Endometriosis is a chronic inflammatory condition that significantly impacts fertility, affecting an estimated 30% to 50% of individuals struggling to conceive. While endometriosis is commonly known for causing pelvic pain, painful periods, and fatigue, one of its most serious effects is its ability to impair reproductive function, even in cases where symptoms may be mild or absent. Understanding how endometriosis affects fertility is critical for those seeking answers on their journey to parenthood.
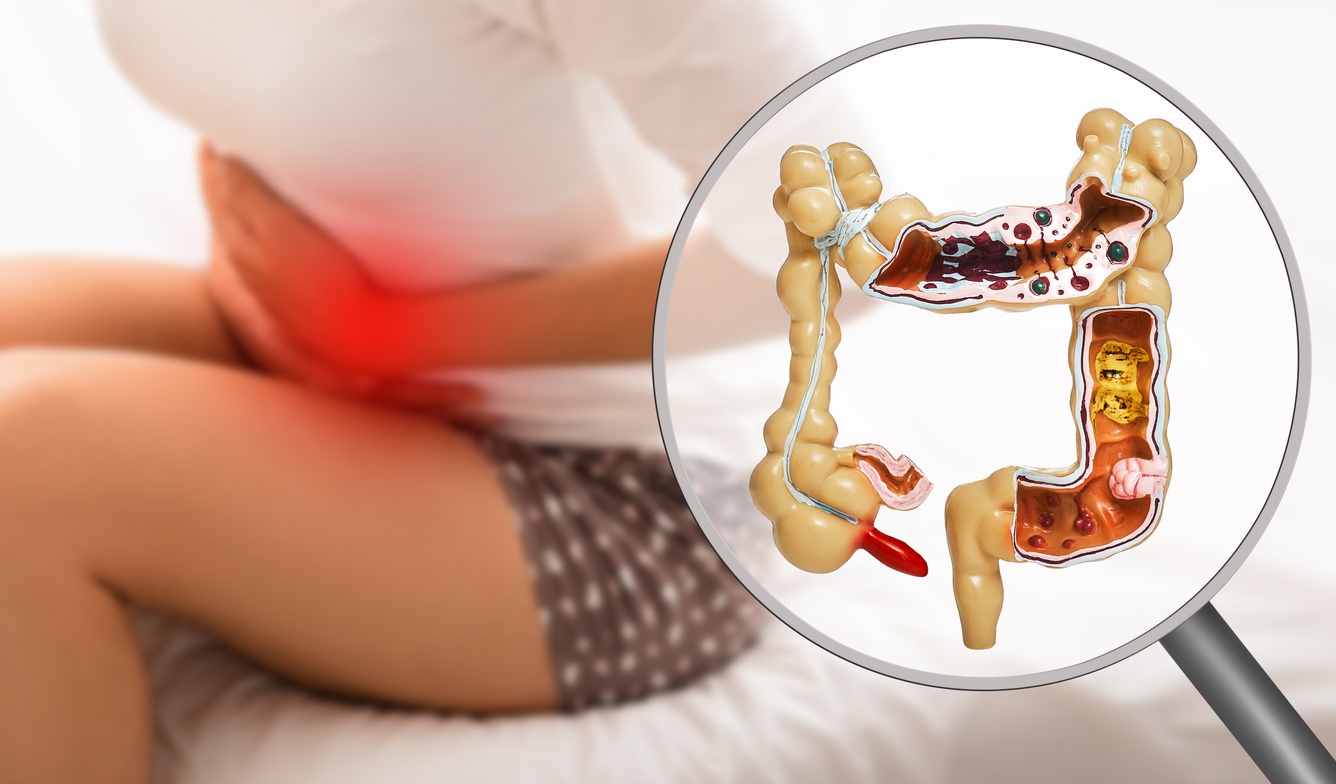
At its core, endometriosis involves the growth of tissue similar to the endometrial lining outside the uterus, often on the ovaries, fallopian tubes, uterus, pelvic walls, bowel, and even beyond. These lesions respond to the menstrual cycle, leading to inflammation, internal bleeding, and the formation of scar tissue and adhesions. Over time, these changes can distort pelvic anatomy, create blockages, and interfere with the delicate processes of ovulation, fertilization, and implantation.
One of the primary ways endometriosis affects fertility is by damaging or blocking the fallopian tubes. When these tubes are obstructed by scar tissue or adhesions, the egg and sperm cannot meet, preventing natural conception. Endometriosis on the ovaries can also lead to the formation of endometriomas—chocolate cysts filled with old blood—that may compromise ovarian function and reduce egg quality and ovarian reserve.
Even when the anatomy appears normal, endometriosis can still interfere with fertility at the cellular level. The chronic inflammation associated with endometriosis alters the pelvic environment, making it hostile to sperm and eggs. It can disrupt hormone signaling, impair follicle development, and affect the endometrial lining, reducing the chances of successful implantation of an embryo.
In some cases, the condition may affect fertility silently, without obvious symptoms, making it particularly frustrating for those experiencing unexplained infertility. Many people only discover they have endometriosis during a fertility workup or while undergoing laparoscopic surgery.
Fortunately, treatment options exist that can improve fertility outcomes for those with endometriosis. Laparoscopic excision surgery to remove endometriosis lesions and restore normal pelvic anatomy has been shown to increase the chances of natural conception, especially in mild to moderate cases. For those with advanced disease or additional fertility factors, assisted reproductive technologies (ART) like in vitro fertilization (IVF) offer a promising path to pregnancy.
Unlike hormonal therapies commonly used to manage pain and suppress endometriosis, fertility-focused treatments are designed to optimize the reproductive process rather than suppress ovulation. Working with a fertility specialist who understands the complexities of endometriosis is crucial for creating a personalized and effective treatment plan.
Endometriosis can pose significant barriers to conception through anatomical damage, inflammation, and hormonal disruption. However, with early diagnosis, expert care, and the right fertility strategies, many people with endometriosis can build the families they dream of. If you’re trying to conceive and suspect endometriosis, seeking prompt evaluation from a specialist is an essential first step toward improved fertility and hope for the future.