
Labwork and Blood Tests for Endometriosis
While several companies are working to develop one, there is no single blood test that can definitively diagnose endometriosis yet. It takes a long time to determine if a test has the reliability “so that no patients with actual endometriosis would be missed and no women without endometriosis would be selected for potentially unnecessary additional procedures” (Signorile & Baldi, 2018). Fassbender et al. (2015) notes that such tests might help receive a diagnosis more quickly so that “no women with endometriosis or other significant pelvic pathology are missed who might benefit from surgery for endometriosis associated pain and/or infertility”.
In our Diagnosis section, you can read more about some of the types of blood tests that are under investigation. Other blood tests can be used to rule out other problems and can give an indication to investigate further but are not specific to endometriosis (such as CRP and CA-125). You can also find information in the Diagnosis section about the use of ultrasounds and magnetic resonance imaging (MRI’s) in endometriosis.
“The gold standard for the diagnosis of peritoneal endometriosis has been visual inspection by laparoscopy followed by histological confirmation [7].However, the invasive nature of surgery, coupled with the lack of a laboratory biomarker for the disease, results in a mean latency of 7–11 years from onset of symptoms to definitive diagnosis. Unfortunately, the delay in diagnosis may have significant consequences in terms of disease progression. The discovery of a sufficiently sensitive and specific biomarker for the nonsurgical detection of endometriosis promises earlier diagnosis and prevention of deleterious sequelae and represents a clear research priority….The most important goal of the test is that no women with endometriosis or other significant pelvic pathology are missed who might benefit from surgery for endometriosis-associated pain and/or infertility [17–19].”
(Fassbender et al., 2015, para. 1, 5)

Before and after surgery- tips on preparing
We get a lot of questions about what to expect before and after surgery. On our Resources page, we have added a section on Preparing for Surgery- Pre and Post-Operative.
In the Before Surgery section, you’ll find links to topics such as:
In the After Surgery section, you’ll find topics such as:
- What to Expect in the Weeks After Skilled Excision Surgery
- Managing Expectations Pre- and Post- Op
- Pelvic Therapy Resources
Another often asked question is whether your endo is “coming back” or persisting after surgery. This is a complicated question, but this might help:
Check out the Resources page for more information!

Migraines- overlap of common conditions or close tie to endo?
Both migraines and endometriosis affect a high percentage of the population. Endometriosis affects about 10-15% of the population, while migraines affect >12% of the population (Parasar, Ozcan, & Terry, 2017; Yeh, Blizzard, & Taylor, 2018). So is any association between the two just an overlap of two common conditions? Or is there something that ties the two together?
According to several studies, there is a higher prevalence of migraines in people with endometriosis. One study noted that “the risk of endometriosis was significantly higher in migrainous women” and that “women of reproductive age who suffer from migraine should be screened for endometriosis criteria” (Maitrot-Mantelet et al., 2020). Another study noted a “linear relationship exists between migraine pain severity and the odds of endometriosis” (Miller et al., 2018). One study also attempted to account for the effects of hormones on migraines and endometriosis and found evidence of a “co-morbid relationship between migraine and endometriosis, even after adjusting for the possible effects of female hormone therapies on migraine attacks” (Yang et al., 2012).
Curious about other related conditions? Check out Related Conditions

Bowel Endometriosis Surgical Management
While many individuals have bowel/gastrointestinal symptoms with endometriosis (like diarrhea, constipation, bloating, and pain with defecation), most will not have endometriosis directly on the bowel itself. (See more on bowel endometriosis here). For those that do, there are different approaches to its surgical management.
The different approaches might include shaving, excision, and resection. Studies reveal the advantages and disadvantages of the different techniques- you can read some of those studies here. Most experts express using a team approach (such as involving a colorectal surgeon), using imaging to help guide planning before surgery (with preference for MRI), and decisions based on each individual. Those with more advanced skill in working with bowel endometriosis cite low complication rates. (You can find more on the experts’ opinions in Nancy’s Nook Facebook Group in Unit 2: Surgery).

Genetics of endometriosis: what are the risks?
Is there a genetic component to endometriosis? According to various studies, there is. (You can find links to several of these studies, including the ones below, in Origin Theories of Endometriosis.) This past week someone asked if there is an increased risk if there is a family history on your father’s side. According to this study, there is a “definite kinship factor with maternal and paternal inheritance contributing”.
Another often asked question is how strong is the risk associated within families. According to one study, there is an estimated 5.2 increased risk between sisters and a 1.6 increased risk in cousins. The study also stated that among twins, there was a 51% increased risk. Another study indicated that there is a “sixfold increased risk for first-degree relatives of women with laparoscopically confirmed diagnosis of endometriosis”. Another study indicates a “first-degree relatives of affected women are 5 to 7 times more likely to have surgically confirmed disease”. Yet another study indicated that there is a stronger association with genetic risk for “severe” disease versus “minimal” or “moderate”. (Remember that disease severity in staging is based on the anatomy affected and fertility not necessarily the severity of symptoms- see more about that here.)
While this doesn’t mean a relative will definitely have endometriosis just because you do, it does indicate an increased risk, especially for first degree relatives. There are several genes noted to be involved in endometriosis and several mechanisms on how those genes are expressed in endometriosis. While these studies are paving the way to understanding endometriosis, there is still much to be learned.

What does endometriosis look like? And tips on coping with endometriosis
When looking at endometriosis, it is important to know what it looks like, where it is found, and how it functions. This can affect treatment by knowing how medications may or may not affect it and how surgeons can effectively remove it (by knowing its appearance and where to look for it). This week we added the Many Appearances of Endo and Histology of Endometriosis (what it looks like under a microscope) in order to help you understand what endometriosis looks like. More information about the basics of endometriosis can be found in What Is Endometriosis?.
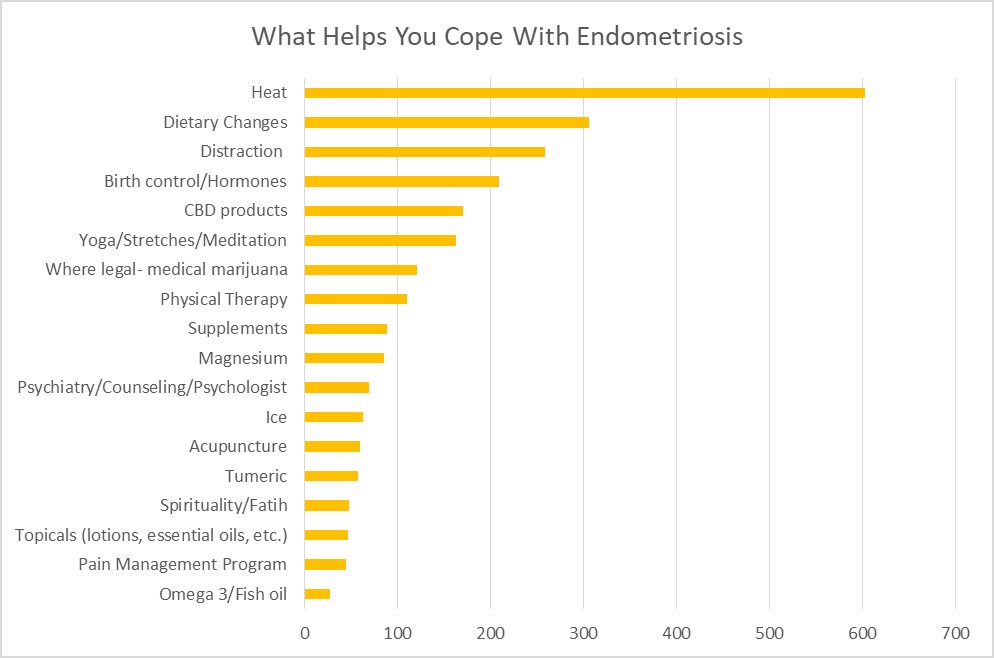
One question that often arises in Nancy’s Nook Facebook group is how to cope with endometriosis while seeking effective treatment. Who better to ask than those who have endometriosis? Several members of the group noted several things that helped them to cope. To date, the most utilized were heat, dietary changes, and distraction. Find out what additional things helped others with endometriosis in Coping with Endometriosis.

Creating an action plan and Staging, Minimal Disease, and DIE
How do you create an action plan for your endometriosis? Where do you start? Start by understanding your disease and knowing your options. This website was created to help you navigate learning about endometriosis. In Endometriosis Action Plan, we show you how to utilize the website and have a directory to the topics currently covered (more is being added so continue to check the website!).
One item added this week to “What is endometriosis” is information about staging, “minimal” endometriosis, and deep infiltrating endometriosis (DIE). Terms about what stage your endometriosis is and what that means can be confusing. Ever been told you have “minimal” disease but think “my symptoms aren’t minimal!”? What does DIE (deep infiltrating endometriosis) really mean? Find out here.
Endometriosis Action Plan
How to use this website
This website is designed to help you navigate learning all you can about the latest research on endometriosis, so that you can make informed decisions about your care. It takes some time, but it is worth doing the work!
- Forget all you’ve been told about endometriosis and look at it with fresh eyes. Many outdated myths about endometriosis are still being perpetuated.
- Start at the beginning and learn what endometriosis is. Also, refer back as needed about more in depth information, such as how endometriosis behaves and how that can influence treatment options. Sometimes further questions remain and you might find more information in our Frequently Asked Questions. The search bar can be helpful as you explore.
- Learn about symptoms. Some you may not have even correlated with endometriosis. Knowing why you have certain symptoms can help understand your disease, better understand treatment options, and be better able to cope with it.
- Learn how other related conditions can mimic or overlap endometriosis symptoms. It’s not always just endometriosis causing problems.
- Learn about how endometriosis is diagnosed (hint- surgery with biopsy confirmation) and how other diagnostic tests can help guide care.
- Learn about your treatment options and latest research to help to make informed choices.
- Research resources that can help you as you learn about endometriosis and navigate your care plan.
- Feel connected with others and know you are not alone on this endometriosis journey.
- Use this information when discussing options with your health care provider. You are your own best advocate!
Looking for something in particular? Using the search bar on the website will be your best option. Below are listed topics as of August 2020:
Nancy’s Nook Website Topics
- What Is Endometriosis?
- Overview
- Origins
- Origin Theories of Endometriosis
- More Evidence Against Reflux Theory of Origin
- Endometriosis Overview
- In depth on endo
- Leptin and its role in endometriosis
- Role of Estrogen Receptor-β in Endometriosis
- Progesterone Resistance in Endometriosis
- Weird places endometriosis has been found
- Random Endometriosis Findings
- Risks of Heart Disease, Perspective on Research
- Symptoms
- Overview
- Additional symptoms
- Additional Symptoms and Symptoms Based on Endometriosis Locations
- Pain
- Introduction: Pain
- Pain with Endometriosis and what influences pain levels
- Pain Associated with Minimal Endometriosis
- Location of endometriosis lesions and where pain may be felt
- Pelvic Floor Dysfunction links
- Pain with Penetration
- Brokengirl: The secret shame of chronic pelvic pain and the unseen consequences of our current care paradigm for endometriosis care
- Sexual Functioning
- Pain with Penetration
- Post coital bleeding
- Bowel/gastrointestinal
- Bowel/GI endometriosis
- Fatigue and Inflammation
- Inflammation with endometriosis
- Inflammatory markers and endometriosis (CRP and CA-125)
- Fatigue in Endometriosis
- Study on Prostaglandin E2 and bacterial growth in endometriosis with response from Dr.Redwine
- Infertility
- Fertility Issues
- Infertility links
- Thoracic (diaphragm)
- Thoracic Endometriosis
- Comments on Thoracic Endometriosis
- Ovaries
- Ovaries and Endometriomas
- Urinary (bladder, ureters, and kidneys)
- Urinary System (Bladder, Ureters, and Kidney)
- Other
- Endometriosis Systemic Effects
- Immune System
- Adhesion Related Information – Articles, Links, and Resources
- Endometriosis and Exercise
- Diagnosis
- Overview
- Surgery
- Ultrasound Use with Endometriosis
- Magnetic Resonance Imaging (MRI’s) and endometriosis
- Clinical diagnosis of endometriosis: a call to action- from AJOG
- Treatment
- Overview
- Treatment
- How is endometriosis treated?
- The Standard of Care is Not Sufficient!
- Surgery
- Why Surgery
- Why excision is recommended
- Endometriosis Appearance and Location: Impact on Surgical Success
- The Cost Effectiveness of Surgical Excision of Endometriosis: an unpublished study
- Should laser vaporization and electrocoagulation of endometriosis be banned
- Robotic Surgery
- Adhesion prevention
- Pelvic Adhesions
- What to Expect in the Weeks After Skilled Excision Surgery
- Managing expectations pre-op and post op
- Medications
- Pain Medications
- Hormonal Medications
- A Quick Guide to Pain Control
- Medication to Prevent Recurrence
- Effects of long term low estrogen states
- Physical Therapy
- “Everyone should do Kegels” and other pelvic floor myths
- Physical Therapy Resources
- Other Therapies
- Pain Management
- Mental Health
- Alternative and Complementary Therapies
- Diet and Nutrition
- Related Conditions
- Overview
- Adenomyosis
- Endometrial/Uterine Polyps
- Interstitial Cystitis/Bladder Pain Syndrome
- Pelvic Floor Dysfunction
- Fibroids
- Polycystic Ovarian Syndrome (PCOS)
- Pudendal Neuralgia & Vulvodynia
- Pelvic Congestion Syndrome
- Occult Hernia
- Resources
- Overview
- Resources
- Choosing your surgeon
- Managing the relationship with your current doctor
- Personal Medical History Template
- Things to pack for the Hospital
- Why Patients Have a Role to Play in Changing the Status Quo of Endometriosis
- Endometriosis The Patient Perspective, AAGL presentation
- Informed Choice Evidence Report: APPG Womens Health from March 2017
- UK Resources
- Australia Resources
- Links, Videos, and Podcasts
- Articles and Website Links
- Podcasts and Videos
- Insurance and Finances
- Tips for Dealing with Insurance
- Insurance: Tricare
- Lack of Endometriosis Surgery Reimbursement in the US links
- Endometriosis affects absenteeism and presenteeism
- Infertility
- Infertility links
- Teens
- Teens and Endometriosis
- Pregnancy
- Pregnancy and Endometriosis
- LGBTQIA+
- LGBTQIA+ Resources
- Transgender and Endometriosis Studies
- Frequently Asked Questions
- Overview
- Is there a link between heart disease and endometriosis?
- What effects can long term low estrogen cause?
- Can endometriosis persist after hysterectomy/ovary removal
- Is There Microscopic or Occult Endometriosis
- Is endometriosis an autoimmune disease? Any association with autoimmune?
- Does endometriosis increase my risk of cancer?
- Patient Stories
- Overview
- Barriers to Care
- Endometriosis: A Husband’s Perspective
- Endometriosis is so much worse than a bad period
- Impact of endometriosis on women’s lives: a qualitative study
- Parenting is Hard, Even Harder with Endometriosis

Support Awareness and Have Fun!
Are you looking to get outside, socially distance, AND support endometriosis awareness? Several organizations have set up Virtual 5K’s that can be done anywhere!
Here are two that are coming up:
August 29, 2020, Anytime, Any Place: Feeling separated from the endometriosis community, Dr. Andrea Vidali and Dr. Sallie Sarrel launched the Endo Summit Virtual 5K. Registrants can walk, run, amble, or saunter their 5K outside or inside to get their custom designed Instagram or Facebook filter medal. Endo Summit 5K masks are also available for purchase.
“We wanted everyone to know, that while treatment and care is on hold or looks different for many, to change life with endometriosis we must stay connected,” says Endometriosis Summit Co-Founder Sallie Sarrel. “Our goal is to raise awareness for endometriosis all over the world.”
To register for the Endo Summit Virtual 5K go to: https://www.theendometriosissummit.com/virtual-5k.html
October 3-12, 2020, Anytime, Any Place: Run to End Endo, normally a road race through Edmonton, moved online making the run accessible to all. Proceeds support The Endometriosis Network, Canada’s first registered charity dedicated to raising awareness of endometriosis and helping those it affects.
The mission of TENC is to promote awareness while providing education, support and resources nationally, for people with endometriosis and those whose lives it touches. The Run to End Endo can be found on Facebook and Instagram @RuntoEndEndo.
To register for the Run to End Endo Virtual 5K go to: https://raceroster.com/events/2020/32531/run-to-end-endo-2020


Endo in weird places, pelvic physical therapy, and FAQ answered
Endometriosis has been found in some strange places. One of the places it is very rarely found is the heart. We recently added to “Weird places endometriosis has been found” two surgical videos of endometriosis being removed from around the heart.
Pelvic physical therapy can be a useful tool in treating symptoms created by endometriosis. We added a few extra resources to understand what pelvic physical therapy entails and how it can help.
Someone recently asked a question about whether you could still get an endometrioma after a hysterectomy. You can find the answer in Frequently Asked Questions: Can endometriosis persist after hysterectomy/ovary removal

New in UK Resources, Inflammation with Endo, and Teens with Endo
In our UK Resources, someone shared with us when you can expect to hear about the surgical findings after you’ve had surgery.
In Inflammation with Endometriosis, we look at how mast cells can affect the inflammatory process in endometriosis.
In Teens and Endometriosis, we added a couple of studies:
- Audebert, A., Lecointre, L., Afors, K., Koch, A., Wattiez, A., & Akladios, C. (2015). Adolescent endometriosis: report of a series of 55 cases with a focus on clinical presentation and long-term issues. Journal of minimally invasive gynecology, 22(5), 834-840. Retrieved from https://pubmed.ncbi.nlm.nih.gov/25850071/
“Adolescent endometriosis is not a rare condition. In our study a familial history was reported in more than one-third of patients. Among those patients treated for DIE, there was a trend for higher rates of recurrences (symptoms or lesions) that required repeat laparoscopy. However, the impact on subsequent fertility appeared to have been limited.”
- Song, X. C., Yu, X., Luo, M., Yu, Q., & Zhu, L. (2020). Clinical characteristics and postoperative symptoms of adolescent endometriosis among 85 cases. Journal of Pediatric and Adolescent Gynecology. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32619717/
“Pelvic pain was the main symptom in adolescent endometriosis and was greatly improved after surgery. It should also be noted that genital malformation may be an important factor in younger adolescent endometriosis.”

Endometriosis: leaving disease behind and calling it something else
The move back to mental health issues and central sensitization issues is dangerous. It gives inadequately trained surgeons tools to abuse patients who still have active disease. Most of the time, the patients we refer on have been dismissed as neurotic, and or told it is cs and they still have improperly treated endometriosis. I know there are pelvic pain conditions that are caused by things other than endometriosis. But when we fail to adequately treat patients and then label them and put them into mental health treatment while ignoring the active disease, we are stepping backward 100 years into the hysterical woman era or even further into the times of ancient Greece.
When the esteemed Prof Shirley Pearce of the UK showed us that abnormal mental states clear with adequate treatment, I find using these “new approaches” of including mental health dx before adequately treating the patient to be misogynist, disrespectful to women, transgender and others. It becomes a tool to abuse patients even further, offering excuses to use drug therapy where skilled surgery is missing.
Now, a large study in China has noted that central sensitization begins to clear in a few short months after pain is relieved with proper surgery. That crutch will soon go away, no, wait, misinformation takes on a life of its own and misleads the industry for decades. The drug companies take advantage of those surgeons who do not have advanced skills by marketing the drug for moderate to severe symptom relief. However, in their own literature, Dr. David Redwine noted that it was not as effective as claimed, but continues to be marketed as an effective tool. If physicians are not reading the fine print and actually asking patients how they are doing, this gets missed. This disease impacts interactions with family, with partners/spouses, with employers, with education efforts, and physicians should be inquiring about how patients are doing in these areas. These poor interactions are not mental health issues, they are PERITONEAL QUALITY PAIN issues, and deserve to be heard and addressed. If the physician does not treat other pelvic pain generators then referring on to pain managers is a compassionate thing to do, or to pelvic PT, or even consider that all endometriosis may not haveall been removed, or has recurred and needs to be addressed. Too often physicians insist on a course of medical suppression and never follow up how the patient is doing. When a group of physicians in Thunder Bay. Ont. thought they were curing endometriosis with triple dose Danazol, I asked the crowd why the doctors believed that? The answer was, “we don’t go back, because they do not believe us.”
Other times physicians will leave disease on the bladder or bowel as insignificant and “treat” it with medical menopause meds. Wrong on many levels as there is no medication that treats endometriosis and low estrogen states occurring thru suppression with drugs has lifelong impact, not immediately acknowledged. Small vessel heart disease, permanent bone loss, and cognitive issues have all been associated with low estrogen states cause by medical menopause (drug induced) or surgical castration. The reasons for such an approach need to be questioned as the drug companies now maintain a speakers bureau of physicians and these physicians are treating patients.
Indeed, these concerns get pushed on down the patient’s life span and once they have occurred, you can’t go back. Those choosing to not excise disease, take the easy way out with suppressive drugs, creating a future of significant health issues for which they accept no current responsibility. Drugs have a role in gynecology, but they do not treat endometriosis and suggesting that they do, is misleading patients.

