Endometriosis causes pain, multiple bowel symptoms and infertility, among many other debilitating symptoms, in about 10% of women, mostly in the reproductive age range. Developing research has shown that there is a link to various autoimmune conditions.
Table of contents
- Understanding Endometriosis
- The Immune System’s Role
- Is Endometriosis an Autoimmune Disease?
- Systemic Lupus Erythematosus (SLE) and Endometriosis
- Sjögren’s Syndrome (SS) and Endometriosis
- Rheumatoid Arthritis (RA) and Endometriosis
- Autoimmune Thyroid Disorders (ATD) and Endometriosis
- Coeliac Disease (CLD) and Endometriosis
- Multiple Sclerosis (MS) and Endometriosis
- Inflammatory Bowel Disease (IBD) and Endometriosis
- The Bigger Picture
- The Path Ahead
Understanding Endometriosis
Endometriosis is a chronic gynecological disorder characterized by the presence of endometrial-like tissue growing outside the uterus. This means the cells look like those which line the inner part of the uterus but differ markedly in multiple ways at the molecular level. The more we find out the less it is clear what the origins are. However, they are likely partly genetic and partly based on other multiple influences of the environment on your body and genes.
The Immune System’s Role
Research suggests that abnormalities in the immune system may play a key role in the development of endometriosis. These abnormalities could prevent the immune system from effectively clearing ectopic endometrial cells, regardless of how they get there, allowing them to implant and grow outside the uterus. This hypothesis suggests that endometriosis might be, at least in part, an immunity-associated disorder.
Furthermore, endometriosis is often associated with a chronic inflammatory response, triggered by the presence of ectopic endometrial-like cells. This inflammation, coupled with the immune system’s inability to effectively remove ectopic cells, could partly explain the chronic pain often associated with endometriosis.
Is Endometriosis an Autoimmune Disease?
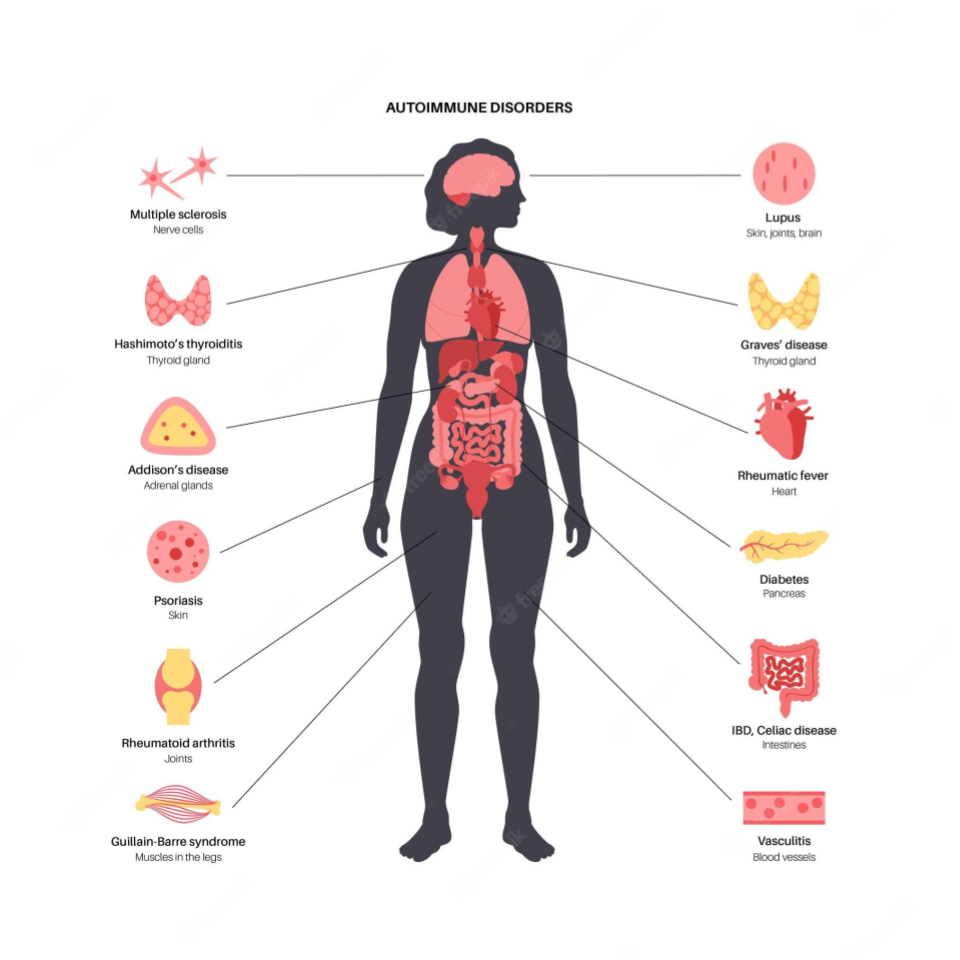
Autoimmune diseases occur when the immune system mistakenly attacks the body’s own cells, viewing them as foreign invaders. The link between endometriosis and autoimmune diseases is still being explored, but multiple studies suggest that women with endometriosis may have a higher risk for certain autoimmune diseases. It is not clear if endo carries a risk of developing autoimmune diseases or if the reverse is true or if they simply share common molecular mechanisms which results in both potentially occurring in any given individual. At this point it is important to stress that an “association” does not mean “cause”.
This review aims to delve into the current state of research on the association if endometriosis is an autoimmune disease. It presents key findings from population-based studies, discusses the potential implications, and highlights areas for future research.
Systemic Lupus Erythematosus (SLE) and Endometriosis
Systemic Lupus Erythematosus (SLE) is an autoimmune disease characterized by inflammation and damage to various body tissues, including the skin, joints, kidneys, and heart. Some studies have suggested a positive association between endometriosis and SLE.
One study suggested a seven-fold increase in the odds of having SLE among women with endometriosis. However, the study relied on self-reported diagnoses, which may introduce bias. A more recent cohort study found a more modest but still significant elevation in SLE risk among women with endometriosis.
Sjögren’s Syndrome (SS) and Endometriosis
Sjögren’s Syndrome (SS) is an autoimmune disorder characterized by dry eyes and mouth, often accompanied by other systemic symptoms. Several studies have investigated the potential link between SS and endometriosis.
A meta-analysis of three case-control studies found a 76% higher odds of SS in women with endometriosis. However, these studies had small sample sizes and wide confidence intervals, indicating a need for further research. Confidence intervals describe the range of results around a measurement which indicate how accurate the conclusion might be. The tighter it is among measurements the better.
Rheumatoid Arthritis (RA) and Endometriosis
Rheumatoid Arthritis (RA) is a chronic inflammatory disorder affecting many joints, including those in the hands and feet. Some studies have suggested a link between endometriosis and an increased risk of developing RA.
One meta-analysis, for example, found a 50% increased risk of RA among women with endometriosis. Again, the studies included in the analysis had limitations, including small sample sizes and wide confidence intervals.
Autoimmune Thyroid Disorders (ATD) and Endometriosis
Autoimmune thyroid disorders (ATDs), including Graves’ disease and Hashimoto’s thyroiditis, occur when the immune system attacks the thyroid gland, leading to either overactivity (hyperthyroidism) or underactivity (hypothyroidism) of the gland.
A meta-analysis of three case-control studies suggested a non-significant increase in the odds of ATD in women with endometriosis. However, the studies had high heterogeneity and low-quality scores, suggesting that further research is needed.
Coeliac Disease (CLD) and Endometriosis
Coeliac disease (CLD) is an autoimmune disorder where ingestion of gluten leads to damage in the small intestine. Some studies have suggested a possible link between endometriosis and CLD.
A meta-analysis of two case-control studies found a four-fold increase in the odds of CLD among women with endometriosis. Again, these studies had small sample sizes and wide confidence intervals, indicating a need for further research.
Multiple Sclerosis (MS) and Endometriosis
Multiple Sclerosis (MS) is a chronic disease that attacks the central nervous system. Current research on the association between MS and endometriosis is limited and inconclusive, with some studies suggesting a possible link while others finding no significant association.
Inflammatory Bowel Disease (IBD) and Endometriosis
Inflammatory bowel disease (IBD), including Crohn’s disease and ulcerative colitis, is characterized by chronic inflammation of the gastrointestinal tract. Some studies indicate a possible association between IBD and endometriosis.
One study found a 50% increase in the risk of IBD among women with endometriosis. However, the study had a small sample size and the confidence interval was wide, indicating a need for further research.
The Bigger Picture
While the evidence for an association between endometriosis and certain autoimmune diseases is compelling, it’s important to emphasize that correlation or association does not imply causation. Further research is needed to determine whether endometriosis actually increases the risk of developing autoimmune diseases or vice versa, or whether the two share common risk factors or underlying mechanisms.
The potential link between endometriosis and autoimmune diseases highlights the importance of a comprehensive approach to women’s health. For women with endometriosis, being aware of the potential increased risk of autoimmune diseases can inform their healthcare decisions and monitoring.
The Path Ahead
The intersection of endometriosis and autoimmune diseases is a complex and evolving field of research. Better understanding the relationship between these conditions could help improve diagnosis, treatment, and ultimately, the quality of life for patients with endometriosis.
By continuing to explore this connection, we are gaining new insights into the pathophysiology of endometriosis and autoimmune diseases, potentially leading to novel treatments and preventive strategies.
Reference: