Exploring the complex world of health and medical conditions can sometimes feel like navigating through a labyrinth. The similarities between certain conditions often blur the lines, making it challenging for individuals and even healthcare professionals to differentiate between them. This is notably true in the case of endometriosis and inflammatory bowel disease (IBD), two disorders that share several overlapping symptoms and characteristics. We’ve recently been discussing endometriosis and the bowel, this article aims to shed light on these conditions, highlighting the differences, similarities, and the challenges faced in their diagnosis.
Table of contents
Symptoms of Endometriosis
The signs and symptoms of endometriosis can vary greatly, making it a complex disease to diagnose. Some of the most common symptoms include dysmenorrhea (painful periods), dyspareunia (painful intercourse), chronic pelvic pain, and gastrointestinal symptoms like diarrhea, constipation, and abdominal pain. Because endometriosis symptoms often overlap with GI symptoms, getting a diagnosis in general can be tricky, but especially if it may be impacting the bowels which is estimated in about 5-12% of cases, whereas approximately 90% of those with endometriosis suffer from gastrointestinal symptoms. In many cases, these symptoms can be mistaken for other conditions, leading to delays in diagnosis.
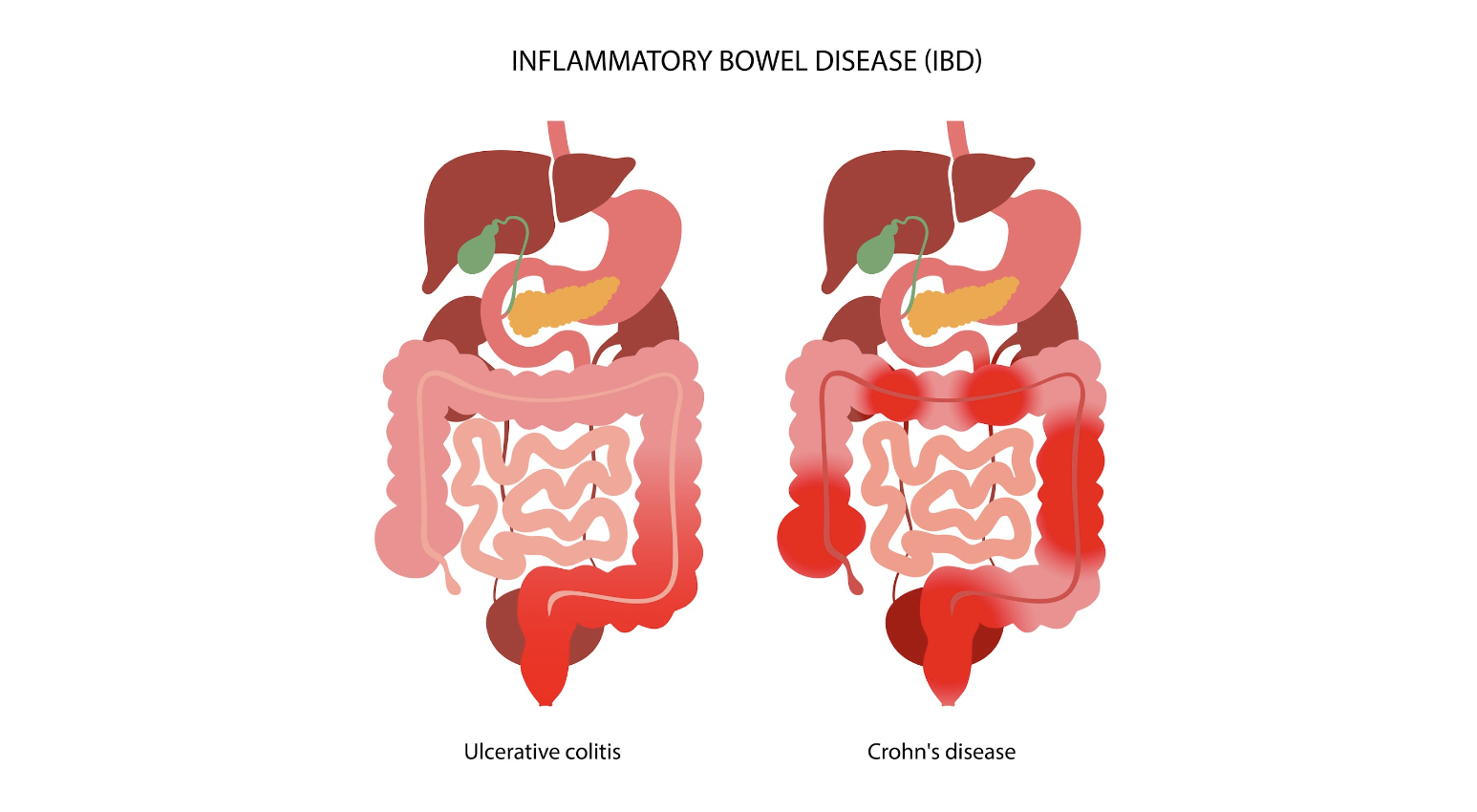
Inflammatory Bowel Disease: An Overview
Inflammatory bowel disease (IBD) is an umbrella term that encompasses two chronic autoimmune disorders: ulcerative colitis (UC) and Crohn’s disease (CD). These conditions are characterized by the chronic inflammation of the gastrointestinal tract, which can lead to a wide range of symptoms, including abdominal pain, diarrhea, weight loss, and fatigue.
The prevalence of IBD is highest in Europe, with reported cases reaching up to 505 per 100,000 for UC in Norway and 322 per 100,000 for CD in Italy. Like endometriosis, IBD can significantly impact an individual’s quality of life, necessitating long-term management strategies to control symptoms and prevent complications.
The Overlap: Endometriosis and IBD
Interestingly, endometriosis and IBD share several common traits, including immune dysregulation and overlapping clinical manifestations like abdominal pain and bowel-related symptoms. This overlap often poses a significant diagnostic challenge, as endometriosis can mimic IBD or vice versa, leading to delays or indeterminate diagnosis.
In fact, endometriosis has often been termed as having “IBD-like” features due to the similarities in symptoms and underlying pathophysiology. This has led to substantial interest in the potential link between these conditions, with several studies investigating the co-occurrence of endometriosis and IBD.
Investigating the Link: Endometriosis and IBD
To understand the potential link between endometriosis and IBD, numerous studies have been conducted, ranging from case reports and clinical series to epidemiological research. These studies have reported varying results, further highlighting the complexity of these conditions and the challenges associated with their diagnosis and management.
Case Reports and Clinical Series
Many case reports have been published that highlight the diagnostic challenges associated with endometriosis and IBD. For instance, several cases have been reported where an initial diagnosis of CD was later revised to intestinal endometriosis upon histopathological examination. Similarly, other case reports have documented instances where an initial diagnosis of UC was later confirmed to be appendiceal endometriosis.
Conversely, there have also been cases where an initial diagnosis of endometriosis was later revised to be CD upon histopathological examination. Additionally, several case reports have documented instances where both CD and endometriosis were diagnosed in the same patient.
Epidemiological Studies
In addition to case reports and clinical series, several epidemiological studies have investigated the co-occurrence of endometriosis and IBD. One such study, a nationwide Danish cohort study, reported a 50% increase in the risk of IBD in women with endometriosis compared to the general population. This increased risk persisted even more than 20 years after a diagnosis of endometriosis, suggesting a genuine association between the two conditions..
Another study, a retrospective cross-sectional study conducted in Israel, found that 2.5% of patients with endometriosis also had a diagnosis of IBD, compared to 1% in the general population. A recent Italian case-control study found that among 148 women with endometriosis, five had IBD, although this did not reach statistical significance.
The Challenge of Temporality
One of the critical aspects of evaluating the association between endometriosis and IBD is the issue of temporality, or the order in which the conditions are diagnosed. Many studies do not provide information on the temporal sequence of endometriosis and IBD, which poses a significant challenge in determining a cause-effect relationship between the two conditions.
Furthermore, the diagnosis of endometriosis often faces delays, with an average delay of seven years estimated between the onset of symptoms and definitive diagnosis. This delay further complicates the evaluation of the temporal relationship between endometriosis and IBD.
Distinguishing Between Endometriosis and IBD
Given the overlapping symptoms and shared characteristics of endometriosis and IBD, distinguishing between these conditions can be challenging. Both conditions can result in similar symptoms, such as abdominal pain and bowel-related symptoms, which can lead to misdiagnosis or delayed diagnosis.
In cases where endometriosis and IBD coexist, the symptoms can be atypical and cyclic, and fibrosis caused by chronic inflammation can lead to obstruction of the intestinal lumen. Therefore, it’s essential for healthcare professionals to consider both conditions when evaluating patients with such symptoms.
In cases of intestinal endometriosis, endoscopic biopsies may reveal IBD-like lesions. However, these lesions may represent an epiphenomenon of endometriosis rather than a true IBD. Hence, patients with concurrent IBD and endometriosis should be adequately followed up for the reassessment of IBD diagnosis over time.
The Role of Treatment in the Risk of IBD
The treatment of endometriosis could potentially influence the risk of developing IBD. For instance, oral contraceptives are a common treatment for endometriosis, and a meta-analysis of 14 studies suggested an increased risk of IBD among users of oral contraceptives. Additionally, non-steroidal anti-inflammatory drugs (NSAIDs), often used for pain relief in endometriosis, have been reported to increase the risk of IBD.
The Need for Further Research
Though existing research has shed some light on the association between endometriosis and IBD, there is still much to uncover. Further research is needed to better understand the temporal relationship between endometriosis and IBD in cases of co-occurrence and identify predictors that could be useful for evaluation and management of these patients.
Understanding these conditions and their potential links can not only improve diagnostic accuracy but also inform treatment strategies and improve the quality of life for those affected.
Distinguishing between endometriosis and inflammatory bowel disease can be a challenging task due to the overlapping symptoms and shared characteristics of these conditions. However, understanding the nuances of these conditions and the potential links between them can lead to improved diagnostic accuracy and more effective treatment strategies. As research progresses in this area, we hope to gain a better understanding of these complex conditions and continue to improve the lives of those affected.
Related Reading:
- Finding an Endometriosis Specialist: Your Guide to Effective Treatment
- Unraveling the Connection Between Endometriosis and Autoimmune Diseases
References:
- Parazzini F, Luchini L, Vezzoli F, Mezzanotte C, Vercellini P. Gruppo italiano perlo studio dell’endometriosi. Prevalence and anatomical distribution of endometriosisin women with selected gynaecological conditions: results from amulticentric Italian study. Hum Reprod 1994;9:1158–62.
- Bulun SE. Endometriosis. N Engl J Med 2009;360:268–79.
- Weed JC, Ray JE. Endometriosis of the bowel. Obstet Gynecol 1987;69:727–30.
- Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology 2012;142:46–54.
- Nielsen NM, Jorgensen KT, Pedersen BV, Rostgaard K, Frisch M. The co-occurrence of endometriosis with multiple sclerosis, systemic lupus erythematosus and Sjogren syndrome. Hum Reprod 2011;26:1555–9.