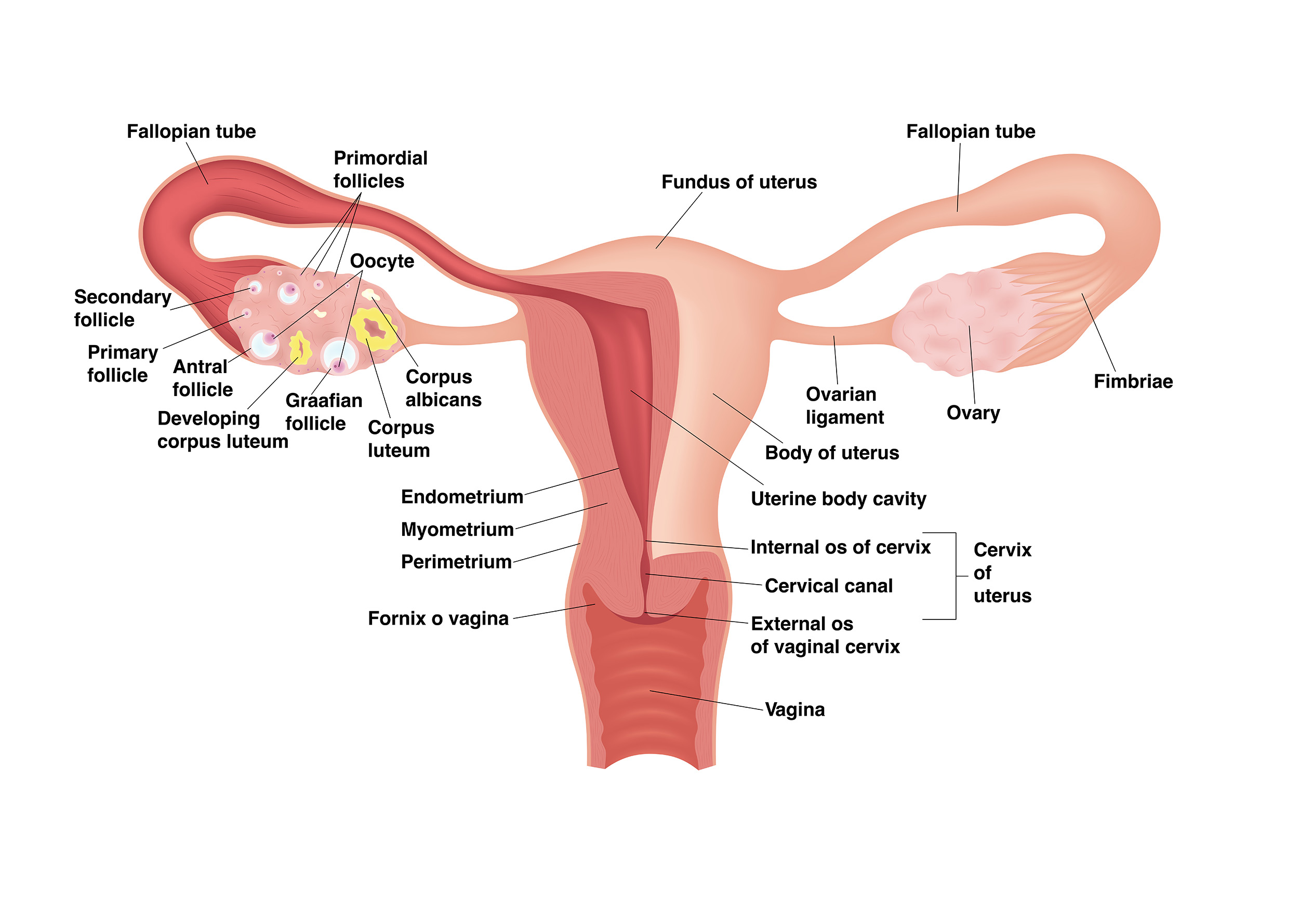
What are endometriomas anyway? Endometriosis is classified into three main types: superficial peritoneal endometriosis, deep infiltrating endometriosis, and endometriomas (see more about that here). Endometriomas are ovarian cysts lined by endometriotic tissue and can be filled with blood (why they are at times called “chocolate cysts”). Like the other types of endometriosis, no one knows for sure how they form. It has been theorized that endometriosis tissue on the surface of the ovary invades and forms a cyst like formation or they start as a functional ovarian cyst with gradual infiltration of endometriotic tissue. Endometriomas have been found in up to 44% of those with endometriosis and are associated with deep infiltrating endometriosis (Cranney, Condous, & Reid, 2017).
Endometriomas can be suspected with ultrasound or MRI, but as with other types of endometriosis, surgery is gold standard for diagnosis (Gałczyński et al., 2019). Endometrioma treatment can often be focused on the effect on fertility, so it is important to consider your goals when looking at treatment options. While medications are used to manage endometriomas, “endometriomas do not respond to medical therapy alone, thus usually surgical treatment is necessary” (Gałczyński et al., 2019). Many may be hesitant to perform surgery for fear of loss of healthy ovarian function and may put off surgery until the endometrioma reaches a certain size. However, Gałczyński et al. (2019) reports that treating “early-stage endometrioma provides less damage to the ovary by a less invasive surgical procedure which decreases the risk of iatrogenic premature ovarian failure” and that “long-term ovarian endometriosis leads to persistent inflammation” that can lead to loss of ovarian function. Skill of the surgeon is important in this aspect.
Gałczyński et al. (2019) reports that “the level of expertise in endometriotic surgery is inversely correlated with inadvertent removal of healthy ovarian tissue along with the endometrioma capsule”. There are multiple surgical techniques that can be used to treat endometriomas and there is no consensus on the best method, although ovarian cystectomy (removal of the ovarian cyst) is the preferred method based on studies (Pais et al., 2021). One recently published study cites “excisional surgery allows for pain resolution, a high rate of spontaneous pregnancies and a lower recurrence rate of ovarian cysts when compared to drainage and ablation techniques” (Angioni et al., 2021).
The aggravating thing about endometriomas is the likelihood of recurrence. It can hard to tell true recurrence rates from studies because “recurrence is variously defined in the literature as the relapse of pain, clinical or instrumental detection of an endometriotic lesion, repeat rise in CA 125 levels, or evidence of recurrence found during repeat surgery,” which results in the wide range of reported recurrence in studies (Ceccaroni et al., 2019). In addition, the method of surgical treatment has a bearing on recurrence rate (excision versus draining etc.). One study reported recurrence rates to be “24.2% for patients aged 20–30 years, 17.7% for 31–40 years, and 7.9% for 41–45 years” (Li et al., 2019). Other studies have echoed that younger age was linked to increased recurrence (Gałczyński et al., 2019). While younger age seems to have a direct correlation with recurrence, other factors not as much. For instance, Gałczyński et al. (2019) reports that the “diameter of the tumor, stage of endometriosis, coexistence of deep-infiltrating endometriosis, or uni- or bi-lateral involvement of ovaries were all not associated with the risk of recurrence” and that the “median time to recurrence was 53 months”.
There is also controversy about the use of hormonal suppression to prevent recurrence. Some studies and a meta-analysis report that there is not enough evidence for the use of medications to help prevent recurrence, while others indicate that it may delay but will not prevent recurrence (Gałczyński et al., 2019; Li et al., 2019; Wattanayingcharoenchai et al., 2021). Confusing? Others agree that it is- with one commentary stating that “so what are we to believe and what should we advise women affected by endometriosis to do?” (Saridogan, 2020). In the end, we each have to do our research, look at our individual goals, and decide what is best for our unique situation.
Endometriosis after a hysterectomy or menopause
References
Angioni, S., Scicchitano, F., Sigilli, M., Succu, A. G., Saponara, S., & D’Alterio, M. N. (2021). Impact of Endometrioma Surgery on Ovarian Reserve. In Endometriosis Pathogenesis, Clinical Impact and Management (pp. 73-81). Springer, Cham. Retrieved from https://link.springer.com/chapter/10.1007/978-3-030-57866-4_8
Ceccaroni, M., Bounous, V. E., Clarizia, R., Mautone, D., & Mabrouk, M. (2019). Recurrent endometriosis: a battle against an unknown enemy. The European Journal of Contraception & Reproductive Health Care, 24(6), 464-474. Retrieved from https://www.tandfonline.com/doi/abs/10.1080/13625187.2019.1662391
Cranney, R., Condous, G., & Reid, S. (2017). An update on the diagnosis, surgical management, and fertility outcomes for women with endometrioma. Acta obstetricia et gynecologica Scandinavica, 96(6), 633-643. Retrieved from https://obgyn.onlinelibrary.wiley.com/doi/full/10.1111/aogs.13114
Gałczyński, K., Jóźwik, M., Lewkowicz, D., Semczuk-Sikora, A., & Semczuk, A. (2019). Ovarian endometrioma–a possible finding in adolescent girls and young women: a mini-review. Journal of ovarian research, 12(1), 1-8. Retrieved from https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-019-0582-5
Li, X. Y., Chao, X. P., Leng, J. H., Zhang, W., Zhang, J. J., Dai, Y., … & Wu, Y. S. (2019). Risk factors for postoperative recurrence of ovarian endometriosis: long-term follow-up of 358 women. Journal of ovarian research, 12(1), 1-10. Retrieved from https://link.springer.com/article/10.1186/s13048-019-0552-y
Pais, A. S., Flagothier, C., Tebache, L., Almeida Santos, T., & Nisolle, M. (2021). Impact of Surgical Management of Endometrioma on AMH Levels and Pregnancy Rates: A Review of Recent Literature. Journal of Clinical Medicine, 10(3), 414. Retrieved from https://www.mdpi.com/2077-0383/10/3/414
Saridogan, E. (2020). Postoperative medical therapies for the prevention of endometrioma recurrence–do we now have the final answer?(Mini-commentary on BJOG-19-1705. R2). Authorea Preprints. Retrieved from https://d197for5662m48.cloudfront.net/documents/publicationstatus/41937/preprint_pdf/d4903f81caf3e8838e672d7631e6b8bd.pdf
Wattanayingcharoenchai, R., Rattanasiri, S., Charakorn, C., Attia, J., & Thakkinstian, A. (2021). Postoperative hormonal treatment for prevention of endometrioma recurrence after ovarian cystectomy: a systematic review and network meta‐analysis. BJOG: An International Journal of Obstetrics & Gynaecology, 128(1), 25-35. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32558987/




comments are closed .