence of one condition does not preclude the existence of the other. Therefore, it is crucial to consider both conditions in the evaluation of patients with CPP.
Diagnosis of Interstitial Cystitis
The diagnosis of IC and endometriosis involves various tests and procedures, including the Potassium Sensitivity Test (PST), cystoscopy with hydrodistention, and laparoscopy.
Laparoscopy
Laparoscopy for direct visualization of endometriosis lesions and taking a biopsy is the gold standard for endometriosis diagnosis.
Read more: The Different Tests Used to Diagnose Endometriosis
Potassium Sensitivity Test (PST)
The PST is a diagnostic test developed to detect abnormal permeability of the bladder epithelium, a key factor in the pathophysiology of IC. Previous studies have validated the use of the PST in diagnosing IC, particularly at the early stages of the disease.
Cystoscopy with Hydrodistention
Cystoscopy with hydrodistention is a diagnostic procedure often used to confirm the presence of IC. The bladder is filled with sterile water under passive hydrostatic pressure, then slowly drained. The presence of submucosal petechial hemorrhages, or glomerulations, confirms the diagnosis of IC.
Biopsy
During cystoscopy under anesthesia, your provider may remove a sample of tissue (biopsy) from the bladder and the urethra for examination under a microscope. This is to check for bladder cancer and other rare causes of bladder pain.
Urine cytology
Your provider collects a urine sample and examines the cells to help rule out cancer.
Conclusion
This article highlights the complex interplay between IC and endometriosis in the context of CPP. It underscores the need for careful evaluation and simultaneous consideration of these conditions in patients with CPP. A multidisciplinary approach, including the use of PST and concurrent cystoscopy and laparoscopy, is crucial for accurate diagnosis and effective treatment of concurrent interstitial cystitis and endometriosis.

Endo-Fighting Microbiome Optimization: Research-based Tips
Endometriosis is partly caused by, and causes, inflammation. The origin or genesis of this
inflammation is probably multifactorial but recent research suggests that the microbiome, the
community of microorganisms living in or on the human body, plays an important role through
inflammatory pathways. Dysbiosis, which means an imbalance or impairment of the microbiota,
is observed in endometriosis, and is thought to both contribute to and result from endo.
Studies have focused on the gut, peritoneal fluid, and female reproductive tract microbiota to
identify specific microbiome signatures associated with endometriosis. The gut microbiome, in
particular, has been extensively studied. Changes in bacterial composition, such as increased
levels of Proteobacteria and decreased levels of Lactobacilli, have been observed in the gut of
endometriosis patients. Other body sites, including the peritoneal fluid and female reproductive
tract, also show altered microbiota in endometriosis.
The dysbiosis observed in endometriosis is believed to contribute to the disease through
various mechanisms. One theory suggests that bacterial contamination, particularly with
Escherichia coli, in the menstrual blood may lead to inflammation and immune activation in the
peritoneal cavity, contributing to endometriosis development. Dysbiosis can also affect
estrogen metabolism, through dysfunction of the so called “estrobolome”. This can lead to
increased levels of circulating estrogen and a hyper-estrogenic state, which promotes
endometriosis. Additionally, dysbiosis-induced epigenetic changes and immune modulation
may play a role in direct endometriosis pathogenesis.
Research on the microbiome in endometriosis is still in its early stages, but it holds promise for
potential diagnostic and therapeutic approaches. Microbiome testing could potentially be used
as a non-invasive tool for detecting endometriosis, complementing current imaging modalities.
The technology for doing this is already here and you can get it ordered. However, the meaning
of the results is still not well understood in any given individual. So, it’s complicated.
Beyond testing, manipulating the microbiome through interventions like probiotics, antibiotics,
or dietary modifications may offer new treatment options for endometriosis. To the extent that
you can diversify your microbiome and get it to a healthier state, this is something that can be
done with little risk or cost today. Options available to you are covered below, most of which
are focused on the bacterial part of your microbiome.
Future studies will explore the role of different types of microorganisms, beyond bacteria, such
as viruses and fungi, and utilize advanced analytical methods like shotgun metagenomics and
metabolomics to gain a more comprehensive understanding of the microbiome in
endometriosis. Newer technologies like this are significantly accelerating gains in knowledge.
Meanwhile, emerging understanding of the bidirectional relationship between endometriosis
and the microbiome has implications for potential treatment strategies available today.
Antibiotics:
Antibiotics could be used to target specific bacteria associated with dysbiosis in
endometriosis, especially if you are diagnosed with small intestinal bacterial overgrowth (SIBO).
Animal studies have shown that treatment with antibiotics can reduce the size of endometriotic
lesions and associated inflammation. In humans, we know that chronic endometritis (infection
of the uterine cavity) seems to play a role in development of endo. However, this requires
expert guidance. It’s critical to exercise caution with antibiotic use to avoid disrupting healthy
commensal (good bacteria) microbiota and contributing to antimicrobial resistance. You don’t
want to grow a bug that might be resistant to multiple antibiotics down the line.
Probiotics:
Probiotics are live bacteria that can have beneficial effects on your microbiome
health and diversity when consumed. Studies in animal models have demonstrated that certain
probiotic strains, such as Lactobacillus gasseri, can suppress the development and growth of
endometriotic lesions. Probiotics may modulate the immune response and restore a healthier
microbiota composition, potentially mitigating the inflammatory processes associated with
endometriosis. However, again, this requires expert guidance because, for example, it could
lead to ineffectiveness against or exacerbation of SIBO. This is partly because there are at least
three different general types of SIBO, based on what type of gas is produced by the
microbiome.
Prebiotics:
Prebiotics are basically food substances that selectively promote the growth of
beneficial bacteria in the gut. By providing a favorable environment for beneficial bacteria,
prebiotics can help restore a healthy microbiota balance. An example of a prebiotic shown to
be beneficial in SIBO treatment is partially hydrolyzed guar gum (PHGG). Further research is
needed to investigate the potential roles of prebiotics in endometriosis treatment, but it could
be a gamechanger for simple treatment of various intestinal disorders, leaky gut and so on.
Dietary modifications:
Diet can hugely influence the composition and activity of the
microbiome. Consuming a diet rich in fiber and plant-based foods, which are known to support
a diverse and healthy microbiota, may have beneficial effects on endometriosis. Low FODMAPs
diets, which restrict fermentable carbs, can help. Omega-3 polyunsaturated fatty acids (PUFAs),
found in fatty fish, flaxseeds, and chia seeds, have shown anti-inflammatory properties and
have been associated with a lower incidence of endometriosis. Incorporating these dietary
changes, among many others, may help modulate the microbiome and reduce inflammation.
Immunomodulation:
The microbiome has profound effects on the immune system, and
targeting the immune response could be a potential avenue for endometriosis treatment.
Modulating the immune system through therapies such as immune-suppressing medications or
immune-modulating agents may help regulate the inflammatory processes associated with
endometriosis. The idea here is to keep it as natural as possible, but sometimes prescription
medications may turn out to be necessary.
Please keep in mind that these treatment implications are based on current research, primarily
in the lab and animal models, and further studies are needed to validate their effectiveness and
safety in humans. Additionally, personalized approaches considering an individual’s specific
microbiota composition and disease characteristics may be necessary for optimal treatment
outcomes. It is exciting research in development and will be part of upcoming revolutionary
advances which take us far beyond hormonal manipulation for endo management. Since these
approaches are exploring the root cause of endo, treatments will likely be therapeutic as
opposed to simply something that reduces symptoms, which is the case with today’s hormonal
therapies.
The best part is that with proper expert guidance, much of the above can be used today
because, in most cases, the risk and cost are relatively low.
References:
Uzuner, C., Mak, J., El-Assaad, F., & Condous, G. (2023). The bidirectional relationship between
endometriosis and microbiome. Frontiers in Endocrinology, 14, 1110824. doi:
10.3389/fendo.2023.1110824
Moreno, I., Franasiak, J. M., & Endometrial Microbiome Consortium. (2020). Endometrial
microbiota—new player in town. Fertility and Sterility, 113(2), 303-304. doi:
10.1016/j.fertnstert.2019.10.031

Understanding Fatigue and Endometriosis: A Practical No-Nonsense Guide
Fatigue is a common symptom these days, but for those living with endometriosis, it can be
particularly challenging. While it’s not one of the primary symptoms of endometriosis, fatigue is
often reported by women who have endo. What’s the relationship? What are some potential
causes and what can you do to regain some lasting energy, without hocus pocus “cures”, more
coffee, or energy drinks?
If you’re not sure if you have endometriosis, please remember that not all symptoms are
directly related to or caused by endo. While many can be related, something else can be
wrong. For example, you can have anemia from various causes, adrenal or thyroid disease and
many other conditions, some of which can be serious. Chronic fatigue is a very challenging
condition to treat but before treatment you first must get to the root cause or causes. This
requires either a mainstream internal medicine or family medicine doctor that is going to
carefully explore every angle with you. Most will just get basis tests and not spend much time
with you, because their time is limited by today’s healthcare mess. Alternatively, seek out an
integrative and/or functional medicine physician who is trained to approach all disease by
tracing it down to the root cause. This is critical and not just a matter of getting a few blood
tests. If you’re “lucky” something obvious might pop up on basic testing. But most of the time
it’s not that straightforward. Do it right!
If you already know you have endo and are experiencing fatigue along with other symptoms of
endometriosis, make sure your endo specialist is aware of this. They can help evaluate how root
causes may be in play that are directly related to endo or adenomyosis, provide an accurate
diagnosis or diagnoses, and develop a personalized treatment plan. Everyone is not the same.
Understanding Fatigue and Endometriosis:
The Impact of Chronic Pain:
Endometriosis, in most, is characterized by chronic pelvic pain, which can significantly impact
quality of life. Living with constant pain can be exhausting both physically and mentally, leading
to fatigue. Additionally, the stress and emotional burden associated with chronic pain can
further contribute to fatigue.
Hormonal Imbalances:
Hormonal imbalances play a role in the development and progression of endometriosis.
Estrogen, in particular, is thought to promote the growth of endometrial tissue outside the
uterus. Fluctuations in estrogen levels throughout the menstrual cycle can result in fatigue and
tiredness. Furthermore, if you are in a hormone balancing program of some kind, excess
progesterone can definitely cause fatigue. “Balancing hormones” requires an expert hand
because it is like conducting a symphony orchestra, as opposed to throwing in a few hormones
to see what happens. Beyond that, it is not just a matter of balancing estrogen and
progesterone. For example, people with endometriosis are six times more likely to have an
underactive thyroid. So, again, it’s a symphony orchestra, not a small band that needs
conducting for best results.
Sleep Disturbances:
Endometriosis often leads to sleep disturbances due to pain, discomfort, and hormonal
imbalances. Insufficient or poor-quality sleep can easily leave one feeling fatigued during the
day. It is essential to prioritize sleep hygiene and seek strategies to improve sleep, such as
creating a relaxing bedtime routine and ensuring a comfortable sleep environment.
Anemia:
Endometriosis and adenomyosis can lead to heavy or prolonged menstrual and inter-menstrual
bleeding, which can result in iron deficiency anemia. Iron is vital for carrying oxygen to the
body’s tissues, and when its levels are low, fatigue and weakness can occur. Bringing iron levels
up may mean taking iron supplements for a while or it can as simple as adjusting your diet to
include iron-rich foods, like leafy veggies.
Inflammation and Immune Dysfunction:
Endometriosis is associated with chronic inflammation and immune system dysfunction. The
inflammatory response and immune activation can definitely contribute to fatigue. Strategies
that reduce inflammation, such as a healthy diet rich in anti-inflammatory foods, regular
exercise, and stress management techniques, may help alleviate fatigue symptoms.
Management Strategies for Fatigue:
Pain Management:
Effective pain management is essential for reducing fatigue associated with endometriosis. Your
doctor may recommend over-the-counter pain relievers, such as nonsteroidal anti-
inflammatory drugs (NSAIDs), to help alleviate pain and inflammation. Hormonal treatments,
such as birth control pills or hormonal intrauterine devices (IUDs), can also be prescribed to
regulate hormone levels and reduce pain. Of course, narcotics are an option but that can lead
to feeling loopy and fatigued, defeating the purpose. Gabapentin and similar drugs can help
with central sensitization and might be used just for transition while you reduce pelvic floor
inflammation triggers using multi-modality therapies. Pelvic floor physical therapy is critical.
Integrative modalities like acupuncture and acupressure can help as well. Endo excision surgery
is always part of the conversation and requires an expert to minimize the risk of multiple repeat
surgeries.
Lifestyle Modifications:
a. Regular Exercise: Engaging in regular exercise can improve energy levels and reduce fatigue.
It might be counter-intuitive to go out and exercise if you are already feeling beat, it works.
Even low-impact activities like walking, swimming, or practicing yoga can have a positive
impact. Start with light exercises and gradually increase intensity based on your comfort level.
Consult with a trainer or a physical therapist to determine the best exercise plan for you.
b. Balanced Diet: A well-balanced anti-inflammatory antioxidant diet plays a crucial role in
managing fatigue and supporting overall health. Incorporate a variety of fruits, vegetables,
whole grains (whole food plant-based diet), and lean proteins into your meals. These provide
essential nutrients which work together, including iron and other vitamins, which can help
combat anemia-related fatigue. Limiting processed foods, sugary snacks, and caffeine can also
promote more stable energy levels throughout the day. Given that endo is inflammatory and
the damage that is caused is based on reactive oxygen species oxidation, it is critical to keep
inflammation low and anti-oxidation high. Your body is a very complex laboratory which also
works like a symphony orchestra when tuned properly. It needs the right fuel, and an expert
nutritional “conductor” can help select and tune up the right plan for you.
c. Adequate Hydration: Drinking enough water throughout the day is important for maintaining
optimal energy levels. Dehydration can exacerbate fatigue, so aim to consume at least eight
glasses of water daily. Carry a refillable water bottle with you as a reminder to stay hydrated.
This is not directly related to endo but is a forgotten baseline critical need to maintain a slightly
alkaline, antioxidant and anti-inflammatory status.
Stress Management:
a. Mindfulness and Relaxation Techniques: Practicing mindfulness meditation, deep breathing
exercises, or progressive muscle relaxation can help reduce stress and improve energy levels.
Find a quiet and comfortable space and allocate a few minutes each day for relaxation
exercises. There is a lot of choose from including various forms of yoga, Tai Chi, Qigong,
mindfulness, biofeedback techniques like Heart Math, meditation and so on. These days there
are various mobile apps and online resources available to guide you through some these
techniques. But it is important to select something that resonates with you. If you are not “into
it”, it won’t help.
b. Engage in Activities You Enjoy: Participating in activities that bring you joy, and relaxation can
help alleviate stress and combat fatigue. Whether it’s reading, listening to music, taking a warm
bath, or spending time in nature, make time for activities that help you unwind and recharge.
Do something that makes you laugh. This all has psycho-biological proof behind it.
c. Prioritize Self-Care: Self-care is essential in managing fatigue and overall well-being. Set aside
regular time for self-care activities such as taking a bubble bath, getting a massage, practicing
gentle yoga, or indulging in a hobby you love. Remember that self-care looks different for
everyone, so find activities that resonate with you and make them a priority.
Support Networks:
a. Seek Emotional Support: Living with endometriosis is emotionally challenging. Connecting
with others who share similar experiences through support groups or online communities can
provide valuable emotional support, validation, and information. Sharing experiences, seeking
advice, and knowing you are not alone can help in managing fatigue and the overall impact of
endometriosis. Everyone is different and some of the solutions you hear about may not work
for you, but it is good to hear about them. The only prudent caveat might be that if something
sounds too good to be true in this setting, check it out through trusted credible sources and
your endo specialist.
b. Involve Loved Ones: Educate your loved ones about endometriosis and how it affects your
energy levels. Communicate your needs and limitations so that they can offer support and
understanding. Having a strong support system can make a significant difference in managing
fatigue and coping with the challenges of endometriosis.
c. Consider Counseling: If fatigue and the emotional impact of endometriosis are strongly
impacting your mental well-being, consider seeking professional counseling or therapy.
Everyone needs help at some point in their life. A mental health professional can provide
guidance, coping strategies, and a safe space to process your emotions.
Conclusion:
By implementing these management strategies, you can better cope with fatigue and improve
your quality of life. Remember that everyone’s experience with endometriosis is unique, and it
may take time to find the strategies that work best for you. Seek support from an
endometriosis specialist and other practitioners noted above, make lifestyle modifications,
prioritize self-care, and build a strong support network. Ideally, seek out an endo specialist who
is not only a surgeon but is also either trained in integrative holistic care or has a team that
provides these valuable support and treatment options. With the right tools and resources, you
can more effectively manage fatigue and navigate the challenges of living with endometriosis.
References:
Johnson NP, Hummelshoj L; World Endometriosis Society Montpellier Consortium. Consensus
on current management of endometriosis. Hum Reprod. 2013;28(6):1552-1568.
Nnoaham KE, Hummelshoj L, Kennedy SH, et al. World Endometriosis Research Foundation
Women’s Health Symptom Survey Consortium. World Endometriosis Research Foundation
global study of women’s health consortium. Fertil Steril. 2011;96(2):366-373.
Hadfield R, Mardon H, Barlow D, Kennedy S. Delay in the diagnosis of endometriosis: a survey of
women from the USA and the UK. Hum Reprod. 1996;11(4):878-880.
Vercellini P, Vigano’ P, Somigliana E, et al. Endometriosis: pathogenesis and treatment. Nat Rev
Endocrinol. 2014;10(5):261-275.
Ferrero S, Esposito F, Abbamonte LH, et al. Quality of life in women with endometriosis: a
narrative overview. Minerva Ginecol. 2019;71(6):464-478.
Mathias SD, Kuppermann M, Liberman RF, et al. Chronic pelvic pain: prevalence, health-related
quality of life, and economic correlates. Obstet Gynecol. 1996;87(3):321-327.
Hartwell D, Jones K, Hinshaw K, et al. Sleep disturbances and fatigue in women with
endometriosis. Am J Obstet Gynecol. 2019;221(6):638.e1-638.e14.
Vitale SG, La Rosa VL, Rapisarda AMC, et al. Impact of endometriosis on quality of life and
psychological well-being. J Psychosom Obstet Gynaecol. 2017;38(4):317-319.
Giudice LC. Clinical practice. Endometriosis. N Engl J Med. 2010;362(25):2389-2398.
La Rosa VL, De Franciscis P, Barra F, et al. Sleep quality in women with endometriosis: a
systematic review and meta-analysis. J Clin Med. 2020;9(6):1834.
Panir K, Schjenken JE, Robertson SA, et al. Immune interactions in endometriosis. Expert Rev
Clin Immunol. 2019;15(6):649-662.
Koga K, Takamura M, Fujii T, et al. Dysfunction of innate immune system in the development of
endometriosis. Reprod Med Biol. 2018;17(1):49-55.
Agarwal SK, Chapron C, Giudice LC, et al. Clinical diagnosis of endometriosis: a call to action. Am
J Obstet Gynecol. 2019;220(4):354.e1-354.e12.

The Different Tests Used to Diagnose Endometriosis
Endometriosis is a common condition affecting an estimated 10% of women in the United States. Unfortunately, it can be tricky to diagnose, and no single test can definitively confirm it. To diagnose endometriosis, doctors must use a combination of tests. This blog post will discuss the different tests used for diagnosing endometriosis.
History and Physical Exam
The first step in diagnosing endometriosis is taking a history and a physical exam. During this exam, your doctor will assess your abdomen and pelvis for any signs of swelling or tenderness. They may also order blood work to check hormone levels and screen for other conditions with similar symptoms.
Can you see endometriosis on blood test?
Imaging Tests
Your doctor may also order imaging tests such as an ultrasound or MRI (magnetic resonance imaging) scan to better look at your reproductive organs and rule out any other possible causes of your symptoms. Ultrasounds use sound waves to create images of internal organs. MRIs use magnetic fields to produce detailed images of soft tissue structures like the uterus and ovaries.
Laparoscopy
Finally, if all other tests come back inconclusive or your doctor suspects endometriosis due to its similarity with other conditions, they may recommend a laparoscopy. This procedure involves inserting a tiny camera into the abdomen through small incisions near the navel area. This tiny camera allows them to look at the pelvic area better and take samples for further testing if necessary. Laparoscopies are usually done under general anesthesia, so you will not feel anything during the procedure.
Endometriosis can be hard to diagnose because its symptoms are often very similar to other conditions, such as period discomfort, ovarian cysts, or pelvic inflammatory disease. If you think you have endometriosis, you must talk to your doctor as soon as possible so they can determine what type of testing is right for you and how best to treat it. Working with the right healthcare provider ensures you receive the best care possible for managing your condition and improving your overall quality of life.

Endometriosis Surgery Risks
Endometriosis is a condition that affects millions of women around the world. Endometriosis occurs when tissue similar to the tissue found in the uterus grows outside the uterus. This can create intense pain and other health complications, such as infertility. While surgery may be an option for some, it is essential to understand the risks associated with endometriosis surgery before making a decision.
Types of Surgery for Endometriosis
Several types of surgeries exist to treat endometriosis, including minimally invasive (laparoscopy or robotics) and open surgery (laparotomy.) Minimally invasive surgery typically involves making small incisions in the abdomen so that a camera can be inserted into the body to view abnormal endometriosis growths or lesions. Laparotomy involves a larger incision and allows for more extensive examination and treatment. Almost all top endometriosis surgeons worldwide prefer minimally invasive surgery vs. open surgery.
Risks Associated With Endometriosis Surgery
As with any surgery, there are risks associated with endometriosis surgery. These include bleeding, infection, and nerve damage due to surgery or anesthesia during the procedure. During surgical procedures, there is also a risk of harm to surrounding organs such as the bladder or bowels. Additionally, there is a risk that a surgeon will not remove all of the endometriosis tissue during surgery. This incomplete removal could lead to recurrent symptoms or disease if not appropriately addressed by your doctor post-surgery.
Other Treatment Options for Endometriosis
Suppose you are concerned about undergoing surgery for your endometriosis. In that case, other treatment options are available such as hormone therapy or medications used to reduce pain and inflammation caused by endometrial growths or lesions. Additionally, lifestyle changes such as exercise and diet might help reduce endometriosis’s associated symptoms without requiring surgery. Speak with your doctor about other options that may work best for you before deciding on any procedure related to your endometriosis diagnosis.
Find the best endometriosis specialists around the world!
Featured specialists:

Why was iCareBetter built?
A message from Dr. Saeid Gholami, the founder and CEO at iCareBetter:
The story behind the movement
When I used to practice as a primary care doctor, I saw patients’ struggles to find doctors that could do proper endometriosis surgery. Endometriosis patients often came back to our clinic month after month without change in their pain and suffering. Many patients had multiple failed surgeries. That was because almost all gynecologists claimed expertise in endometriosis surgery. Unfortunately, patients could not differentiate truly skilled gynecologists from others for treating endometriosis. One specific patient that I still think of after a decade was a thirty-five years old lady with rectal bleeding during her periods. I recall her coming back every month until everyone believed she was seeking attention. And no one could help her. We tried hard to find endometriosis surgeons for the patients, but no doctor would be able to show enough knowledge and expertise to earn our trust. Some of them claimed endometriosis expertise, but after a couple of questions, we realized that they could not manage the complexity of this disease.
Someone needs to stand up and build a solution when there is a problem. That is how the world has improved since the beginning of humanity. And it was our turn to make something to enhance the world of endometriosis patients. We created iCareBetter to help patients find doctors who possess the knowledge and surgical skills needed for endometriosis treatment. iCareBetter makes the search for endometriosis doctors much more effortless and removes the randomness of finding an endometriosis specialist. By having a platform of peer-vetted endometriosis surgeons, patients can focus on finding a doctor that will match their criteria and personal needs. Criteria such as location, cost, team, and areas of expertise can define a patient’s path to recovery. And patients do not have to worry about the doctor’s basic understanding, empathy, and skills of endometriosis care.
Searching for an endometriosis surgeon is very hard. Most of the time, you have no idea about their surgical skills and whether they will be able to treat your case. iCareBetter evaluates gynecology surgeons for their skills in managing different types and locations of endometriosis. Their surgical expertise is peer vetted, so their ability to do safe surgery. We bring endometriosis specialists closer to patients.
What is iCareBetter’s mission?
To help endometriosis patients receive efficient care. To educate patients on endometriosis, to better understand endometriosis and patient’s needs. Patients wait years to receive a diagnosis, are sent to various specialties, and undergo multiple surgeries, and very few people take their pain seriously. iCareBetter mission is to improve endometriosis patients’ lives by providing them with what is needed the most; doctors that can handle each individual’s unique case.
Who is behind iCareBetter?
I, Dr. Saeid Gholami, am the founder of iCareBetter. I have training as an MD, MBA, and MS in Digital Technology. My training is not in OBGYN, and at the moment, I do not provide care to patients. I founded iCareBetter with my financial resources and then had some family and friends invest in the company to support us. None of the investors are related to the current doctors on the website. And none of the doctors on the website have any ownership or leadership position in the company.
Last words
Like every other life-changing initiative, ours started with a personal story and someone who wanted to make a change. My personal goal has been to improve patients’ lives at the minimum cost for them. And we are just at the beginning of the road. There are many patients with endometriosis who need help. And we have several problems to solve for the patients and the community. Nothing will stop us as long as endometriosis patients use iCareBetter to find hope and care for their debilitating pain and suffering.

What Are The Cost Drivers For Running iCareBetter?
From the beginning of iCareBetter, money has always been questioned. Some think iCareBetter should offer services for free to providers because it costs nothing. But there is a high administration cost for running iCareBetter. The charges come from educating patients and providers about endometriosis and quality of care, maintaining and improving the website, and responding to patients’ and providers’ requests and questions. I am going to share our costs with you in this article.
The costs for operating iCareBetter:
Education about endometriosis and the importance of expert provider
It takes an average of 10 years for a person with endometriosis to get a proper diagnosis. Then several years go by, trying various hormones, artificial menopause, and suboptimal surgeries. After many years and multiple failed treatments, a patient might find an expert who understands endometriosis and how to treat it. We at iCareBetter want to cut that time to less than a year and help patients connect with the expert endometriosis provider as soon as possible. Achieving this goal requires extraordinary efforts in educating the public, patients, and providers. Therefore, we are responsible for making educational content and distributing it on the internet. Content creation and distribution are crucial for raising awareness about endometriosis, the importance of skilled surgery, and fighting misinformation. And it costs money and takes significant effort to create and distribute good educational content about endometriosis.
Reviewing doctors’ applications
iCareBetter takes a significant financial loss on each application; please continue reading for more explanation. After we receive an application with three full surgical videos (mostly between 2-4 hours long), our team has to de-identify all documents and prepare the videos and questionnaire for reviewers. It takes 5-10 hours per application, costing us about $500 on average to prepare the application for review. Then we send the videos and the rest of the applications to reviewers and follow up with them multiple times to submit their reviews. After the reviewers send their reviews, they get compensated for their time. Compensating the reviewers cost us, on average, $350 per application. Therefore on each application, we spend $850 and only charge $400. Consequently, we lose $450 on reviewing each application.
Website maintenance, APIs, and optimization
iCareBetter has an online website core to its services to patients and providers. Providers use the website to apply for vetting. Patients use search engines and many other features on the website to find doctors and learn about endometriosis. Almost all of these features are paid plugins, apps, or APIs. Moreover, there is a sophisticated web developing team behind iCareBetter to deliver the results to our community. Keeping a high-quality website that serves patients and providers with high standards is costly.
Answering questions from patients and providers
Every day our team receives many questions and inquiries from patients, advocates, and providers. It is our responsibility to answer them. Here are some examples:
- Patients:
“Do you have a doctor in region X?”
“Does doctor Y accept new patients?”
“I can not get someone from Dr. Y’s office to answer me, has their phone number changed?”
“Why does the link to this article is broken?”
- Doctors:
“How can I join the platform?”
“I am changing my office location; please update my info.”
“I want to apply for more specialized surgery areas. How can I do that?”
Every question we receive from a patient or a doctor is our top priority. These questions can define the care plan or the surgery outcome for one or more patients. So we are committed to answering these questions. And answering questions needs the time and focus of a reliable person. And this is another layer of costs added.
Final words
The list of costs does not stop here, but I hope you have seen enough information to justify our desire to make money to keep iCareBetter alive. It costs to run a website that aims to be patient-centric, uplifts the community, and brings transparency to the endometriosis community for a better patient outcome.
Please let us know what you think about this matter.

Endometriosis And Menopause: Everything You Need To Know
If you’ve been told that endometriosis goes away after menopause, this may not be the case. So, this may not be a great strategy if you’re trying to “wait out” endo through perimenopause and into menopause.
It is reasonable to think that chronic conditions of your female reproductive organs, like endo, might also go away when you stop having periods. Here’s a look at how endo may or may not change after menopause, based on what we know about molecular biology and hormonal changes as you get older.
This article will cover:
1- Does menopause cure endometriosis?
2- Endometriosis management after menopause
3- Endometriosis after menopause: The molecular biology
4- Endometriosis Symptoms after menopause
5- Endometriosis-molecular level
6- Estrogen replacement after menopause with endo: is it safe?
7- How about compounded natural or bioidentical hormones?
8- How about plant-based phytoestrogens?
9- When is surgery an option for peri and post-menopause endometriosis?
Does menopause cure endometriosis?
Natural menopause does not occur overnight and it might take years before estrogen levels from the ovaries become negligible. Active growth of endo may decrease at this point but, given other estrogen sources discussed in this article and internal molecular factors, it may not stop. So, trying to wait out endometriosis until menopause is final may give it another 5 years or more to grow and cause problems. An active treatment strategy to address endo that persists into peri-menopausal years might limit the damage and lead to better results.
Endometriosis management after menopause
After menopause, the management of endometriosis may become more difficult because by this point in life endo may have been present for decades, even if previously removed partially once or twice by surgery. At this point symptoms may be due to endo as well as scarring and fibrosis, which is part of the body’s normal healing process. The associated problem is that fibrosis and scar does not respond to any medical therapy. This, in turn, means that surgery is the main, if not the only, option for treatment after menopause in many cases. Of course, everyone is different and pelvic floor therapy and supportive care are also in the mix.
Endometriosis after menopause: The molecular biology
Endometriosis cells and tissue look very similar to the normal uterine endometrial lining. Both are stimulated to grow and both try to shed monthly under cycling hormonal influence. During a menstrual period, endometrial tissue has the ability to shed and exit via the cervix and vagina. Unfortunately, the similar-looking endometriosis tissue has no way to exit the body and gets trapped, causing inflammation, scarring, and pain.
Uterine endometrial tissue needs the hormone estrogen to grow, and usually, but not always, so does endometriosis. When you go through menopause naturally, your ovaries produce less estrogen. This causes symptoms such as hot flashes and night sweats. But the commonly held belief is that endometriosis may improve, or even go away, with the reduction in estrogen production by ovaries. We now understand why this does not happen in all women through molecular biology research.
Endometriosis at a molecular level
While many factors control endo growth, including immunologic ones, exploring the molecular biology of hormones in menopause suggests that hormones can undoubtedly be a big part of the picture. In addition to the usual conversation about external estrogen from ovaries, which decreases towards menopause, intra-cellular production of estrogens also plays a critical role in the pathogenesis of endometriosis. This increases in peri and postmenopausal women who have persistent active endometriosis lesions.
Without getting lost in the details of hormone enzyme activation and deactivation, which results from genetic switches getting turned on and off, suffice to say that research supports the following. There is local estrogen production in endometriosis cells, which activates other feedback loops at the cellular level. This activation of loops causes even more estrogen production and resistance to progesterone (the balancing hormone). This affects macrophages and pro-inflammatory cytokines (e.g., TNF-α and IL-1β), which sets off another chain reaction. These also create molecular signals (e.g., VEGF) that stimulate microscopic blood vessel formation to feed the endo cells and activate anti-apoptotic genes (e.g., Bcl-2), creating more endo growth. This leads to local tissue trauma, nerve stimulation, fibrosis, and pain.
Endometriosis Symptoms after menopause
What happens to your symptoms could depend on the severity of your symptoms before menopause and hormonal and inflammatory balance. If your endometriosis is mild, it may get better with menopause. If your disease is severe, symptoms are more apt to persist. Why? Several reasons: scarring and fibrosis that only gets worse and a molecularly more active endo type that persists and keeps growing after menopause. It is currently impossible to predict what type you may have and what molecular signals are in play in any given individual.
If your symptoms don’t improve even after you’ve stopped having menstrual cycles, surgery may be the best option for you. Surgery to remove all of your endometriosis and fibrosis will often be more effective than medication. Years of growth and fibrosis can lead to more local nerve noxious stimulation, and the first step is to remove this. Medications, including natural enzyme supplements, will not dissolve scars, and any persistent active endo is also more difficult to control after menopause. Many other molecular signaling paths are operational, making it harder to determine the best target to block abnormal effects. All the various inter and intracellular signaling forms are under intense research.
Types of Endometriosis Pain & Natural, Medical & Surgical Treatment
Estrogen replacement after menopause with endo: is it safe?
All of the above concerns how, when, and where estrogen is produced. But how this affects cells in your body, including endometriosis cells, depends on the presence or absence of estrogen receptors. You can think of the estrogen molecules as little keys which float through your bloodstream and tissues (or locally produced on or near the endo cells), and the estrogen receptors are like little locks present in and on the cells. The two have to connect, or the key has to fit the lock to produce a molecular signaling event at the cellular level. One of these signaling events is whether or not to stimulate growth.
There are different estrogen receptors called estrogen receptor alpha (ERα) and beta (ERβ). In some estrogen-sensitive tissues, like the breast or uterus, these two types can be variably pro-growth, and in others, they can be inhibitory. In addition, there is a progesterone receptor (PR) that binds progesterone in the same fashion via a lock and key mechanism. Endometriosis cells have overexpression of mainly ERβ and underexpression of PR. This imbalanced expression of receptors leads to progesterone resistance and amplification of the growth signal provided by estrogen. This only scratches the surface of incredible complexity, but hopefully, you get the idea.
In general, to alleviate postmenopausal hot flashes, depending on whether you have a uterus or not after menopause, estrogen alone is often prescribed (no uterus) or combined with progesterone (the uterus is in). This is because progesterone balances the effect of estrogen on the uterus and reduces the risk of endometrial cancer due to estrogen-induced overgrowth of the endometrium.
The exact ratio of alpha (ERα) and beta (ERβ) and the amount of PR present can be variable in endometriosis. It can change over time into menopause or after surgically induced menopause due to early removal of the ovaries. So, theoretically, any hormonal replacement will affect endo cells to some degree and may amplify the degree to which local estrogen is produced, as discussed above. The degree to which this happens and evolves is not predictable from person to person.
Where does that leave us? It comes down to risk vs. benefit discussion because a reasonable amount of estrogen replacement after menopause can help the quality of life and bone health. Studies have not proven whether or not this can activate or amplify endometriosis growth after menopause.
How about compounded natural or bioidentical hormones?
The long answer to this is very complex and depends highly on the quality of these hormones and whether or not the dosages are correctly mixed and, if one were to use combinations that are applied to the skin, degree of absorption, and much more. The problem with synthetic vs. natural arguments notwithstanding, the effect on the very variable and unpredictable receptor signaling described above remains theoretically unchanged. There is also a higher risk of inadvertently taking a higher dose since many are locally prepared and thus subject to less regulation. Get a highly qualified opinion and possibly several opinions and do a lot of due diligence personal research before going this route.
How about plant-based phytoestrogens?
Plant estrogens, otherwise known as phytoestrogens, uniquely attach to estrogen receptors. They can bind to either type of estrogen receptor but preferentially bind to ERβ. In doing so, they take up space and block the ability of regular estrogen to bind to the receptor. In terms of helping menopausal symptoms, estrogen receptors also exist on blood vessels, and the binding of phytoestrogens helps stabilize the blood vessels, reducing hot flashes. The effect is less than that caused by regular estrogen but is helpful in many women. At the same time, there can be a relative blockade at the endometriosis cell level. Again, given the differences regarding receptors and signaling effects between individuals, this is not 100% predictable but can be a win-win nonetheless.
Along the natural, integrative line of thought, a couple of corollary strategies is how the estrobolome and seaweed figure into this puzzle. First, the estrobolome is part of your gut microbiome that can metabolize the excess estrogen in your body and eliminate it. This includes the excess estrogen produced by ovaries, local estrogen created at the cell level, and the toxin type of estrogens called xenoestrogens. Keeping your microbiome healthy and happy with probiotic supplements or fermented foods is the action time. Second, we know that seaweed can predictably reduce circulating estrogen. This can retard any hormonal influence on the regrowth of endo, especially if the bulk of any disease is removed surgically.
Read more: Postmenopausal Malignant Transformation of Endometriosis
When is surgery an option for peri and post-menopause endometriosis?
If symptomatic endo is suspected as one gets closer to menopause, it merits discussion about expert removal of as much as possible via excision surgery. Ideally, a surgeon should remove all visible lesions in this case. Even if undetectable microscopic implants are left behind, removal of pain-producing scars/fibrosis and the bulk of any active endo limits the number of cells that might grow back over time, whether or not hormonal replacement is taken.
There is one more reason for considering surgical removal. If you have a family history of cancer or have active endo as you enter menopause, given the known molecular abnormality overlap between endo and cancer (e.g., ARID1A), the risk of malignant degeneration may be higher. This is a highly individualized situation, but some can be critical to balancing the surgical risks vs. potential benefits.
Surgical concerns
So, with all of the above in mind, is there a reason NOT to have surgery to remove endo, especially if you have symptoms as you get close to or enter menopause? Of course! Even minimally invasive surgery is not risk-free, and the risks can increase as you get older. Scarring and fibrosis from advanced endometriosis possibly increased from prior surgeries, leading to complications and damage to organs, including the bowel. For this reason, selecting an über expert surgeon at that point in life is crucial.
An über expert surgeon can handle pretty much any possible finding in the pelvis and abdomen. Moreover, they can address oncology risk concerns if you are at higher risk with a family history. This means that the right surgery for cancer would be performed if cancer were suspected or found during surgery. But short of cancer, this surgeon needs to be able to handle small bowel, rectal, bladder, ureteral involvement, even disease in the upper abdomen and diaphragm. Deep infiltrating endometriosis implants are more common if they have been allowed to grow over the years. This full-spectrum surgeon might be a gynecologic oncologist who has experience in endo excision. But even they may need a cardiothoracic surgeon if endo involves the chest cavity. Cardiothoracic surgery is an entirely separate specialty of surgery. Alternatively, a minimally invasive surgery team including an endo excision trained GYN surgeon, a urologist, a general surgeon, and possibly more would need to be available. It can be a logistic challenge to gather such a team, but this is usually possible in centers that specialize in endometriosis surgery.
Join endometriosis forum and discover endometriosis stories
Read on endometriosis forum: What are the long term side effects of lupron?
Get in touch with Dr. Steve Vasilev
More articles from Dr. Steve Vasilev:
Understanding the Connection between Endometriosis and Cancer
How to tell the difference between endometriosis and ovarian cancer
What would happen to the signs and symptoms of endometriosis after menopause?
The author of this article, Dr. Steven Vasilev MD is a fellowship-trained, triple board-certified integrative gynecologic oncologist specializing in complex pelvic robotic surgery. He focuses on advanced & reoparative endometriosis excision and molecular integrative healing, especially as it applies to women of older reproductive age and in menopause.

What Does Endometriosis Feel Like? Types of Endometriosis Pain & Natural, Medical, and Surgical Treatment
Learn How People Feel Endometriosis Pain in Different Locations
Endometriosis pain is hard to explain to people who have never experienced it. Why? For many reasons. One of them is that each patient with endometriosis (endo) will endure their specific type of pain. Some patients experience pain during sex, while others may have pain after sex. Another example is that some patients have endometriosis pain in the lower back, and others sometimes have it all over the back and even the hips!
Want to know how to deal with endo pain? In this article, we will review the various types of endo pains, their locations, characteristics, and treatments.
Get the pdf Version of this article
Read more: How Do I Know If I Have Endometriosis? Endometriosis Signs
Endometriosis signs and Symptoms
Table of Contents
1- Where is Endometriosis Pain Felt?
2- What Does Endometriosis Pain Feel Like?
3- Why Do Endometriosis Patients Experience Different Types of Pain?
4- Different Types of Pain and Their Origins
5- How Does Endometriosis Pain Differ From Menstrual Pain?
6- Endometriosis Pain Treatment Options
7- Do You Have Endometriosis Pain?
Where is Endometriosis Pain Felt?
Unfortunately, it can be difficult to distinguish exactly where endo pain is coming from. This difficulty is because endometriosis pain can feel non-specific and may affect various parts of your body at different times. Can endometriosis cause back pain? Yes. Some patients experience endometriosis rectal pain or generalized pelvic pain – while other people with endo might have pain in their chest, back, or even hips. To that end, pain location usually results from where the endometriosis tissues reside inside the body.
What Does Endometriosis Pain Feel Like?
It can be tough to explain what endometriosis pain feels like. This is especially true when a woman tries to explain this pain to a guy. For one, most women complain that endo pain feels like very excruciating period cramps. However, unlike period cramps, many patients with endometriosis report that this sensation is not limited to just the area surrounding the uterus. Patients with endometriosis often experience:
- Pelvic pain
- Abdominal pain
- Pain during bowel movements
- Sciatic pain
- Pain during or after intercourse
- Leg pain
- Rectal pain
- Pain with urination
Menstruation can exaggerate these types of endo pains. But many patients experience these symptoms outside their period.
Why Do Endometriosis Patients Experience Different Types of Pain?
Endometriosis is a chronic inflammatory condition that affects each patient differently. Why? For the most part, the type of endometriosis pain you experience will depend on the location of the lesions and the progression of the disease. Furthermore, feeling the pain in one part of the body doesn’t mean that it originated from that body part. It is because pain often radiates to other parts of the body.
Different Types of Pain and Their Origins
Pelvic Pain
Endometriosis is when tissue similar to the endometrium grows outside the uterus. In most cases, these tissues grow in areas close to the uterus, i.e., your pelvis, reproductive organs, and abdomen.
Meg Connolly, diagnosed at the age of 23 with endometriosis, said that:
“Endometriosis causes a pain that’s very difficult to describe. It’s more than just ‘bad cramps’ — it’s the type of pain that even over-the-counter (OTC) medicine won’t resolve.”
Back Pain
Can you have back pain with endometriosis? Absolutely. The endometrial growths can stick to the front of your pelvic cavity or your lower back. Endo back pain presents deep within the body. This condition can result in sciatic pain.
Is the back pain you experience caused by endometriosis? Back pain is a common ailment among patients of all demographics. However, endometriosis back pain stems from deep inside the body. Furthermore, another indication your back pain might be from endometriosis is that it won’t improve by seeing a chiropractor or changing your posture.
Leg Pain
Leg pain can result from endometriosis when the lesions grow near or on the sciatic nerve. Patients describe endometriosis leg pain as the following:
- A dull throb
- A sharp stabbing sensation
- A sudden spasm that feels similar to a leg cramp
Patients with severe leg pain from endometriosis may have difficulty walking comfortably or standing up quickly.
Pain During Intercourse
Endometriosis tissue and scars around it can result in a painful nodule to touch. These nodules may occur in several places, including:
- Cervix
- Uterus
- Pelvic cavity
- Rectovaginal septum
The presence of these nodules may lead to sharp pain felt in the vaginal or abdominal areas during sexual intercourse or immediately after.
Endometriosis Painful Bowel Movements
Endometriosis tissue can grow in the bowel wall or the space between your rectum and vagina. This abnormal growth results in these symptoms:
- Diarrhea
- Difficulty passing urine
- Irritable bowel syndrome (IBS)
- Painful bowel movements
Bowel pain can be sharp and consistent. Moreover, pain from the bowels can worsen if combined with poor lifestyle habits, such as diets high in greasy processed foods.
How Does Endometriosis Pain Differ From Menstrual Pain?
Endo pain is different from normal menstrual pain. But also pain from this disorder typically feels different for each person who experiences it. However, there are a few things that set endo pain apart from menstrual pain, including:
- Endo pain is typically chronic, lasting for more than six months.
- The pain happens several times in the month, before and during your menstrual cycle.
- Frequently the pain is severe. As a result of this severity, over-the-counter pain relievers typically do not provide relief.
- Endometriosis pain is often consistent. Therefore patients can usually recognize it when the symptoms come on.
Endometriosis Pain Treatment Options
Pain relief for endometriosis can be natural, medical, or surgical. Learn more about these three types below. But it is important to know that natural and medical solutions are mostly temporary relievers from this list, and surgery is considered the most permanent treatment.
*Note: iCareBetter is not endorsing any of the treatments but instead provides a list of what helps other patients and routinely performed treatments.
Natural Treatment for Endometriosis Pain:
- Rest
- Turmeric
- Light exercise
- Castor oil
- Ginger tea
- Dietary changes
- Pelvic massage
- Herbal supplements
- A heating pad or hot water bottle
Medical Treatment:
- OTC pain medications
- Physical therapy
- Prescription pain medication
- Mental health provider that specializes in pain management
- Some physicians prescribe hormonal therapy, such as contraceptives. However, new research shows this treatment for endometriosis pain is not a one-size-fits-all solution. A recent study out of Yale came to the following conclusion:
- “PR (progesterone receptor) status is strongly associated with response to progesterone-based therapy. Receptor status in endometriosis could be used to tailor hormonal-based regimens after surgery and negate trialing progestin-based therapy to determine resistance. Ascertainment of PR status may allow for a novel, targeted, precision-based approach to treating endometriosis.”
Surgical Treatment
- Minimally Invasive Surgery for endometriosis is a way to remove endometriosis lesions permanently and help with the pain. In this procedure, the surgeon cuts small incisions into the abdomen and inserts a thin tube with a viewing light (a scope) into the body. Then this scope can visualize lesions, take tissues samples, and remove scarring.
- A laparotomy is a surgical procedure where the surgeon cuts and opens the abdomen and does not use thin tubes. However, laparotomy is more extensive than minimally invasive surgery and is not often performed in modern medicine due to the risk of complications.
Read more: How to Find an Endometriosis Specialist for Diagnosis, Treatment, & Surgery
Do You Have Endometriosis Pain?
What type of endo pain do you have? And how would you describe it? If you want to find an experienced endometriosis specialist or a different kind of endo provider near you, you can do so on our platform, iCareBetter.

How Do Endo Fertility Issues Impact the Mental Health of a Person?
Endometriosis (endo) can cause many issues. Endometriosis patients may have difficulty becoming pregnant or maintaining a full-term pregnancy. Up to 70% of women with endometriosis get pregnant without medical treatment. However, 30 to 50% of patients with endo experience fertility issues and may need endometriosis fertility treatments or surgery. Up to 50% of all women with infertility have endometriosis. According to the abstract in a study published in the International Journal of Women’s Health:
“The most common clinical signs of endometriosis are menstrual irregularities, chronic pelvic pain (CPP), dysmenorrhea, dyspareunia and infertility. Symptoms of endometriosis often affect psychological and social functioning of patients. For this reason, endometriosis is considered as a disabling condition that may significantly compromise social relationships, sexuality and mental health.”
Read More: How Do Endo Fertility Issues Impact the Mental Health of a Person?
Why Are Women Impacted Emotionally By Reproductive Disorders?
A plethora of reasons exists as to why women can experience deep emotional impact by a diagnosis of a reproductive disorder or a condition that could cause issues with fertility. Some women already worry about getting pregnant anyway, so an endometriosis diagnosis surely doesn’t help. Here’s a shortlist of some reasons reproductive issues can affect the emotional health of women with endometriosis:
- Pressure to conceive right away
- Worries about each stage of the pregnancy, from implantation to delivery
- Pressured to have a child, even if the person is unsure or not ready
- Possible medical interventions, such as IVF
- Stress and emotional drainage that can result from endometriosis fertility treatments
- Possible laparoscopy endometriosis surgery
Multiple studies demonstrate that a woman’s ability to conceive and bear a child plays a big part in her emotional health and self-esteem. While many women don’t want to have children, a large portion does. But, they might not be ready for a baby when they receive their endometriosis diagnosis. According to a study out of the Iranian Journal of Reproductive Medicine:
“While infertility is not a disease, it and its treatment can affect all aspects of people’s lives, which can cause various psychological-emotional disorders or consequences including turmoil, frustration, depression, anxiety, hopelessness, guilt, and feelings of worthlessness in life.”
Read More: How Does Endometriosis Cause Infertility?
Endometriosis Patients with Fertility Issues Need Emotional Support
Most endometriosis patients with fertility issues benefit by having a mental health provider as part of their multidisciplinary team.
Endometriosis impacts many facets of a person’s life. A recent study concluded that:
“Furthermore, there is an urgent need to develop and evaluate interventions for supporting women and partners living with this chronic and often debilitating condition.”
All Endometriosis Patients Could Benefit From Emotional Support
Many endometriosis patients with fertility issues express no desire to have children. Therefore, some women are unaffected by infertility that might arise from endo. However, it’s essential to keep these women in mind because their feelings matter, too. Perhaps some did not want to have kids now but were hoping to someday in the future? Or maybe they are just not with the right person to have children with them?
Whatever the case may be, it’s significant that healthcare providers do not overlook a patient’s emotional needs, even if they say it doesn’t bother them if they cannot have kids. Perhaps a person in this situation may not need as intense emotional support, but they should see a mental health provider have a chance to talk about these feelings and think them through. Some interventions can help one conceive or be ready to conceive even with an endometriosis diagnosis. However, it’s significant to remember that the further the disease has progressed, the more complex it is to treat it to regain fertility. Therefore, when you are unsure if you want to have a baby, it’s still wise to have all the lesions removed as soon as you can and conduct proper follow-up.
Seeking a Mental Health Provider Experienced With Endometriosis
Endometriosis is a complex and often misunderstood disease. Therefore, women who battle this condition daily, especially those with fertility issues, require a mental health professional familiar with this inflammatory disorder.
Endometriosis encompasses many domains of a patient’s life, and fertility issues are not the only things that impact women’s emotional health. When seeking out a professional, it’s critical to find someone familiar with the disease and its emotional impact on patients.
Importance of Friends and Family
In addition to adding a robust mental health provider to your team, it’s also essential that you seek support from your loved ones. Please encourage them to attend appointments with you to have a better understanding of the condition. When the people closest to you can comprehend the emotional roller-coaster accompanying infertility, they will be better prepared to support you emotionally.
When a patient receives a diagnosis such as endometriosis, pain management, and other care items often become the priority. Therefore, it can be easy to overlook the emotional aspect of this condition, especially in someone with fertility issues. This is why it’s essential to do your research and find an experienced endometriosis expert to head up your team.
Do You Have Fertility Issues Caused By Endometriosis?
We want to hear from you. What are your thoughts on the emotional challenges? Do you have a solid mental health provider on your team? Leave your responses in the comments below.

Endometriosis and Pregnancy: Natural, Medical, & Surgical Options
Natural, Medical & Surgical Treatment of Endometriosis Infertility
Endometriosis (endo) is a common condition that affects up to 10% of all women globally. But most people do not realize this condition’s impact on a significant proportion of women. Endometriosis and pregnancy complications are a common coincidence. Up to 50% of women with infertility have endo.
Endometriosis and pregnancy can be problematic for patients. And sometimes, endometriosis treatments are needed to conceive. Keep reading to learn more about fertility options for women with endo.
Read More: How Does Endometriosis Cause Infertility?
Lack of Evidence-Based Research Stalls Treatment Options
Endometriosis is sometimes like the elephant in the room that no one wants to discuss or do enough research. However, that needs to change because endometriosis is often a disabling condition, and people should know about it. Not only does this condition impact the patient’s quality of life, but it also affects the potential for some of these patients to have a family. This situation can affect a marriage, other family members, a partner, etc.
Options for treating women with endometriosis and pregnancy issues can be natural, medical, surgical, or surgery-assisted. Let’s review the latest fertility treatments and courses of action for women affected by endometriosis. First, we will briefly discuss how endometriosis and pregnancy are related.
Can You Get Pregnant with Endometriosis?
Natural
Getting pregnant with endometriosis is not always easy, but it’s a reality for most patients who have the condition and want to conceive. It’s important to emphasize that the body can and still does get pregnant. There are things such as an endometriosis diet that might help. Let’s look at the good numbers. Up to 70%, according to some studies, of women with mild to moderate endometriosis will become pregnant without medical intervention.
Medically-Assisted
Statistics show that about 75% of women with severe endometriosis (stage III/IV) will conceive if they desire. Two-thirds of those pregnancies occurred naturally, and one-third with the help of the endometriosis fertility treatment.
If you have endometriosis and are having troubles getting or maintaining a pregnancy, and you wish to carry full-term, here are some medical options that may interest you:
- Freeze some eggs: Your ovarian reserve of eggs can decline due to endometriosis. Therefore, some endo specialists recommend preserving your eggs in case you wish to conceive later. Just note that this can be an expensive option.
- Superovulation and intrauterine insemination (SO-IUI): If you have normal fallopian tubes, mild endometriosis, and a partner with healthy sperm, this might be the best choice for you.
- Fertility medications: Doctors can prescribe medications to produce up to two or three mature eggs. There are also progestin injections that are often used to help fertility issues.
- Frequent ultrasounds: If a person is trying to get pregnant, they may go in for frequent ultrasounds to identify when the eggs are most mature. At that time, a doctor can insert the partner’s collected sperm.
- In-Vitro Fertilization (IVF): This treatment involves the extraction of the egg and sperm. The egg is fertilized outside the body and then implanted into the uterus.
Endometriosis Surgery For Infertility
Many women with endometriosis do become pregnant without medical assistance. However, studies suggest that endometriosis surgery does help a woman to become pregnant without difficulty.
- Removal of endometriosis tissue: Evidence shows that pregnancy rates improve if the endometriosis tissues are removed surgically.
- Removal of tissue or large endometriosis cysts: Large cysts and tissue accumulation can contribute to infertility. Removing these can help the patient conceive.
- Routine follow-up: Women with endometriosis often have cysts that relapse after treatment. It is crucial to complete follow-up visits and possibly have complementary surgeries down the road.
How Your Stage of Endometriosis Impacts Fertility
A diagnosis of endometriosis is a heavy thing to take in, primarily since it’s known to impact a woman’s reproductive organs. Studies have shown that the extent of endometriosis present during laparoscopy correlates with fertility.
Do You Have Concerns About Endometriosis and Fertility?
We want to hear from you. What is your biggest concern about the fertility impact of endometriosis? Or does it concern you at all? Leave your answers in the comments below. If you need medical attention that is not emergent, be sure to find a vetted endometriosis specialist who is familiar with the disease and modern treatments.

Endometriosis and Fertility: Statistics, Facts, & Fiction
Debunking the Myths Surrounding Endometriosis and Reproduction
Disinformation about endometriosis and how it can impact reproduction is thick. As a matter of fact, not just endometriosis and fertility, the entire disorder is shrouded in junk information, and so it often goes misunderstood and mistreated. To learn more on this topic, read our previous article, titled: “Endometriosis Facts and Myths: Dispelling the Misconceptions.”
Does endometriosis cause infertility? In some cases, yes. However, in most cases, women with endometriosis can and do get pregnant without any medical assistance or intervention of any kind. There is still a myth that if you become pregnant, that can manage the endometriosis (endo) symptoms and even help resolve disease progression.
This statement couldn’t be further from the truth, and it’s an example of a widespread myth about endometriosis and fertility. Furthermore, this school of thought can put additional pressure on women with endometriosis to get pregnant as quickly as possible once they get a diagnosis. As you can imagine, this dangerous misinformation can alter their expectations in terms of treatment for fertility and their outlook on endometriosis in general.
So, Can You Get Pregnant If You Have Endometriosis?
The real truth is that the connection between endometriosis and reproduction is complex. Can you get pregnant if you have endometriosis? Yes, many people can and do. However, having the right endometriosis specialist to help you along the way can make all the difference in your journey. Click here to learn more about finding vetted endo specialists near you. In this article, we will review the disease and lay out the facts regarding endometriosis and fertility.
What is Endometriosis?
Endometriosis is an inflammatory disorder in which tissue similar to the uterus lining grows in places outside the uterus. Often these growths happen on the surface of the uterus, ovaries, fallopian tubes, or other organs within the pelvic cavity – such as the bladder or bowel. In some cases, these endometriosis growths have occurred in distant organs.
Endo growths can cause pain, scarring, and sometimes infertility. Because this tissue is similar to the uterine lining, it also bleeds and sheds once a month during hormonal changes. Typically in the uterus, this period tissue and blood have a means of escaping through the vagina. However, this blood and tissue often accumulate inside the body with endometriosis and causes inflammation and pain. As one can imagine, over time, scar tissue growths with subsequent menstrual cycles develop. Eventually, this scar tissue can fuse organs, immobilize organs, and even damage the fallopian tubes.
Alarming Statistics About Endometriosis & Fertility
- Endometriosis is widespread, affecting between six and ten percent of the general female population. That’s more than 170 million worldwide.
- In patients with pelvic pain, infertility, or both, endometriosis frequency is higher – between 35 percent to 50 percent.
- Between 25 percent to 50 percent of infertile women have endometriosis.
- Between 30 percent to 50 percent of women with endometriosis are infertile.
- Endometriosis affects approximately the same number of women around the world that have diabetes.
- The cost of endometriosis in the US is between $86 Bn – $116 Bn.
- It takes, on average, eight years from the onset of symptoms for a patient to get a diagnosis. This can impact all patients, but especially those of who wish to keep their fertility intact.
Endometriosis Facts About Fertility and Reproduction
- There are ways to get pregnant with endometriosis.
- Hormonal therapy does not cure endo.
- Endometriosis is related to your menstrual cycle and hormonal changes within your body.
- Endometriosis tissue can be removed during laparoscopy. Depending on the location of the growths and the extent of damage, this can sometimes restore fertility.
- There is a type of endometriosis that can cause cancerous lesions, typically dark chocolate brown.
- The causes are uncertain, and there is no “cure” for endometriosis.
- Genes seem to play a role in the occurrence of endo.
Myths About Endometriosis and Fertility
- Pregnancy is not a cure or a way to relieve symptoms of endometriosis. Women should not be pressured or encouraged to get pregnant to help with endometriosis and fertility or alleviate pain or other symptoms. While some women experience less endo pain and symptoms during their period, that does not mean it works the same for all women.
- Do not believe any physician that tells you a hysterectomy is the “gold standard” treatment for endometriosis. As mentioned above, there is no “cure” for endometriosis. Until a specialist is inside the body and can view the number and the placement of the endometriosis lesions, they cannot decide whether a hysterectomy would even solve the problems. Also, some women might make themselves infertile (whether they mind or not, it is an emotional part of this disorder) by having a hysterectomy done that was never needed.
- You do not need to have a major medical procedure to get an endometriosis diagnosis or remove some growths and lesions. With modern equipment, skilled specialists, and advanced technology (often robotic surgical equipment), you can have endometriosis diagnosis and treatment with laparoscopy. This type of procedure is minimally invasive and only leaves behind a few puncture wounds.
- Abortion does not cause endometriosis.
- Endometriosis does not cause ovarian cancer. Although a type of endo involves cancerous tumors, this does not mean that having endometriosis makes you more likely to develop cancer.
- The most important myth to bust is that there is no treatment for endometriosis. Just because there is no “cure” for this pelvic inflammatory disorder does not mean there are no treatment options, even when it comes to endometriosis and infertility.
If you have endometriosis, what is the most common thing you have heard regarding endo and reproduction?

Does Endometriosis Cause Infertility? Covering the Basics
Learn More About the Connections Between Endometriosis and Infertility
Endometriosis (endo) diagnosis can be a frightening thing. Very frightening. While this inflammatory condition can be binary or non-binary, women of child-bearing age are prone to issues with reproduction due to endo. So does endometriosis cause infertility? Keep reading as I break down the basics on this topic. I will also discuss the emotional impact on patients.
What is Endometriosis?
Endometriosis is a chronic inflammatory condition. In this disease, endometrium-like lesions (the tissue that lines the uterine walls) grow outside the uterus. These glands or stroma cause chronic inflammatory reactions. Endometriosis tissue can occur on the surface of other body parts in the pelvic cavity and distant organs such as the diaphragm, lung, and heart.
Because these endometrial-like lesions shed blood and tissue, many problems result. Pain is a common symptom because the blood and tissue have no way to leave the body. This pressure can result in unbearable pain and other symptoms. If you would like to learn more about what endometriosis is, check out our previous article.
What Happens When Endometriosis Does Cause Infertility
It can. 25 to 50% of women with infertility have endometriosis, and 30 to 50% of women with endometriosis have infertility. However, it is very encouraging to know that most women with endometriosis can become pregnant.
This statistic is significant. Many younger women with this disorder feel psychological effects due to the possibility of not being able to have kids. Not all patients carry this same sentiment. Growing numbers of people do not want to have children. However, for those who do, these thoughts and emotions about fertility can be devastating. Then, endometriosis patients who do conceive often worry about the pregnancy and subsequent delivery of the baby.
How Endometriosis and Fertility are Connected
The association between endometriosis and infertility is well-established. However, there may be multifactorial reasons why it occurs, including molecular, mechanical, environmental, and genetic causes.
There are some theories to explain infertility in endometriosis. The following are just a few:
- Inflammation leads to the production of chemicals known as cytokines. These cytokines can inhibit the egg and sperm from meeting each other, which makes fertilization more difficult.
- Endometriosis-related scarring and adhesions can block the fallopian tubes or uterus space. This blockage makes it difficult for the sperm to meet the egg and implant in the endometrium.
- Endometriosis lesions on the ovaries can inhibit ovulation and block the release of an egg.
Read More: How Does Endometriosis Cause Infertility?
Other Data on Endometriosis and Reproduction
Studies have also demonstrated that the enzyme, Aromatase may also play a role in endometriosis infertility. There is an abnormally high level of this enzyme in the endometrium and endometriosis lesions in patients with endometriosis. In the uterus, this enzyme may affect both natural endometrial development and its receptivity for the implantation of the fetus.
Progesterone is another hormone that may play a role in implantation failure. Resistance to this enzyme can affect reproduction, as it is necessary for a normal pregnancy. In some studies, progesterone receptors displayed abnormalities and caused dysregulation in the endometrial layer of the uterus in patients with endometriosis. Levels of progesterone should increase with pregnancy, but with endometriosis, this process is delayed and can cause an unopposed estrogen state that cannot sustain fertility.
Endometriosis Infertility Treatment Options
Patients with endometriosis do have a substantial risk of infertility or problems getting pregnant. According to studies, the amount of endometrial-like tissue visible during a laparoscopy correlates with the possibility of future fertility. For this reason, if you have endometriosis and would like to become pregnant, early treatments for endo and fertility are crucial. This is because the stage of endo might progress within time, which increases the risk of infertility.
Laparoscopy: A Common Treatment for Endometriosis
Can endometriosis cause infertility? Yes, in some patients. However, in most cases, endo does not entirely prevent conception. Traditional treatments for endometriosis approached most cases of endo with total hysterectomies. But these approaches are now outdated. New science-based evidence shows that hysterectomies and oophorectomies are not always needed. That is because these surgeries do not often work to remove all the endometriosis tissue.
A skilled endometriosis specialist goes in the pelvic and abdomen with thin tubes and excises the endometrial-like tissue for best surgery results. This surgery often requires OB-GYN surgeons with advanced training in endometriosis treatment. It typically involves advanced surgical equipment, such as laparoscopy, robotics, and AI technology.
Now let’s review the endometriosis treatment options in the context of pregnancy and fertility.
Medical Treatment Options for Endometriosis
- Ovarian suppression, such as hormonal therapies or oral contraceptives, is not recommended for women who wish to conceive. This highly-debated advice gained support from a large study that found no difference in pregnancy rates and live birth rates in patients with endometriosis who took a hormone vs. placebo.
- An endometriosis diet by nutritionists that work on endo can be helpful. The diet can help increase the patient’s likelihood to conceive with endometriosis and maintain that pregnancy to a full-term birth.
- The Guideline Development Group (GDG) does not recommend the prescription of adjunctive hormonal treatment before surgery in infertile women with endo.
Surgical Treatment Options for Endometriosis
- The goals of surgery are to remove all macroscopic endometriosis implants and return the pelvic cavity to normal anatomy. While these are the goals, not all surgical procedures or endometriosis specialists will stop this inflammatory disorder or restore the pelvic cavity to its normal anatomy.
- It’s crucial to weigh the pros and cons of surgical intervention.
- Endometriosis minimal invasive surgery by an expert is the preferred surgical procedure because:
- It causes minimal damage to the tissue.
- It’s assisted with magnification.
- There is a relatively fast recovery time.
- Mostly only a short hospital stay is involved.
How Women with Endometriosis Suffer Emotional Impact
Women who deal with endometriosis reproductive problems may experience a variety of feelings, such as:
- Stress
- Worry
- Grief
- Confusion
- Anger
- Sadness
- Feelings of inadequacy
As mentioned above, over 30% of women with fertility problems have endometriosis. If a woman is already distressed about becoming pregnant, the shock of an endometriosis diagnosis may amplify those emotions.
Furthermore, women with endometriosis may feel further pressure to have kids sooner to increase their likelihood of success. But, that’s not always practical. Some do not have a partner or might not even know if they want to have kids. Perhaps they are with someone who does not wish to or is not ready for kids. They might also be with someone they have not been with for very long, so they are unsure if they want children. Many factors can cause stress on women with endo to try to get pregnant right away.
For those ready and trying to get pregnant, fertility issues caused by endometriosis may also create feelings of frustration, hopelessness, and sadness. These feelings are the reasons why it’s crucial to incorporate a mental health expert as part of your holistic endometriosis treatment team.
Psychological Impact of Fertility Treatment for Endo Patients
Furthermore, a whole new slew of emotions comes with those patients who move on to endometriosis fertility treatment. Excitement. Happiness. Disappointment. Sadness. You and your partner can do these things to help prepare for these possible feelings:
- Prepare and be ready for the emotional journey ahead
- Cope with grief and loss associated with unsuccessful prior attempts or miscarriages
- Develop strategies for coping with the news of other people’s births and pregnancies
- Keep the communication lines between you and your partner open and discuss feelings throughout the entire process
Did endometriosis cause infertility issues for you? How has that impacted your life?

Find Endometriosis Specialists for the Best Possible Outcomes
Why You Need an OB-GYN Who Specializes in Endometriosis
Endometriosis is common (affecting nearly 190 million women worldwide) but poorly understood by many medical professionals. It’s hard to find endometriosis specialists who have completed advanced training. With the proper endo specialist, medical treatment or surgery can lessen your pain, improve your quality of life, and manage complications.
Endometriosis is a chronic pain condition that affects 10-15% of women of reproductive age. It causes painful periods, bleeding between periods, pain during sexual intercourse, and discomfort when passing urine or feces. Despite causing chronic pelvic pain, many medical professionals have a poor understanding of the condition.
In this article, we will look into what endometriosis is and explore how to improve diagnosis, treatment, and outcome factors.
What is Endometriosis?
Endometriosis affects menstruating women and girls and some women post-hysterectomy or post-menopause. The condition also can affect transgender men and non-binary individuals. Endometriosis affects roughly 190 million people worldwide, with immune, genetic and hormonal factors all likely to be at play.
To understand Endometriosis, we first need to understand the endometrium or lining of the uterus.
The Endometrium
A large proportion of the endometrium is stromal cells. Stromal cells regulate cell growth and change during the menstrual cycle.
Endometrial glands line the endometrium. During the menstrual cycle, they widen in response to greater blood flow.
Each cycle, stromal cells, and endometrial glands slough off as part of menstruation.
Endometriosis Lesions
The presence of endometrium-like cells found outside the uterus causes the classic endometriosis symptoms. Discourse exists, but scientists have concluded a genetic basis to the cells’ presence, with endometrium-like cells migrating inappropriately during embryogenesis.
Endometriotic lesions can be in the ovaries, uterine ligaments, fallopian tubes, and pouch of Douglas (the space between the uterus and rectum). In some, lesions are present outside the pelvic cavity. Locations include the bowel, urinary tract wall, diaphragm, lungs, abdomen, and pericardium (the sack around the heart).
The endometrial-like tissue responds to the natural cycle of hormones and also produces some hormones by itself. This tissue has cycles of growth and bleeding.
Whereas menstrual blood in the uterus leaves the body via the vagina, the blood and tissues cannot escape from endometriosis lesions. This trapped cells and tissue leads to the painful processes of inflammation, adhesions, and scarring.
What does it feel like to have Endometriosis?
Although pain is the most common complaint, Endometriosis causes a wide range of symptoms, including:
- Painful periods
- Heavy periods (menorrhagia)
- Vaginal bleeding between periods
- Pain on passing urine or feces
- Bowel symptoms include bloating, constipation, diarrhea, or bleeding from the bowel
- Pain during intercourse
- Tiredness
- Depression
- Infertility.
Social and Emotional Effects
Severe pain can interrupt daily life for many patients. This interruption may include missing school, taking days off work, or being unable to socialize. A study in 2020 found that in over half of women, the pain had reduced their professional, physical, and sexual activity.
Endometriosis is associated with low mood. 15% of women are diagnosed with depression, with an average age at diagnosis of 22.
Infertility
Infertility can be the only symptom of Endometriosis for some women. Around 30-50% of patients cannot get pregnant owing to inflammation, pelvic adhesions, blockage of the fallopian tubes, and changes to the pelvic anatomy.
Other Symptoms
Additional symptoms are dependent on the location of endometriosis lesions. For example, an endometriotic lesion in the lung could cause breathlessness or chest pain. A study of over 2000 patients found that endometriotic nodules caused leg and buttock pain, as well as numbness, similar to sciatic pain.
Misdiagnosis and incorrect management are therefore common for women with symptoms that are not classic to pelvic endometriotic lesions.
Endometriosis Myths
The average delay in the diagnosis of Endometriosis is more than seven years, leading to “unnecessary suffering and reduced quality of life.” This delay leads many people to the internet to conduct their own research before and during diagnosis. However, the internet is awash with myths.
The importance of educating yourself via a reputable source such as iCareBetter cannot be understated.
Find Endometriosis Specialists for Appropriate Diagnosis & Treatment
The widespread misunderstanding of Endometriosis hinders its diagnosis and treatment. The inappropriate investigation, treatment with analgesics, or hormonal suppression do little to manage the cause while delaying diagnosis. Women who felt they were not listened to nor understood by doctors have described frustration, anger, annoyance, and sadness.
Reassuringly, appropriate diagnosis and treatment can lead to significant improvements in pain. This is precisely why it is crucial to find an endometriosis specialist. Only highly specialized surgeons with a comprehensive team can perform a thorough excision to remove endometriotic lesions, including extra-pelvic locations. Complete removal can significantly improve overall outcomes, including relief from pain and increased quality of life.
iCareBetter Endometriosis Care
iCareBetter is a platform that connects patients with experts in endometriosis care. At iCareBetter, patients have access to surgeons who have completed advanced training. These professionals have shown expertise in the diagnosis and treatment of complex Endometriosis. iCareBetter utilizes a transparent and unbiased system to ensure that only doctors with proven advanced excision skills and a comprehensive care team can be on their surgeons’ list.
Patients can select their surgeon based on their specific symptoms. This empowers patients to consult a doctor who truly understands the complexity of their condition. Patients can access specialists for endometriosis in the pelvis, bowels, bladder, thorax, heart, or diaphragm. They also can find help with infertility issues.
A highly specialized endo surgeon will take a holistic approach to treatment. This holistic approach includes managing secondary comorbidities such as infertility, even in stage III and IV disease patients.
At iCareBetter, patients can also access expert physical therapists who understand the condition. Working with a physical therapist gives access to myofascial release techniques, visceral mobilization, and the tools to manage a susceptible nervous system for better pain management.
Team-based expert care improves post-operative outcomes. For some iCareBetter doctors, post-treatment reports of satisfactory pain relief could be over 80%, with less than 20% of women requiring subsequent pelvic surgery. Moreover, many patients see reduced pain relief requirements post-recovery.
Standards of excellence, such as those endorsed by iCareBetter, must become a driving force behind treatment protocols for Endometriosis. Women should no longer shoulder the pain and reduced quality of life associated with substandard care.
Conclusion
Endometriosis occurs due to the presence of endometrium-like cells found outside the uterus. The resulting inflammation, adhesions, and scarring can cause severe pain and symptoms related to the location of the lesions. By connecting patients with expert surgeons in endometriosis care, iCareBetter empowers patients to access the care leading to better outcomes. Advanced surgical excision, physical therapy, and an expert team-based approach can reduce pain, as well as skillfully manage secondary complications.
Find endometriosis specialists today.

Impact of Living with Endometriosis on Mental Health
(All research studies mentioned in this article about the impact of endometriosis on mental health enrolled people with assigned female gender at birth. However, to be inclusive to all people with endo, we use people throughout the article.)
Being diagnosed with endometriosis (endo) and living with it can bring up a lot of emotions. It can mean making space for changes that you may never have predicted or accounted for. Endometriosis impacts nearly 200 million people worldwide, but there is pernicious misinformation and a lack of awareness and understanding among the medical community and the larger society. This misinformation and lack of awareness stand in the way of receiving a timely diagnosis.
It takes, on average, over seven years for a person who has endometriosis to get a diagnosis. Essentially, this means experiencing intense pain, feeling unheard over and over, and being gaslit at a systemic level for at least seven years.
In most countries, managing the pain and heavy periods remain the first line of treatment for endometriosis. If one is lucky, they can access endometriosis excision surgery. However, the impact of endometriosis goes beyond just the physical. The effect of endometriosis on mental health and the emotional wellbeing of the person is enormous.
Link Between Endometriosis Pain and Mental Health
The mental health struggles of living with endometriosis vary from person to person. The debilitating chronic endometriosis pain, one of the most common symptoms, is a critical factor that impacts the quality of life and mental health. Along with the cyclic pelvic pain, one may also experience other types of pain in varying degrees:
- Non-menstrual pelvic pain
- Pain during ovulation, urination, and/or bowel movements
- Pain during sex
- Sciatic pain
- Pain post and during orgasms
- Widespread full-body pain.
Research published in the International Journal of Women’s Health Health looked at the link between common symptoms of endometriosis and mental wellbeing.
It found that a person experiencing chronic pelvic pain (CPP) is likely to feel higher levels of anxiety and depression, which can further amplify the perception and severity of pain, thus placing them in a vicious circle of physical and psychological distress.
Figure 1: The vicious circle of chronic pelvic pain and psychological disease.
Pelvic Pain Causes Further Effects of Endometriosis on Mental Health
A study found that endometriosis patients with pelvic pain had poorer quality of life and mental health than those with asymptomatic endometriosis. It also showed that non-menstrual pelvic pain impacts all the variables of a person’s life. Thus, the study emphasized psychological interventions as an essential aspect of the endometriosis treatment plan and pain management treatments and interventions.
In another meta-analysis of 99,614 people from 24 different studies, researchers found that chronic pelvic pain was a primary factor contributing to the higher rates of depression in patients with endometriosis. This study emphasized that treating this kind of depression with antidepressants without the efforts towards managing the chronic pain would indeed be ineffective.
The Emotional Reality of Endometriosis
Studies have tried to understand the impact and management of endometriosis within the medical healthcare system. But still, the health system has largely overlooked the effect of endometriosis on mental health.
Living with endometriosis can make daily activities a struggle, mainly due to the unpredictability of pain and fatigue. The struggle makes some tasks nearly impossible. These tasks can include planning, working, socializing, exercising, eating, or even basics like cooking, cleaning, and bathing. This inability fuels guilt and anxiety. Furthermore, the debilitating pain being reduced to “just a bad period” or “psychosomatic” often leaves one feeling gaslit, isolated, depressed, and sometimes suicidal.
This distress increases due to the lack of systemic and psychosocial support. When the BBC spoke to 13,500 people (female assigned at birth) with endometriosis, more than 50% of the respondents felt suicidal ideations.
This is a battle
For someone living with chronic pain every day, even a short-lived moment of low pain brings ease, which allows one to hope for a future not controlled by pain. However, grief sets in quickly as fatigue and flare-ups follow. These changes make life with endometriosis incoherent and an inescapable dance between hope and grief. A Swedish study concluded that people living with painful endometriosis underwent a constant struggle for coherence in their lives. It emphasized that healthcare providers should validate this struggle by understanding the disease-related grief.
The anxiety around pain and health, the grief related to the future, the loneliness and isolation often bring up the feeling that chronic pain has monopolized one’s life. Endometriosis becomes the central point around which all decisions revolve. It takes away the body’s ability to be reliable and the capacity to feel safe within it. It often changes the way one views themselves and takes the world in.
One of the ways we feel safe in the world is by feeling safe in our bodies. Then what happens to our sense of safety when the body is a constant source of never-ending pain?
The Trauma of Endometriosis
Experts define trauma as the experience of being left alone with one’s pain. Endometriosis isn’t different. Having to constantly explain one’s pain to medical doctors, families, and friends and still not being believed is an isolating and traumatizing experience. For some, this experience of being gaslit gets stored in the body and pushes the nervous system into a hypervigilant state (Fight, Flight, Freeze).
This experience of trauma can bring up various responses, anger being one of them. The anger can be at the world, the state, the body, the systems, other people, or the pain. It becomes our protective mechanism in response to the powerlessness that one feels while coping with endometriosis.
The Way Forward
In treating endometriosis, it becomes necessary to consider its impact on mental health and provide psychosocial support to people with endometriosis and their families. Unlike the conventional medical belief that solely focuses on the physiological aspects, a multidisciplinary approach integrating the mind and the body is necessary.
A trauma-informed psychotherapist specialized in treating endometriosis, and chronic pain can be helpful. A therapist trained in chronic pain management understands endometriosis, related diagnoses, and its trauma. This understanding is an integral part of the healing process. Seeing the light at the end of the tunnel is complicated and sometimes impossible with pain. Verbalizing the pain, having the hardships validated, acknowledged, and believed can be an empowering experience. Just as people seek medical help for their physical symptoms, seeking help for mental health struggles is an integral part of the endometriosis journey. If therapy is hard to access, support groups for endometriosis can be a step forward. You should know that you are not alone in your experience, and you can have support. The supports that you get can be a lifeline to your mental health.
Author: Anindita Kundu, Trauma Psychotherapist.
How has endometriosis impacted your mental health? Have you considered working with a mental health specialist to help you?

Questions to Ask Your Physical Therapist When you have endometriosis
Author: Dr. Rebecca Patton, PT, DPT
“I feel like you’re the first physical therapist who understands endo.” It’s a statement I wish I didn’t hear as often as I do. Unfortunately, there has not been a resource specifically made to evaluate pelvic physical therapists’ knowledge about endometriosis before iCareBetter.
Education for physical therapists regarding endometriosis needs more advanced continuing education courses. But it doesn’t typically happen until after completing a doctoral program. For perspective, I self-taught for several years before seeking specific classes related to endometriosis care. Therefore, it wasn’t until years after specializing in pelvic pain treatment that I realized the inefficiency of care for those with endometriosis. We can do better, but we have a long way to go.
Communicating with a pelvic physical therapist before seeking treatment can allow you to ask important questions to ensure you’re finding a provider that is a good fit for you. For achieving this goal, take advantage of time-saving strategies such as a phone consultation before committing to a therapist. Here are a few questions you may want to ask during that phone consultation or the first visit with a pelvic physical therapist for your endometriosis issues.
Endometriosis Care Process with iCareBetter
1- Find an expert based on keyword/ specialty or state
2- choose your doctor from the list
3- Get the contact info
4- First call and consultation.
5- Get info regarding costs and care process
6- Receive care
Top endometriosis physical therapists
Endometriosis Physical Therapy
Table of contents
1. Are you familiar with the disease process and current treatment standards for endometriosis?
2. Do they consider the whole body when treating your symptoms?
3. Do they practice trauma-informed care specifically related to healthcare trauma?
4- How much time will you have for a session?
1. Are you familiar with the disease process and current treatment standards for endometriosis?
It is helpful when your treating therapist is up to date on current treatment standards, as with any diagnosis. Unfortunately, there is no specific physical therapy protocol for treating patients with endometriosis. However, physical therapists should understand who will be involved in your healthcare team and have a multidisciplinary approach (1). I aim to establish what provider, either GYN or expert surgeon, will be a point of contact on that first visit.
2. Do they consider the whole body when treating your symptoms?
Endometriosis is known as a pelvic disease, but we know it is much more than that. Your physical therapist needs to tap into their education to evaluate and treat the whole body. The secondary effect of endo is often an upregulated nervous system. On the initial visit, it is typical that your physical therapist will look at movement patterns from your neck to your feet. Internal pelvic floor assessments are common but certainly do not need to happen on the first visit. Pelvic floor function is only one component in a much larger picture of your overall function. Your individual goals and comfort will dictate how much treatment involves pelvic floor treatment.
Advanced Treatments and education
Treatment involving the abdominal wall fascia, diaphragm, and viscera (organs) require additional advanced coursework compared to treating the pelvic floor. Therefore, you can ask them if they have taken additional coursework to treat the abdomen to get an idea of their experience. There is not one single treatment philosophy for the abdomen, but some courses focus on continuing education in this area. The most common that I am familiar with are The Barral Institute (2), Ramona Horton MPT, DPT (3), and Institute of Physical Art (4). Other courses involve manual nerve techniques such as Lumbar and Sacral Nerve Manual Assessment through the Herman and Wallace Pelvic Rehab Institute (5). These are just a few of the many available resources your physical therapist may use to learn more after graduate school. Some pelvic physical therapists create their treatment tanks to teach one another these skillsets.
Treatment strategies that help regulate an upregulated nervous system may be part of your care. These strategies can look like gentle hands-on treatment, questions to help you process how you relate to your body, and creating mindfulness along with movement. The connection of how our nervous system interprets information from our body is complex. A physical therapist can be a valuable resource to help you better understand the pain response and the nervous system.
3. Do they practice trauma-informed care specifically related to healthcare trauma?
Trauma-informed care in physical therapy does not substitute mental health treatment. A trauma-informed approach concerning physical therapy means understanding the entirety of the patient’s experience and the effects of that experience. Medical trauma can have a lasting response on an individual’s well-being (6). We know that those with endo, on average, have a delayed diagnosis. This delay can lead to a complicated relationship with the medical providers. Many patients with endo are seeking out pelvic PT after years of seeing various specialists. These experiences with the medical system can create barriers to a patient feeling comfortable with a new provider.
For this reason, a trauma-informed approach to treatment is essential. Awareness of how these experiences may have impacted their patient is a critical portion of providing affirming care. You can ask your physical therapist about some processes that they use to create a safe environment. These processes should include consent before any treatment or touching, checking in with your emotions and body reaction during manual therapy, and providing adequate time to provide education throughout the session.
4. How much time will you have for a session?
Asking this question can ensure you have an idea of what to expect when going into your appointment. There is no magic number of minutes that will create a perfect appointment. However, the nature of endo being more complex means I prefer more time to establish a care plan. There are multiple factors to consider during the first evaluation. These factors include sexual health, daily function, bowel and bladder health, and personal goals. Having realistic expectations for each session is helpful to decrease additional medical trauma and find a therapist that fits your needs.
Patient care and human interaction are complex, and sometimes it takes time to establish a level of comfort with your PT. Every session of PT may not equal a breakthrough in pain. Retraining the nervous system takes time, especially when the body has been protecting itself due to chronic pain.
Ultimately, endo care is ideally a multidisciplinary approach. Your physical therapist can work closely with your gynecologist and other healthcare team members to find the best individual plan for you.
If you have more questions about pelvic physical therapy, reach out for more information.
Would you mind sharing with us what pleasant or unpleasant experiences you have had with your PT?
References:
1. Agarwal SK, Foster WG, Groessl EJ. Rethinking endometriosis care: applying the chronic care model via a multidisciplinary program for the care of women with endometriosis. Int J Womens Health. 2019;11:405-410. Published 2019 Jul 23. doi:10.2147/IJWH.S207373
2. Jean-Pierre Barral, DO, MRO(F), RPT. The Barral Institute. Accessed September 1st, 2021. https://www.barralinstitute.com/
3. Ramona Horton, MPT, DPT. Herman and Wallace Pelvic Rehabilitation Institute. Accessed August 27th, 2021. https://hermanwallace.com/faculty/ramona-horton
4. Institute of Physical Art. 2015-2021. Accessed August 19th, 2021. https://instituteofphysicalart.com/
5. Nari Clemmons PT, PRPC. Herman and Wallace Pelvic Rehabilitation Institute. Accessed August 20th, 2021. https://hermanwallace.com/faculty/nari-clemons6. Michelle Flaum Hall and Scott E. Hall. When Treatment Becomes Trauma: Defining, Preventing, and Transforming Medical Trauma. American Counseling Association. March 24th, 2013. Accessed August 19th, 2021. https://www.counseling.org/knowledge-center/vistas/by-year2/vistas-2013/docs/default-source/vistas/when-treatment-becomes-trauma-defining-preventing-

Endometrioma 101: Understanding Deep Ovarian Endometriosis
Your Guide to Ovarian Endometrioma: Treatment, Symptoms, Doctors, Etc.
Endometrioma (deep ovarian endometriosis) can be difficult to treat due to controversies and challenges surrounding the best approaches, treatment, and diagnosis. Many of these hurdles result from misunderstandings about the condition and underlying disease process – deep ovarian endometriosis.
If you suffer from these ovarian endometriosis lesions, our sincere thoughts go out to you. Often known as “chocolate cysts,” some consider endometriomas as the most severe threat to a woman’s reproductive system (aside from cancerous tumors found in the reproductive tract). Furthermore, these lesions don’t always respond well to medical treatment and can potentially ruin the health of ovarian tissue. This article will help you understand endometrioma, symptoms, and deep ovarian endometriosis treatment.
Get the pdf Version of this article
Table of contents:
1- What is Endometriomas (Deep Ovarian Endometriosis)?
2- Recurrence of The Lesions Following Surgery
3- linical Impact of Endometriomas (in Women of Reproductive Age)
5- Treatment and Surgery Options
6- Final Thoughts and Question for Readers
What is Endometriomas (Deep Ovarian Endometriosis)?
Endometriomas happen when endometrial-like tissue grows inside the ovary or sometimes outside. Endometrioma is very common and affects between 17-44% of endo patients. Endometriomas are typically an advanced form of endometriosis, meaning stage three or four.
Surgery is often necessary to remove the endometriomas. However, eliminating endometrioma cysts and capsules is an advanced procedure and needs excellent skills. This surgery can potentially lead to partial or complete loss of ovarian function, especially if done by less experienced surgeons. These cystic masses can cause extreme challenges for women undergoing fertility treatments, i.e., assisted reproductive technologies (ART).
Endometriomas are dark-fluid-filled cavities, and they can present in a variety of shapes and sizes. An ultrasound can show suspected cases of endometrioma, but confirmation needs surgery and histology. Therefore, getting a diagnosis of endometrioma can be riddled with challenges.
Recurrence of The Lesions Following Surgery
On our social media accounts, we receive many questions about the topic of endometrioma recurrence. We took to Instagram to get the responses from endometriosis specialists about this recurrence. Here are some of their responses:
“It depends on several factors including the age of the patient, method of surgery, the experience of the surgeon, etc. In the literature, recurrence rates of over 30% have been reported, although I have personally not seen that high of recurrence risk.”
“We’ve had ovarian recurrence rates of less than 10 percent in our two years of follow-ups of about 85 patients with ovarian endometriomas.”
“What’s important is to completely free the ovary and excise the peritoneum or uterosacral ligament it was adherent to, apart from excising the cyst. This will truly help reduce recurrence rates compared to just doing a cyst excision and leaving peritoneal disease behind.”
“I share the same opinion, in my center, our recurrence rate is less than 8% a good technique and excision of all zone of endometrioma even peritoneal improve outcomes, also as previously said it depends on many factors like endometrioma size, multiple endometriomas, and post-op treatment.”
“We have a very low recurrence rate. This is because often, during surgery, only the visible endometrioma cysts are removed. Anything under 2 cm is out of our visual field.”
Clinical Impact of Endometriomas (in Women of Reproductive Age)
Endometriomas does not cause infertility in all women it affects. However, studies show that between 25% to 50% of women with infertility have endometriosis, and 30% to 50% of women with endometriosis have infertility. However, that does not mean that endometrioma will necessarily cause infertility in women of reproductive age, especially when diagnosed and treated early with the best-practice treatments that have evolved over the years.
One of the leading fertility challenges is that ovarian lesions affect the number of eggs in ovarian tissue. Endometrioma can also impair the maturation of the egg and cause the woman to have a lower antral follicle count (AFC) and Anti-Müllerian hormone (AMH). Also, women with endometriomas often have high follicle-stimulating hormone (FSH) levels.
Major Concerns:
- Intense pelvic pain
- Possible infertility
- Decrease ovarian function
- It can place women of child-bearing age at a higher risk of cancer
Treatment and Surgery Options
Treatment for endometriomas will vary from person to person. The number of lesions and the staging of the disease progress are just a couple of the factors that will influence the right treatment plan for you.
Treatment for Females of Reproductive Ages
Many OB-GYNS and other healthcare providers still practice old treatments for endometriosis that don’t effectively manage the disorder. It’s a complicated condition. Thus, there are many myths and misconceptions about endometriosis.
Women of reproductive ages who wish to maintain fertility should have a fertility specialist in their multidisciplinary endometriosis team. Women with endometriomas may respond to some of the following treatments:
Non-surgical treatments: These treatment options are temporary choices to manage pain and complications in the short term.
- Medication therapy
- Observation
Surgical treatment: this may include:
- Drainage
- Laser ablation
- Capsule excision (the procedure of choice for most top experts)
Final Thoughts and Question for Readers
Have you had to deal with endometrioma? If so, please share how it has impacted your endo journey.

7 Ways to Prepare For First Endometriosis Specialist Appointment
Diagnosis. Treatment. Surgery. Many Topics May Be Discussed At Your Visit
An endometriosis specialist appointment is not something you do every day (although sometimes it might feel like all day while you’re waiting there). However, the time you get to talk with the doctor may be pretty short. During that moment of consultation with the endometriosis (endo) specialist, you might feel brain fogged or bombarded. Whether it’s the diagnosis, treatment, surgery, pain management, or an endometriosis symptom you want to bring up, it’s easy to forget an essential topic while you’re there.
To make the most out of your initial endometriosis specialist appointment with an endometriosis specialist, we’ve made a list of seven ways you can prepare for the visit. First, we will give a short description of what endometriosis is.
Table of contents
7 Ways to Prepare for Endometriosis Specialist Appointment
Endometriosis Care Process with iCareBetter
What’s Endometriosis?
Endometriosis is a female medical disorder in which tissue similar to the endometrium (tissue that lines the walls of the uterus) grows outside the uterus. This endometriosis tissue can grow on the surface of the uterus, ovaries, intestines, fallopian tubes, bladder, or other organs in the body.
During menstruation, this tissue releases blood, and it sloughs off. However, this blood and tissue often remain trapped with no way to escape the body. This increased pressure can result in moderate to severe pain, among other symptoms. If you want to learn more about endometriosis and get a general background on the condition, read our article, “Endometriosis 101: Covering the Basics.”
Why You Are Here
People of various ages and demographics are subject to this often debilitating inflammatory pelvic disorder. Whether you have confirmed the diagnosis of endometriosis or if you need surgery to verify its presence and remove lesions – these suggestions can help you prepare for the endometriosis specialist appointment. There are many stages of endometriosis. Whether you’ve got into a specialist early on your journey or later, the important thing is that you are here now – exploring treatment options.
7 Ways to Prepare for Endometriosis Specialist Appointment
Once you have found an experienced endometriosis specialist, it’s essential to prepare yourself for the doctor’s appointment ahead of time. There is no concrete test to diagnose endometriosis (outside of surgery). Therefore, it’s imperative to have a solid understanding of the signs and symptoms of endo and detailed accounts of your own experience ready. Simple things such as medical records or journals that list all your endometriosis symptoms are a vital arsenal that will help you and your doctor determine your treatment plan.
1. Gather Your Records.
Unfortunately, most people with endometriosis have had many doctor appointments before seeing an endometriosis specialist. Therefore, you should have some medical records for them to review during your first appointment with an endo specialist. Gather everything from your regular medical history from your general practitioner to your OB/GYN records, testing, imaging, blood work, etc. Even if you think the particular doctor appointment or medical history is insignificant, you might be surprised by the various conditions linked to endometriosis. Bring it all. This information could play a vital role in your endometriosis treatment.
2. Keep a Journal of Endometriosis Symptoms/Pain.
Write down all the possible endo signs and symptoms you’ve had leading up to the doctor’s appointment. If you get a visit scheduled, and it’s a couple of weeks out, start the journal at that time, but also include the signs and symptoms you’ve experienced leading up to that point. Then, from that date until your appointment, write down all the different types of symptoms you experience. Include everything, even if you don’t think it’s relevant, like colds, headaches, stomach issues, shortness of breath, chest pain, etc. Also, be sure to include your emotions and feelings because endometriosis can significantly impact mental health and can lead to conditions such as depression and anxiety. Emotions and mental health are essential as you might want to include a counselor as part of your holistic endometriosis treatment team.
3. Bring This Printable Guide.
At endometriosis.org, they’ve created a convenient guide that can help you describe your symptoms and know what to ask your endometriosis specialist. Click here for the PDF. Please print it out and answer all the questions. Bring this with you to your doctor’s appointment to help specifically describe your endometriosis pain and other symptoms.
4. Take All Your Medications With You.
The importance of this cannot be understated. Even if you have a medication reconciliation (also known as a “med rec” for short) from your doctor, it’s important to realize those are not always up-to-date with everything you take. This inconsistency is especially true if you are on medications from multiple specialists or take supplements as well. The best way for your endo specialist to have a complete picture of all the medicines you are currently taking is by bringing them with you to the doctor’s appointment. You should include any supplements or over-the-counter medications. Bring in the physical bottles along with any medication history records.
5. Prepare Yourself Mentally.
Go into the appointment with the bold mindset that you will ask every single question you have to gain clarity on your endometriosis diagnosis and treatment options. Endometriosis is an aggressive inflammatory disorder that can have a devastating impact on your quality of life. It would help if you carried an even more aggressive attitude toward trying to stop it dead in its tracks.
6. Bring a List of Questions.
What’s been bothering you the most? Pain? Bowel symptoms? Bring a list of all the important questions that you want answers to. Writing them down will help you not forget during the appointment. Furthermore, when the doctor sees you have a list of questions you want answers to, it makes it harder for them to get up and walk out of the room like the appointment is over. If something like that has ever happened to you, we are sorry you’ve experienced this. That’s why it’s crucial to find a vetted endometriosis expert.
7. Take a Support Person With You.
Finding a good endo expert is no easy task (unless you use iCareBetter to connect you to one). If you are the type of person who is a bit shy or feels intimidated, you should bring your best support person to the appointment with you. Even if you are not nervous about your first endometriosis specialist appointment, having someone you trust by your side can help you process the information and encourage you along your journey. If no one you would like to accompany you, consider bringing a recorder and taping the visit. Because this can help you go back later and make sure you’ve understood all the information. Most doctors will have no qualms about recording your visit.
Endometriosis Care Process with iCareBetter
1- Find an expert based on keyword/ specialty or state
2- choose your doctor from the list
3- Get the contact info
4- First call and consultation.
5- Get info regarding costs and care process
6- Receive care
We Want to Hear From You
Have you been to an endometriosis specialist (OB-GYN experienced in endo)? If so, is there anything you wished you would have done differently? If you’ve not been to an endo specialist yet, what is your biggest concern about the first doctor visit?

Endometriosis Facts & Myths: Dispelling the Misconceptions
Debunking the Myths About Endometriosis & Exploring the Facts
One in ten women worldwide is affected by endometriosis, also known as “endo,” for short. While this number is an estimate, the actual figures may be higher. Not only is the person with this inflammatory disorder affected, so are the family members and people around her due to the often debilitating effects of this disease. Endometriosis facts are important because it is complex and often misunderstood even though it’s a common disorder. Because of this, there are many myths and misconceptions regarding endometriosis prognosis, treatment, causes, symptoms, diagnosis, complications, etc.
Focusing on the disease itself often ignores the vicious cycles of stress, fatigue, pain, doctor visits, flare-ups, and loss of productivity experienced by the patient. These factors can lead to a decreased quality of life. Worse is that endometriosis facts come behind outdated treatment options, myths, and misconceptions about this disorder. It takes an average of eight to ten years for a patient to be diagnosed with endometriosis. One of the biggest problems with the misconceptions about endo is that they can prevent women from seeking treatment. Keep reading as we review endometriosis facts and debunk the myths.
Overview of Endometriosis
Endometriosis is a pelvic disorder characterized by endometriosis tissue similar but not the same as the tissue inside the uterus, growing elsewhere. Typically, the growth occurs outside the uterus, ovaries, fallopian tubes, cervix, the surface of the bladder, bowel, and distant organs.
Endometriosis growths can cause pain, scarring, and sometimes infertility. Pain from endometriosis is usually the result of menstrual bleeding from the tissues. Unlike the endometrium inside your uterus, blood that comes from endo tissue outside this organ has no means of escaping the body. This blood causes increased pressure and inflammation, which can result in pain that’s often debilitating. If you would like to learn more information about endometriosis, please read our introduction article, “Endometriosis 101: Covering the Basics.”
Why is it Difficult to Diagnose endometriosis?
Studies show that it can take an average of seven years or more for a woman to get an endometriosis diagnosis. Why is this? Endometriosis signs and symptoms are often similar to other conditions, such as irritable bowel syndrome or pelvic inflammatory disease (PID). Therefore, it’s often mistaken for another illness. Furthermore, the myths and misconceptions we discuss below also prevent a lot of women from seeking help. For this reason, it’s crucial to get the endometriosis facts clear. Keep reading as we debunk the myths and state the facts.
Myth #1: Severe Period Pain is Normal
Nineteenth-century doctors were often perplexed by “women’s problems.” As a result, women were often discounted as being unstable mentally. While the attitudes and thoughts have improved since, some of those old beliefs persist, including those regarding period pain.
Many patients with endometriosis hear that their severe period pain is “normal.” Pain and cramping are normal during menstruation. However, the pain should not be so intense that it interferes with functioning or impacts the quality of life. If your period pain is so severe that you cannot carry out daily activities, you should seek an endometriosis expert.
Myth #2: A Hysterectomy Cures Endometriosis
Endometriosis growths are tissues “similar” to those inside of the uterus. It is not the same tissue. Simply removing the uterus and/or ovaries without excising any endometriotic implants growing outside the uterus will not cure it.
Myth #3: Endometriosis Only Affects the Pelvic Area
Locations within the pelvis, such as the surface of the uterus, bladder, or fallopian tubes, are the most common locations where endometriosis growths occur. However, endo can occur elsewhere in the body. In some cases, endometriosis growths have been present in distant organs, such as the lungs.
Myth #4: Endometriosis Symptoms are Simply a “Heavy Period”
Bleeding during menstruation can be heavy at times. However, it should not exceed the saturation of a pad or tampon in one hour. If you experience that degree of bleeding, you should bring this up with your healthcare provider. The fact is that many women with endometriosis experience abnormally heavy flow due to the excess tissue.
Myth #5: Douching Causes Endometriosis
No scientific evidence links douching with the development of endometriosis.
Myth #6: Having an Abortion Can Cause Endometriosis
No scientific evidence demonstrates that having an abortion causes endometriosis. Those who claim otherwise might be confusing endometritis and endometriosis.
Myth #7: You’re Too Young to Have Endometriosis
A common misconception is that endometriosis is rare or doesn’t occur in young women and teenagers. As a result, many doctors do not consider an endometriosis diagnosis in young women with typical symptoms. Endometriosis facts demonstrate that teenagers and women in their early 20s can have the disorder. Most people with endometriosis state they experienced endo symptoms during adolescence.
Myth #8: Endometriosis Can Be Prevented
It’s not clearly understood what causes endometriosis. Therefore, there are no proven ways to prevent this inflammatory condition. Anything else is purely speculation at this point.
Myth #9: Endometriosis is Always Painful
Not all women with endometriosis experience pain. Studies show that some women with advanced stages of endometriosis do not experience pain as a symptom.
Myth #10: Pregnancy is a Cure for Endometriosis
This misconception about endometriosis is slowly beginning to fade. However, not quickly enough! Pregnancy fluctuates hormones in the female body, which can temporarily suppress some symptoms of endometriosis. However, these symptoms usually recur for most patients following the pregnancy. Therefore, it’s not a cure.
Myth #11: Menopause Cures Endometriosis
Endometriosis symptoms often occur during menstruation, but many women experience them long after periods stop. Following menopause, the body still produces small amounts of hormones, and the endometriosis tissue still responds to them, thus causing pain. For many women, the symptoms of endometriosis may improve after menopause, but that does not mean it’s a cure. Depending on the case, it might be necessary to remove endometriosis implants or adhesions even after menopause.
Myth #12: Hormonal Therapy Cures Endometriosis
Doctors have been treating endometriosis for years using hormonal therapy drugs. However, these medications do not have long-term effects on the disease itself. Hormones can help relieve the symptoms temporarily and even shrink the growths, but they do not cure endometriosis.
Myth #13: Endometriosis is Cancer
Endometriosis growths are not cancerous. To date, there is little evidence that shows endometriosis directly causes cancer. However, some types of cancers are more common in women who have endometriosis. Endometrial cancer is also known as uterine cancer. Many studies have examined the relationship between the two, and one showed that merely 0.7 percent of patients with endometriosis had endometrial cancer at the 10-year follow-up. Therefore, endometriosis does not equal cancer, but it may increase the risk of cancer.
Myth #14: Tubal Endometriosis Always Causes Infertility
Tubal endometriosis is not very common, and it does not always cause infertility. Does endometriosis cause infertility? It can be in many cases, but the mechanisms of infertility in endometriosis remain multifactorial. Can you get pregnant with endometriosis? It is possible, and many women do – especially with proper treatment early on.
Myth #15: Endometriosis Symptoms Are the Results of Emotional Distress (It Is All in Your Head)
Yes. People have heard many times that emotional distress could be the cause of their endometriosis and pain. This statement is false. The fact is, endometriosis is a highly complex disorder with many underpinnings. Those with endometriosis often experience emotional distress as an impact of the symptoms such as pain and infertility. But emotional distress it’s not the cause of endometriosis symptoms.
Endometriosis quick facts:
1- There is no blood test available for the diagnosis of endometriosis.
Mehedintu C, J Med Life, 2014
2- The diagnosis of endometriosis starts by taking a good history from patients, and performing a detailed physical exam including pelvic exam. In some cases, a doctor might ask for MRI and Ultrasound to have a more thorough picture. But the ultimate diagnosis is only possible with laparoscopic /robotic surgery and taking a biopsy for histopathology. There is no blood test that can tell if you have endometriosis.
3- Studies show that those with endometriosis have an increased risk of developing depression and anxiety disorders.
Chen LC, et al, J Affect Disord, 2016
4- Pelvic pain due to endo occurs a day part of an inflammatory cycle which can affect the pelvic organs and functions such as sitting, sex, bowel movements and even urination. Pelvic floor physical therapy can help with restoring balance to the pelvic floor muscles.
Dr. Juan Michelle Martin, Endometriosis Physical Therapist.
5- “The most common clinical signs of endometriosis are menstrual irregularities, chronic pelvic pain, dysmenorrhea (painful periods), dyspareunia (painful sex), and infertility.”
Lagana AS, et al, Int J Womens Health. 2017
We Want Your Input
Are there any endometriosis myths or misconceptions we did not list here? Let us know in the comments below!

A Multidisciplinary Team for Endometriosis is Key to Positive Outcomes
Why Your Endometriosis Treatment Plan Should be Multidisciplinary
Endometriosis (endo) is a chronic and progressive disorder characterized by the growth of endometriosis tissue outside the uterus. This disorder often affects various organs in the body and results in pain and other issues. In addition to the intense physical and often debilitating symptoms of the disease, it can also take a toll on mental and spiritual health. Therefore, a multidisciplinary team (MDT) approach to endometriosis pain, surgery, and disease management leads to the best outcomes for patients. Keep reading to learn how.
What is Endometriosis?
Pronounced (en-doe-me-tree-O-sis), endometriosis is a chronic inflammatory disorder in which a type of tissue that is similar to the endometrial tissue that normally grows inside the uterus, grows outside this organ. Sometimes, the endometriosis tissue appears on the outer side of the uterus. These lesions can also grow on the ovaries, fallopian tubes, bladder wall, and on the outside of other organs within the pelvic cavity and other regions of the body.
Endometriosis is often a very painful and debilitating disease. During menstruation, these endometriosis growths shed blood into the body which is not able to be released. This causes an increase in pressure throughout the pelvic and sometimes abdominal region. Endo often involves other organs such as the bowels, ovaries, fallopian tubes, vagina, and cervix. In rare cases, it may affect other organs, such as the bladder, lungs, diaphragm, or kidneys. If you would like to learn more information about endometriosis, read our article, “Endometriosis 101: Covering the Basics”.
What is a Multidisciplinary Team Approach in Medicine?
Multidisciplinary care is when multiple members of the healthcare team come together to collaborate to provide optimal care for a patient. When it comes to endometriosis treatment, it’s important to involve various disciplines across the healthcare spectrum to achieve the best possible outcomes for patients.
Benefits of a Multidisciplinary Treatment (MDT) Team for Endometriosis
Draw in endo experts across different care areas to enhance the patient’s prospects and outcomes. Physicians benefit from this approach as they are able to provide a better framework for decision-making on a collaborative level and implementation. These aspects are particularly important when dealing with complex endometriosis cases. When several endo experts work together in unison, the benefits include cross-discipline learning, research, and review.
There is a type of disease, called deep infiltrating endometriosis (DIE). Alarmingly, about 20 percent of endo patients have this type. With DIE, the lesions can penetrate 5 mm deep into the organs affected by the disorder. A multidisciplinary treatment plan is the best approach for better outcomes and improved quality of life for the patient. The resection of DIE lesions requires a surgeon with expertise in endometriosis and a multidisciplinary approach coordinated by the endo specialist.
In fact, in 2019, the Society for Women’s Health Research assembled a team of clinicians, researchers, and patients to deliberate on the barriers in the commonly accepted forms of endometriosis treatment and management. The team underscored the importance of comprehensive and interdisciplinary approaches to disease and pain management for proper treatment and diagnosis.
Who comprises an Endometriosis Multidisciplinary Team?
The following are some of the endometriosis experts that come together and help treat patients holistically:
Endometriosis Surgeon (Gynecologist):
If you have endometriosis, a regular obstetrics-gynecological surgeon is not going to suffice. It’s important to have an endometriosis specialist, who is an OB surgeon with experience in the treatment of this pelvic disease. An endometriosis laparoscopy is often needed to diagnose and treat the disease. It’s important to choose a surgeon familiar with endo to ensure all lesions are removed. Learn more about endometriosis specialists and how to find a vetted physician in our article here.
Colorectal Surgeon (Bowel Surgeon):
If the endometriosis affects the bowel, surgical excision may be necessary to remove the lesions. Surgical treatment, such as full-thickness disc excision or a bowel resection should only be performed by an experienced colorectal surgeon. This physician will participate in the care from the diagnostic workup to surgical treatment and follow-up care.
Urologist (Genitourinary Tract Doctor):
A urologist treats disorders of the urethra, kidneys, urinary bladder, and adrenal glands. Having an experienced urologist as part of your multidisciplinary team can help aid in the treatment of ureter and bladder lesions as well as minimize kidney or bladder complications.
Radiologist Experienced in Endometriosis:
Endometriosis may have several presentations, which can make diagnostic testing challenging. Because endometriosis lesions can present in other areas of the body away from the reproductive organs, it’s important that the radiologist on your team is familiar with the pelvic nerve anatomy and how to detect signs of neural endometriosis.
Physical Therapist/Pelvic Floor Therapist:
Physical therapy can be very important in the treatment of endometriosis. While some patients may require physical therapy to help them adapt to pain and stay mobile, others may need highly specific pelvic floor therapy. A pelvic floor physical therapist can work with the patient to help reduce adhesions and scar tissue which can limit pelvic floor extensibility. These exercises are important to help reduce pain sometimes associated with intercourse or the insertion of a tampon.
Pain Management Doctor:
Endometriosis pain is often the primary complaint and most debilitating symptom of this disease. In fact, it’s not uncommon for the pain associated with endo to become so intense that a person is no longer able to function in daily life. For this reason, a pain management doctor should be a part of the team to improve functioning and overall quality of life.
Psychiatrist/Psychologist:
Anxiety and depression are two of the biggest mental health disorders that often accompany endometriosis. Furthermore, the pain and sometimes infertility that come with this disorder can further aggravate these negative emotions. Therefore, a holistic MDT for endometriosis will include a psychiatrist or psychologist, possibly one who specializes in pain management.
Nutritionist:
Nutrition plays a key role in the processes and regulation of your digestive and immune systems. A proper endometriosis diet can help to reduce the chronic inflammation that keeps the endometriosis lesions growing and spreading. A nutritionist with experience in treating endo patients is key for successful outcomes.
Pathologist:
There are different stages and types of endometriosis. Endometriosis with architectural atypia is one type that may be a precursor of ovarian cancer. Therefore, it’s important that a pathologist carefully examines the lesions to discover if they could be indicative of endometriosis-associated ovarian cancer.
Building Your Multidisciplinary Team for Endometriosis
Who’s got your back? If you have or suspect you might have endometriosis, this is a very important question to ask yourself. iCareBetter is a digital platform that connects endo patients to vetted endometriosis experts across a variety of disciplines. If you have endo, we want to hear from you. Do you already have an MDT for endo? If so, who are the members of your personal team?

How Do I Know If I Have Endometriosis? Endometriosis Signs
Learn Endometriosis Signs & Symptoms & What to Tell Your Dr.
Pelvic pain is common for most women during their period. However, for some – this time of the month comes with excruciating pain due to the medical condition – endometriosis (also known as endo for short). Believe it or not, endometriosis signs extend beyond just the debilitating pain, although, that’s the hallmark symptom of this inflammatory disorder.
If you think you might have endometriosis, it’s important to have a solid foundation of information before you see your doctor for a possible endo diagnosis. Keep reading to learn what endometriosis is and what are the most common signs and symptoms of this condition.
What Is Endometriosis?
Pronounced (en-doe-me-tree-O-sis), endometriosis is a chronic inflammatory disorder of the pelvis where tissue similar to that normally grows inside your uterus, grows elsewhere instead, usually on the outside of it. The endometriosis tissue can block fallopian tubes, cover your ovaries, and even line the organs of your pelvis.
Endometriosis can cause intense pain and fatigue, which makes it a disabling inflammatory condition for many women. Pain from endometriosis can be so intense that sometimes even medication cannot touch it. Other organs commonly involved include the fallopian tubes, bowels, cervix, ovaries, vagina, and pelvic tissue. Rarely, endo may also affect distant organs. Learn more about the disorder in our previous article, “Endometriosis 101: Covering the Basics”.
What Are Endometriosis Signs and Symptoms?
Sadly, endometriosis is an inflammatory disorder that often goes undiagnosed for years because the hallmark symptoms are things that some women take for granted as “normal”: heavy bleeding and pain during periods. If you think you might have endometriosis, it’s important that you know what to look for and when you should notify a doctor. The following are seven common signs of endometriosis:
Dysmenorrhea (painful periods):
Intense pelvic or abdominal pain is one of the most common symptoms of endometriosis. Endometriosis pain is often described as a sharp or stabbing sensation. During menstruation, women with endo may experience very painful periods because the endometrial tissue swells and bleeds every month, just like the uterine lining would. However, because this process is occurring outside the uterus, blood is not easily shed, and this pressure can cause extreme cramping that is much more intense than typical period cramps. Period pain should not disrupt your daily life, so if it does, you need to let your doctor know or find a qualified endo specialist.
Menorrhagia (heavy menstrual bleeding):
While many women bleed heavily during their period, endometriosis can cause significant blood loss. How do you know if your amount of bleeding is excessive? Watch for these signs:
- Passing large clots
- Period goes on longer than a week
- Bleeding through a pad or tampon in an hour
- Too fatigued to carry out daily activities
If you have these symptoms, you may have menorrhagia and should contact a gynecologist. Menorrhagia is sometimes caused by endometriosis, and it can cause anemia and severe fatigue.
Dyspareunia (pain during or after intercourse):
When endometriosis is the cause of painful intercourse, the woman may not experience the pain upon entry, only upon deep penetration. There can be physical and psychological causes of this condition, and endometriosis may be the culprit, as tissue builds up on the other side of the lower uterus or vagina – and sexual intercourse can stretch the tissue. You should talk to an experienced physician if you have pain during or after intercourse.
Chronic Pelvic Pain:
While the inflammatory condition usually involves pain during menstruation, endometriosis pain can occur at any time of the month. Endometriosis causes an increase in pressure due to the excessive tissue in the pelvic cavity. This can cause a chronic pain condition that might be felt exclusively in the pelvis or manifest as abdominal or back pain.
Ovarian Cysts:
There is a type of endometriosis that causes endometriomas (also known as chocolate cysts) to grow on your ovaries. These cysts are non-cancerous but may become large and painful. Also, women who have these may also have other endometrial growths in the abdominal or pelvic areas.
Infertility:
Up to about half of women who have problems with fertility also have endometriosis. Furthermore, up to 50 percent of women who have endometriosis are unable to get or stay pregnant. The relationship between these conditions isn’t always clear as many factors can impact fertility. However, in the event that the endometriosis tissue blocks the reproductive organs, there is a clear connection. Treating the condition can increase your odds of having a baby. If these fertility issues are affecting you, contact an endometriosis specialist.
Bowel/Bladder Problems:
Bathroom visits may be problematic if you have endometriosis lesions growing near your bladder or bowels. And if you are experiencing difficulty with urination or bowel movements or bleeding in the bowel – these may be signs of endometriosis. Also, if you have painful urination, blood in your stool, nausea, or hyper urgency to urinate – you should tell your medical provider immediately.
When to Call Your Healthcare Provider
Share with your healthcare provider any of the following endometriosis signs and symptoms:
- Pain. Pain is the most common sign of endometriosis, and it can be present:
- During or after sex
- With bowel movements
- When urinating during your period
- As chronic abdominal, lower back, or intestinal pain
- Similar to menstrual cramps that get worse gradually
- Bleeding or spotting between periods
- Difficulty getting pregnant or infertility
- Digestive issues or stomach problems such as diarrhea, constipation, bloating, or nausea—especially during your periods

Find an Endometriosis Specialist Doctor for Diagnosis, Treatment, & Surgery
Why It’s Important Your OB-GYN Specializes in Endometriosis?
When it comes to the treatment and management of endometriosis pain and/or other symptoms, all doctors are not the same. In fact, if you have or suspect you might have endometriosis, you should never just walk into the office of a random obstetrics/gynecology (OB-GYN) surgeon.
However, it can be a bit tricky to find an endometriosis specialist that is highly skilled and follows the best treatment practices for this disorder. If you want to learn more about endometriosis, read this article that gives an introduction to the condition, signs and symptoms, causes, complications, and treatments.
With so many myths about endometriosis (endo) – it’s important to separate facts from fiction. Arm yourself with research and a solid foundation of knowledge to help you simplify the process and to get in touch with a trusted endometriosis specialist. Keep reading to find out why it’s so important to use an endo expert, red flags that your doctor/surgeon is not the right fit, and how to find an endometriosis specialist near you.
Join endometriosis forum or Instagram page and discover endometriosis stories & discussions
This article will cover:
- What is an Endometriosis Specialist?
- How are Endo Specialists Different than Typical Gynecologists?
- The Role of Endometriosis Specialists in Treatment
- Finding the Right Doctor for Endometriosis Treatment
- Considerations When Looking for an Endometriosis Specialist
- Red Flags About a Potential Endometriosis “Expert”
- How Can I Find an Endometriosis Specialist Near Me?
What is an Endometriosis Specialist ?
Doctors with extensive experience in treating and caring for patients with this condition are known as endometriosis specialists. They are typically obstetricians and gynecologists (OB/GYNs), which are doctors who treat female pelvic organs, reproductive issues, and deliver babies. Therefore, most endometriosis specialist are also skilled surgeons.
Read more: 7 Ways to Prepare For First Endometriosis Specialist Appointment
How are Endometriosis Specialist Different than Typical Gynecologists ?
Practitioners who specialize in endo care mostly for patients with endometriosis. From surgical treatment to medical management, their guidance is unparalleled to that of a gynecologist who serves general patients. You find endometriosis specialist at large teaching hospitals, medical centers, and private practices with gynecological surgeons.
The Role of Endometriosis Excision Specialist in Treatment
The right specialist will have extensive knowledge of this disorder and the additional surgical training and skills it takes to effectively treat endo and the related conditions. Furthermore, the endo doctor should also have experience with modern techniques and access to state-of-the-art equipment – which often includes robotic or laparoscopic surgical tools. Additionally, openness to complementary treatments and a thorough understanding of various treatments are some other advantages of choosing an endometriosis expert and not just a regular OBGYN.
Patients report the most important thing about a surgeon is that they take their time and carefully listen to you. A good surgeon will pay attention when you speak and not challenge your knowledge or experience.
Read more: Common endometriosis symptoms
Uncommon symptoms of endometriosis
Finding the Right Doctors Who Specialize in Endometriosis
Endometriosis is a painful disorder that affects up to 10% of women. It is caused by cells similar to those in the lining of the uterus growing outside of it, leading to pain and other symptoms such as fatigue, heavy menstrual cycles, and infertility. As endometriosis can be challenging to diagnose and treat, finding the right doctor for your condition is essential for successful treatment. When selecting a doctor for endometriosis treatment, let’s look at what you should consider.
Types of Doctors
When looking for a doctor to treat your endometriosis, consider seeing an experienced OB-GYN or a Reproductive Endocrinologist (RE) specializing in treating fertility problems. An expert OB-GYN can provide surgical options, general care for your reproductive health, and address any issues related to your pain. They may also be able to refer you to an RE if they believe further testing or treatments are necessary.
An RE specializes in diagnosing and treating difficulties with fertility, including endometriosis. They have received specialized training in reproductive medicine, making them uniquely qualified to diagnose and treat endometriosis. Seeing an RE may help you get a more accurate diagnosis and provide access to treatments such as hormone therapy or surgery that can relieve the symptoms of endometriosis and achieve fertility.
Qualities To Look For
When selecting a doctor for endometriosis treatment, there are certain qualities that you should look for to ensure that you are getting the best care possible. Your doctor should have experience treating endometriosis, understand the physical and psychological aspects of living with this condition, and provide comprehensive care from diagnosis through treatment options and follow-up visits.
Choosing the right doctor for your endometriosis treatment is essential for successfully managing this chronic disorder. When selecting a physician, make sure they have experience treating this condition and understand both its physical and psychological components so they can provide comprehensive care from diagnosis through follow-up visits. By doing so, you can ensure that you receive appropriate care explicitly tailored to your needs and get relief from your symptoms to lead a healthier life.
Considerations When Looking for an Endometriosis Specialist
Your endometriosis specialist will be a teammate with the common goal of getting you to living your best life. Ask a lot of questions and listen to the answers. Here are some considerations when looking for an endometriosis expert near you:
- Does the doctor have experience with various medical conditions related to endometriosis?
- Does the doctor specialize in the treatment of adult or adolescent endometriosis? Or both?
- Is the doctor receptive to your information and input? What is their attitude towards your healthcare treatment?
- Does the doctor rush you through assessments and questions, or do they take their time?
- Does the doctor speak to you in terms you understand? (This is particularly important during the explanation of tests and/or surgical procedures.)
- What is the doctor’s belief on the use of hormonal therapies? Do they have medical justifications for prescribing them? Can they tell you the pros and cons of these options?
- Do you feel comfortable speaking with the doctor? Endometriosis pain and symptoms can be hard to discuss, so it’s important you feel at ease.
- Does the doctor work in cooperation with other professionals to offer holistic treatment, (i.e. physical therapists, pain specialists, psychotherapists, gastroenterologists, etc.)?
Red Flags About a Potential Endometriosis Expert
It’s important that you pick an expert who knows what they’re doing to support you. Unfortunately, there are a lot of myths surrounding surgical best practices when it comes to endo treatment. What’s even worse is that some of these options could result in infertility or other issues, and not even address the underlying endometriosis condition.
The following are red flags that could indicate the doctor you are speaking with is not a trusted endometriosis specialist:
Red Flags
- If the doctor views hysterectomy as a definitive treatment. Caution any doctor who says removing your uterus/ovaries will cure you. While this may be the correct course for some patients, it’s not a cure-all solution as endo lesions can affect other body parts and endo tissue could continue to grow.
- If the doctor says endo symptoms will go away with menopause. In medically, naturally, and surgically-induced menopause – there are women who have endometriosis afterward.
- If the doctor says mild stages of endometriosis won’t cause infertility. This is just false. “Mild” or “minimal” stages of endo can still produce significant symptoms, including those that impact fertility.
- If the doctor says that negative tests rule out an endo diagnosis. Tests such as labs, ultrasound, or magnetic resonance imaging (MRI) can help with diagnosing and staging endometriosis, but they cannot rule it out. Technology has advanced, and transvaginal ultrasound can help in assessing and staging endometriosis, however, it cannot rule out the diagnosis. Same is true for MRIs and laboratory studies.
- Hormone therapy will cure endometriosis. Studies show that hormonal medications can help temporarily reduce endometrial lesions, but they do not cure the disease.
- If the doctor suggests that recurring endometriosis cannot be treated.
- If the doctor tells you that you are too young to have endometriosis. This belief is completely false. In fact, there are adolescents who had chronic pelvic pain that were diagnosed with deep infiltrating endometriosis (DIE).
- If the doctor suggests it’s only irritating bowel syndrome (IBS). Many symptoms of endometriosis and IBS overlap. As such, this is often a misdiagnosis given to people who in fact are suffering from endometriosis. Please notice that this doesn’t mean that the patient doesn’t also have IBS in conjunction with endo.
How Can I Find an Endometriosis Specialist Near Me ?
Now that you’ve read more about the importance and what to look for in an endometriosis specialist, are you ready to connect with someone in your area? At iCareBetter, our passion is to connect patients with vetted endo specialists. Go to the directory to learn how we can help you get on the road to health and improve your quality of life.
Top Endometriosis Specialist and Doctor
Endometriosis specialist New York
Endometriosis specialist California
Endometriosis specialist Virginia
Endometriosis Care Process with iCareBetter
1- Find an expert based on keyword/ specialty or state
2- choose your doctor from the list
3- Get the contact info
4- First call and consultation.
5- Get info regarding costs and care process
6- Receive care

What are the First Signs of Endometriosis and Symptoms: Everything You Need to Know
Sharp. Stabbing. Burning. Throbbing. Aching. All these adjectives have been used to describe endometriosis pain. Endometriosis is a condition that, for some women, can cause excruciating uterus pain. Some describe it as feeling like their insides are being pulled out of their bodies. Even worse – pain medication doesn’t cut through or provide relief for many patients with this condition. Therefore, an endometriosis diagnosis can be very serious and life-changing news.
Our commitment to our patients runs deep, and our mission is to help patients with endometriosis pain and other complications find the skilled doctors they need.
Read more: How to Find an Endometriosis Specialist for Diagnosis
As our first introduction to the disorder, we will give you a brief overview of the signs and symptoms of endometriosis, its causes, complications, and treatment options (or, as we like to call it – hope). First, we will give you general information on the disease and cover what endometriosis is.
Table of contents
3- Signs and Symptoms of Endometriosis
5- Complications of Endometriosis
7- Treatment for Endometriosis
8- Surgical Treatment Options for Endometriosis:
10- Find a Vetted Endometriosis Expert
What is the Endometrium?
The endometrium, also known as the endometrial lining, is the tissue that comprises the “wallpaper”, or lining of the uterus. The uterus is the pear-shaped organ that houses a growing baby. During pregnancy and menstruation, the endometrium plays vital functions.
What is Endometriosis?
Endometriosis is pronounced (en-doe-me-tree-O-sis). Endometriosis is a medical condition in which tissue similar to what normally lines the inner walls of the uterus, also known as the endometrium, grows outside the uterus. It is often a very painful, even debilitating disorder. It may involve the ovaries, fallopian tubes, bowels, vagina, cervix, and the tissues that line the pelvis. In rare cases, it can also affect other organs, such as the bladder, kidneys, or lungs.
Signs and Symptoms of Endometriosis
Not all women will experience the same symptoms of endometriosis or degree of intensity/severity. Some women may not experience any symptoms at all.
20 Signs and Symptoms of Endometriosis
It is also important to keep in mind that the severity of symptoms is not a solid indicator of the progress of the disease. There are women with advanced stages of endometriosis who experience no symptoms at all and others with mild cases who endure many. Common endometriosis symptoms include:
- Painful periods, or dysmenorrhea
- Infertility
- Diarrhea during period
- Pain during intercourse
- Heavy or abnormal menstrual flow
- Abdominal or pelvic pain after vaginal sex
- Painful urination during or between menstrual periods
- Painful bowel movements during or between menstrual periods
- Gastrointestinal problems, including bloating, diarrhea, constipation, and/or nausea
Mechanisms of signs and symptoms of endometriosis:
Painful periods (dysmenorrhea)
Cyclic release of multiple inflammatory factors activates nerve fiber growth, leads to cell damage and fibrosis, and exacerbates pain during periods.
Infertility
The overall mechanisms can include tubal blockage, local inflammation, uterine muscle dysfunction, local hormonal alterations, and much more.
Diarrhea during menstrual periods
Diarrhea may result from endometriosis growing directly on the rectal muscle or endometriosis inflammatory substances. Local production of inflammatory molecules can lead to hyper-motility of the sigmoid and rectum muscles, which can manifest as cramping and diarrhea.
Pain during intercourse (dyspareunia)
Endometriosis implants have more nerve endings than usual (hyperinnervated) and can produce pain with pressure. The act of intercourse can apply this pressure on the upper vaginal area and uterosacral ligaments, which are common locations of endo implants. Once this pain occurs and local inflammation further causes tension in the pelvic floor, the muscles surrounding the vagina can contract, which worsens the problem.
Heavy or abnormal menstrual flow
Endometriosis can impact your bleeding by increasing stress from pain or damage to the ovaries, which can change local hormonal function.
Abdominal or pelvic pain after vaginal sex
Uterine and pelvic floor spasms are part of regular orgasms. When these areas are hypersensitive due to endometriosis, spasms lead to continued contractions and pain that lasts for a while. In addition, rectal fusion to the posterior vaginal wall will also cause more direct pain and inflammation by the vaginal area pulling on the rectal wall. Also, as you probably recognize, any event that stirs up the pelvis and causes some trauma leads to increased molecular signaling, further amplifying the problem.
Painful urination during or between menstrual periods (dysuria)
Painful and frequent urination is a prevalent symptom of endometriosis. Endo cells and responding inflammatory cells produce inflammatory molecular signals that aggregate in the area of injury. These molecular signals affect all pelvic organs, including the bladder, leading to bladder wall spasms. Moreover, interstitial cystitis is common in endometriosis patients and can also be a factor. In the worst-case scenario, endo lesions implant inside the bladder, which can also cause cyclic bleeding from the bladder (hematuria).
Painful bowel movements during or between menstrual periods (dyschezia)
Endometriosis causes inflammation and fibrosis or scarring as your body attempts to heal. This inflammation and fibrosis can severely alter the anatomy in the pelvis and distort the rectal course, gluing it to the uterus, cervix, and posterior vaginal wall. This angulation can cause constipation and trouble evacuating stool, while the inflammatory signals cause the rectal muscles to hyper-contract. These mechanisms lead to painful bowel movements, which worsen during the cyclic increases in inflammatory molecules. In the worst-case scenario, the endo will grow through the rectum wall over time, causing cyclic rectal bleeding.
Gastrointestinal problems, including bloating, diarrhea, constipation, and nausea
Generally, intestinal symptoms of endometriosis can be direct or indirect or related to conditions like small intestinal bacterial overgrowth (SIBO). Even if there are no direct implants on the bowel, the endo inside the abdomen and pelvis can cause enough inflammation to irritate the intestine and cause symptoms. In addition, endometriosis implants directly on the bowel can worsen the symptoms.
Join the discussion and discover other stories :
What were your uncommon symptoms of endometriosis?
What were your endometriosis symptoms?
Does Endometriosis Go Away After Menopause?
Causes of Endometriosis
One cause of endometriosis is the direct transplantation of endometrial cells into the abdominal wall during a medical procedure, such as a cesarean section. Besides this known cause of endometriosis, other theories exist as to how it develops:
1. One theory is that during the menstrual cycle, a reverse process takes place where the tissue backs up through the fallopian tubes and into the abdominal cavity, where it attaches and grows.
2. Another theory is a genetic link. This is based on studies that show if someone has a family member with endometriosis, they are more likely to have it as well.
3. Some also suggest that the endometrial tissues travel and implant in other body parts via blood or lymphatic channels, like cancer cells spread.
4. A fourth theory suggests that all cells throughout the body have the ability to transform into endometrial cells.
Complications of Endometriosis
The following are complications of endometriosis if left untreated or in advanced stages of the disorder:
- Infertility/subfertility
- Chronic pelvic pain that can result in disability
- Anatomic disruption of involved organ systems (i.e., adhesions, ruptured cysts, renal failure)
Diagnosis of Endometriosis
The diagnosis starts with assessing signs and symptoms and then performing imaging studies such as MRI and ultrasonography. But the confirmation or exclusion of the endometriosis diagnosis is only possible with surgical biopsy and histopathology. Laparoscopy is the gold-standard surgical modality for diagnosis in all cases.
Treatment for Endometriosis
Endometriosis needs a multidisciplinary team approach for effective and holistic treatment. This team should include the following medical professionals:
- Nutritionist
- Physical therapist
- Endometriosis surgeon
- Mental health therapist
- Pain management specialist
Pain is often the biggest complaint from patients with endometriosis. Therefore, many treatment options are aimed at pain control. So first, here are some options for women to help temporarily ease the pain of endometriosis:
- Exercise
- Meditation
- Breath work
- Heating pads
- Rest and relaxation
- Prevention of constipation
These therapies may be used in combination with medical and/or surgical options to lessen the pelvic pain associated with this disorder. Furthermore, alternative therapies exist that may be used in conjunction with other interventions, and those include but are not limited to:
- Homeopathy
- Immune therapy
- Allergy management
- Nutritional approached
- Traditional Chinese medicine
*Be sure to discuss any of these treatment options with a physician before implementing them.
The Right Medical Treatment For You:
Options for medical and/or surgical treatments for endometriosis are going to depend on several factors, including:
- Desire for pregnancy
- The extent of the disease
- Type and severity of symptoms
- Patient opinions and preferences
- Overall health and medical history
- Expectations of the course of the disease
- Patients’ tolerance level for medications, therapies, and/or procedures
In some cases, management of pain might be the only treatment. In others, medical options may be considered. The following are typical non-surgical, medical treatments for endometriosis:
- “Watch and Wait” approach, where the course of the disease is monitored and treated accordingly
- Pain medication (anything from non-steroidal anti-inflammatory drugs [NSAIDs] to other over-the-counter and/or prescription analgesics)
- Hormonal therapy, such as:
- Progestins
- Oral contraceptives with both estrogen and progestin to reduce menstrual flow and block ovulation
- Danazol (a synthetic derivative of the male hormone testosterone)
- Gonadotropin-releasing hormone antagonist, which stops ovarian hormone production
Surgical Treatment Options for Endometriosis:
Despite their effectiveness in symptom control, pain medications can have significant side effects. Moreover, these medications do not stop the progression of the disease, and symptoms might return once stopped. But on the other side, surgery can lead to long-term relief and can prevent further damage to tissues. Your treatment plan should be a shared decision based on your desires, goals, and abilities.
Almost all endometriosis surgical procedures are laparoscopic or robotic. These are minimally invasive surgeries in which small tubes with lights and cameras are inserted into the abdominal wall. It allows the doctor to see the internal organs and remove endometriosis.
Common procedures include:
Excision of endometriosis:
In this technique, a surgeon cuts out much or all of the endometriosis lesions from the body. Therefore, surgeons avoid leaving any endometriosis lesions behind while preserving normal tissues. This technique is widely adopted by highly skilled endometriosis surgeons who are world leaders.
Ablation of endometriosis:
In this technique, a surgeon burns the surface of the endometriosis lesions and leaves them in the body. Most top experts highly criticize this ablation method. Ablation is most popular with surgeons who have not received enough training to do excision. As a result, these surgeons are not comfortable performing excision, and they do the ablation.
Hysterectomy:
this is a surgery in which surgeons remove the uterus and sometimes ovaries. But, many surgeons consider hysterectomy an outdated and ineffective treatment for endometriosis. Almost all top endometriosis surgeons reject doing it unless there is a clear indication for hysterectomy such as adenomyosis.
Laparotomy:
this surgical procedure cuts and opens the abdomen and does not use thin tubes. Therefore it is more extensive than a laparoscopy. Very few surgeons still do laparotomy because of its complications. Almost none of the top endometriosis surgeons do laparotomy for endometriosis.
Multidisciplinary care
Along with effective surgical treatment, the patient should start working with endometriosis experts in physical therapy, mental health, nutrition, and pain management to achieve the best possible outcome.
Get in touch with Dr. Steve Vasilev
More articles from Dr. Steve Vasilev:
Endometriosis And Menopause: Everything You Need To Know
Understanding the Connection between Endometriosis and Cancer
What would happen to the signs and symptoms of endometriosis after menopause?
Physical Therapy Before Excision Surgery for Endometriosis
Endometriosis can cause multiple issues for patients. And it can create the need for a multidisciplinary care team to address chronic pelvic pain. Physical therapy is one example of part of a multidisciplinary treatment plan for endometriosis symptoms. Guest writer Rebecca Patton, PT, DPT, discusses considerations for using physical therapy while awaiting excision surgery:
Pelvic physical therapy has gained more following and prompted much-needed discussions in recent years. However, pelvic physical therapy looks quite different for someone with chronic pelvic pain and endometriosis.
The reality is that pelvic physical therapists may be the first line of defense to refer a patient to a specialist. First, because we have direct access, meaning a patient can see us for an evaluation before seeing a physician. Second, because symptoms of endometriosis are often missed or dismissed by referring providers. In the latter case, someone may be referred to physical therapy before excision surgery or even before seeing an endo specialist.
Physical therapists can optimize care by helping a patient get to a specialist while providing physical therapy treatment.
If we are seeking to provide the best care available for the treatment of endo, getting a faster diagnosis and referring a patient to an excision specialist is the primary goal. With a thorough medical history including bowel and bladder habits, menstrual symptoms, pelvic pain symptoms, previous treatment, and understanding the patient’s experience, a pelvic physical therapist can create a differential diagnosis list that may include endometriosis. If endometriosis is suspected, a referral to an excision specialist should be given to the patient and explained.
Endo specialists’ wait times vary greatly depending on where you are located.
In my personal experience in Phoenix, AZ, a large metropolitan area with several specialists, it takes anywhere from 3-12 months. More time if we are in the middle of a global pandemic. Decreased access in rural areas may also increase waiting times. One positive change is the inclusion of virtual appointments which may improve access for those in rural areas.
During the waiting period, the goal is to manage pain and maintain some regularity with bowel and bladder habits until excision surgery. Internal pelvic floor retraining may or may not be appropriate during this time.
As mentioned before, physical therapy before excision surgery is going to look different from treatments for other conditions. As a patient, you want to ensure the physical therapist you are seeing treats patients with endo regularly. You may want to consult with them prior about how often they treat patients with endo and what treatments they use specifically. Additional coursework for visceral and abdominal manual therapy techniques, nerve mobilization, and myofascial therapy techniques will be helpful.
Most studies research the effectiveness of physical therapy following excision surgery. What about physical therapy before excision surgery?
Zhao et al. (1) found that 12 weeks of PMR (progressive muscle relaxation) training is effective in improving anxiety, depression, and quality of life of endometriosis patients under GnRH agonist therapy. These participants had not received excision surgery.
Awad et al. (2) found improvements in posture and pain with an 8-week regular exercise program in those diagnosed with mild to moderate endometriosis. This exercise program included posture awareness, diaphragm breathing, muscle relaxation techniques, lower back and hip stretches, and walking. Of note, this exercise program was not vigorous exercise. These participants were also receiving hormonal treatment but not receiving pain medication.
Both studies did not say that physical exercise or PMR plays a role in the prevention of the occurrence or progression of endometriosis. Both studies were short-term (8-12 weeks) and did not explore pain management directly before excision or outcomes after excision.
In the time that a patient is waiting for excision surgery, I believe physical therapy treatment can be effective at minimizing overall pain levels and improving quality of life.
A few factors to keep in mind if you are seeking pelvic physical therapy before excision surgery:
1. Your symptoms after physical therapy should not last more than 1-2 days and should feel manageable. Being bedridden for a week after physical therapy is not a helpful treatment. If you experience this, be sure to communicate it with your physical therapist to adjust the plan. Not all pelvic PTs are experienced with this type of treatment and they may create an exercise plan that is too vigorous.
2. Internal pelvic floor treatment is not always the most helpful in this situation and may exacerbate symptoms. An individualized plan is important to discuss with your provider.
3. You are in charge of your body. If you don’t feel like treatment is working then communicate that to your team and discuss other options. It is always okay to voice your concerns to change the treatment to fit you best.
4. Treatment before surgery requires a multidisciplinary team. This may include other pain management options including medication.
iCareBetter is doing the groundwork to vet pelvic physical therapists.
Rebecca Patton PT, DPT (If you are seeking a pelvic PT, I accept consultations through my website for in person and telehealth appointments: https://www.pattonpelvichealth.com/)
For more resources on physical therapy for endometriosis see: https://nancysnookendo.com/learning-library/treatment/lessons/physical-therapy-resources/
References
Zhao L, Wu H, Zhou X, et al.: Effects of progressive muscular relaxation training on anxiety, depression and quality of life of endometriosis patients under gonadotrophin-releasing hormone agonist therapy. Eur J Obstet Gynecol Reprod Biol, 2012, 162: 211–215. [PubMed] [Google Scholar]
Awad E, Ahmed HAH, Yousef A, Abbas R. Efficacy of exercise on pelvic pain and posture associated with endometriosis: within subject design. J Phys Ther Sci. 2017;29(12):2112-2115. doi:10.1589/jpts.29.2112 [NCBI]

