
Does Endometriosis Cause Bowel Problems
Endometriosis, a chronic medical condition that affects up to 10% of women worldwide, has a significant impact on various aspects of a woman’s life, including
Bowel endometriosis is a form of deep infiltrating endometriosis (DIE) where endometrial-like tissue grows on or within the walls of the bowel, most commonly the rectum, sigmoid colon, and occasionally the small intestine, appendix, or cecum. This condition can cause a wide range of gastrointestinal and pelvic symptoms, often mimicking other disorders like irritable bowel syndrome (IBS) or inflammatory bowel disease (IBD). Because of its complex nature and overlapping symptoms, bowel endometriosis is frequently misdiagnosed or overlooked, delaying effective treatment.
Endometriosis is a chronic condition in which tissue similar to the lining of the uterus (the endometrium) grows outside the uterus, triggering inflammation, scar tissue formation, and adhesions. In the case of bowel endometriosis, these lesions infiltrate the bowel wall, leading to pain, digestive issues, and, in some cases, obstruction. While endometriosis can affect many parts of the body, bowel involvement is one of the most severe manifestations, affecting up to 12% of individuals with endometriosis and often occurring alongside other pelvic or deep infiltrating lesions.
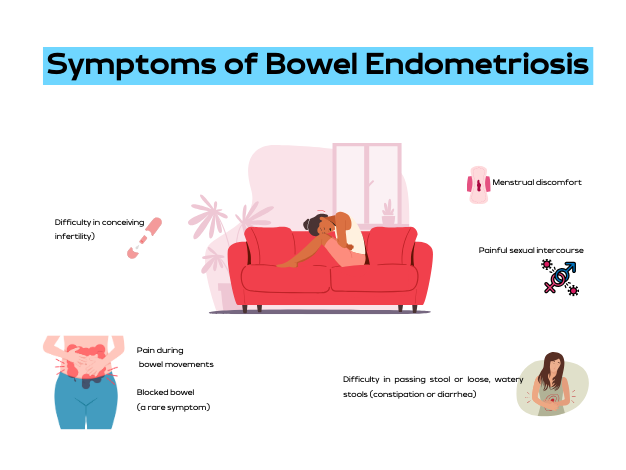
Symptoms of Bowel Endometriosis
The symptoms of bowel endometriosis can be cyclical—worsening during menstruation—or persist throughout the month. This condition is especially tricky to diagnose because it mimics several gastrointestinal and gynecological conditions. Common symptoms include
In some cases, bowel endometriosis can cause partial or complete bowel obstruction, which may require urgent medical or surgical intervention. For individuals trying to conceive, bowel endometriosis may also negatively impact fertility due to inflammation, scarring, and anatomical distortion.
Diagnosing Bowel Endometriosis
Diagnosing bowel endometriosis requires a high index of suspicion, especially in individuals with persistent gastrointestinal and pelvic symptoms that worsen around their menstrual cycle. A thorough history, physical examination, and targeted imaging are critical for accurate diagnosis.
Treatment Options for Bowel Endometriosis
Management of bowel endometriosis depends on the severity of symptoms, the extent of bowel involvement, and the patient’s reproductive goals. A multidisciplinary team including a gynecologist, colorectal surgeon, and radiologist is often needed for optimal care.
When performed by skilled surgeons, laparoscopic excision of bowel endometriosis can significantly improve pain, bowel function, and fertility outcomes.

Endometriosis, a chronic medical condition that affects up to 10% of women worldwide, has a significant impact on various aspects of a woman’s life, including

Endometriosis is a condition affecting roughly 11% of women worldwide, predominantly those of reproductive age. An even more specific form of this ailment is bowel

Bowel endometriosis, a complex and severe variant of endometriosis, is a condition best navigated with a deep understanding of its details. This guide aims to

Endometriosis is a common but often under-recognized condition, primarily affecting women between 15-50. It results from the growth of tissue similar to the endometrium (the
Endometriosis, a common health concern among women, can manifest itself in various ways, one of them being bowel problems. But how exactly can endometriosis cause
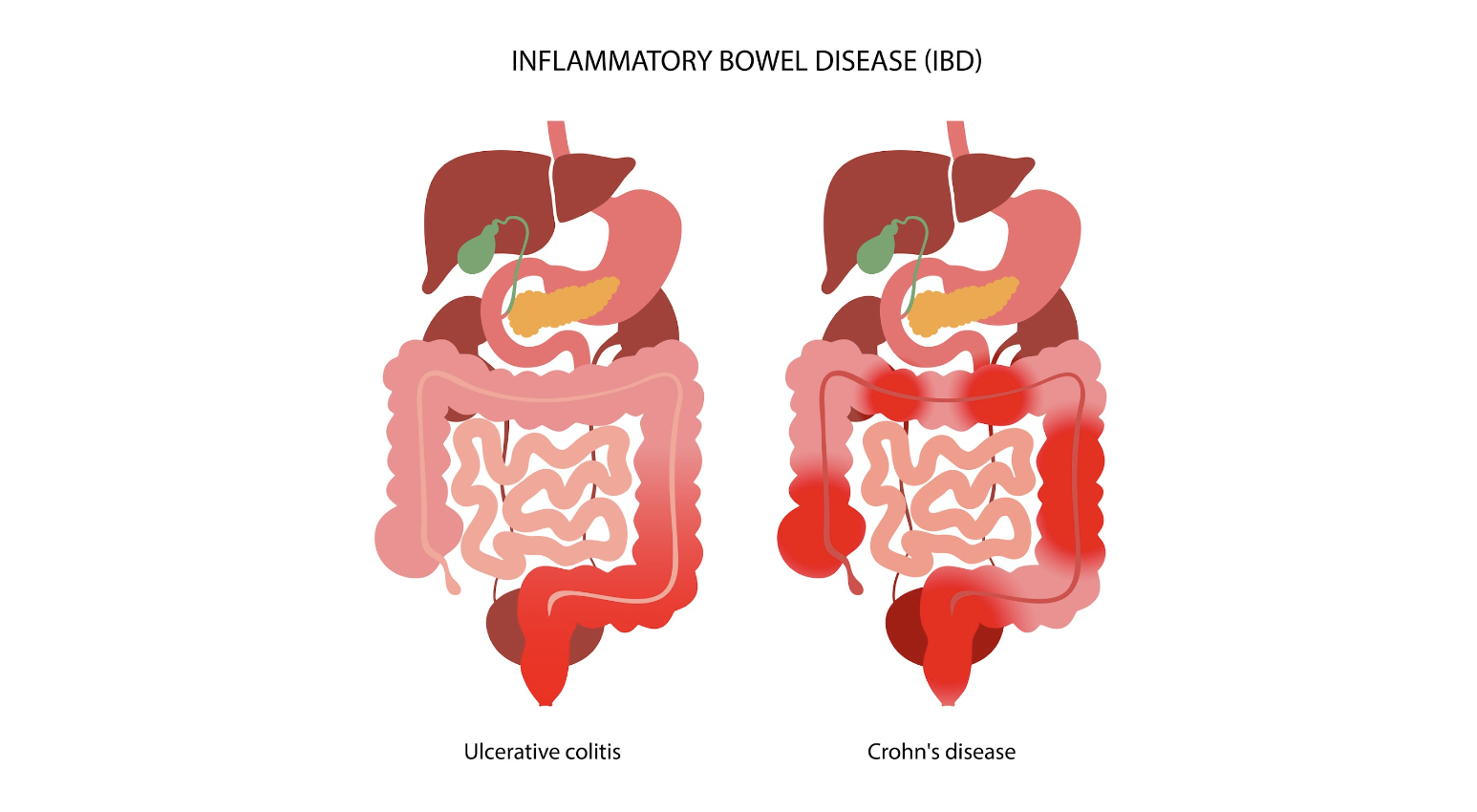
Exploring the complex world of health and medical conditions can sometimes feel like navigating through a labyrinth. The similarities between certain conditions often blur the

In our recent blog, we highlighted the significance of addressing bowel endometriosis, a condition prone to misdiagnosis. Whether individuals have struggled with lifelong bowel issues

Bowel Endometriosis is a debilitating chronic health condition that affects a significant number of women worldwide. This disease is characterized by the growth of endometrial-like

Endometriosis is an often misunderstood condition estimated to affect up to 10% of women. It also affects other gender groups. The primary symptom of endometriosis

Endometriosis is associated with several “digestive complaints, including abdominal pain, bloating, diarrhea, constipation, rectal bleeding, and dyschezia” (Raimondo et al., 2022). Raimondo et al. (2022)
There are different approaches to the surgical management of bowel endometriosis, such as shaving, excision, and resection. Different studies reveal the advantages and disadvantages of the different techniques.
Gastrointestinal (GI) symptoms are common with endometriosis, anywhere from one third to up to 85% of endometriosis patients have GI symptoms, usually with a gradual