The Definitive Guide: Finding the Right Pelvic Pain Doctor
Persistent, unrelenting pelvic pain can be an agonizing and debilitating experience, significantly impacting one’s quality of life. However, navigating the intricate landscape of healthcare providers and specialists can be daunting, especially when seeking relief from this complex condition. This comprehensive guide aims to shed light on the various specialists equipped to address pelvic pain, empowering individuals to make informed decisions and receive the care they deserve.
Understanding Pelvic Pain: A Multifaceted Condition
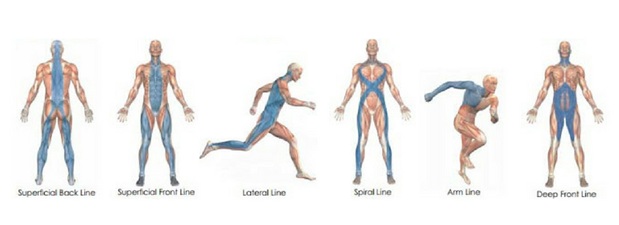
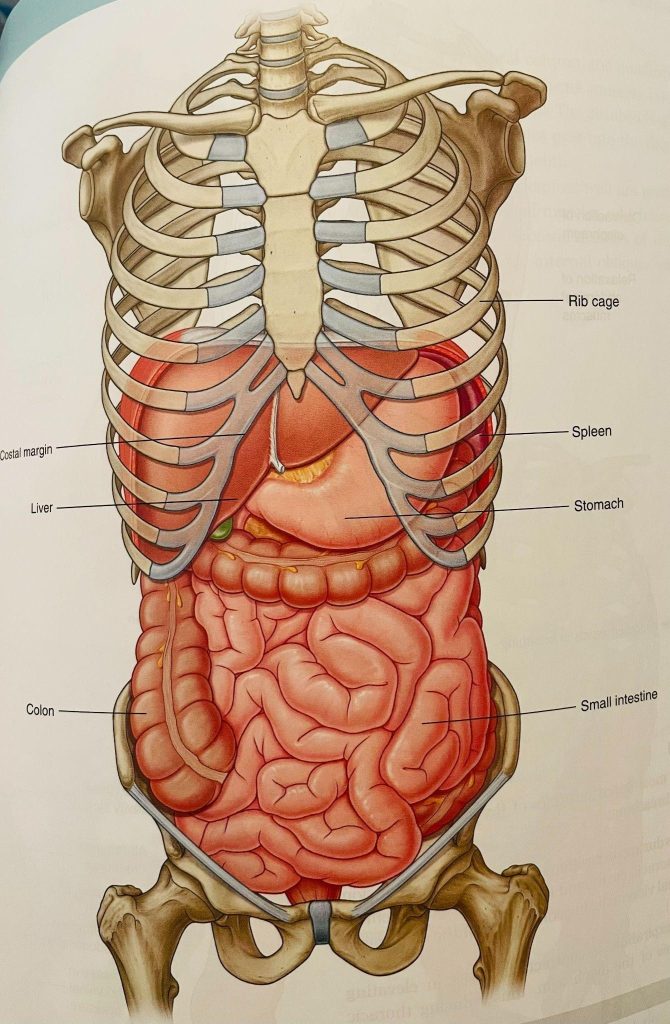
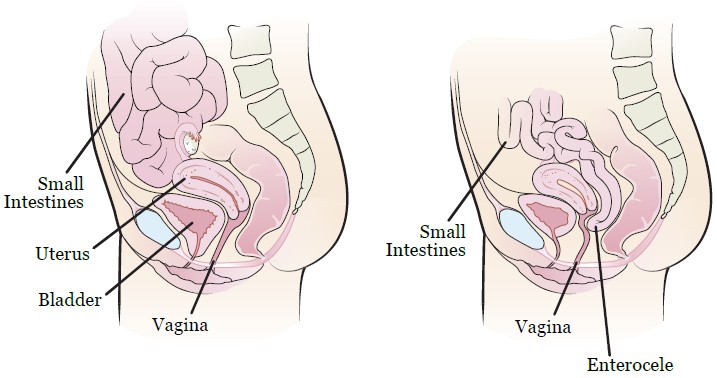
Pelvic pain is a broad term encompassing discomfort or aching sensations within the lower abdominal region, extending from the navel down to the pubic area. This condition can manifest in various forms, ranging from acute, short-lived episodes to chronic, persistent pain lasting six months or longer. The underlying causes of pelvic pain are diverse, often stemming from an intricate interplay between the reproductive, digestive, urinary, and musculoskeletal systems.
Exploring the Spectrum of Pelvic Pain Specialists
When it comes to addressing pelvic pain, a multidisciplinary approach is often required, involving collaboration among various medical professionals. Each specialist brings unique expertise and perspectives, tailoring treatment plans to the specific needs of the individual.
1. Gynecologists: Guardians of Reproductive Health
Gynecologists are medical doctors specializing in the diagnosis and treatment of conditions affecting the female reproductive system. These professionals are well-versed in addressing pelvic pain stemming from conditions such as endometriosis, ovarian cysts, uterine fibroids, and pelvic inflammatory disease (PID). While gynecologists can provide valuable insights and treatment options, they may not be equipped to handle complex or chronic cases of pelvic pain that extend beyond the reproductive system.
2. Urologists: Experts in Urinary and Male Reproductive Health
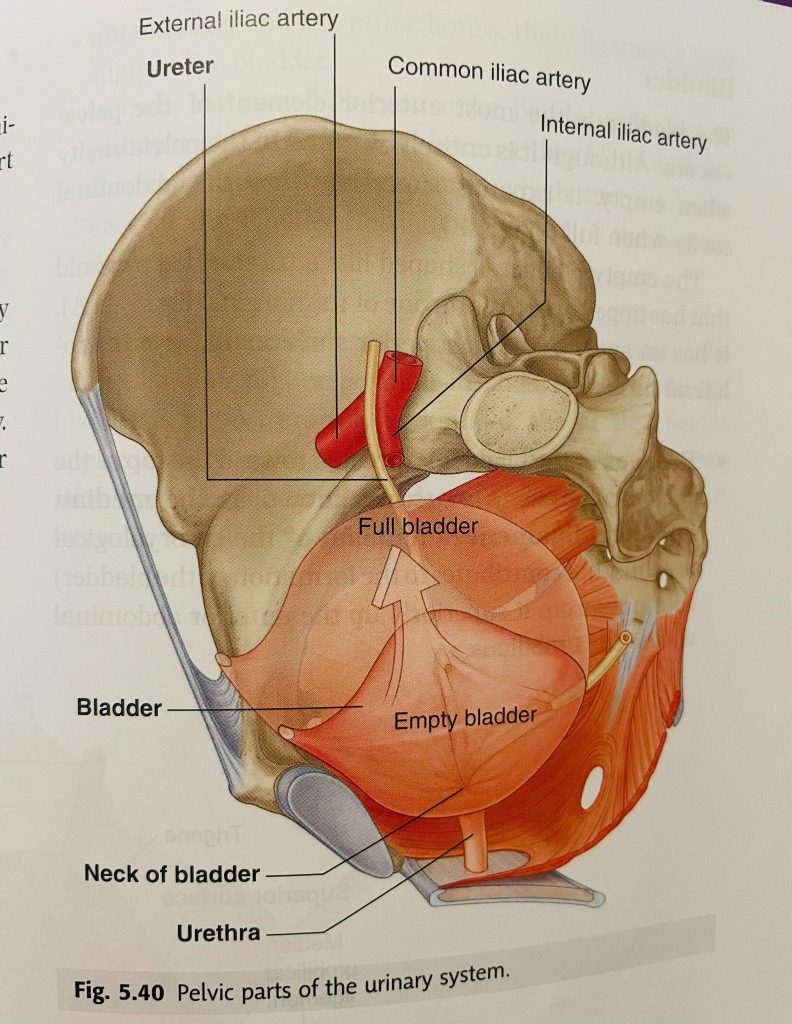
Urologists are medical specialists dedicated to the diagnosis and treatment of conditions related to the urinary tract and male reproductive system. For individuals experiencing pelvic pain associated with conditions like interstitial cystitis, chronic prostatitis, or urinary tract infections, a urologist’s expertise can be invaluable. Additionally, urologists play a crucial role in addressing pelvic pain in men, an often overlooked aspect of this condition.
3. Gastroenterologists: Navigating Digestive System Disorders
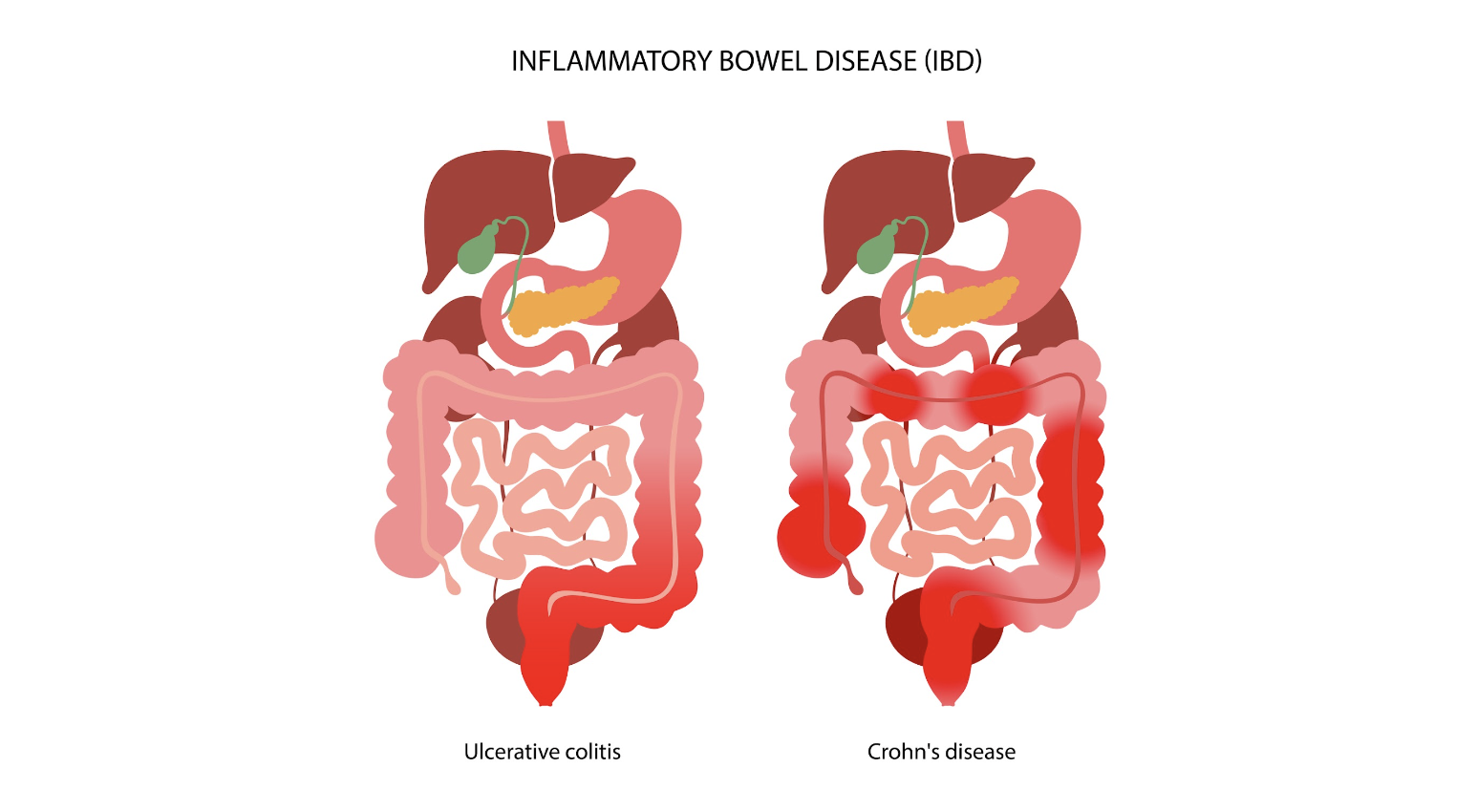
The digestive system can be a significant contributor to pelvic pain, with conditions like irritable bowel syndrome (IBS), diverticulitis, and inflammatory bowel diseases (IBD) frequently manifesting as lower abdominal discomfort. Gastroenterologists, specialists in the diagnosis and treatment of digestive system disorders, can be instrumental in identifying and managing pelvic pain originating from the gastrointestinal tract.
4. Pelvic Pain Specialists: The Comprehensive Approach
While the aforementioned specialists offer valuable insights and expertise within their respective domains, individuals suffering from chronic or complex pelvic pain may benefit from the comprehensive care provided by a pelvic pain specialist. These medical professionals have undergone extensive training in diagnosing and treating a wide range of pelvic pain conditions, taking a holistic approach that considers the intricate interplay between various bodily systems.
Pelvic pain specialists are uniquely equipped to address conditions such as vulvodynia, pudendal neuralgia, hypertonic pelvic floor dysfunction, and persistent genital arousal disorder (PGAD). They employ a multidisciplinary approach, collaborating with other specialists, physical therapists, and mental health professionals to develop personalized treatment plans tailored to each individual’s needs.
Factors to Consider When Choosing a Pelvic Pain Doctor
When seeking medical care for pelvic pain, it is crucial to consider several factors to ensure a positive and effective experience.
1. Expertise and Experience
Evaluate the doctor’s level of expertise and experience in treating pelvic pain conditions. Inquire about their training, certifications, and the number of patients they have treated with similar conditions. Experienced pelvic pain doctors often have a deeper understanding of the complexities involved and may be better equipped to provide comprehensive care.
2. Bedside Manner and Communication
A compassionate and attentive bedside manner can significantly impact the patient-doctor relationship and the overall treatment experience. Look for a pelvic pain doctor who actively listens to your concerns, provides clear explanations, and fosters an environment of trust and open communication.
3. Treatment Approach
Inquire about the doctor’s treatment philosophy and approach to managing pelvic pain. Some may favor a more conservative approach, starting with lifestyle modifications and medications, while others may recommend interventional procedures or surgery when appropriate. Ensure that the doctor’s treatment approach aligns with your preferences and values.
4. Accessibility and Convenience
Consider the doctor’s office location, hours of operation, and availability for appointments. If you require frequent visits or have mobility limitations, choosing a conveniently located practice can make a significant difference in your overall experience.
5. Insurance Coverage and Costs
Before committing to a particular doctor or treatment plan, verify your insurance coverage and understand the associated costs. Inquire about the practice’s billing policies, out-of-pocket expenses, and any available financial assistance programs to ensure that the treatment is accessible and affordable.
Finding the Right Pelvic Pain Doctor Near You
With the abundance of healthcare providers and specialists available, finding the right pelvic pain doctor in your area can be a daunting task. Fortunately, several resources can aid in your search:
- Referrals from Primary Care Physicians: Your primary care physician or gynecologist may be able to provide recommendations for reputable pelvic pain specialists in your area.
- Online Directories and Reviews: Utilize online directories and review platforms to research pelvic pain doctors in your vicinity. Read patient reviews and ratings to gain insights into the doctor’s expertise, bedside manners, and overall patient satisfaction.
- Hospital and Medical Center Websites: Many hospitals and medical centers have dedicated sections on their websites featuring profiles of their physicians, including pelvic pain specialists. These profiles often provide information about the doctor’s qualifications, areas of expertise, and contact information.
- Professional Organizations: Organizations such as the International Pelvic Pain Society (IPPS), the International Society for the Study of Sexual Health (ISSWSH), and the American Urogynecologic Society (AUGS) maintain directories of pelvic pain specialists, which can be a valuable resource in your search.
- Support Groups and Online Communities: Connecting with others who have experienced pelvic pain can provide invaluable insights and recommendations for finding the right doctor. Participate in online support groups or local community organizations to tap into this collective knowledge.
Remember, finding the right pelvic pain doctor may require patience and perseverance. Don’t hesitate to seek second or third opinions until you find a healthcare provider who understands your needs and with whom you feel comfortable.
Preparing for Your Appointment: Empowering Yourself
Once you have identified a potential pelvic pain doctor, it is essential to prepare for your appointment to ensure a productive and informative consultation. Here are some tips to help you get the most out of your visit:
- Keep a Detailed Pain Journal: Document your pelvic pain experiences, including the location, intensity, duration, and any potential triggers or alleviating factors. This information can provide valuable insights to your doctor and aid in accurate diagnosis and treatment planning.
- Compile Medical Records: Gather all relevant medical records, including test results, imaging scans, and previous treatments or medications. Providing your doctor with a comprehensive medical history can facilitate a more informed assessment.
- Prepare a List of Questions: Write down any questions or concerns you may have regarding your condition, treatment options, potential side effects, or lifestyle modifications. An open and honest dialogue with your doctor can lead to a better understanding and more effective treatment plans.
- Consider Bringing a Support Person: Having a trusted friend or family member accompany you to your appointment can provide emotional support and an additional set of ears to help you remember important details discussed during the consultation.
- Be Open and Honest: Pelvic pain can be a sensitive and personal topic, but it is crucial to be open and honest with your doctor about your symptoms, concerns, and any relevant personal or medical history. This transparency can help your doctor provide the most appropriate and effective care.
Conclusion: Embracing a Collaborative Journey
Navigating the complexities of pelvic pain can be a challenging and often frustrating experience. However, by understanding the various specialists available and their areas of expertise, you can take an active role in your healthcare journey. Remember, finding the right pelvic pain doctor may require patience and perseverance, but the rewards of receiving personalized, comprehensive care and relief from your symptoms are invaluable.
Embrace a collaborative approach with your healthcare provider, actively participate in your treatment plan, and don’t hesitate to seek second or third opinions if necessary. With the right support and guidance, you can regain control over your health and reclaim the quality of life you deserve.
REFERENCES:
https://pelvicrehabilitation.com/pelvic-doctor-specialized
https://www.pelvicpaindoc.com/blog/pelvic-pain-specialist-vs-ob-gyn-whats-the-difference
https://www.cvmus.com/blog/female-patient-guide-pelvic-pain-specialists
https://nyulangone.org/doctors/condition/pelvic-pain
http://www.medparkhospital.com/en-US/disease-and-treatment/pelvic-pain

The Autoimmune Protocol for Endometriosis
Navigating Nutrition for Symptom Relief
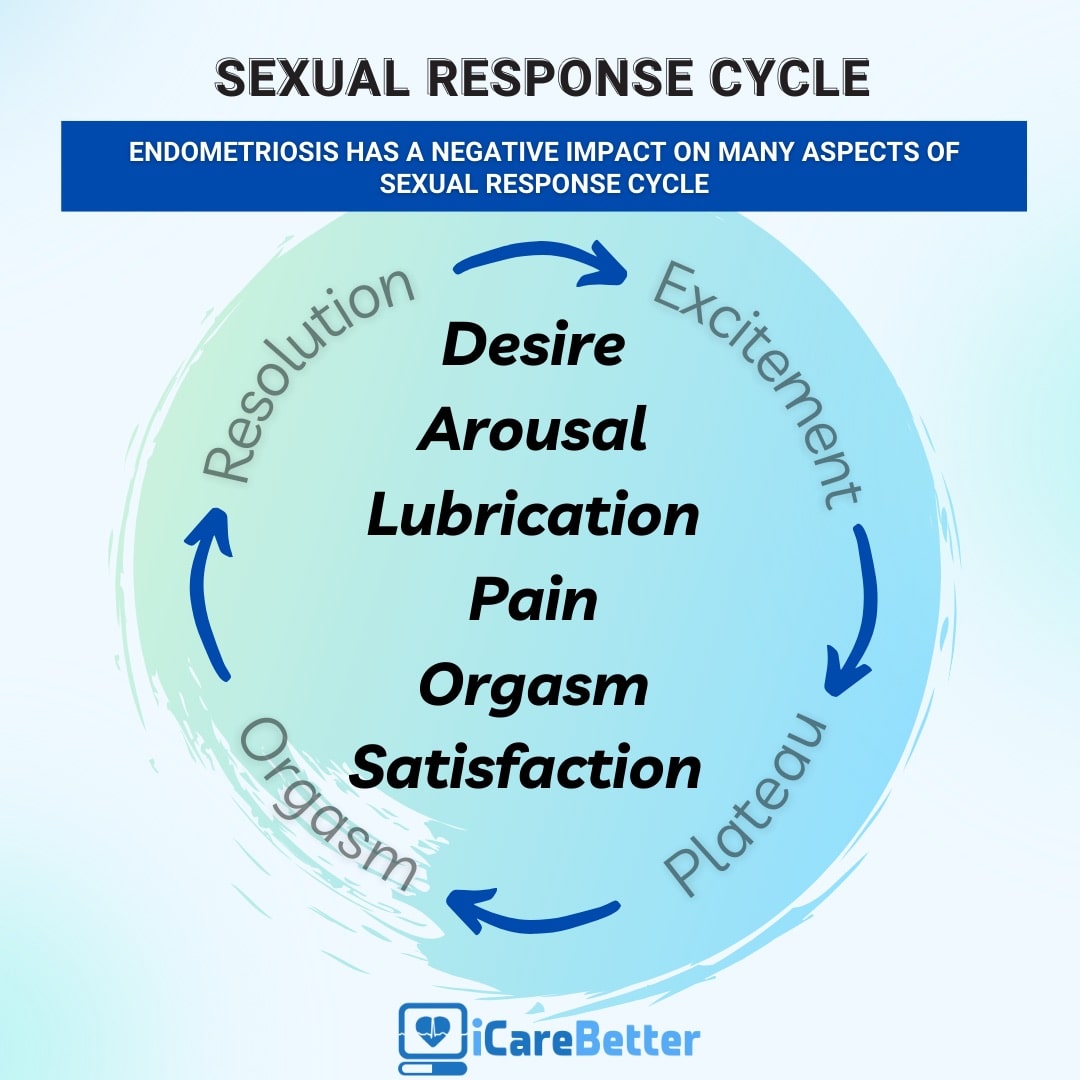
Endometriosis is a challenging condition affecting many women, causing symptoms like painful periods, heavy bleeding, digestive issues, and weight changes. As a registered dietitian specializing in endometriosis and fertility, I understand the importance of finding effective nutrition strategies to alleviate these symptoms. One approach that has gained attention is the Autoimmune Protocol (AIP). Let’s explore what AIP is, which foods are allowed and restricted, how it can impact endometriosis, and its potential impact on food relationships.
Understanding Endometriosis
It’s important to note that endometriosis is not an autoimmune condition; it’s a chronic inflammatory condition where tissue similar to the lining inside the uterus grows outside of it. While some dietary protocols claim to reverse or cure endometriosis, such claims should be considered red flags. Currently, there is no known cure for endometriosis, and excision surgery is regarded as the gold standard of care. However, nutrition can be supportive of managing symptoms and improving quality of life.
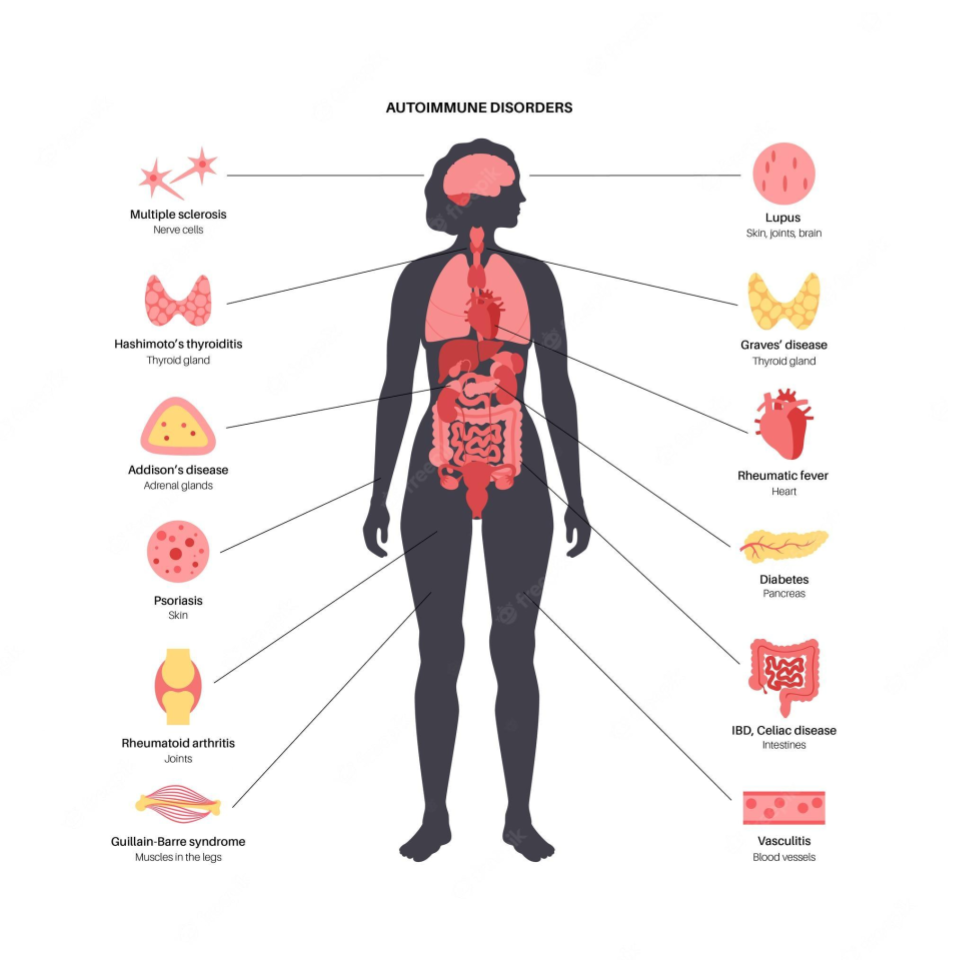
What is the Autoimmune Protocol (AIP)?
The Autoimmune Protocol (AIP) is an elimination diet designed to reduce inflammation, support gut health, and manage autoimmune conditions. Although endometriosis is not an autoimmune condition, the anti-inflammatory principles of the AIP for endometriosis can still be beneficial for symptom management.
Allowed Foods on the Autoimmune Protocol for Endometriosis
Meat and Fish: Grass-fed, pasture-raised, and wild-caught options are preferred. These provide essential amino acids, omega-3 fatty acids, and minerals like zinc and iron.
Nutrients: Omega-3 fatty acids (anti-inflammatory), protein (tissue repair), zinc (immune function), Iron
Vegetables: All non-nightshade vegetables, such as leafy greens, cruciferous, and root vegetables.
Nutrients: Fiber (digestive health), vitamins A, C, and K (antioxidant properties, bone health), folate (cell function).
Fruit: In moderation, focusing on berries and other low-glycemic options.
Nutrients: Vitamin C (immune support), antioxidants (reduce oxidative stress), fiber.
Healthy Fats: Avocado, coconut oil, olive oil, and animal fats from AIP-approved sources.
Nutrients: Monounsaturated fats (heart health), medium-chain triglycerides (energy).
Herbs and Spices: Non-seed-based spices like turmeric, ginger, and garlic.
Nutrients: Curcumin from turmeric (anti-inflammatory), allicin from garlic (antimicrobial).
Fermented Foods: Sauerkraut, kimchi, and kombucha for gut health.
Nutrients: Probiotics (digestive health), vitamins K2 and B12 (bone health, energy metabolism).
Foods Not Allowed on AIP for Endometriosis
Grains: Wheat, rice, oats, and other grains
Dairy: Milk, cheese, yogurt, and butter
Legumes: Beans, lentils, peanuts, and soy
Nightshade Vegetables: Tomatoes, peppers, eggplants, and potatoes
Nuts and Seeds: All types, including nut-based oils
Processed Foods: Any food containing additives, preservatives, and artificial ingredients
Refined Sugars: All forms of processed sugar and artificial sweeteners
Why People with Endometriosis Often Feel Better on AIP
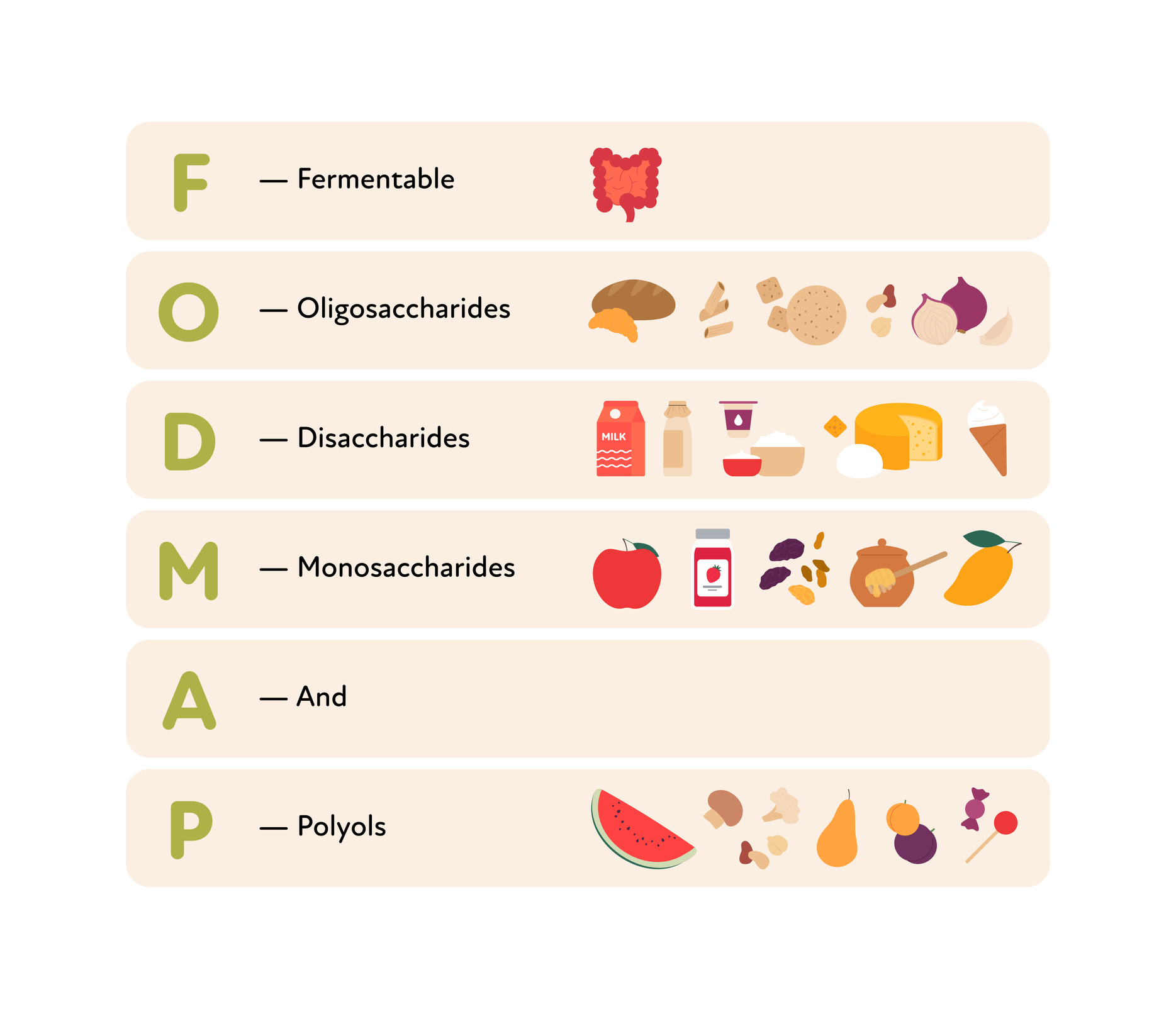
Many people with endometriosis find relief following the Autoimmune Protocol. One way that it may reduce symptoms is by reducing high-FODMAP foods. FODMAPs (Fermentable Oligo-, Di-, Mono-saccharides, and Polyols) are short-chain carbohydrates that can be poorly absorbed in the gut, leading to bloating, gas, and abdominal pain. By removing these foods, AIP can improve gut health and reduce digestive discomfort. Additionally, the AIP diet is rich in omega-3 fatty acids and vitamins A, C, D, and E, all of which have been associated in research with reduced endometriosis pain due to their anti-inflammatory and immune-supporting properties.
The Challenges of Restrictive Nutrition Plans
While the autoimmune protocol for endometriosis can provide relief for some, it is essential to acknowledge the potential pitfalls of highly restrictive diets:
Sustainability Issues: Long-term adherence to restrictive diets can be difficult. People may struggle with social situations, meal planning, and finding suitable food options.
Feelings of Failure: Not being able to stick to a strict diet can lead to feelings of failure, guilt, and decreased self-esteem.
Disordered Eating: Restrictive diets can contribute to disordered eating patterns, such as orthorexia (an obsession with eating “pure” foods) or binge eating.
Eating Disorders: These are serious mental health conditions characterized by unhealthy eating behaviors and attitudes toward food and body image. Examples include anorexia nervosa, bulimia nervosa, and binge eating disorder. Restrictive diets can exacerbate these conditions, leading to severe physical and psychological consequences.
A Balanced Approach: Combining AIP Foods with Flexibility
Incorporating AIP-approved foods can be beneficial in managing endometriosis symptoms due to their anti-inflammatory and nutrient-dense properties. However, it is crucial to maintain a flexible approach:
Personalization: Tailor the AIP framework to individual needs and preferences. Rather than completely eliminating the “not-allowed” list, consider incorporating whole grains, low-fat dairy (lactose-free may be beneficial), and including the nutrient-dense foods the plan recommends regularly.
Balanced Diet: Ensure a well-rounded endometriosis diet by including a variety of foods. Balance is vital to preventing nutrient deficiencies and maintaining a positive relationship with food.
Mindful Inclusion: To maintain a healthy relationship with food and body, honor your hunger and include foods you enjoy regularly. This includes foods with added sugars and processed foods. We know from research that diets don’t work long-term and are associated with poor health outcomes in the long term, weight gain, and bingeing. Rather than restricting these foods, include them when you are hungry for them without guilt, and focus on nutrient-dense foods most of the time.
Conclusion
The autoimmune protocol for endometriosis can offer temporary relief by reducing inflammation and supporting gut health. However, it is vital to approach any restrictive diet with caution, considering long-term sustainability and mental well-being. By focusing on AIP-approved foods while allowing for flexibility and personalization, individuals can find a balanced path to symptom relief and improved quality of life. Remember, diet is one tool in the endometriosis tool kit, but it is not curative, and symptom management often requires a multidisciplinary approach. As always, consult with a healthcare professional or dietitian to tailor dietary strategies to your unique needs and health goals.
Sources:
https://www.sarahraerdn.com/endo-and-ic/autoimmune-Protocol-for-endometriosis
Protocol-for-endometriosis
Arab A, Karimi E, Vingrys K, Kelishadi MR, Mehrabani S, Askari G. Food groups and nutrient consumption and risk of endometriosis: a systematic review and meta-analysis of observational studies. Nutr J. 2022 Sep 22;21(1):58. doi: 10.1186/s12937-022-00812-x. PMID: 36138433; PMCID: PMC9503255.
Barnard ND, Holtz DN, Schmidt N, Kolipaka S, Hata E, Sutton M, Znayenko-Miller T, Hazen ND, Cobb C, Kahleova H. Nutrition in the prevention and treatment of endometriosis: A review. Front Nutr. 2023 Feb 17;10:1089891. doi: 10.3389/fnut.2023.1089891. PMID: 36875844; PMCID: PMC9983692.
Influence of diet on the risk of developing endometriosis. Joanna Jurkiewicz-Przondziono, Magdalena Lemm, Anna Kwiatkowska-Pamuła, Ewa Ziółko, Mariusz K. Wójtowicz. DOI: 10.5603/GP.a2017.0017. Ginekol Pol 2017;88(2):96-102.
Marcinkowska, A.; Górnicka, M. The Role of Dietary Fats in the Development and Treatment of Endometriosis. Life 2023, 13, 654. https://doi.org/10.3390/ life13030654
Barnard, N.D., Holtz, D.N., Schmidt, N., Kolipaka, S., Hata, E., Sutton, M., Znayenko-Miller, T., Hazen, N.D., Cobb, C., & Kahleova, H. (2023). Diet associations in endometriosis: a critical narrative assessment with special reference to gluten. Frontiers in Nutrition, 10. https://doi.org/10.3389/fnut.2023.1166929
Yalçın Bahat P, Ayhan I, Üreyen Özdemir E, İnceboz Ü, Oral E. Dietary supplements for treatment of endometriosis: A review. Acta Biomed. 2022 Mar 14;93(1):e2022159. doi: 10.23750/abm.v93i1.11237. PMID: 35315418; PMCID: PMC8972862.
Amini L, Chekini R, Nateghi MR, Haghani H, Jamialahmadi T, Sathyapalan T, Sahebkar A. The Effect of Combined Vitamin C and Vitamin E Supplementation on Oxidative Stress Markers in Women with Endometriosis: A Randomized, Triple-Blind Placebo-Controlled Clinical Trial. Pain Res Manag. 2021 May 26;2021:5529741. doi: 10.1155/2021/5529741. PMID: 34122682; PMCID: PMC8172324.

Understanding Laparoscopic Surgeries and Scar Management
In an era where medical advancements continually push boundaries, laparoscopic procedures have emerged as a game-changer, offering patients a minimally invasive approach to various surgical interventions. These cutting-edge techniques have revolutionized the way we perceive and experience surgical treatments, minimizing trauma and promoting faster recovery times.
The Laparoscopic Advantage: A Paradigm Shift in Surgical Approach
Conventional open surgeries, while effective, often left patients grappling with significant scarring, prolonged recovery periods, and increased discomfort. Laparoscopic surgeries, on the other hand, have ushered in a new era of minimally invasive procedures, harnessing the power of advanced imaging and precision instruments.
Rather than relying on large incisions, laparoscopic surgeries employ specialized tools and a slender, illuminated instrument called a laparoscope. This remarkable device, equipped with a miniature camera, is inserted through a small incision, enabling surgeons to visualize the internal organs and perform intricate procedures with unparalleled precision.
Scarring Concerns: Addressing a Common Apprehension
Despite the numerous benefits of laparoscopic surgeries, one concern that often weighs on patients’ minds is the potential for scarring. While the incisions made during these procedures are significantly smaller than those of traditional open surgeries, the formation of scars remains a possibility.
However, it is essential to understand that scarring is a natural part of the body’s healing process and is not necessarily an indication of complications or improper surgical technique. In fact, the minimally invasive nature of laparoscopic surgeries often results in less noticeable scarring compared to open procedures.
Scar Formation: Understanding the Healing Process
To appreciate the intricacies of scar management, it is crucial to comprehend the underlying mechanisms of wound healing. When the skin is injured, the body initiates a complex cascade of events to repair the damaged tissue.
The healing process involves several phases, including inflammation, proliferation, and remodeling. During the proliferation phase, new blood vessels form, and collagen fibers are deposited, laying the foundation for scar tissue formation.
Factors Influencing the Appearance of Scars
While scarring is an inevitable consequence of any surgical procedure, several factors can influence the appearance and severity of scars. These include:
- Genetics: An individual’s genetic makeup plays a significant role in determining their propensity for scarring. Some individuals may be more prone to developing hypertrophic or keloid scars, which are characterized by excessive collagen production and raised thickened scar tissue.
- Age: Younger individuals generally have a more robust healing response, which can contribute to more pronounced scarring. As individuals age, their healing capabilities may diminish, potentially resulting in less visible scars.
- Skin Tone: Individuals with darker skin tones may be more susceptible to developing hyperpigmented scars, which can appear darker or lighter than the surrounding skin.
- Wound Healing Factors: Various factors, such as infection, poor nutrition, and underlying medical conditions, can impair the wound healing process and potentially lead to abnormal scarring.
Scar Management Strategies for Laparoscopic Surgeries
While scarring is an inevitable part of the healing process, there are several strategies that can be employed to minimize the appearance of scars following laparoscopic surgeries:
1. Surgical Technique and Incision Placement
Experienced surgeons skilled in laparoscopic techniques often place incisions in strategic locations, such as natural skin creases or areas where scarring is less noticeable. Additionally, careful tissue handling and meticulous surgical techniques can minimize trauma and promote optimal healing.
2. Postoperative Care and Scar Massage
Proper postoperative care is crucial for promoting optimal scar healing. Adhering to your surgeon’s instructions regarding wound care, activity restrictions, and follow-up appointments can significantly impact the appearance of scars.
Scar massage, a technique involving gentle massaging of the scar tissue, can help break down collagen fibers and improve the texture and appearance of scars over time.
3. Topical Treatments and Silicone Sheeting
Various topical treatments, such as silicone-based gels or sheeting, can be applied to scars to help hydrate and flatten them. These products create an occlusive environment, which can promote collagen remodeling and improve scar appearance.
4. Laser Therapy and Injectables
For more stubborn or hypertrophic scars, laser therapy or injectable treatments like corticosteroids may be recommended. These advanced techniques can help reduce scar thickness, improve texture, and address issues like hyperpigmentation or redness.
5. Sun Protection
Protecting scars from excessive sun exposure is crucial, as UV radiation can exacerbate hyperpigmentation and potentially worsen scar appearance. Diligent use of broad-spectrum sunscreen and protective clothing can help minimize these effects.
Embracing the Benefits: Laparoscopic Surgeries and Beyond
While scarring is an inevitable part of any surgical procedure, the minimally invasive nature of laparoscopic surgeries often results in less noticeable scarring compared to traditional open procedures. By understanding the factors influencing scar formation and employing appropriate scar management strategies, patients can optimize their healing outcomes and embrace the numerous benefits that laparoscopic surgeries have to offer.
From faster recovery times and reduced discomfort to improved cosmetic results, laparoscopic surgeries represent a significant advancement in the field of medicine. As technology continues to evolve, we can expect even more innovative approaches to minimize scarring and enhance patient outcomes.
Exploratory Laparoscopy: A Diagnostic Marvel
In addition to its surgical applications, laparoscopy has proven invaluable as a diagnostic tool, enabling physicians to explore and visualize internal organs with remarkable clarity. This exploratory laparoscopy approach has revolutionized the way various conditions are diagnosed and treated, particularly in cases where traditional imaging techniques may not provide sufficient information.
One of the primary advantages of exploratory laparoscopy is its ability to directly visualize organs and tissues, allowing for a more accurate and comprehensive assessment. This can be especially beneficial in diagnosing conditions such as:
- Abdominal or pelvic pain of unknown origin
- Suspected endometriosis or other gynecological conditions
- Gastrointestinal disorders, including inflammatory bowel diseases
- Liver or gallbladder abnormalities
- Potential adhesions or scar tissue formation from previous surgeries
By providing a direct visual examination, exploratory laparoscopy can help identify the underlying cause of symptoms, guide treatment decisions, and even facilitate immediate intervention if necessary.
Minimizing Risks and Maximizing Benefits
While laparoscopic procedures, including exploratory laparoscopy, are generally considered safe and minimally invasive, it is essential to acknowledge and address potential risks. These may include:
- Bleeding or injury to surrounding organs or structures
- Infection at the incision site or within the abdominal cavity
- Adverse reactions to anesthesia or medications
- Potential for conversion to open surgery in case of complications
To mitigate these risks, it is crucial to choose experienced and skilled surgeons who are well-versed in laparoscopic techniques. Additionally, adhering to pre-operative instructions, disclosing relevant medical history, and following post-operative care guidelines can contribute to a smoother recovery process.
Laparoscopy Recovery Time: A Quicker Comeback
One of the most significant advantages of laparoscopic procedures, including exploratory laparoscopy, is the relatively shorter recovery time compared to traditional open surgeries. While recovery times can vary depending on the specific procedure and individual factors, patients typically experience:
- Reduced postoperative pain and discomfort
- Shorter hospital stays, often discharged within a day or two
- Faster return to normal activities and work
- Quicker resumption of regular diet and routine
It is important to note that recovery times can be influenced by factors such as the complexity of the procedure, the patient’s overall health, and adherence to postoperative instructions. However, in general, laparoscopic surgeries offer a more streamlined recovery process, allowing patients to resume their normal lives more quickly.
The Future of Minimally Invasive Procedures
As medical technology continues to advance, the field of laparoscopic surgery and minimally invasive procedures is poised for even greater advancements. Ongoing research and innovation are paving the way for:
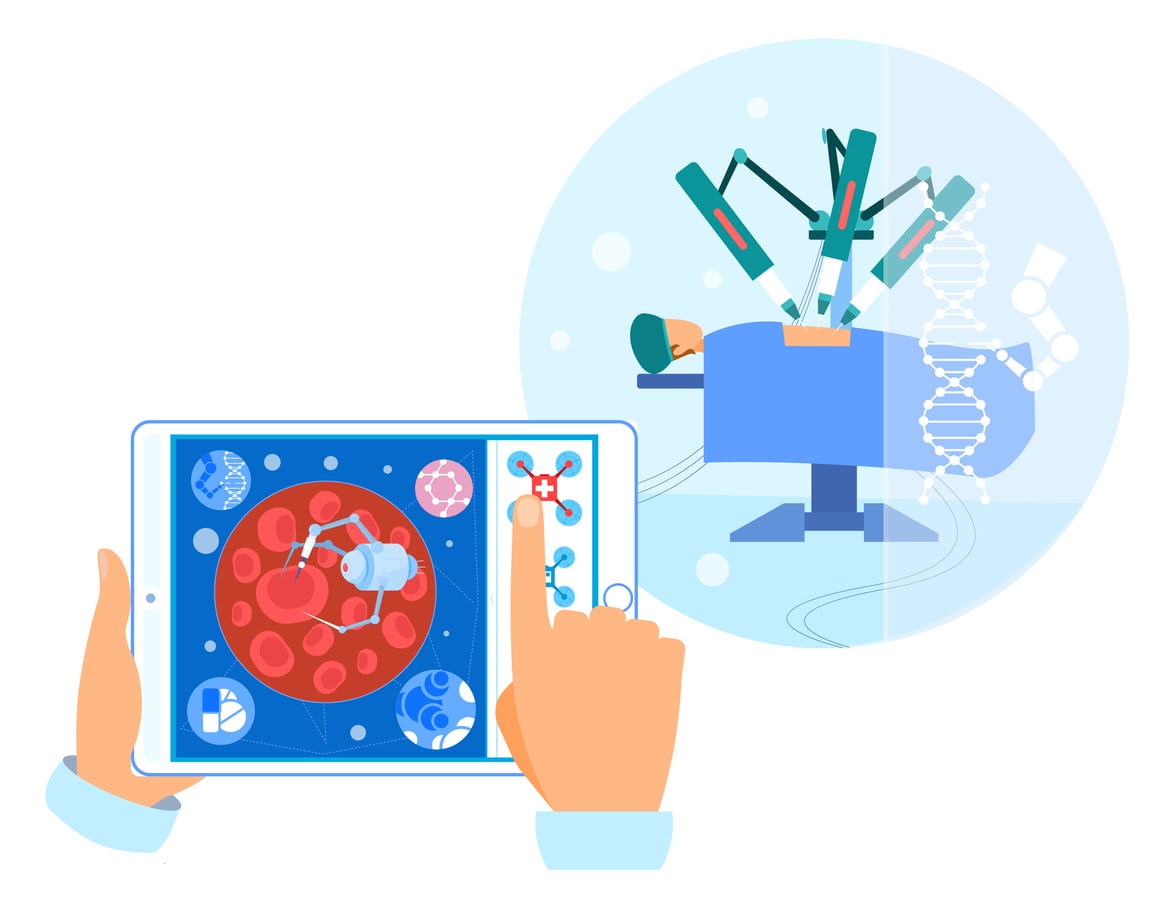
- Robotic-assisted laparoscopic surgeries, enhancing precision and control and better visualization of endometriosis lesions
- Smaller and more advanced laparoscopic instruments
- Improved imaging and visualization techniques
- Incorporation of artificial intelligence and machine learning for surgical planning and guidance
- Development of novel scar management therapies and techniques
These advancements aim to further minimize scarring, reduce recovery times, and improve overall patient outcomes, solidifying the role of laparoscopic procedures as a preferred choice for a wide range of surgical interventions.
Embracing a New Era of Surgical Excellence
The rise of laparoscopic surgeries and minimally invasive procedures represents a significant milestone in the field of medicine, offering patients a path to improved surgical outcomes, faster recovery times, and reduced scarring. As we continue to embrace these cutting-edge techniques, it is essential to stay informed, seek guidance from experienced healthcare professionals, and prioritize personalized care and scar management strategies.
By combining technological advancements with a deep understanding of the healing process and scar formation, we can unlock a new era of surgical excellence, where minimally invasive procedures become the norm, and patients can confidently embark on their journey towards optimal health and well-being.
REFERENCES:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9358567
https://www.allaboutwomenmd.com/knowledge-center/what-is-laparoscopic-surgery.html

How to Find an Expert Endometriosis Specialist?
The Endometriosis Enigma
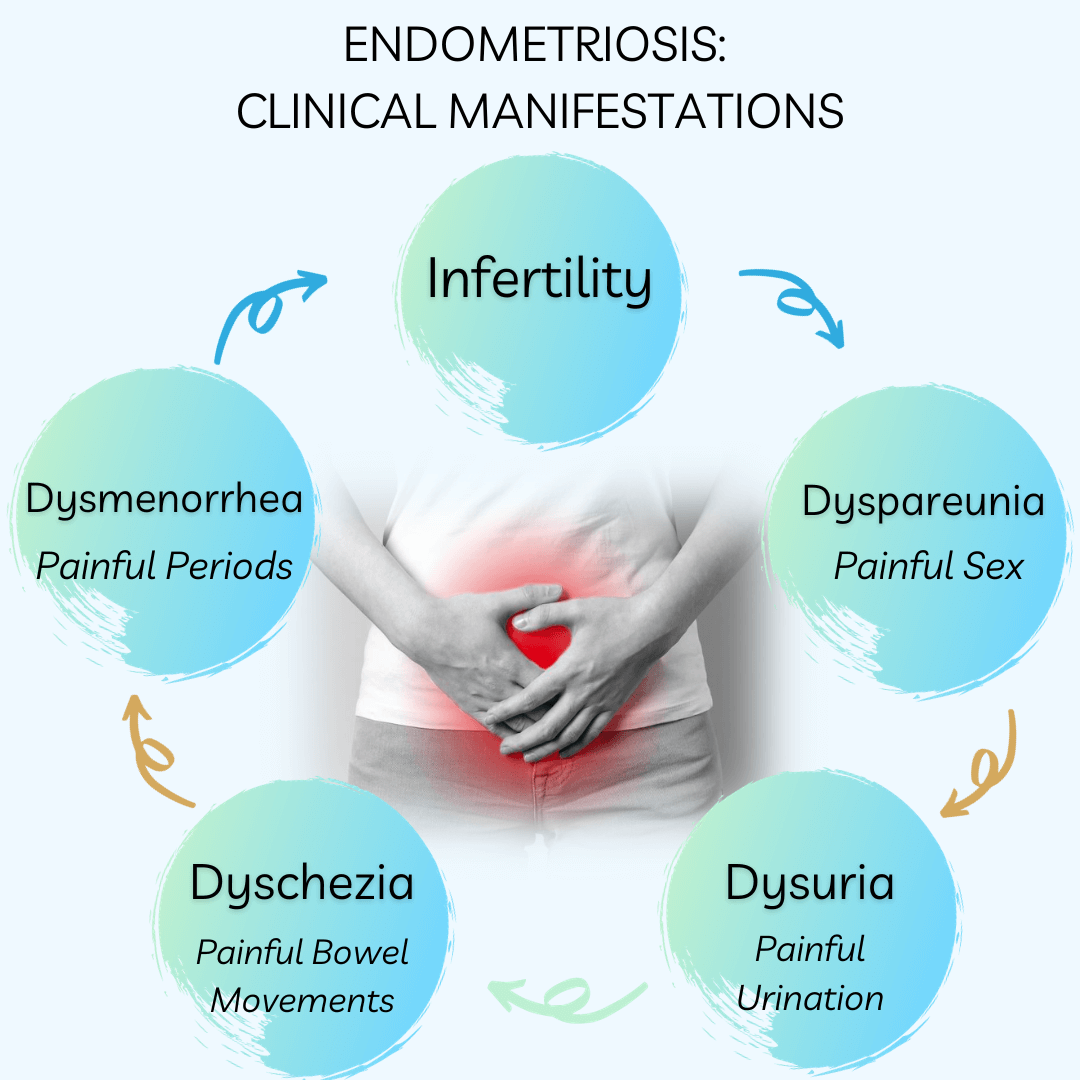
For countless individuals grappling with the perplexing condition of endometriosis, the journey toward finding a knowledgeable and compassionate specialist can be an arduous one. This chronic disorder, characterized by the growth of endometrial-like tissue outside the uterus, often evades timely diagnosis and effective treatment. The debilitating symptoms, encompassing excruciating pelvic pain, heavy menstrual bleeding, and even infertility, can severely impact one’s quality of life.
Navigating the labyrinth of healthcare professionals can be a daunting task, especially when faced with the frustrating reality that many gynecologists lack the specialized training and expertise to accurately identify and manage endometriosis. The absence of a dedicated medical specialty solely focused on this condition further compounds the challenge.
The Pursuit of Expertise
Fortunately, amidst this landscape of uncertainty, a select group of medical professionals have dedicated their careers to unraveling the complexities of endometriosis. These esteemed authorities, often based in larger metropolitan areas or affiliated with teaching hospitals, have emerged as beacons of hope for those seeking relief from the relentless grip of this enigmatic condition.
However, the quest to locate these specialists can be akin to finding a needle in a haystack. With no official designation or certification process, the onus falls squarely on the patient to navigate the intricate web of resources and recommendations.
Leveraging Support Networks
One of the most invaluable resources in this arduous journey is the collective wisdom of endometriosis support groups and online communities. These platforms not only serve as a sanctuary for shared experiences but also as a treasure trove of insights, enabling individuals to tap into the collective knowledge of those who have walked the path before them.
By engaging with these support networks, patients can gain access to a wealth of information, including recommendations for reputable specialists, insights into their treatment approaches, and firsthand accounts of experiences with various healthcare providers.
Consulting Primary Care Physicians
While primary care physicians may not possess the specialized expertise required to treat endometriosis, they can serve as invaluable allies in the quest for specialized care. These healthcare professionals often maintain a network of referrals and can provide guidance on navigating the complexities of the healthcare system.
Harnessing Online Resources
In the digital age, the power of online resources cannot be understated. Organizations such as the Endometriosis Foundation of America and the American Society for Reproductive Medicine offer comprehensive databases and referral services, enabling patients to identify specialists in their vicinity who specialize in the diagnosis and treatment of endometriosis.
Additionally, endometriosis-focused blogs, forums, and social media platforms can serve as valuable repositories of information, providing insights into the experiences of others who have navigated similar journeys.
Vetting Potential Specialists
Once a list of potential specialists has been curated, the process of vetting and selecting the most suitable healthcare provider begins. This critical phase involves a multifaceted approach, encompassing both objective and subjective evaluations.
Key considerations include:
- Expertise and Experience: Assessing the specialist’s specific training, certifications, and extensive experience in treating endometriosis, particularly in complex cases or those involving fertility challenges.
- Treatment Approach: Evaluating the specialist’s philosophical alignment with your preferences and needs, whether it be a focus on medication, surgical interventions, or a holistic, multidisciplinary approach.
- Collaborative Mindset: Determining the specialist’s willingness to engage in a collaborative partnership, valuing your input, addressing your concerns, and fostering an environment of open communication.
- Compassion and Empathy: Gauging the specialist’s ability to exhibit genuine compassion, empathy, and understanding towards the unique challenges and experiences associated with endometriosis.
- Reputation and Reviews: While acknowledging that reputation alone should not be the sole determinant, seeking insights from others who have experienced the specialist’s care can provide valuable context.
Embracing Second Opinions
In the realm of endometriosis care, the pursuit of a second opinion should be viewed not as a sign of doubt but rather as a proactive step toward ensuring the most comprehensive and personalized treatment plan. By consulting multiple specialists, patients can gain a broader perspective, compare treatment philosophies, and ultimately make an informed decision that aligns with their individual needs and goals.
Preparing for the Appointment
Once a specialist has been selected, thorough preparation is key to maximizing the value of the consultation. Gathering comprehensive medical records, documenting symptoms and their impact on daily life, and articulating specific concerns and questions can facilitate productive dialogue and enable the specialist to gain a holistic understanding of the patient’s unique circumstances.
Advocating for Yourself
Throughout this journey, it is imperative for individuals to embrace the role of an active advocate for their own health and well-being. While endometriosis specialists possess invaluable expertise, no one understands the nuances of one’s experiences better than the individual themselves.
Cultivating the confidence to voice concerns, ask probing questions, and respectfully challenge recommendations that do not align with personal beliefs or goals is an essential component of forging a truly collaborative partnership with a healthcare provider.
Embracing a Holistic Approach
While the pursuit of an endometriosis specialist is a critical step, it is essential to recognize that addressing this complex condition often requires a multidisciplinary, holistic approach. Incorporating complementary therapies, lifestyle modifications, and emotional support can enhance the effectiveness of medical interventions and promote overall well-being. By embracing a comprehensive and individualized treatment plan, patients can optimize their chances of achieving lasting relief and regaining control over their lives.
Perseverance and Resilience
The journey towards finding an endometriosis specialist is rarely a linear one. It may be punctuated by setbacks, disappointments, and moments of frustration. However, it is essential to cultivate a mindset of perseverance and resilience, recognizing that the ultimate goal – finding a compassionate and knowledgeable healthcare partner – is worth the effort.
By remaining steadfast in their pursuit, individuals can navigate the challenges with grace and determination, ultimately emerging victorious in their quest for comprehensive care and a better quality of life.
In conclusion, the path to finding an endometriosis specialist is a winding and often arduous one, but it is a journey that holds the promise of relief, understanding, and empowerment. By leveraging the collective wisdom of support networks, harnessing the power of online resources, and embracing a proactive and collaborative approach, individuals can navigate this quest with confidence and emerge victorious in their pursuit of comprehensive care.
REFERENCES:
https://www.endofound.org/preparing-to-see-a-doctor
https://www.everydayhealth.com/endometriosis/finding-endometriosis-expert-what-you-need-know
https://www.elanzawellness.com/post/how-to-find-an-endometriosis-specialist-in-the-us

Decoding the Mystery of Scar Endometriosis
Endometriosis, a perplexing condition where endometrial-like tissue is found outside the uterus, manifests in various forms. Among them is scar endometriosis, a rare yet distressing subtype that warrants heightened awareness and understanding. This is often a consequence of surgical procedures. Scar endometriosis can profoundly impact an individual’s quality of life, necessitating prompt diagnosis and effective management.
Introduction
Scar endometriosis, an extrapelvic manifestation of endometriosis, is characterized by the growth of endometrial-like tissue within or around a surgical scar. While its incidence is relatively low, ranging from 0.03% to 1.08% of endometriosis cases, the symptoms can be just as debilitating and the diagnosis challenging. This article delves into the intricacies of scar endometriosis, shedding light on its causes, symptoms, diagnosis, and treatment options, empowering individuals to navigate this intricate condition with knowledge and confidence.
Etiology: Unveiling the Root Causes
The precise etiology of scar endometriosis remains a subject of ongoing research and debate. However, several theories have been proposed to explain its development:
- Iatrogenic Transplantation: This widely accepted theory suggests that during surgical procedures, endometriosis cells inadvertently become implanted within the surgical incision or scar tissue. This phenomenon is particularly common in obstetric and gynecological surgeries, such as cesarean sections, hysterectomies, and laparoscopic procedures.
- Lymphatic or Vascular Dissemination: Similar to other forms of endometriosis found in the body, these cells may travel through lymphatic or vascular channels, eventually seeding and proliferating within surgical scars or distant sites.
- Metaplastic Transformation: This theory proposes that specialized cells within the surgical scar undergo metaplastic changes, transforming into endometrial-like cells under the influence of specific hormonal or environmental factors.
While these theories provide plausible explanations, the exact mechanisms underlying scar endometriosis remain elusive, underscoring the need for further research to unravel the complexities of this condition.
Clinical Manifestations: Recognizing the Signs
The clinical manifestations of scar endometriosis can vary, making early recognition a challenge. However, certain symptoms may raise suspicion and prompt further investigation:
- Cyclical Pain: One of the hallmark symptoms is cyclical pain or discomfort at the surgical scar site, often coinciding with menstrual periods. This pain can range from mild to severe and may radiate to adjacent areas.
- Swelling or Lump: Many people with scar endometriosis report the presence of a palpable lump or swelling at the scar site. This lump may fluctuate in size and tenderness throughout the menstrual cycle.
- Cyclical Bleeding: In some cases, patients may experience cyclical bleeding or discharge from the surgical scar, further indicating the presence of endometriosis.
- Dysmenorrhea and Pelvic Pain: Scar endometriosis can coexist with pelvic endometriosis, leading to additional symptoms such as dysmenorrhea (painful periods) and chronic pelvic pain, especially if endometriosis has been left untreated.
It is crucial to note that the absence of cyclical symptoms does not necessarily exclude the possibility of scar endometriosis, as some cases may present with non-cyclical pain or discomfort.
Diagnostic Approach: Piecing Together the Puzzle
Diagnosing scar endometriosis can be challenging due to its non-specific symptoms and the need for a multidisciplinary approach. The diagnostic process typically involves the following steps:
- Medical History and Physical Examination: A thorough medical history, including details of previous surgeries, menstrual patterns, and associated symptoms, is essential. During the physical examination, healthcare professionals may palpate the surgical scar site for any palpable masses, nodules, or tenderness.
- Imaging Modalities: Various imaging techniques can aid in the diagnosis and assessment of scar endometriosis:
- Ultrasonography: Ultrasound is often the initial imaging modality employed, as it can detect hypoechoic or heterogeneous lesions with irregular borders at the scar site.
- Magnetic Resonance Imaging (MRI): MRI provides detailed information about the extent and depth of the lesion, aiding in surgical planning.
- Computed Tomography (CT) Scan: While less commonly used, CT scans can help differentiate scar endometriosis from other conditions, such as hernias or malignancies.
- Biopsy and Histopathological Examination: Ultimately, a definitive diagnosis requires a biopsy or surgical excision of the lesion, followed by histopathological examination. The presence of endometrial glands and stroma within the scar tissue confirms the diagnosis of scar endometriosis.
It is essential to note that a multidisciplinary team including gynecologists, radiologists, and pathologists may be necessary to establish an accurate diagnosis and develop an appropriate treatment plan.
Treatment Strategies: Alleviating the Burden
The management of scar endometriosis aims to alleviate symptoms, prevent recurrence, and preserve fertility when desired. The treatment approach is multifaceted and tailored to each individual’s unique circumstances:
- Surgical Intervention: Wide surgical excision with clear margins is the ideal treatment for scar endometriosis. This procedure involves the complete removal of the endometriosis lesion(s), including any affected surrounding tissue or muscle layers. In cases of extensive involvement, abdominal wall reconstruction with mesh reinforcement may be recommended.
- Hormonal Therapy: While not a definitive treatment, hormonal therapies such as oral contraceptives, progestins, or gonadotropin-releasing hormone (GnRH) agonists can provide temporary symptom relief, and some research shows that these therapies may suppress the growth of lesions. However, these medications may have side effects and do not address the underlying lesion.
- Combined Approach: In some cases, a combined approach involving surgical excision followed by adjuvant hormonal therapy may be recommended and may reduce the risk of recurrence.
- Pain Management: Effective pain management strategies, including the use of non-steroidal anti-inflammatory drugs (NSAIDs) or other analgesics, may be necessary to alleviate discomfort associated with scar endometriosis.
It is crucial to engage in shared decision-making with healthcare professionals, weighing the risks and benefits of each treatment option to determine the most appropriate course of action.
Preventive Measures: Minimizing the Risk
While the complete prevention of scar endometriosis may not be feasible in all cases, certain measures can be taken to reduce the risk of its development:
- Meticulous Surgical Technique: During surgical procedures, particularly those involving the uterus or pelvic region, strict adherence to meticulous surgical techniques is paramount. This includes minimizing the risk of cell seeding, proper handling of surgical specimens, and thorough irrigation of the surgical site.
- Containment of Tissue Biopsies: The use of endo-bags or containment devices during laparoscopic procedures can help prevent the inadvertent dissemination of endometriosis cells into the surgical field.
- Careful Wound Closure: Ensuring proper closure of the peritoneum and fascial layers during abdominal surgeries can help minimize the risk of endometriosis cell implantation within the surgical site.
- Postoperative Monitoring: Regular follow-up and vigilance for any signs or symptoms of scar endometriosis in the postoperative period can aid in early detection and prompt management.
While these preventive measures cannot guarantee the complete elimination of scar endometriosis, they can contribute to reducing the risk and promoting better outcomes for patients undergoing surgical procedures.
Psychological Impact and Support
Scar endometriosis can have a profound impact on an individual’s psychological well-being, often leading to feelings of frustration, anxiety, and diminished self-esteem. The chronic pain, discomfort, and potential impact on fertility can take a toll on mental health, underscoring the importance of holistic care and support.
Healthcare professionals should be attuned to the psychological needs of patients with scar endometriosis and provide access to counseling, support groups, or mental health resources as needed. Building a strong support system and fostering open communication can empower an individual to cope with the challenges of this condition more effectively.
Fertility Considerations
For individuals desiring fertility, the impact of scar endometriosis on fertility is a significant concern. While the condition itself may not directly affect fertility, the presence of pelvic endometriosis or the surgical interventions required for treatment can potentially impact fertility outcomes.
In such cases, a multidisciplinary approach involving reproductive endocrinologists and fertility specialists may be necessary. Fertility preservation techniques, such as egg or embryo freezing, may be considered for people undergoing extensive surgical procedures. Ongoing monitoring and tailored treatment plans can help optimize fertility outcomes for those affected by scar endometriosis.
Emerging Treatments and Research Frontiers
While current treatment modalities for scar endometriosis have shown promising results, ongoing research efforts aim to further enhance our understanding and management of this condition. Some emerging areas of interest include:
- Targeted Therapies: The development of targeted therapies that selectively inhibit the growth or proliferation of endometriosis could potentially offer more effective and less invasive treatment options.
- Stem Cell Therapy: Preliminary research explores the potential of stem cell therapy in regenerating or repairing damaged tissue, potentially reducing the need for extensive surgical interventions.
- Genetic and Molecular Studies: Investigating the genetic and molecular mechanisms underlying scar endometriosis could provide insights into its pathogenesis and pave the way for personalized treatment strategies.
- Improved Diagnostic Techniques: Ongoing efforts to refine imaging modalities and develop novel biomarkers could enhance the accuracy and timeliness of scar endometriosis diagnosis.
As research continues to advance, the future holds promise for more effective, personalized, and minimally invasive approaches to managing scar endometriosis.
Multidisciplinary Care: A Collaborative Approach
Scar endometriosis often requires a multidisciplinary approach involving various healthcare professionals, each contributing their expertise to ensure comprehensive care. This collaborative team may include:
- Gynecologists: Gynecologists play a pivotal role in diagnosing, treating, and managing scar endometriosis, as well as addressing any associated pelvic endometriosis or fertility concerns.
- Radiologists: Radiologists are essential in interpreting imaging studies and guiding the diagnostic process, particularly in cases where surgical intervention is being considered.
- Pathologists: Pathologists provide crucial insights by examining tissue samples and confirming the diagnosis of scar endometriosis through histopathological analysis.
- Surgeons: Surgical specialists, such as general surgeons or plastic surgeons, may be involved in the surgical management of scar endometriosis, particularly in cases requiring complex reconstructive procedures or mesh reinforcement.
- Pain Management Specialists: Chronic pain associated with scar endometriosis may necessitate the involvement of pain management specialists to develop effective pain control strategies.
- Mental Health Professionals: Psychologists, counselors, or therapists can provide invaluable support in addressing the psychological impact of scar endometriosis and promoting overall well-being.
Effective communication and collaboration among this multidisciplinary team are essential to ensure comprehensive, coordinated care tailored to each patient’s unique needs.
Patient Education and Advocacy
Empowering patients through education and advocacy is crucial in addressing the challenges posed by scar endometriosis. Healthcare professionals should prioritize providing accurate and up-to-date information to patients, fostering a better understanding of the condition, its implications, and available treatment options.
Patient support groups and advocacy organizations play a vital role in raising awareness, promoting research, and advocating for improved access to care and resources. These platforms can also serve as a valuable source of support, allowing individuals with scar endometriosis to connect, share experiences, and gain strength from one another. By fostering a collaborative approach between healthcare professionals, patients, and advocacy groups, we can collectively work towards improving the quality of life for those affected by scar endometriosis and advancing our understanding of this complex condition.
Conclusion
Scar endometriosis, a rare and often overlooked manifestation of endometriosis, presents unique challenges in diagnosis and management. However, by raising awareness, promoting early recognition, and embracing a multidisciplinary approach, we can better support everyone affected by this condition.
Through meticulous surgical techniques, targeted therapies, and ongoing research, we can strive to alleviate the physical and emotional burdens associated with scar endometriosis. Additionally, fostering open dialogue, patient education, and advocacy efforts can empower an individual to navigate this journey with knowledge, support, and resilience. By unraveling the enigma of scar endometriosis, we can pave the way for more effective treatments, improved quality of life, and a deeper understanding of this intricate condition, ultimately providing hope and solace to those affected.
REFERENCES:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2851454
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10024799
https://www.shreeivfclinic.com/endometriosis/scar-endometriosis
https://casereports.bmj.com/content/2014/bcr-2014-206693
https://www.mdpi.com/2296-3529/9/2/20

Does Removing Endometriosis and Fibroid Tumor Increase the Chances of Pregnancy?
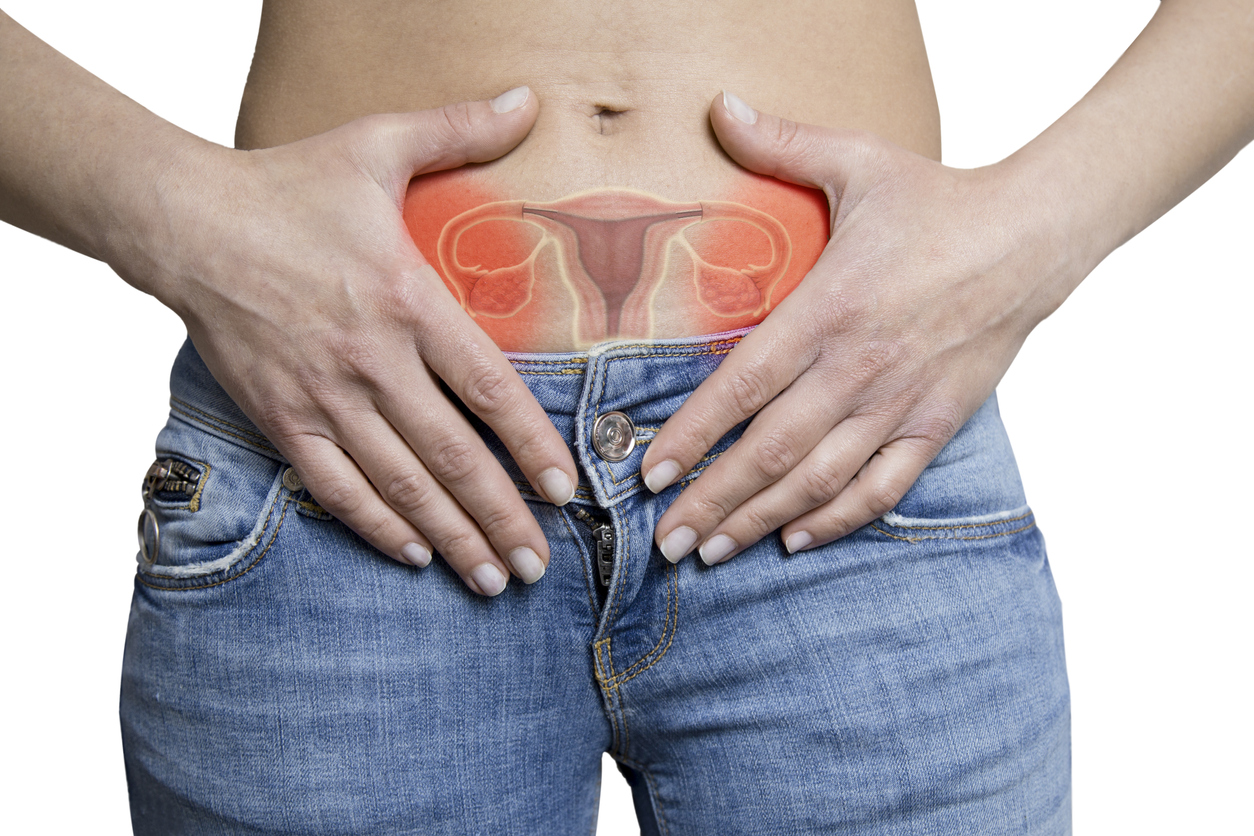
Overview of Endometriosis and Fibroids
Endometriosis and uterine fibroids are prevalent gynecological conditions that can profoundly impact a woman’s reproductive health and fertility. Endometriosis, affecting approximately 10% of individuals assigned female at birth (AFAB), occurs when endometrial-like tissue is found outside of the uterus, primarily in the abdominopelvic cavity. Fibroids, on the other hand, are non-cancerous growths made up of fibrous tissue and smooth muscle cells that develop in or around the uterus. They may also be called uterine myomas or leiomyomas and affect an estimated 20–40% of AFABs, often during their childbearing years.
While these conditions are distinct, they share some common characteristics, including the potential to cause infertility and pregnancy complications. This article aims to provide a comprehensive understanding of the effects of endometriosis and fibroids on pregnancy, as well as the various treatment options available to maintain fertility.
Endometriosis and Infertility
Endometriosis is a leading cause of infertility, responsible for approximately 50% of infertility cases. The condition can impair fertility by obstructing the fallopian tubes, disrupting the hormonal milieu, causing inflammation, and altering endometrial development, thereby reducing the chances of successful embryo implantation.
However, it’s important to note that many individuals with endometriosis can still conceive naturally or with the assistance of fertility treatments. The impact of endometriosis on fertility may depend on the severity and location of the endometrial lesions.
Fibroids and Fertility
While fibroids are generally non-cancerous, their presence can affect fertility in several ways. Submucosal fibroids, which protrude into the uterine cavity, can significantly reduce the chances of successful embryo implantation and pregnancy rates during assisted reproductive technologies (ART) such as in vitro fertilization (IVF).
Intramural fibroids, which grow within the uterine muscle wall, can also impair fertility by distorting the uterine cavity and disrupting the hormonal environment necessary for successful implantation and placentation.
Endometriosis and Pregnancy Outcomes
People with endometriosis may face an increased risk of certain adverse pregnancy outcomes, including:
- Placental abnormalities (placenta previa, placental abruption)
- Preterm birth
- Pregnancy-induced hypertension/preeclampsia
- Cesarean delivery
The risk of these complications may be influenced by factors such as the severity of endometriosis, the presence of infertility, and the use of fertility treatments. However, many individuals with endometriosis can have successful, uncomplicated pregnancies.
Fibroids and Pregnancy Outcomes
Fibroids can also impact pregnancy outcomes in various ways. Individuals with fibroids may be at an increased risk of:
- Placental abnormalities (placental abruption, placenta previa)
- Preterm labor and delivery
- Fetal malpresentation (breech presentation)
- Cesarean delivery
- Postpartum hemorrhage
The risk of these complications may be influenced by factors such as the size, number, and location of the fibroids. Large fibroids, or those located in the uterine cavity, may pose a greater risk to the pregnancy.
Treatment Options for Fertility Preservation
For individuals with endometriosis or fibroids who desire future fertility, surgery or removal of the endometriosis lesions and/or fibroid(s) may be recommended to improve their chances of conception and reduce the risk of pregnancy complications.
Endometriosis Surgery
While there is no one-size-fits all approach to addressing endometriosis, surgical excision or removal of the lesions is thought to be the ideal approach to addressing the lesions directly. This minimally invasive surgery aims to remove the lesions while preserving the uterus and ovaries, allowing for future fertility.
Fibroid Removal
For individuals with fibroids who wish to maintain their fertility, a myomectomy may be recommended. This surgical procedure involves the removal of fibroids while preserving the uterus. Depending on the size, number, and location of the fibroids, myomectomies can be performed through various approaches, including:
- Hysteroscopic myomectomy (for submucosal fibroids)
- Laparoscopic myomectomy (for intramural or subserosal fibroids)
- Abdominal myomectomy (for larger or multiple fibroids)
The choice of approach depends on factors such as the size and location of the fibroids, as well as the surgeon’s expertise and the patient’s preferences.
Fertility Outcomes After Surgery
Studies have shown that those who undergo endometriosis excision or myomectomy for fibroid removal can achieve pregnancy rates ranging from 50-60%. However, it’s important to note that these procedures do not guarantee fertility, and the success rates may vary depending on factors such as age, severity of the condition, and the presence of other infertility factors.
Pregnancy Monitoring and Management
For those with endometriosis or fibroids who become pregnant, close monitoring and specialized care may be recommended to mitigate potential risks and ensure the best possible outcomes for both the mother and the baby.
This may involve regular ultrasound examinations to monitor fetal growth and placental function, as well as close monitoring for signs of preterm labor or other complications. In some cases, additional interventions or precautions may be necessary, such as bed rest, medication, or early delivery.
Non-Surgical Treatment Options
While surgical tumor removal is often the preferred option for those seeking to preserve fertility, there are also non-surgical treatment options available for managing endometriosis and fibroids. These include:
Endometriosis:
- Hormonal therapies (e.g., birth control pills, GnRH agonists)
- Anti-inflammatory medications
- Complementary therapies (e.g., dietary modifications, exercise)
Fibroids:
- Gonadotropin-releasing hormone (GnRH) agonists
- Selective progesterone receptor modulators (SPRMs)
- Uterine artery embolization (UAE)
- Magnetic resonance-guided focused ultrasound (MRgFUS)
These non-surgical options may be used to manage symptoms, reduce tumor size, or provide temporary relief before pursuing fertility treatments or tumor removal surgery.
Emerging Treatments and Future Directions
Research is ongoing to develop new and improved treatment options for endometriosis and fibroids, with a particular focus on preserving fertility and minimizing the risk of adverse pregnancy outcomes.
Some areas of active research include:
- Novel hormonal therapies and targeted therapies for endometriosis
- Improved surgical techniques for myomectomy and endometriosis excision
- Non-invasive tumor removal methods (e.g., MRgFUS, UAE)
- Preventative strategies to reduce the risk of endometriosis and fibroid development
As our understanding of these conditions continues to evolve, it is hoped that more effective and less invasive treatment options will become available, improving the quality of life and reproductive outcomes for individuals affected by endometriosis and fibroids.
Emotional and Psychological Support
The journey through endometriosis, fibroids, and infertility can be emotionally and psychologically challenging for many. It’s essential to recognize and address the emotional impact of these conditions, as well as the stress and anxiety that can accompany fertility treatments and pregnancy complications.
Support groups, counseling, and mental health resources can be invaluable in helping individuals cope with the emotional and psychological aspects of their condition and treatment. Healthcare providers should be mindful of these needs and provide appropriate referrals and support services as needed.
Conclusion
Endometriosis and fibroids are common gynecological conditions that can have a significant impact on fertility and pregnancy outcomes. While these conditions can pose challenges, there are various surgical and non-surgical options and treatment strategies available to help individuals achieve their desired family size while mitigating potential risks.
By working closely with their healthcare providers, people with endometriosis or fibroids can develop personalized treatment plans that address their individual needs and preferences. With proper management and care, those suffering from these conditions can successfully navigate pregnancy and achieve their dreams of parenthood.
REFERENCES:
https://www.webmd.com/women/uterine-fibroids/what-if-i-have-uterine-fibroids-while-pregnant
https://www.acfs2000.com/fibroids-and-endometriosis.html
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3608270
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9187594

Navigating the Road to Recovery: A Comprehensive Guide to Endometriosis Surgery Aftercare
The journey towards relief from endometriosis often involves surgical intervention, but the road to recovery can be a winding one. While endometriosis surgery offers hope for alleviating debilitating symptoms, the post-operative phase demands patience, diligence, and a steadfast commitment to self-care. This comprehensive guide aims to equip you with the knowledge and strategies necessary to navigate the recovery process with confidence and ease.
Understanding the Endometriosis Surgery Landscape
Endometriosis, a chronic condition characterized by the growth of endometrial-like tissue outside the uterus, can wreak havoc on an individual’s quality of life. When medications and lifestyle modifications fail to provide adequate relief, surgical intervention may become a viable option. Minimally invasive approaches are now the go-to approaches for endometriosis surgery.
Laparoscopy: A Minimally Invasive Marvel
Laparoscopy, a minimally invasive procedure, is the preferred approach for endometriosis surgery. This technique involves making small incisions in the abdomen and inserting a laparoscope—a slender camera—to visualize and remove endometrial lesions or scar tissue. Laparoscopy offers numerous advantages, including reduced recovery time, minimal scarring, and a lower risk of complications.
Robotic Surgery: A More Advanced Approach
While you may hear mixed opinions on whether robotic surgery is better or worse than a laparoscopic approach, it appears that robotics are the way of the future. Providers using a robotic approach have to undergo more extensive surgical training, but the outcomes may be superior. While the operative time, or time and anesthesia, can be longer than laparoscopic surgeries, the visualization is undoubtedly better. Endometriosis can present with some hard-to-see or hard-to-recognize lesion types, and using this approach may be a better way to visualize those hard-to-see lesions to remove them.
Laparotomy: The Open Approach
This is an older approach that has been replaced with minimally invasive approaches, but you may still occasionally see someone undergo a laparotomy. In cases of extensive endometriosis or when laparoscopy is not feasible, laparotomy, an open surgical procedure, may be recommended. Laparotomy involves a larger incision in the abdomen, allowing for better visualization and access to deeply infiltrating endometriosis lesions. While more invasive, laparotomy may be necessary in certain circumstances.
Preparing for the Post-Operative Journey
Before embarking on the recovery path, it is crucial to lay the groundwork for a smooth transition. Your healthcare provider will provide specific instructions tailored to your unique situation, but here are some general guidelines:
- Arrange Transportation: Have a trusted friend or family member available to drive you home after the procedure, as you will be unable to operate a vehicle immediately following surgery.
- Stock Up on Essentials: Ensure your pantry and refrigerator are stocked with easily digestible foods, such as soups, broths, yogurt, and fruits, as well as plenty of fluids to stay hydrated.
- Prepare for Medication Management: Discuss any necessary medication adjustments with your healthcare provider, including pain relievers, antibiotics, and laxatives to aid in post-operative recovery.
- Create a Comfortable Environment: Arrange your living space to minimize unnecessary movement and exertion, ensuring easy access to essential items and a comfortable resting area.
The First Few Days: Taking It Slow
The initial days following endometriosis surgery are crucial for initiating the healing process. During this time, it is essential to prioritize rest and follow your healthcare provider’s instructions diligently:
- Manage Pain and Discomfort: Take prescribed pain medications as directed to alleviate discomfort and promote healing. Applying a heating pad or ice pack to the incision site can also provide relief.
- Stay Hydrated and Nourished: Consume plenty of fluids and easily digestible foods to support your body’s recovery efforts. Avoid heavy, greasy, or spicy meals that may cause digestive discomfort.
- Embrace Gentle Movement: While rest is essential, light movement, such as short walks around the house, can aid in circulation and prevent complications like blood clots.
- Monitor Incision Sites: Keep an eye on your incision sites for signs of infection, such as redness, swelling, or pus drainage. Follow your healthcare provider’s instructions for proper wound care.
The Weeks Ahead: Gradual Progress and Patience
As the days turn into weeks, your body will continue its healing journey. During this phase, it is important to strike a balance between rest and gentle activity, while adhering to your healthcare provider’s recommendations:
- Increase Activity Levels Gradually: After the initial recovery period, you can gradually increase your activity levels, starting with light exercises like walking or gentle stretching. Listen to your body and avoid overexertion.
- Manage Expectations: Recovery timelines can vary significantly based on the extent of the surgery, your overall health, and individual healing rates. Be patient and celebrate small victories along the way.
- Attend Follow-up Appointments: Keeping scheduled follow-up appointments with your healthcare provider is crucial for monitoring your progress and addressing any concerns or complications that may arise.
- Seek Support: The recovery process can be emotionally and physically taxing. Reach out to loved ones, support groups, or mental health professionals for encouragement and guidance during this journey.
Returning to Normal Activities: Listening to Your Body
As you continue to heal, the desire to resume your normal routine may become increasingly strong. However, it is essential to listen to your body and follow your healthcare provider’s advice regarding the appropriate timeline for returning to various activities:
- Work and School: Depending on the nature of your job or studies, you may be able to return to work or school within two weeks of the surgery. However, if your responsibilities involve physical labor or strenuous activity, a longer recovery period may be necessary.
- Exercise and Sports: Low-impact exercises like walking or light yoga can typically be resumed within a few weeks, but strenuous activities and high-impact sports should be avoided until your healthcare provider gives the green light.
- Intimate Relationships: It is generally recommended to abstain from sexual activity for at least six weeks after endometriosis surgery to allow for proper healing. Discuss any concerns with your healthcare provider.
- Travel and Vacations: While short trips may be possible within a few weeks, it is advisable to postpone extended travel or vacations until you have fully recovered, typically within 6-8 weeks after the surgery.
Embracing a Holistic Approach to Recovery
Recovery from endometriosis surgery extends beyond physical healing; it encompasses emotional and mental well-being as well. Embracing a holistic approach can enhance your overall recovery experience:
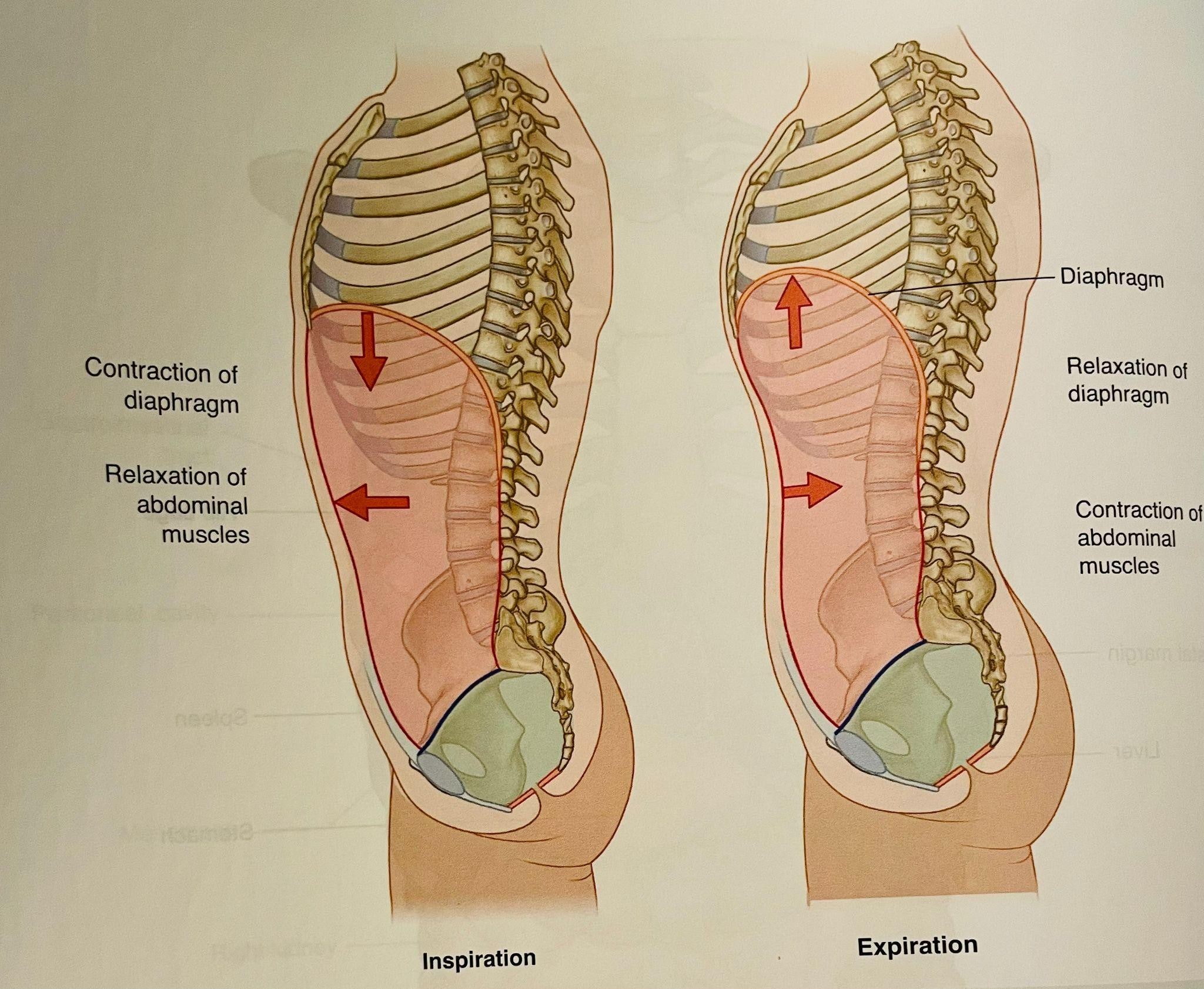
- Prioritize Stress Management: Chronic stress can hinder the healing process. Incorporate relaxation techniques like deep breathing exercises, meditation, or gentle yoga into your routine to promote a calm and peaceful mindset.
- Seek Emotional Support: Endometriosis can take a toll on mental health, and the recovery process can be emotionally taxing. Lean on your support system, join support groups, or consider seeking professional counseling to navigate the emotional challenges.
- Nourish Your Body: A balanced diet rich in whole foods, antioxidants, and anti-inflammatory nutrients can aid in the healing process and promote overall well-being. Consult with a nutritionist or dietitian for personalized dietary recommendations.
- Stay Positive and Patient: Recovery from endometriosis surgery is a journey, and setbacks or slower progress than anticipated can be disheartening. Maintain a positive mindset, celebrate small victories, and trust in the healing process.
Addressing Potential Complications and Recurrence
While endometriosis surgery aims to alleviate symptoms and improve quality of life, it is important to be aware of potential complications and the possibility of recurrence:
- Recognizing Signs of Complications: Be vigilant for signs of infection, excessive bleeding, or worsening pain, and promptly report any concerns to your healthcare provider. Especially around the incision sites, look for abnormal redness, swelling, heat, or pain.
- Managing Recurrence Risk: Endometriosis can recur after surgery, even with the best surgery. However, the persistence of endometriosis can occur when not all lesions are removed. Discuss long-term management strategies with your healthcare provider.
- Exploring Alternative Treatments: If endometriosis symptoms persist or recur despite surgery, explore alternative treatment options such as hormonal therapy, pain management techniques, or complementary therapies in consultation with your healthcare provider.
Fertility Considerations After Endometriosis Surgery
For many individuals with endometriosis, preserving fertility is a significant concern. Endometriosis surgery can potentially improve fertility outcomes, but it is crucial to have an open dialogue with your healthcare provider about your goals and options:
- Timing for Conception: Depending on the extent of the surgery and your overall health, your healthcare provider may recommend waiting a specific period before attempting conception to allow for complete healing.
- Assisted Reproductive Technologies: In cases of moderate to severe endometriosis, assisted reproductive technologies (ART), such as in vitro fertilization (IVF), may be recommended to improve pregnancy chances.
- Fertility Preservation Options: If you are considering future fertility but are not ready for conception immediately after surgery, discuss fertility preservation options like egg freezing with your healthcare provider.
Embracing a Positive Mindset and Self-Care
The recovery journey after endometriosis surgery can be physically and emotionally challenging, but embracing a positive mindset and prioritizing self-care can make a significant difference:
- Celebrate Small Victories: Recovery is a process, and every milestone, no matter how small, deserves celebration. Acknowledge and appreciate your progress, even on days when it may seem insignificant.
- Practice Self-Compassion: Be kind and patient with yourself throughout the recovery process. Healing takes time, and setbacks are a natural part of the journey. Treat yourself with the same compassion you would extend to a loved one.
- Engage in Enjoyable Activities: While rest is essential, engaging in low-impact activities that bring you joy and relaxation can boost your mood and overall well-being. Read a book, listen to music, or indulge in a favorite hobby that doesn’t strain your recovery.
- Seek Professional Support: If you find yourself struggling with anxiety, depression, or other mental health concerns during the recovery process, don’t hesitate to seek professional support from a therapist or counselor.
Endometriosis Surgery Recovery: A Transformative Journey
Recovering from endometriosis surgery is a transformative journey that requires patience, perseverance, and a commitment to self-care. While the road may be winding, embracing a positive mindset, following your healthcare provider’s guidance, and listening to your body’s needs can pave the way for a successful recovery and improved quality of life. Remember, every person’s journey is unique, and with the right support and strategies, you can navigate this path with resilience and emerge stronger on the other side.
REFERENCES:
https://my.clevelandclinic.org/health/treatments/4620-endometriosis-surgery
https://www.healthline.com/health/endotough/surgery-for-endometriosis

Can Endometriosis Cause Vomiting?
A Perplexing Condition
Endometriosis, a disorder affecting an estimated 176 million women worldwide, is characterized by the abnormal growth of endometrial-like tissue outside the uterus. While pelvic pain and infertility are well-recognized symptoms, many individuals remain unaware of the connection between endometriosis and gastrointestinal issues, including vomiting.
The Gastrointestinal Manifestations
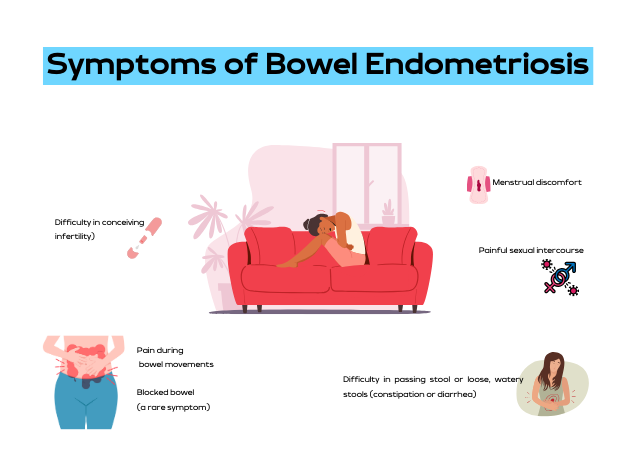
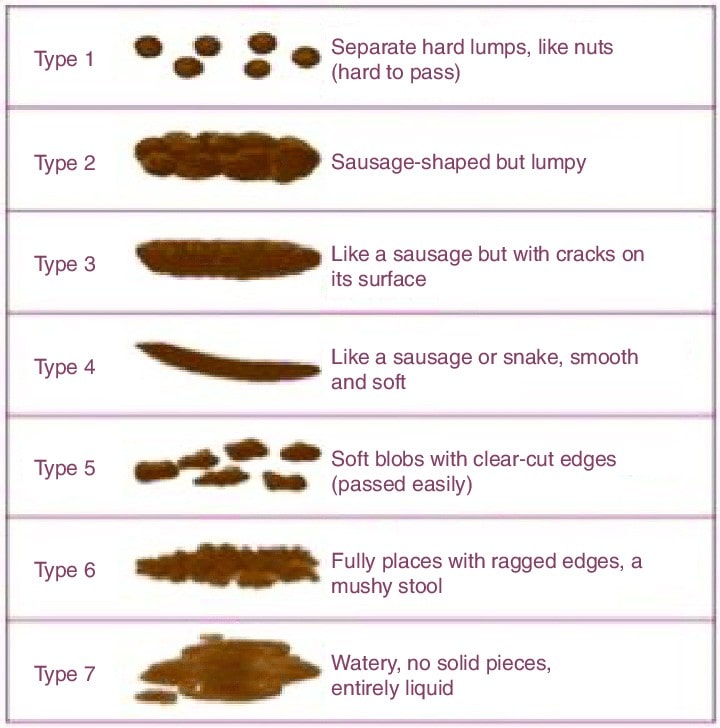
Contrary to popular belief, gastrointestinal symptoms are nearly as prevalent as gynecological symptoms in women with endometriosis. Interestingly, 90% of patients with this illness initially have gastrointestinal issues such as bloating, diarrhea, constipation, uncomfortable bowel movements, nausea, or vomiting.
Bloating: A Persistent Symptom
Bloating is the most often reported symptom, impacting an astounding 83% of endometriosis-affected women. The ongoing discomfort could significantly affect everyday activities and the general quality of life.
Vomiting and Nausea: The Often Ignored Symptoms
Despite occasionally taking center stage, nausea and vomiting are unpleasant symptoms that can significantly affect people with endometriosis. These symptoms may point to a complex interaction between the disease and gastrointestinal function, regardless of where the endometrial lesions are located in relation to the colon. Additionally, vomiting and nausea can result from severe pain and discomfort.
The Link Between Endometriosis and IBS
To make matters worse, endometriosis can mimic symptoms of Irritable Bowel Syndrome (IBS), such as frequent bloating and irregular bowel movements. When seeking assistance from a gastroenterologist, many women receive an IBS diagnosis before identifying the underlying endometriosis.
This is typical: A young woman visits a gastroenterologist due to bloating and constipation. She was diagnosed with IBS following an upper endoscopy and colonoscopy that showed no visible digestive problems. Her IBS symptoms do not go away, though, because endometriosis is the underlying cause of them.
Small Intestinal Bacterial Overgrowth (SIBO)
There is a common link between endometriosis and small intestinal bacterial overgrowth (SIBO), a disorder marked by a notable build-up of bacteria in the small intestine. As a result of this overgrowth, patients with endometriosis may have more severe digestive issues, such as bloating, gas, diarrhea, and abdominal pain.
The lactulose-hydrogen breath test measures the amounts of hydrogen and methane in the breath. It is a straightforward, noninvasive, and reasonably priced method of diagnosing SIBO.
Strategies for Treatment
Although there is currently no recognized treatment for endometriosis, there are several ways to help control symptoms, including nausea and vomiting:
- Surgical Intervention: Laparoscopic excision surgery can reduce symptoms by treating the underlying cause by removing endometriosis tissue.
- Hormonal Medications and Contraceptives: Hormonal therapy can lessen symptoms.
- Pain Management: Physicians may recommend over-the-counter pain relievers to patients to alleviate the discomfort associated with endometriosis and gastrointestinal issues.
- SIBO Treatment: Medication alone is not enough to reduce gastrointestinal issues associated with endometriosis; lifestyle modifications are also helpful.
Seeking Professional Guidance
You should consult a physician if you experience nausea, vomiting, or severe abdominal discomfort regularly. A thorough assessment that involves imaging scans, a laparoscopy, and a pelvic examination may be required to get an accurate diagnosis and develop a care plan.
The Value of Prompt Intervention
If endometriosis is not treated, it can have a major negative impact on a person’s quality of life. Recognizing and seeking care for gastrointestinal symptoms such as nausea and vomiting as soon as possible might help people’s chances of receiving treatment and managing their symptoms.
Conclusion
Beyond infertility and pelvic pain, endometriosis is a complex disease. People can increase their chances of receiving treatment and managing their symptoms by recognizing and obtaining care for gastrointestinal symptoms like nausea and vomiting as soon as possible. Women with endometriosis can improve their overall quality of life and take back control of their lives by using a multidisciplinary strategy that includes lifestyle changes, medicinal therapies, and support networks.
REFERENCES:
https://www.medicalnewstoday.com/articles/endometriosis-and-nausea
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4535676

Adenomyosis and Endometriosis, Differences and Similarities
Adenomyosis and endometriosis, two different yet similar conditions, have long challenged the medical community with their manifestations and elusive origins. While sharing some similarities, these disorders have characteristics that demand meticulous examination and unique approaches to management. This article discusses adenomyosis and endometriosis, their differences, symptoms, causes, and cutting-edge diagnostic and therapeutic avenues.
Understanding the Fundamental Differences Between Endometriosis and Adenomyosis
A crucial distinction lies at the heart of these conditions: the location of the disease growth. In adenomyosis, the endometrial cells, which typically line the uterine cavity, infiltrate and embed themselves within the muscular walls of the uterus itself. This invasion results in a thickening of the uterine walls, causing potential complications.
Conversely, endometriosis involves the abnormal proliferation of endometrial-like tissue beyond the uterus, often colonizing surrounding organs such as the ovaries, fallopian tubes, and even the bladder or intestines. This misplaced tissue behaves similarly to the endometrium, undergoing cyclic shedding and bleeding, which can lead to the formation of adhesions, cysts, and scarring within the affected areas.
The Spectrum of Symptoms
While adenomyosis and endometriosis share some common symptoms, there are distinct nuances that can help in their differentiation. Both conditions can manifest as pelvic pain, particularly during menstrual cycles, as well as heavy or irregular bleeding patterns. However, adenomyosis may present with an enlarged, tender uterus, while endometriosis can cause pain during bowel movements, urination, or sexual intercourse, depending on the location of the endometrial implants.
The Disease’s Origins and Potential Causes
Despite extensive research, the exact causes of adenomyosis and endometriosis remain unclear. However, certain risk factors have been identified that may increase an individual’s susceptibility to these conditions.
For adenomyosis, factors such as prior uterine surgeries, multiple pregnancies, and increased exposure to estrogen have been implicated as potential contributors. Endometriosis, on the other hand, has been linked to a family history of the condition, early onset of menstruation (before age 11), short menstrual cycles (less than 27 days), and heavy periods lasting more than seven days.
Two widely discussed reasons for the development of endometriosis are cell misplacement during organogenesis and retrograde menstruation. However, the exact mechanisms underlying the development of both conditions remain elusive, highlighting the need for further research.
Diagnosing Endometriosis vs. Adenomyosis
Diagnosing adenomyosis and endometriosis can be a complex and multifaceted process, often requiring a combination of various diagnostic tools and techniques.
For adenomyosis, imaging modalities such as transvaginal ultrasound and magnetic resonance imaging (MRI) can provide valuable insights into the thickness and texture of the uterine walls, potentially revealing the presence of abnormal growths or cysts. However, in some cases, a definitive diagnosis may only be possible by examining uterine tissue samples obtained during a hysterectomy or biopsy.
Endometriosis, on the other hand, frequently requires a surgical procedure known as laparoscopy. During this minimally invasive procedure, a tiny camera is inserted into the abdominal cavity, enabling the surgeon to inspect for the presence of endometriosis implants visually and, if necessary, obtain tissue samples for further analysis.
While imaging techniques like ultrasound and MRI can suggest the presence of endometriosis, they may not always detect smaller lesions or implants, making laparoscopy the gold standard for definitive diagnosis.
Treatments
The management of adenomyosis and endometriosis is a highly individualized process tailored to each patient’s unique circumstances, symptom severity, and fertility goals. For both conditions, initial treatment often involves over-the-counter pain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), to alleviate discomfort and manage heavy bleeding. Hormonal contraceptives, including birth control pills, progestin-only intrauterine devices (IUDs), and gonadotropin-releasing hormone (GnRH) agonists, can also be employed to regulate menstrual cycles and suppress the growth of endometrial tissue.
In cases where medical management proves inadequate, surgical interventions may be considered. For adenomyosis, options include robotic-assisted excision of the affected uterine tissue or, in severe cases, a hysterectomy (removal of the uterus). Endometriosis similarly requires laparoscopic surgery to remove endometriosis implants and adhesions or, in some instances, a hysterectomy with bilateral salpingo-oophorectomy (removal of the uterus, fallopian tubes, and ovaries).
It is crucial to note that while surgery can alleviate symptoms, it does not necessarily cure endometriosis, as the condition may recur. Ongoing management and close monitoring are often necessary to ensure optimal outcomes.
Fertility Implications
Both adenomyosis and endometriosis can have profound impacts on an individual’s fertility and reproductive health. Endometriosis, in particular, is a leading cause of infertility and subfertility, as the presence of endometriosis implants and adhesions can impede ovulation, disrupt the fallopian tube function, and create an inhospitable environment for embryo implantation. In cases of adenomyosis, the abnormal thickening of the uterine walls can make it challenging for embryos to implant successfully, increasing the risk of miscarriage or complications during pregnancy.
A multidisciplinary approach involving fertility specialists and gynecologists may be necessary for individuals seeking to conceive. Treatment options may include assisted reproductive technologies (ART) such as in vitro fertilization (IVF), intrauterine insemination (IUI), or the use of fertility medications to induce ovulation. In severe cases of adenomyosis or endometriosis, where fertility preservation is not a priority, a hysterectomy or other surgical interventions may be recommended to alleviate symptoms and improve overall quality of life.
Coping Mechanisms
Living with chronic conditions like adenomyosis and endometriosis can be emotionally and physically taxing, often leading to feelings of anxiety, depression, and a diminished sense of well-being. A holistic approach that addresses these conditions’ physical and psychological aspects can be instrumental in improving overall quality of life.
In addition to medical interventions, complementary therapies such as routine exercise, meditation, massage, and acupuncture can be beneficial for managing pain and reducing stress levels associated with adenomyosis and endometriosis.
Furthermore, seeking support from professional counselors, therapists, or support groups can provide a valuable outlet for individuals to share their experiences, receive emotional support, and learn coping strategies from others navigating similar journeys.
Research and Cutting-Edge Advancements
The field of gynecological research is constantly evolving, with scientists and clinicians tirelessly exploring innovative approaches to understanding, diagnosing, and treating adenomyosis and endometriosis.
One promising avenue is the development of non-invasive diagnostic techniques, such as advanced imaging modalities or biomarker analysis, which could eliminate the need for invasive procedures like laparoscopy in some cases.
Additionally, ongoing research into these conditions’ genetic and molecular underpinnings may yield insights into novel therapeutic targets and personalized treatment strategies tailored to an individual’s unique genetic profile.
Furthermore, advancements in robotic-assisted surgical techniques and minimally invasive procedures continue to enhance precision, reduce recovery times, and minimize the risk of complications associated with traditional surgical interventions.
Raising Awareness
Despite their prevalence, adenomyosis and endometriosis often remain misunderstood and overlooked, leading to delays in diagnosis and inadequate support for patients.
Raising awareness about these conditions is crucial in empowering patients to advocate for their health, seek timely medical attention, and spread understanding within their personal and professional circles.
Everyone should consider promoting open dialogue, sharing personal experiences, and collaborating with healthcare professionals, advocates, and support organizations. By doing so, we can break down barriers, challenge misconceptions, and ensure that individuals affected by adenomyosis and endometriosis receive the compassionate care and support they deserve.
A Multidisciplinary Approach: Collaborating for Comprehensive Care
Endometriosis and adenomyosis are complex. Therefore, they demand a comprehensive and multidisciplinary approach involving various specialties.
Gynecologists, physical therapists, pain management specialists, mental health professionals, and fertility experts are the pieces that can help. These experts must collaborate to develop individualized treatment plans that address each patient’s unique needs and goals.
This multidisciplinary team can provide holistic care through open communication and a collaborative mindset. Holistic care can cover medical management, psychological support, and fertility preservation strategies. The multidisciplinary team and holistic care ensure the best possible outcomes for patients.
A Journey That Needs Hope and Resilience
The challenges posed by adenomyosis and endometriosis can be daunting. Therefore, it is essential to have hope and resilience throughout the journey. These conditions, though chronic, are manageable. Individuals can reclaim control over their lives and pursue their dreams with the proper support, management strategies, and a positive mindset.
In conclusion, the complex nature of adenomyosis and endometriosis demands a multifaceted approach that combines science, compassion, and a deep understanding. By collaboration, raising awareness, and innovative solutions, we can overcome this disease now and in the future.
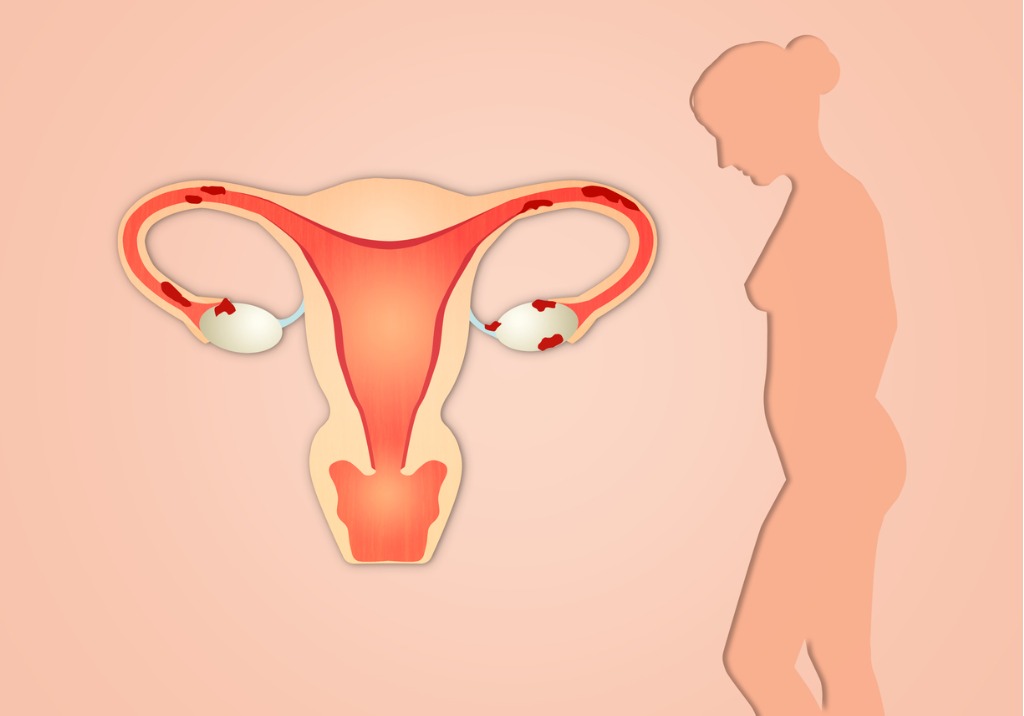
Endometriosis and Adhesions: Correlations and Treatments
What is Endometriosis?
Endometriosis is a complex disorder characterized by the growth of endometrial-like tissue (the tissue that usually lines the uterus) in locations outside the uterine cavity. This misplaced tissue behaves similarly to the endometrium, thickening, breaking down, and bleeding with each menstrual cycle. However, unlike the endometrium, which is expelled during menstruation, the displaced endometrial tissue cannot exit the body, leading to inflammation, scarring, and the formation of adhesions.
Understanding Adhesions
Adhesions are fibrous bands of scar tissue that form abnormal connections between typically separate organs or tissues. Although they can form anywhere in the body, they are most frequently found in the pelvic area when endometriosis is present, binding organs like the uterus, fallopian tubes, ovaries, and intestines.
Causes of Adhesions in Endometriosis
One major contributing factor to the formation of adhesions in the pelvic cavity is endometriosis. Adhesions may occur as a result of the inflammatory process that endometriotic lesions cause via the following mechanisms:
- Bleeding and Inflammation: Endometriotic lesions have the potential to bleed during menstruation, which can trigger an inflammatory reaction in the tissues around them. Scar tissue that forms due to this inflammation may stick to adjacent organs or tissues.
- Surgical Interventions: Endometriosis patients frequently require surgery to manage related problems or remove endometriotic lesions. Certain surgical treatments can unintentionally cause adhesions to form while the body repairs itself.
- Endometriotic Implants: There is a chance that endometriotic implants will encourage the formation of adhesions. As the implants grow and mature, they may adhere to the surrounding tissues, creating fibrous bands that keep organs together.
Differentiating Between Adhesion Pain and Endometriosis Pain
Adhesions and endometriosis are comparable conditions that frequently coexist. However, there may be some distinctions. The inflammatory process that takes place inside the endometriotic lesions itself is directly related to endometriosis discomfort. Adhesion discomfort, on the other hand, results from the binding and restricted movement of organs because of the scar tissue’s fibrous bands.
Effect on Life Quality
Endometriosis and adhesions both severely impair a woman’s quality of life and are frequently linked to infertility, chronic pelvic discomfort, and other issues. Adhesions can cause organ displacement, intestinal blockages, and disturbances to normal physiological functioning, all of which can worsen the symptoms of endometriosis. They may also make endometriosis surgeries more difficult since they may mask endometriotic lesions and complicate surgical procedures.
Diagnosis and Treatment
Diagnosing Endometriosis Adhesions
It can be difficult to diagnose adhesions linked to endometriosis. Although laparoscopic or open surgery is frequently necessary for a conclusive diagnosis, adhesions may be better understood by using imaging methods like magnetic resonance imaging (MRI) and ultrasound.
The surgeon can visually evaluate the pelvic cavity during a laparoscopic operation to check for adhesions. Adhesions can manifest as thin, filmy, transparent bands or as thick, dense, opaque structures, depending on the severity of the condition.
Treatment Approaches
Adhesions in endometriosis are usually treated with a mix of surgical and pharmaceutical procedures:
- If adhesions are severe and substantially reduce a patient’s quality of life, surgery may be necessary to remove them. This can be accomplished via laparoscopic surgery, depending on the degree and location of the adhesions. Carefully separating the adhesions from the afflicted organs during the surgical operation minimizes stress and stops new adhesion formation. Because they lower the chance of new adhesion creation than open treatments, minimally invasive techniques like laparoscopic surgery are frequently chosen.
- Treatment for Endometriosis: To stop adhesions from recurring, the underlying endometriosis must be addressed. Hormonal therapy is one option for treating endometriosis; it suppresses hormones, reduces inflammation, and treats symptoms. To eliminate the cause of inflammation and lower the chance of adhesion formation, it may occasionally be advised to remove or ablate endometriotic lesions.
It is crucial to remember that the course of therapy should be customized to the needs of each patient, taking into account the degree of adhesions, the severity of endometriosis, and any possible effects on quality of life and fertility.
Endometriosis and Adhesions: A Complex Interaction
Although endometriosis and adhesions are distinct conditions, they frequently coexist and have complex interactions. While endometriosis can result in tissue damage and inflammation that can contribute to the formation of adhesions, adhesions can exacerbate the symptoms of endometriosis and complicate surgical operations.
To manage the associated discomfort, preserve fertility, and improve overall quality of life, women with endometriosis and adhesions require a correct diagnosis and treatment plan. Medical experts can develop comprehensive therapeutic methods tailored to the patient’s needs by understanding these two conditions’ relationships.
Conclusion:
Two distinct illnesses that can have a major effect on a person’s health and quality of life are adhesion and endometriosis. In cases of endometriosis, endometrial-like tissue proliferates extraordinarily, resulting in fibrous scar tissue that may unintentionally stick to other organs. Prolonged pelvic pain; organ displacement; and surgical complications can arise from adhesion formation caused by endometriosis-induced inflammation. For many disorders, selecting the best therapy requires a precise diagnosis and an effective treatment plan that may involve medication and surgery. Knowing the connection between adhesions and endometriosis enables medical professionals to treat patients with greater specialization and comprehensive care, improving their overall health and well-being.

Unraveling the Links Between Endometriosis and Mental Health
Endometriosis is a medical condition often associated with severe pelvic pain and fertility issues. This disease might have significant psychological implications. This article reviews the relationship between endometriosis and mental health, highlighting how the physical symptoms of this disorder can translate into emotional distress.
Understanding Endometriosis
Endometriosis is a prevalent systemic and gynecological condition characterized by the abnormal growth of uterine lining cells, known as endometrium, outside the uterus. These abnormal cell growths can affect various organs, including the ovaries, fallopian tubes, and sometimes even the bladder, intestines, and rectum.
The symptoms of endometriosis include chronic pelvic pain, heavy menstrual periods, pain during sexual intercourse, and infertility. It’s estimated that about one in 10 women of reproductive age experience endometriosis, with the condition mainly impacting women in their 30s and 40s. An estimated 40% of women with infertility have endometriosis.
1- The Pain-Depression Connection in Endometriosis
The chronic pain associated with endometriosis can significantly disrupt a woman’s daily life, causing distress and leading to mental health conditions like depression and anxiety. The persistent pain can trigger feelings of hopelessness and helplessness. The debilitating effects of endometriosis pain can impact work, social interactions, and intimate relationships, contributing to feelings of isolation and lowered self-esteem.
2- Psychological Toll of Challenges of Endometriosis Diagnosis
One of the significant mental health challenges associated with endometriosis comes from the often lengthy and distressing diagnostic process. It’s not uncommon for women to experience symptoms for several years before receiving a diagnosis. Such delays in diagnosis, often due to the normalization of symptoms by healthcare professionals, can exacerbate the psychological distress associated with the condition.
Moreover, women with endometriosis often report feeling dismissed or misunderstood by healthcare professionals, which can further impact their mental health. A lack of understanding and acknowledgment of the chronic pain experienced by these women can lead to feelings of invalidation and frustration.
3- The Impact of Endometriosis on Relationships
The physical symptoms of endometriosis can significantly influence a woman’s relationships. Painful intercourse, one of the common symptoms of the condition, can cause strain in intimate relationships, leading to feelings of guilt, resentment, and anxiety. On top of that, infertility challenges can also be a complex issue in relationships. Furthermore, individuals with endometriosis might have constant chronic pain and reduced energy for participation in events. This lack of energy and presence can majorly impact a person’s relationships. These factors’s deteriorating effects on relationships can further exacerbate mental health conditions like depression and anxiety.
4- Endometriosis and Work-Life
The impact of endometriosis extends to a woman’s professional life. The heavy menstrual bleeding and severe pain associated with the condition can make maintaining a regular work schedule challenging. This work-life issue can lead to feelings of guilt and stress, further contributing to the development of mental health conditions.
5- Racial and Ethnic Differences in Endometriosis and Mental Health Impact
There’s limited research on racial and ethnic differences in endometriosis and its mental health impacts. However, a review study found that compared with white women, black and Hispanic women were less likely to be diagnosed with endometriosis. This lack of diagnosis will make the whole treatment and diagnosis process longer, which will result in more adverse mental health impacts.
6- Treatment Options and Their Psychological Implications
While there’s no definitive cure for endometriosis, various treatment options can help manage the symptoms. These include over-the-counter pain medications, hormone therapies, and, in severe cases, surgical treatments. However, the effectiveness of these treatments can vary, and the prospect of long-term management can lead to feelings of anxiety and depression.
Furthermore, some treatments, particularly surgical ones, can have physical side effects that can impact a woman’s body image, leading to further psychological distress.
7- The Role of Support and Therapy
Support groups, counseling, and cognitive-behavioral therapies can play a significant role in managing the emotional distress associated with endometriosis. These strategies can provide patients with some help tools to cope with their physical symptoms, as well as the emotional toll of living with endometriosis.
Concluding Remarks
The links between endometriosis and mental health are complex and deeply personal. Recognizing the psychological implications of endometriosis is a critical step in providing comprehensive care to individuals affected by this condition. By acknowledging the psychological stress associated with this condition, healthcare providers can positively impact the mental health outcomes of women living with endometriosis. Patients with endometriosis should seek help not only for their physical symptoms but also for any emotional distress they may be experiencing. Doing so might improve their quality of life and overall well-being.
References:
https://www.psychiatry.org/news-room/apa-blogs/how-endometriosis-can-impact-mental-health
https://www.drdanielkushner.com/blog/how-does-endometriosis-impact-mental-health
https://www.medicalnewstoday.com/articles/endometriosis-and-depression
https://www.womenspelvicsurgery.com/blog/how-endometriosis-affects-emotional-wellbeing
https://share.upmc.com/2023/07/endometriosis-and-depression

Is Endometriosis an Autoimmune Disease? An In-depth Analysis
Introduction
Endometriosis is a chronic and often debilitating condition that affects around 1 in 10 women in the US. It is characterized by the growth of endometrium-like tissue outside the uterus, often resulting in severe pain and fertility issues. Despite extensive research, the root cause of endometriosis remains unclear. Recent studies, however, have pointed to a potential interplay between endometriosis and autoimmunity, prompting questions about whether endometriosis could be an autoimmune disease.
Understanding Endometriosis
Endometriosis is a complex condition with a wide range of symptoms, varying from person to person. The endometriosis tissue, which is similar to the tissue that lines the uterus, can grow in several places outside the uterus, such as the ovaries, abdomen, and bowel. This misplaced tissue can bleed and become inflamed, leading to symptoms such as:
- Severe cramps
- Chronic pelvic pain
- Nausea or vomiting
- Heavy menstrual flow
- Pain during sexual intercourse
- Bowel or urinary problems
- Infertility
The Immune System and Autoimmunity
To understand the potential link between endometriosis and autoimmunity, it’s crucial to first understand what autoimmunity means. The immune system, which is designed to protect the body against harmful pathogens, can sometimes mistakenly attack its own cells, tissues, or organs. This misguided immune response leads to autoimmune diseases, which can cause a wide array of symptoms depending on the part of the body affected. Examples of autoimmune diseases include Celiac disease, Rheumatoid Arthritis, and Multiple Sclerosis.
Endometriosis and Autoimmunity: The Connection
Although endometriosis is not officially classified as an autoimmune disease, research has suggested a possible link between the condition and problems with the immune system. Endometriosis may cause inflammation and an imbalanced immune response, which could potentially trigger the onset of an autoimmune disease. Alternatively, an existing autoimmune disease could exacerbate the symptoms of endometriosis.
Autoimmune Disorders Linked to Endometriosis
Several autoimmune disorders have been partially linked to endometriosis, including:
- Multiple Sclerosis (MS)
- Sjögren’s Syndrome
- Lupus
- Inflammatory Bowel Disease (IBD)
- Celiac Disease
- Rheumatoid Arthritis
- Hypothyroidism
- Addison’s Disease
Endometriosis: Not Officially an Autoimmune Disease
While there are clear links between endometriosis and certain autoimmune diseases, it’s important to note that endometriosis is not officially classified as an autoimmune disease. The exact cause of endometriosis remains unknown, and more research is needed to fully understand the complex interplay between endometriosis and the immune system.
Endometriosis: Immune System Dysfunction and Inflammation
Research has found evidence of immune system dysfunction in individuals with endometriosis. This includes elevated levels of inflammation and disturbances in the function of certain immune cells. This immune dysfunction could potentially contribute to the development and progression of endometriosis.
The Impact of Autoimmunity on Endometriosis Severity
Recent studies suggest that the presence of a co-existing autoimmune disease may be an indicator of more severe stages of endometriosis. This may be due to the additional inflammation and immune system dysfunction caused by the autoimmune disease, which could exacerbate the symptoms and progression of endometriosis.
Autoimmune Treatments for Endometriosis
Current treatments for endometriosis primarily focus on managing symptoms and preventing disease progression, as there is currently no cure. These treatments include hormonal medications, pain relievers, and surgery. While treatments for autoimmune diseases typically involve suppressing the immune system, these treatments have not been found to be effective for endometriosis. However, research is underway to explore potential immunotherapy treatments for the condition.
Endometriosis and Other Health Risks
Endometriosis is associated with several other health risks beyond autoimmune diseases. For instance, endometriosis may also be linked to asthma, allergies, and some cardiovascular diseases.
Endometriosis and Cancer
There is some evidence to suggest that endometriosis may be linked to certain types of cancer. Specifically, endometriosis may increase the risk of developing ovarian cancer and a specific type of breast cancer.
Conclusions and Future Directions
The potential link between endometriosis and autoimmunity presents a complex avenue for future research. While more studies are needed to fully understand this connection, the current findings could have significant implications for the diagnosis and treatment of endometriosis. By better understanding the role of the immune system in endometriosis, researchers may be able to develop more effective treatments and potentially even discover a cure for this debilitating condition.
References
https://www.medicalnewstoday.com/articles/326108
https://pelvicrehabilitation.com/is-endometriosis-an-autoimmune-disease/
https://autoimmune.org/disease-information/endometriosis/
https://www.nature.com/articles/s41598-021-94877-z

Understanding Endometriosis and Stomach Cramps
Endometriosis is a medical condition that affects approximately 10% of women globally. Its symptoms can be debilitating and significantly impact the quality of life of those affected. One of the most commonly reported symptoms of endometriosis is stomach cramps. This article delves into the relationship between endometriosis and stomach cramps, unraveling the causes, symptoms, and available treatment options.
What is Endometriosis?
Endometriosis is a health disorder that occurs when tissue similar to the uterus’s endometrium begins to grow in areas outside the uterus. These areas may include the ovaries, fallopian tubes, the lining of the pelvic cavity, and, in some cases, the bowels and bladder.
What is Endo Belly?
One term that has gained popularity in endometriosis discussions is “endo belly.” This term refers to the painful abdominal bloating often associated with endometriosis. The bloating, which can be severe, results from inflammation, growths, gas, or other digestive issues related to endometriosis.
Causes of Endo Belly
The exact cause of endo belly still needs to be fully understood. However, several factors have impacted this symptom. The endometrial-like tissue behaves similarly to the endometrium: it thickens, breaks down, and bleeds with each menstrual cycle. However, since this tissue cannot exit the body, it becomes trapped, leading to inflammation and irritation. Over time, this can cause scar tissue to form, leading to various symptoms, including bloating and fluid retention.
Symptoms of Endo Belly
The primary symptom of endo belly is severe bloating, particularly during or just before the menstrual period. The abdomen may fill with air or gas, causing it to appear larger and feel stiff or tight to the touch. This bloating may last for a few hours to a few weeks. Other symptoms that may accompany endo belly include:
- Nausea and vomiting
- Gas pain
- Constipation or diarrhea
- Abdominal discomfort, pain, and pressure
How Endometriosis Causes Stomach Cramps
The stomach cramps associated with endometriosis are often severe and debilitating. These cramps are not merely due to the menstrual cycle but are a direct result of the endometrial-like tissue growing outside the uterus. This tissue resembles the endometrium, building up and breaking down each menstrual cycle. But because this tissue is outside the uterus and cannot exit the body, it gets trapped. This trapped tissue leads to inflammation and irritation, which can cause severe stomach cramps.
Symptoms of Stomach Cramps Due to Endometriosis
The main symptom associated with endometriosis-induced stomach cramps is severe pain, particularly during the menstrual period. This pain can be so intense that it disrupts daily activities and significantly impairs the individual’s quality of life. The pain often worsens throughout the day and can be so severe that the person may not be able to button their pants or may even appear as though they are pregnant.
Treatment for Endometriosis and Stomach Cramps
There are several treatment options available for managing endometriosis and its associated stomach cramps. Treatment choice often depends on the severity of the symptoms, the person’s age, and their future pregnancy plans. The treatment options include:
- Over-the-counter Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or aspirin, may be recommended to manage inflammation and reduce pain.
- Prescription Hormonal Medications: Hormonal pills or devices may help to regulate symptoms.
- Endometriosis Surgery: In severe cases, surgery may be the best option for long-term pain relief. This surgery involves removing the endometriosis and scar tissue from the pelvic and abdominal organs.
When to Consult a Doctor
It’s essential to consult an endo specialist if you’re experiencing severe stomach cramps, mainly if they’re associated with your menstrual cycle. Early diagnosis and treatment can significantly improve your quality of life and prevent potential complications, such as infertility.
Conclusion
Endometriosis and stomach cramps are closely linked. The condition can lead to severe stomach cramps that can significantly impair the quality of life of those affected. However, you can manage the symptoms effectively with proper diagnosis and treatment. Suppose you’re experiencing severe stomach cramps, especially if they’re associated with your menstrual cycle. In that case, it’s essential to consult a healthcare provider for a proper diagnosis and treatment plan.
References:
https://maidenmedical.com/endometriosis-belly
https://www.healthline.com/health/endo-belly
https://www.endofound.org/gastrointestinal-distress
https://www.utphysicians.com/the-pain-of-endometriosis/
https://www.medicalnewstoday.com/articles/endo-belly

Understanding Bladder Endometriosis and Its Treatment
Bladder endometriosis is a medical condition that affects a significant number of women worldwide. It involves the growth of endometrial-like tissue on or in the bladder. This article aims to provide an understanding of bladder endometriosis, how it is diagnosed, and the surgical procedures involved in its treatment.
What is Bladder Endometriosis?
Bladder endometriosis is a subtype of endometriosis, a condition in which cells similar to those that make up the lining of the uterus (endometrium) grow outside of it. In bladder endometriosis, these cells grow in or on the bladder. This can lead to various symptoms, including urinary frequency, pain during urination, and even blood in the urine.
Read More: https://icarebetter.com/can-endometriosis-be-treated-without-surgery/
Epidemiology and Etiology
Bladder endometriosis is relatively uncommon, occurring in approximately 1-2% of all women with endometriosis. It is most frequently diagnosed in women of reproductive age, with an average age of diagnosis around 35 years. Studies have suggested that heritability may play a role in the development of bladder endometriosis, with some women having a family history of the condition.
The exact cause of bladder endometriosis is still being researched. However, four main theories have been proposed:
- The embryonal theory suggests that bladder endometriosis originates from Müllerian remnants in the vesicouterine/vesicovaginal septum.
- The migratory or metastatic theory suggests it is an extension of an adenomyotic nodule of the anterior uterine wall.
- The transplantation theory posits that it results from the implantation of regurgitated endometrium.
- The iatrogenic theory suggests it occurs after pelvic surgery, such as cesarean delivery or hysterectomy.
Symptoms of Bladder Endometriosis
The symptoms of bladder endometriosis can vary from person to person, but often include one or more of the following:
- Frequent urination: The need to urinate often is a common symptom.
- Dysuria: This is a term for pain or discomfort during urination.
- Hematuria: This refers to blood in the urine, which may be visible or detected on a urine test.
- Lower abdominal pain: Some patients may experience pain in the lower abdomen, often worsening during menstruation.
- Recurrent urinary tract infections: Some women may have frequent UTIs.
Read More: https://icarebetter.com/can-endometriosis-grow-inside-the-bladder/
Diagnosis of Bladder Endometriosis
Diagnosing bladder endometriosis can be a complex process, as the symptoms can mimic other conditions such as recurrent cystitis or bladder infections. Various diagnostic modalities are used in the preoperative assessment of bladder endometriosis. These include:
- Transabdominal and transvaginal ultrasound: These are the initial investigations of choice for suspected bladder endometriosis due to their immediate availability and easy access.
- Magnetic resonance imaging (MRI): This imaging technique can not only delineate the morphologic abnormalities of bladder endometriosis but can also potentially identify other common sites.
- Cystoscopy: This procedure allows doctors to view the inside of the bladder and urethra using a thin, lighted instrument.
- CT urogram or MRI urogram: These tests involve injecting intravenous contrast material (a type of dye) into the urinary bladder to obtain images of the urinary tract.
Treatment of Bladder Endometriosis
The treatment of bladder endometriosis typically involves surgery, as medical management is often not effective for this condition. There are several surgical options, including:
- Transurethral resection: This procedure involves the removal of the endometriotic tissue through the urethra using a special instrument.
- Partial cystectomy: This procedure involves the removal of a part of the bladder that is affected by endometriosis.
- Laparoscopic surgery: This is a minimally invasive procedure where small incisions are made in the abdomen to remove the endometriotic tissue.
It’s important to note that the choice of treatment depends on various factors, including the size and location of the endometriotic lesions, the woman’s age, and the presence of other associated conditions.
Long-term Outcomes and Recurrence
Studies have shown that surgical treatment of bladder endometriosis can lead to good results in terms of pain relief and improvement in urinary symptoms. However, endometriosis is a chronic condition, and there is a risk of recurrence. The overall recurrence rate of symptoms is about 30% for combined therapies and about 35% for hormonal treatment alone. Regular follow-up visits are essential to monitor for any signs of recurrence and to manage any ongoing symptoms.
Read More: https://icarebetter.com/can-endometriosis-on-ureter-cause-kidney-shooting-back-pain/
Conclusion
Bladder endometriosis is a challenging condition that requires a comprehensive approach to diagnosis and treatment. It is crucial for women to be aware of the symptoms and to seek medical advice if they are experiencing any urinary problems or pelvic pain. With appropriate treatment, most women with bladder endometriosis can achieve significant relief from their symptoms and improve their quality of life.
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3016174/
https://karger.com/uin/article/89/3/249/322520/Diagnosis-and-Treatment-of-Bladder-Endometriosis
https://academic.oup.com/humrep/article/25/4/884/701431
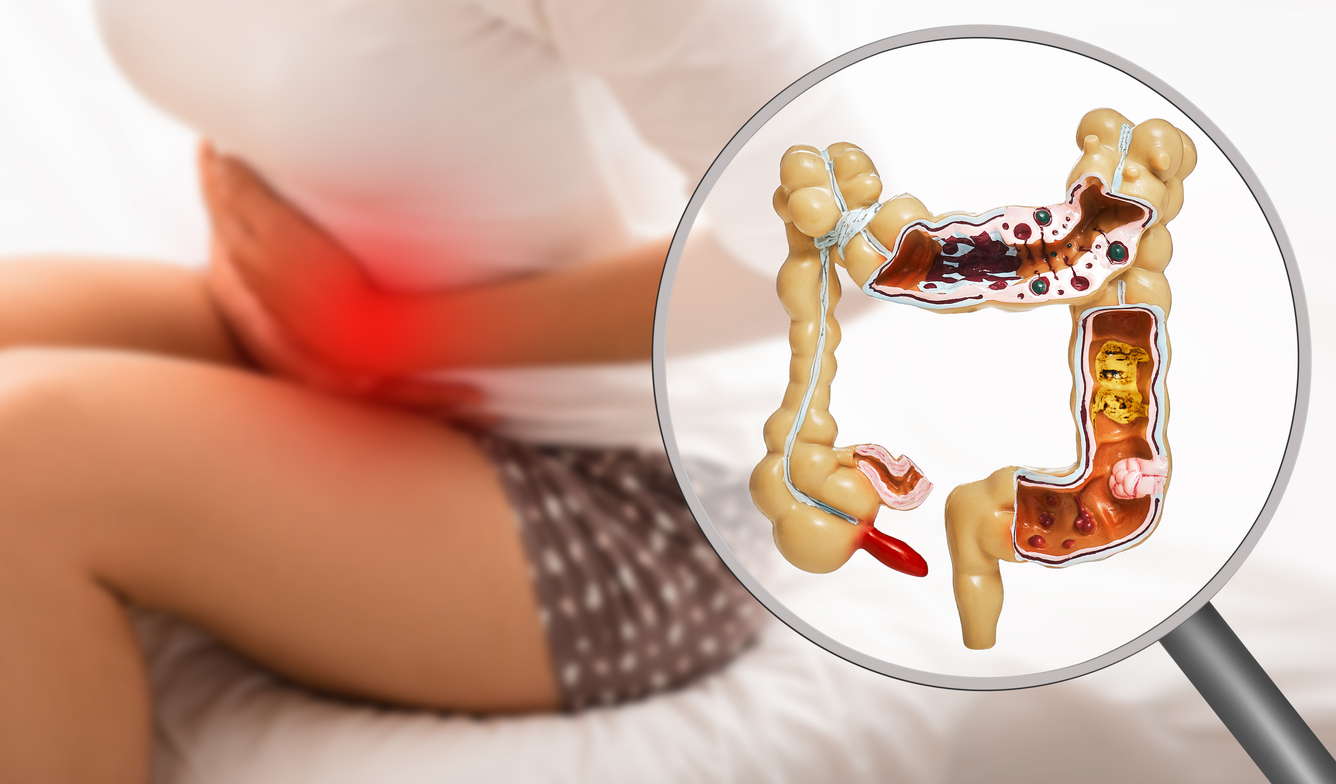
Does Gastrointestinal Endometriosis Cause Infertility
Gastrointestinal endometriosis is a condition that poses numerous health challenges to women, and one of the most concerning questions revolves around its potential impact on fertility. The primary focus of this article is to address the question:
Does gastrointestinal endometriosis cause infertility?
We will dissect this issue by exploring the available medical and scientific evidence.
Understanding Endometriosis and its Symptoms
Endometriosis can manifest with various symptoms, although not all women may experience them. Some common symptoms include:
- Painful periods: Women with endometriosis often experience more intense pelvic pain and cramping before and during their menstrual cycle.
- Chronic lower back/abdominal pain: Another hallmark of endometriosis is persistent pain in the lower back or abdomen.
- Infertility: Endometriosis has been associated with fertility problems, making it more challenging for some women to conceive.
- Excessive bleeding and spotting: Women with endometriosis may experience heavy bleeding during their periods or irregular bleeding between periods due to the presence of adenomyosis.
- Pain during or after intercourse: Endometrial tissue growths can cause pain during sexual intercourse, which can have a significant impact on a woman’s quality of life.
- Gastrointestinal issues: Endometriosis affecting the intestines can lead to symptoms such as painful bowel movements, diarrhea, constipation, and stomach issues like nausea.
- Fatigue: Chronic fatigue is a common complaint among women with endometriosis, which can be attributed to the physical and emotional toll of dealing with the condition.
Endometriosis and Fertility
The relationship between endometriosis and fertility has been a subject of continuous research. Women with endometriosis, particularly moderate to severe forms, often face fertility challenges. However, it’s important to note that endometriosis does not automatically lead to infertility. Many women with endometriosis can and do conceive naturally or with the help of fertility treatments.
How Endometriosis Impacts Fertility
The mechanism through which endometriosis affects fertility is complex and multifaceted. Here are some ways it can potentially interfere with conception:
- Anatomical Distortions: Endometriosis can cause adhesions or scar tissue formation, leading to a distortion of pelvic anatomy. This can block the fallopian tubes or alter the position of the ovaries, hindering the meeting of sperm and egg.
- Inflammatory Environment: Endometriosis creates an inflammatory environment in the pelvic region, which might harm the quality of eggs or sperm and hinder their movement.
- Impact on the Endometrium: Some studies suggest that endometriosis may affect the lining of the uterus (the endometrium), making it less receptive to an implanting embryo.
Gastrointestinal Endometriosis and Infertility: Is there a Connection?
When it comes to the specific question – does gastrointestinal endometriosis cause infertility – the answer is not as straightforward as one might hope. While endometriosis is known to affect fertility in general, the impact of gastrointestinal endometriosis on fertility is less clear.
Evidence suggests that endometriosis involving the bowel or bladder can be more challenging to treat and may require more complex surgical procedures, which could potentially affect reproductive function. However, it’s also important to remember that the presence of gastrointestinal endometriosis does not necessarily mean that a woman will experience fertility problems. However, the inflammation and molecular impacts of endometriosis might still increase the risk of fertility problems.
Treating Gastrointestinal Endometriosis
Medical Treatment
The first line of treatment for endometriosis often involves hormone therapy, such as birth control pills or progestin-based contraceptives, which work by managing symptoms and manipulating hormones. However, these medications do not improve fertility.
Surgical Treatment
Surgery to remove endometriosis patches can potentially improve fertility, especially in cases of moderate to severe endometriosis. However, surgical treatment of gastrointestinal endometriosis can be complex and may carry a higher risk of complications. Depending on the extent of the disease, it may involve resection of a portion of the bowel or bladder.
The Path to Pregnancy with Endometriosis
Surgical treatment can increase the chance of natural and assisted fertility. However, in many cases the patient still needs further support and treatment.
Fertility Treatments
For women with endometriosis who are struggling to conceive, assisted reproductive technologies (ART) such as in-vitro fertilization (IVF) may be an option. While women with severe endometriosis may have a lower success rate with IVF than other women, many are still able to achieve a successful pregnancy with this treatment.
Surrogate pregnancy
There are some options to seek help from other women’s bodies and eggs if necessary and desired.
Maintaining Hope
The journey of dealing with endometriosis and its potential impact on fertility can be emotionally challenging. However, it’s important to maintain hope. Many women with endometriosis, including gastrointestinal endometriosis, are able to conceive and have healthy pregnancies, whether naturally or with the help of fertility treatments.
Final Thoughts
In conclusion, while gastrointestinal endometriosis can pose challenges, it can impact fertility by inflammation and molecular pathways. Each case of endometriosis is unique, and the impact on fertility can vary greatly from one individual to another. If you’re dealing with endometriosis and are concerned about your fertility, it’s important to seek guidance from a healthcare provider who can provide individualized advice based on your specific situation.
Remember, understanding your condition and exploring your options can empower you to make the best decisions for your health and fertility journey. So, while gastrointestinal endometriosis can pose hurdles, they are not insurmountable. With the right treatment and support, the dream of parenthood can still be a reality for many women living with endometriosis.
References:
https://pubmed.ncbi.nlm.nih.gov/32631683/
https://www.obgyn-care.net/blog/does-endometriosis-cause-infertility
https://www.nhs.uk/conditions/endometriosis/complications/
How to Prevent Endometrioma Cysts
Endometrioma cysts, often dubbed as ‘chocolate cysts’ or “endometrioma”, pose a significant health issue for many women worldwide. Understanding how to prevent endometrioma cysts is crucial for maintaining optimal reproductive health. This comprehensive, empathetic guide will walk you through the essentials of endometrioma prevention, demystifying complex medical terms and offering practical advice.
Understanding Endometrioma
Endometrioma, a form of endometriosis, is a condition where tissue similar to the lining of the uterus grows outside the uterus, primarily on the ovaries. This growth often results in cysts filled with blood and tissue products, referred to as ‘chocolate cysts’ due to their dark, chocolate-like appearance. Understanding this condition is the first step in learning how to prevent endometrioma cysts.
Symptoms of Endometrioma
Endometrioma can manifest in a variety of symptoms, some of which are debilitating. Common symptoms include severe menstrual cramps, chronic pelvic pain, discomfort during intercourse, painful bowel movements or urination during menstruation, and fertility issues. In some cases, endometrioma may be asymptomatic, discovered only during a routine check-up or fertility assessment.
Causes of Endometrioma
The exact cause of endometrioma remains a subject of ongoing research. Some theories suggest retrograde menstruation, genetic factors, hormonal imbalances, and immune system dysfunctions. Surgical procedures in the abdominal area may also inadvertently transport endometrial tissue to other parts of the body, leading to endometrioma.
Who is at Risk?
While any woman who menstruates can develop endometrioma, certain factors increase the risk. These include a family history of endometriosis.
How is Endometrioma Diagnosed?
Doctors diagnose endometrioma through several methods, including pelvic examinations, imaging tests like ultrasounds or MRIs, and laparoscopy – a surgical procedure that allows for the visual inspection of pelvic organs. A definitive diagnosis often requires a biopsy, where a small sample of tissue is examined under a microscope.
Why Endometrioma Causes Health Problems
Endometrioma can lead to several health problems, including persistent pain, inflammation, and fertility issues. These cysts can grow, bleed, and cause scarring, leading to complications such as blocked fallopian tubes, adhesions (tissues that bind organs together), and issues with the intestines and bladder.
Preventing Endometrioma: An Overview
While endometrioma cannot be primarily prevented, certain interventions can reduce the risk of progression and recurrence after surgery. These interventions mainly focus on removing the endometriomas through surgery, lowering estrogen levels in the body, and increasing the impact of progesterone-like hormones.
Hormonal Control
Hormonal birth control methods, such as pills, patches, or rings with lower doses of estrogen, can help regulate the menstrual cycle and slow the progression of endometrioma. Intrauterine devices (IUDs) that release hormones may also be beneficial in reducing pain and bleeding.
Lifestyle Factors
Maintaining a healthy lifestyle can influence natural estrogen levels and potentially reduce the risk of endometrioma regrowth and progression. Regular exercise helps decrease body fat, which in turn lowers estrogen levels. Limiting alcohol and caffeine intake can also help, as excessive consumption of either can raise estrogen levels.
Medical Management
For those not trying to conceive, hormonal birth control is often the first line of treatment to manage symptoms.
Surgical Treatment
Excision surgery is usually considered the gold standard and the only treatment that truly removes the endometrioma lesions. The procedure involves removing the endometrioma while preserving as much healthy ovarian tissue as possible. Following surgery, hormonal treatment is typically resumed unless pregnancy is desired.
Complementary and Alternative Medicine (CAM) Therapies
In addition to conventional treatments, some individuals find relief from endometrioma symptoms through complementary and alternative medicine (CAM) therapies. These can include acupuncture, chiropractic, dietary changes, herbs, or supplements. It’s essential to discuss these approaches with your healthcare provider to ensure they’re safe and suitable for your specific needs.
In conclusion, while endometrioma cannot be prevented, understanding the condition, its risk factors, and potential treatments allows women to better manage their reproductive health. Regular check-ups, open communication with healthcare providers, and proactive lifestyle changes are all crucial in dealing with endometrioma and mitigating its effects on one’s life.
References:
https://my.clevelandclinic.org/health/diseases/22004-ovarian-endometrioma
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7754428/
Chocolate Cysts: Everything You Need To Know
Management of ovarian endometrioma
https://www.womenshealth.gov/a-z-topics/endometriosis

Ureteral Endometriosis : Can Endometriosis Spread to the Ureter
Endometriosis is a chronic condition that affects approximately 10-15% of women between 15-50 and other genders as well. This medical condition, characterized by endometrial-like tissue outside the uterus, can impact various body parts. One of the lesser-known facts about endometriosis is its potential to spread to the urinary system, specifically the ureter. This article aims to shed light on the question: “Can endometriosis spread to the ureter?” and delve into the intricacies of this complex issue.
Prevalence of Ureteral Endometriosis
Ureteral endometriosis is a form of urinary tract endometriosis (UTE), which is a rare manifestation of deep infiltrating endometriosis (DIE). Ureteral endometriosis can be either extrinsic, where endometriosis lesions occur outside the ureter causing it to compress, or intrinsic, which happens within the muscular, inner layers of the ureter.
While UTE affects between 0.3% and 12% of endometriosis cases and between 20% and 52.6% of those diagnosed with DIE, ureteral endometriosis is even rarer. Within the entire urinary system endometriosis, the prevalence of ureteral endometriosis is approximately 10%.
Causes of Ureteral Endometriosis
As the exact cause of endometriosis itself is not fully understood, pinpointing the cause of ureteral endometriosis is even more complex. Theories that attempt to explain the origin of ureteral endometriosis include stem cells, immune factors, and retrograde menstruation. In some women, UTE might also be iatrogenic, resulting from previous Caesarean sections.
Read More: Can Endometriosis on Ureter Cause Kidney Shooting Back Pain?
Symptoms Linked to Ureteral Endometriosis
Symptoms of UTE often overlap with those of peritoneal endometriosis. Women with UTE typically experience pelvic pain and dysuria (pain with urination). They may also suffer from frequent urinary tract infections, changes to urination frequency, and hematuria (blood in the urine). However, distinguishing this pain from the one that arises as a result of other forms of pelvic endometriosis is difficult.
Ureteral endometriosis is very rare, with an estimated prevalence of 0.1%. Up to 50% of women with ureteral endometriosis are asymptomatic, 25% have colicky pain, and 15% have gross hematuria. Tissue biopsy and histopathological examination are the gold standard methods for the diagnosis of ureteral endometriosis.
Read More: Can Endometriosis Cause Bowel Issues?
Diagnosing Ureteral Endometriosis
Diagnosing ureteral endometriosis can be quite challenging. It is, therefore, important to consult a specialist who can listen to and understand your symptoms. The initial stages of diagnosis of endometriosis affecting any area include taking the patient’s medical history, followed by pelvic examination and imaging techniques such as ultrasound, sonohysterography, or magnetic resonance imaging (MRI).
Intravenous pyelogram (IVP) is a good imaging technique to predict intrinsic forms of ureteral endometriosis. IVP also helps to evaluate ureter structure after treatment. MRI and Transabdominal ultrasonography can help visualize ureter structure and obstruction in the pelvic region.
Laparoscopic excision surgery followed by histological examination is the gold standard for confirming endometriosis in the urinary tract.
Read More: Can Minimal Endometriosis Cause Infertility
Treating Ureteral Endometriosis
The aim of ureteral endometriosis treatment is to remove endometriosis lesions in the urinary tract and preserve renal function. In cases of mild ureteral endometriosis, medical management, such as combined oral contraceptives, progestin, and aromatase inhibitors, may help with symptoms. However, this is not a permanent solution, and disease progression is expected, so surgical methods are the best option.
The primary treatment for ureteral endometriosis is excision surgery. Although successful medical treatment outcomes have been reported in the literature, medical treatment alone cannot revert the fibrosis resulting from ureteral endometriosis that leads to ureter obstruction.
Conclusion
Ureteral endometriosis, though rare, can cause serious complications, including the potential loss of renal function. Clinical suspicion and preoperative assessment may assist in diagnosis and allow for a multidisciplinary pre-consultation. The laparoscopic surgical approach is based on the extent of the disease and its localization and can be carried out successfully by a highly skilled surgeon.
In conclusion, if there is no other obvious etiology for the presence of unilateral hydroureteronephrosis in women in their reproductive age, the diagnosis of endometriosis should be considered. Early detection and treatment of ureteral endometriosis are essential to prevent severe complications, including the potential loss of kidney function.
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7595017/

How to Treat Deep Infiltrating Endometriosis
Endometriosis, bad enough when endometrial-like cells grow outside the uterus and on the surface of other organs, has an even more troubling variant called Deep-Infiltrating Endometriosis (DIE). This is a severe form of endometriosis defined by these abnormal cells burrowing or invading deeper into tissues and affected organs, like the bowel and bladder. Generally, the depth cutoff to fit this category is more than 5mm below the tissue surface. This guide will shed some light on how we treat and potentially cure deep infiltrating endometriosis in the future. At this time, a long-standing cure is still a stretch, even for superficial endometriosis.
Understanding Deep Infiltrating Endometriosis
The good news is that this condition is relatively rare, affecting only about 1% of women of reproductive age and only 20% of those with endometriosis. The bad news is that molecular data suggests it may be a premalignant disease, along with endometrioma type. However, this is still undergoing research, and the malignancy potential remains low. However, when genetic mutations are shared with an aggressive disease like cancer, this may help explain why endometrioma and DIE types of endo are more likely to cause more local anatomic distortion and harm with pain and subfertility impact, as well as increased metastatic potential (i.e., spread to other parts of the body even if there is no associated cancer).
Anatomic Comparison of Endometriosis Types
Based on the anatomical location of endometriosis within the pelvic and abdominal cavities, there are three major types of endo:
- Superficial endometriosis (Peritoneal endometriosis or PEM): Lesions appear on the surface of organs outside the endometrium. Generally, but not always, they cause the least amount of tissue damage and distortion.
- Ovarian endometriomas (OE): Dark cysts due to old collected blood, also called chocolate cysts, develop in or on the ovaries due to endometriosis.
- Deep infiltrating endometriosis: The most severe form, where the endometrial-like tissue invades deeper into the pelvic organs, wreaking more havoc.
Anatomic locations and clinical degree of disease form the basis for most of the staging systems that are currently used. This is extremely “old school,” and we are about to step into a new age where molecular insights will help with diagnostics and treatment options because abnormal molecular pathways can be targeted with precision therapies.
Molecular Comparison of Endometriosis Types
This is an evolving hot topic of research in endometriosis, which goes well beyond comparisons based on hormonal factors like receptor activity, up and down-regulation, and relative progesterone resistance. It is too early to classify different types of endo by this gene mutation molecular pathway metric, but what is known so far might already help with recurrence and cancer risk mitigation.
What we know is as follows:
- Endometriosis overall (PEM, OE, and DIE types) is a disease of genetic and molecular heterogeneity, meaning multiple genes are affected. Some of these are mutations exactly like those found in cancer, even if no cancer is present or even destined to develop. This means endo may not be one disease entity between different individuals but rather different ones with varying degrees of aggressiveness. On the other hand, in any given individual, there is research data to support “clonal” molecular signature similarities between all three types of endo, meaning one type (e.g., PEM) advances or progresses to the other (OE or DIE).
- Mutations of interest include ARID1A, PIK3CA, KRAS, and PPP2R1A, among others
- Endometrioma type carries the highest risk of malignant degeneration, and ARID1A is considered to be one of the most important driver mutations to clear cell cancer.
- DIE type has a wider range of mutations and is at a lower risk of malignant degeneration, but these mutations may contribute to its more aggressive behavior.
- OE-type risk for malignant degeneration may be higher than that for DIE because the molecular micro-environment differs between these two, with the ovaries possibly being more “permissive” to malignant changes. This does not negate the aggressive, invasive, and potentially metastatic nature of DIE in the absence of cancer.
- Gene mutation expression varies based on epigenetic influences, including diet, lifestyle, toxin exposure, concurrent disease states, mind-body influence, etc.
What does this all mean in summary? Multiple genes are mutated in endometriosis, some of which may or may not lead to a low risk of cancer development but can dictate how aggressive endo types, especially DIE and OE, can be in an individual. These gene mutations can be suppressed or aggravated by epigenetic influences that you have some control over. Evolving research is helping uncover diagnostic and prescription molecular treatment options based on all of this.
Identifying Symptoms of Deep Infiltrating Endometriosis
The symptoms of DIE are similar to general endometriosis but usually more severe. They may include:
- Severe pelvic pain
- Painful urination (dysuria) of bleeding in the urine (hematuria)
- Painful menstruation (dysmenorrhea)
- Genital pain before, during, or after sex (dyspareunia)
- Digestive discomfort and rectal bleeding
- Distant symptoms like pain with breathing, related to possible diaphragm involvement
Causes and Risk Factors of Deep Infiltrating Endometriosis
Notwithstanding recent research advances, the exact cause of endometriosis, including DIE, is unknown. A family history of endo and/or cancer are important to consider. It is not likely that a single cause will be uncovered because of the probable multifactorial nature of endo. However, molecular research is taking this to a different level.
Diagnosing Deep Infiltrating Endometriosis
Since deep infiltrating endometriosis is an advanced form of endometriosis, its diagnosis can be challenging. Usually, multiple diagnostics are used, including medical history, physical examination, histological examination after surgery or upon biopsy (e.g., C-section scar endo), minimally invasive surgery, ultrasound, and MRI. A 3-Tesla (“3T” for short) MRI is probably the most accurate modality, but it still has many shortcomings. In other words, it can be helpful in planning for surgery but should not be used to determine definitively if DIE is present or not. It is as good as it gets but is imperfect, missing up to 20% of DIE.
In many, if not most, cases, the diagnosis will only be apparent and confirmed at the time of surgery. Since it is impossible to accurately predict the full extent of endo before surgery, this is the main reason that it is very prudent to pick the most skilled and experienced surgeon you can find. The more symptomatic you are, the more this is critical to your success. A botched surgery does not make it easier the second time around, and it exposes you to an increased risk of major complications.
Treatment Options for Deep Infiltrating Endometriosis
Medical Treatments
Medical treatments for DIE are extremely limited and basically non-existent. This is because the deep invasive infiltration of disease leads to scarring or fibrosis as your body tries to “wall off” or isolate this disease and heal. Any known medication cannot eliminate fibrosis. What we are left with are pain relievers and hormonal options that are used in all forms of endo, for symptomatic relief and possibly some suppressive effect.
Integrative options are also an option for symptomatic relief, just as they are for any type of endo. This includes mind-body-based biofeedback, nutrition, botanicals, essential oils, acupuncture and acupressure, electrical stimulation (TENS), etc. It is best to formulate an integrative strategy with a relevant practitioner.
Pelvic floor physical therapy (PFPT) is, of course, central to a treatment plan as well. However, depending on lesion location, this should be undertaken with some caution due to possible disruption of deep lesions with internal therapies, making surgery potentially less effective. A teamwork approach should be conducted to evaluate the best strategy.
Surgical Treatments
Surgical excision of DIE lesions and associated fibrosis is by far the best path forward in most cases where DIE is anticipated and/or already diagnosed from prior surgery. The usual admonitions of excision superiority over ablation are even more critical here because ablation or fulguration is totally useless for lesions of uncertain depth. Also, with ablation, there is an elevated risk of damaging tissues like the rectum, bladder, and ureters.
A master surgeon is best equipped for DIE, and, in the author’s opinion, these types of cases should be performed robotically because of the far superior optics and wristed robotic instruments. Further, the surgeon should either be able to handle bowel, bladder, and ureters, including reimplantation where required, or have a well-integrated team ready to participate in a planned fashion. The problem is that it is hard to tell what will be required before surgery. Still, the best efforts through imaging-based mapping and attention to symptoms should be made to adequately prepare for resection/excision of anything found.
DIE most definitely does not mean an automatic hysterectomy recommendation. However, if childbearing is complete, this may need to be discussed for risk vs. benefit to remove all diseased tissue. Similarly, the closer to menopause, the more disease and the higher the risk of malignancy due to family history or genetic testing, the more it is prudent to talk about the risk vs. benefit of ovarian conservation. This should be highly individualized and thoroughly discussed for the best outcome.
Considerations in Surgical Management
Indocyanine Green (ICG) Fluorescence
Indocyanine green (ICG) fluorescence imaging allows surgeons to visualize the details of the ureters and safely remove the maximum amount of infiltrating endometrial tissue without damaging the urinary tract. It is also helpful to determine if a bowel segment that has been operated upon retains good blood supply and viability. This helps avoid complications.
Stenting During Partial Cystectomy or Ureteral Reimplantation
During bladder surgery for urinary endometriosis, surgeons can place stents (tiny plastic catheters) to help protect the ureters (the delicate tubes through which urine travels from the kidneys to the bladder) from further damage or to enhance healing after reimplantation.
Pathology Evaluation
Other than standard pathology evaluation, research evidence suggests several newer assessments might be considered in DIE and OE. Specifically, the more the disease looks clinically aggressive, the more the pathologist should ensure that there is no clear cell cancer component. Beyond that, even with no evidence of cancer, the tissue specimens removed can be assessed for “mitotic index,” meaning whether the pathologist sees many dividing cells. This is more often seen in aggressive disease, even in the absence of cancer. This, in turn, may lead to consideration of some degree of well-tolerated hormone suppression (e.g., micronized progesterone) to potentially reduce recurrence risk. Finally, there are immunohistochemical (IHC) stains for some molecular abnormalities that gene mutations can spawn (e.g., ARID1A). This is not readily available but can be considered, especially in a situation where cancer risk is elevated. In the future, as discussed above, these aberrant molecular pathways will be targeted with precision therapies.
Endometriosis and Fertility
Endometriosis, including DIE, can impact fertility. Consequently, surgeons should employ as many atraumatic surgical techniques as possible to avoid injuring delicate structures in the reproductive system and improve the chances of pregnancy. This is optimized with the robotics platform.
Conclusion
Deep infiltrating endometriosis adds a layer of complexity to the management of endo. Surgery is the optimal therapy, followed by supportive care and strategies to mitigate recurrence if possible. Malignant degeneration is uncommon but possible, which means that, especially with a family history of cancer, genetics testing should be considered. The more complex, the more the need for an endometriosis expert master surgeon in your corner. If the cancer risk is elevated for any of the reasons noted in this article, a gynecologic oncologist should be considered at least as a consultant.
References:
The Diagnosis and Treatment of Deep Infiltrating Endometriosis

How Common is Infertility with Endometriosis
Endometriosis, a medical condition affecting women globally, often poses a significant question:
how common is infertility with endometriosis? This article aims to shed light on this critical question, discussing endometriosis and its relationship with fertility issues, the possible causes and treatments, and the hope that exists for women battling both endometriosis and infertility.
Understanding Endometriosis
Endometriosis is a chronic disorder characterized by the growth of endometrial-like tissue (the lining of the uterus) outside the uterus, inducing a chronic inflammatory reaction. This misplaced tissue can be found on the ovaries, fallopian tubes, and even on the bladder or intestines. The growths can lead to complications, including the formation of scar tissue and cysts, causing pain and potentially affecting fertility.
Read More: Can Endometriosis Be Treated Without Surgery? – Endometriosis Supportive Therapy
Prevalence of Endometriosis
Endometriosis affects an estimated 10–15% of women between 15-50. However, the prevalence dramatically rises to about 25%–50% in women with infertility. Despite the well-supported association between endometriosis and infertility, a causal relationship is yet to be definitively established.
Endometriosis and Infertility: The Connection
Endometriosis can impact fertility in multiple ways, leading to the following complications:
- Impact on Gametes and Embryos: The increased number of inflammatory cells in the peritoneal fluid of women with endometriosis can damage the oocytes (eggs) and sperm and even have toxic effects on the embryo.
- Impairment of Fallopian Tubes and Ovarian Function: Endometriosis can lead to pelvic adhesions, blocked fallopian tubes, and damaged ovaries, which can hinder the process of ovulation and egg release, thus affecting fertility.
- Endometrial Receptivity: The chronic inflammatory state induced by endometriosis can impair endometrial receptivity, affecting the implantation of a pregnancy.
Read More: Can Minimal Endometriosis Cause Infertility
Endometriosis-Associated Infertility: Treatment Approaches
The treatment for endometriosis-associated infertility usually involves a combination of medical and surgical interventions. The choice of treatment depends on several factors, including the age of the woman, the severity of the symptoms, the desire for pregnancy, and the extent of the disease.
Medical Treatment
Medical treatments for endometriosis aim to suppress the growth of endometriosis tissue and relieve symptoms. These treatments include hormonal therapies such as birth control pills, gonadotropin-releasing hormone (GnRH) agonists, and progestins. However, these treatments do not improve fertility rates and are typically used to alleviate pain and other symptoms. They are temporary solutions.
Surgical Treatment
Surgical treatment aims to remove endometrial tissue and restore normal pelvic anatomy. Surgical options include laparoscopy, a minimally invasive procedure. Studies have shown that surgical treatment can improve fertility rates, especially in women with severe endometriosis.
Assisted Reproductive Technology (ART)
In cases where medical and surgical treatments are unsuccessful, assisted reproductive technologies (ART) such as in vitro fertilization (IVF) may be considered. IVF involves the extraction of eggs from the ovaries, which are then fertilized with sperm in a laboratory. The resulting embryos are then transferred back into the uterus.
The Hope for Women with Endometriosis and Infertility
Despite the challenges posed by endometriosis, it’s crucial for women to know that having this condition does not necessarily mean they cannot get pregnant. With the right treatment approach, many women with endometriosis can successfully conceive and carry a pregnancy to term.
In conclusion, understanding how common infertility is with endometriosis is essential for providing effective treatment and support to women dealing with this condition. While endometriosis can indeed impact fertility, it’s important to remember that it’s not the end of the road. With advances in medical technology and treatments, many women with endometriosis are able to overcome their fertility challenges and fulfill their dreams of motherhood.
Read More: Life After Endometriosis Surgery: A Comprehensive Guide
References:
https://www.pennmedicine.org/updates/blogs/fertility-blog/2016/august/endometriosis-and-fertility
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3538128/
https://www.frontiersin.org/articles/10.3389/fsurg.2014.00024
https://obgyn.onlinelibrary.wiley.com/doi/10.1111/aogs.13082

Does Endometriosis Cause Bowel Problems
Endometriosis, a chronic medical condition that affects up to 10% of women worldwide, has a significant impact on various aspects of a woman’s life, including her bowel health. This article will explore the question:
“Does endometriosis cause bowel problems?”
and delve into the symptoms, causes, diagnosis, and treatment of this condition.
What is Endometriosis?
Endometriosis is a medical condition in which tissue resembling the endometrium, the lining of the uterus, grows outside of the uterus. This tissue can grow on various organs, including the ovaries, fallopian tubes, bladder, and even the bowel.
Endometriosis and Bowel Problems
Endometriosis can affect the bowel in various ways, leading to numerous digestive issues. Specifically, endometriosis can grow on or inside the bowel walls, causing symptoms that are often mistaken for other conditions like Irritable Bowel Syndrome (IBS).
Superficial and Deep Bowel Endometriosis
Bowel endometriosis can present in two forms:
- Superficial Bowel Endometriosis: This is when endometriosis is found on the surface of the bowel.
- Deep Bowel Endometriosis: This form of endometriosis penetrates the bowel wall.
In some cases, rectovaginal nodules can start as superficial endometriosis and progress to infiltrate the bowel wall.
Read More: Can Endometriosis Cause Bowel Issues?
Recognizing the Symptoms
The symptoms of bowel endometriosis are similar to those of IBS. However, they can vary with the menstrual cycle, worsening in the days before and during a period. Some common symptoms include:
- Pain with defecation (dyschezia)
- Deep pelvic pain during sex (dyspareunia)
- Rectal bleeding during a period
If you experience these symptoms, it’s crucial to discuss them with your doctor. They may choose to use several techniques for diagnosis, such as a vaginal examination, ultrasound, sigmoidoscopy, laparoscopy, CT, or MRI scan.
Bowel Endometriosis: Causes and Risk Factors
While the definitive cause of endometriosis remains unknown, several potential contributing factors include hormonal imbalances, immune system problems, and genetic factors. Researchers have also found links to genes and stem cells, inflammation, and estrogen levels.
Read More: What Does Bowel Endometriosis Feel Like? Understanding the Pain and Symptoms
Diagnosing Bowel Endometriosis
Diagnosing bowel endometriosis can be challenging due to its similarities with other conditions like IBS. In addition to a physical examination and medical history review, doctors may suggest imaging tests such as transvaginal or transrectal ultrasound, magnetic resonance imaging (MRI), laparoscopy, or barium enema.
Treatment Options for Bowel Endometriosis
The treatment for bowel endometriosis typically involves a combination of painkillers, hormone treatments, and surgeries, depending on the severity of the symptoms. Surgery is usually recommended for bowel endometriosis, with the surgical options varying based on the severity of the condition and the areas affected.
There are three main surgery options for bowel endometriosis:
- The affected segment of the bowel is removed, and the bowel is rejoined (re-anastomosis).
- For smaller areas of endometriosis, the disc of affected bowel is cut away, followed by the closure of the hole in the bowel.
- Affected areas can be “shaved” off the bowel, leaving the bowel intact.
Post-Surgery Recovery and Follow-up
Recovery after any surgery varies depending on the individual. After laparoscopic bowel surgery, you can generally expect to go home within four days. Bowel function may be altered after surgery, particularly with a full resection (re-anastomosis). This does improve over time, although watching your diet to see which food aggravate or improve the situation may be helpful.
The Impact of Delayed Treatment
If bowel endometriosis is not treated properly and promptly, the disease may progress, and quality of life significantly decreases. Small lesions on the bowel can eventually progress and become full-thickness lesions that cause obstruction and may require major bowel surgery.
The Importance of Specialist Care
Because bowel endometriosis deals with your gastrointestinal system, it’s usually not solely treated by a general gynecologist. A collaborative care approach between an endometriosis expert, gastroenterologist, and/or general surgeon may be necessary to treat your bowel endometriosis from all angles.
Read More: Finding an Excision Specialist: What you Need to Know
Conclusion
Understanding the link between endometriosis and bowel problems is vital for improving diagnosis and treatment outcomes. If you’re experiencing symptoms of bowel endometriosis, it’s important to discuss them with your doctor and consider seeing a specialist. In doing so, you’ll be taking an important step towards managing your symptoms and improving your quality of life.
References:
https://www.endometriosis-uk.org/endometriosis-and-bowel
https://www.webmd.com/women/endometriosis/bowel-endometriosis
https://www.everydayhealth.com/endometriosis/bowel-endometriosis/
Endometriosis and constipation
https://drseckin.com/bowel-endometriosis/

Endometriosis Supportive Therapy: Can Endometriosis Be Treated Without Surgery?
Endometriosis is an extremely painful chronic condition, which often also leads to infertility or subfertility, that affects about ten percent of women worldwide. It is characterized by growth of endometrial-like tissue, which normally lines the inside of the uterus, outside of the uterus on pelvic organs, the abdomen, bowel, and beyond. This tissue is not the same as the endometrium, characterized by very different behavior and unique molecular profiles.
Eventually, personalized “theranostic” (therapy and diagnostic) tools will exploit these unique molecular profiles and lead to far better diagnosis, therapy and monitoring approaches. Research is accelerating in this area, which is already very pervasive in other diseases such as cancer and various immuno-inflammatory conditions. Meanwhile, the only therapies that are available to actually treat endometriosis, not just masking of symptoms, are hormonal options and excisional surgery. However, there are major limitations to the argument that hormonal therapies work very well to treat endo rather than simply reduce symptoms. That leaves surgery.
So, in a word, “can endometriosis be treated without surgery?”, the answer is a resounding NO! That is not to say that hormonal and other treatments, including anti-inflammatory and perhaps anti-histamine agents (e.g. Zyrtec), both mainstream and integrative-holistic, don’t help. They might. Let’s unpack this a little bit to give you a roadmap of the options.
Understanding Endometriosis
The exact cause of endometriosis is technically unknown, but we know it is influenced by genetic, genomic, hormonal, immunologic and environmental epigenetic factors. In other words, it is “multi-factorial”. This means the reason you may have endo could be different from why your friend or even your sister does. Endo can also behave very differently because different factors are probably in play in different people. This makes a “standard treatment” hard, if not impossible, to recommend to any given patient. This is changing with the advent of endometriosis bio-molecular pathway research, which will lead to highly individualized targeted treatments. But this is not part of what is available today.
Diagnosis of Endometriosis
Diagnosing endometriosis is very challenging, because the symptoms can mimic other conditions. This is part of the reason that diagnosis is often delayed by 5-10 years and intentional or inadvertent gaslighting is rampant, depending on which specialist was consulted. The doctor may be looking at you through a general practice medical lens, or intestinal, urologic, neurologic or other lenses in forming their opinions.
Rule # 1 is to listen to the patient. This is almost never done to an appropriate extent. Why? Because today’s medical system limitations often lead to five-to-ten-minute visits with a semi-interested and overworked provider who is likely under-informed regarding endometriosis.
When rule #1 is broken, an appropriate evaluation and testing is not likely to be done. Ideally, a clinical suspicion leads to testing that may include ultrasound or MRI, various blood tests, testing for associated conditions and so on. None of these will reliably lead to a diagnosis of endo but can lead to appropriate specialist referrals to get to the root cause of pain, such as endo.
Rule #2 in medicine, in general, is to get a diagnosis before recommending treatment. This is because treatments can be ineffective when treating the wrong condition or, worse, can lead to complications and side effects. Unfortunately, in the author’s strong opinion, this is often violated specifically in endometriosis treatment. A common standard is to offer hormonal therapy to patients to see if it might work because the diagnosis might be endometriosis and endo is, in part, fueled by hormones. This may or may not be reasonable depending upon individual circumstances and choices.
This brings us to rule #3, that we’ll cover next, which proposes that patients should be offered treatment options to select from after informed consent about the potential risks vs the potential benefits based on the best possible scientific evidence. This is not always done very well and certainly depends on the “trust factor” with your selected specialist(s), since scientific evidence is subject to interpretation. Most patients do not realize this.
Conventional Treatment of Endometriosis
Traditional treatment for endometriosis often involves medication or surgery. Medications can include anti-inflammatory pain relievers and hormonal therapies. In the near future medications will include targeted biomolecular non-hormonal therapies, but they are not here yet. Pain relievers are mainly a symptom reducing band-aid and are not intended to treat, so we will not discuss them here either. They can certainly help in overall management, but we will focus on “treatment” in this article.
Hormones aim to either shut down ovarian function (in other words, cut off estrogen) or at least regulate the menstrual cycle, and progesterone analogs, to potentially reduce the growth of endometriosis tissue.
Surgery is used for definitive diagnosis of endo as well as treatment by removing any lesions or implants that are found. In some cases, the two modalities can be used hand in hand, but the order in which they are used, and the nature of the proposed hormonal therapy are important considerations.
Hormonal Treatment
International guidelines are very confusing and inconsistent regarding hormonal therapy for endometriosis. Because of this, recommendations can vary between practitioners. We won’t delve into all these options here, but the following are excellent summary articles on this important topic.
The important points to consider are as follows:
- The ONLY way currently to definitively diagnose endometriosis is through biopsy, usually performed during surgery.
- Starting treatment that can cause extreme side effects and potential long-term harm without first getting a definitive diagnosis seems imprudent. So, if a practitioner offers hormones because they “think” you have endo based on history, examination and perhaps some scans, at least get a second opinion from an endometriosis specialist. This approach is within international guidelines but can cause you a world of misery and potential harm if not managed in expert hands.
- Hormone therapy for endo boils down to either reducing estrogen levels or eliminating estrogen altogether or increasing progestational agent levels to try to medically eliminate endo lesions. Reducing estrogen levels is not possible since there are different types of estrogen, different sources of estrogen and endo lesions themselves can influence local production of estrogen.
- Endometriosis cells differ from endometrial cells that are found in the uterus by being relatively resistant to synthetic progestin or natural micronized progesterone therapy.
- Hormonal therapy is known to reduce pain when endometriosis is the cause. However, studies have shown that pain relief is possible but hormonal therapy fails to significantly retard the growth of endometriosis tissue when objectively tested in pathology laboratories. Further, hormonal therapy cannot eliminate scar tissue or fibrosis caused by endo and this fibrosis by itself can be a cause for pain.
- While unproven, under some circumstances it may be prudent to use less toxic hormonal therapy options to potentially reduce the risk of endo recurrence after surgery.
Surgical Treatment
When symptoms, history, physical exam, scans and laboratory evidence all point to endometriosis as a strong possibility to be the root cause of pain, and/or infertility, minimally invasive surgery should be considered to find out for sure. If endo is diagnosed, then medical hormonal therapy may make sense as part of a highly individualized treatment plan under the guidance of an endo specialist.
The caveat to considering endometriosis surgery is that there are, of course, potential risks and complications even though it is minimally invasive. These risks can be minimized in the hands of an expert surgeon, but they should be considered in a risk-benefit discussion.
More importantly, assuming you have identified an expert endo excision surgeon, surgery is the cornerstone to current effective treatment. While incompletely proven, for many reasons, it appears that excision of endo lesions and scar tissue (fibrosis) rather than burning them away (fulguration) is a better and safer approach. To discover more about surgical considerations, consider the following articles.
Integrative Holistic View of Endometriosis
Since the cause of endo is incompletely understood, but highly multifactorial, and because the reason endo is present in any given individual may vary, either surgery or hormonal therapy or both may fail. Failure is relative. In other words, failure may be defined as no immediate pain improvement, persistent subfertility, or it may mean recurrence years later. These are very different scenarios, requiring different approaches. Also, it’s important to consider whether or not associated conditions have been addressed, such as SIBO or other microbiome irregularities, other inflammatory immune-modulated disease and so on. Finally, pelvic floor physical therapy is not just a symptom band-aid but a critical co-treatment for pelvic floor function before and after surgery. These topics are all beyond the scope of this article, but you can discover more by reading the following articles.
If expert excision surgery and supportive hormonal therapy, when used, fails to alleviate pain then supportive pain management can still improve quality of life. This can be mainstream pain and anti-inflammatory medications like non-steroidal anti-inflammatory (NSAID), nerve block injections, electrical stimulation modalities and/or more holistic approaches including acupuncture, acupressure, mind-body biofeedback approaches such as HeartMath, herbals, aromatherapy and more.
Kicking it up a notch, here is something you do not see covered much other than in a very superficial manner. It is not rocket science but is not simplistic at the potential treatment level either. However, it is something you can implement in a proactive way at any point in your journey. Specifically, this is the impact of nutrition and lifestyle choices, as well as well-selected and targeted supplements, but drilled down a lot further than simply eating right, exercising and de-stressing.
Upcoming bio-molecular therapies will target specific biological pathways that we are now beginning to better understand. Many pathways are already identified, many not. The problem is that there are no mainstream medical therapies, yet which can target these pathways safely and effectively. We know from other related genomically modulated inflammatory diseases, like cancer and auto-immune disorders, that these treatments take a while to develop and offer safely. Meanwhile, many of the genomic, metabolic and epigenetic abnormalities that influence endo are known or at least partly known. With few exceptions, while it is too early to safely use pharmaceutical agents to modulate these abnormalities, nutrients, specific exercise, toxin avoidance, and even state of mind can affect the same pathways abnormalities without risk.
Nutrigenomics and Epigenetics
How do toxins or stress adversely affect your health, while healthy diet and exercise positively influence your health? In large part, relatively new sciences like metabolomics and genomics, and their derivatives, explain this. You are born with your genes and, so far, you can’t alter that deck of cards. Some genes may be “bad” and increase your risk of endo, as well as other diseases. However, not everyone with some bad genes develops disease. The most famous examples are identical twins who inherited the exact same genetics yet might look a little different (e.g. eye or hair color) and often get different diseases. Why?
Anything and everything you eat, drink, get exposed to via skin or breathing, or even think about or emote, can affect your genes through epigenetics. This means these substances and neurochemicals, good or bad, can turn genes on and off. Of course, it is infinitely more complex than that and multiple genes affect one process in many cases. However, you can actively modulate your inflammatory and oxidative state. Do we know what veggie or what thought or what toxin turns what specific gene on or off? No. But we do know how these gene-controlled pathways synergize and work together to create health or facilitate disease.
Conclusion
Surgery is a cornerstone to definitive diagnosis of endo and serves as very important part of treatment. The path to success is a correct diagnosis, attention to detail and a highly individualized treatment plan. This can only be carried out in consultation with endometriosis specialists in medical and surgical management.
Unfortunately, it is not easy to find someone or a team that can fit your needs, but it is a crucial step forward to seek out the best you can. The more complex your situation (e.g. possible advanced disease or repeat surgery) the more you need an excision surgeon with master surgeon skills. Ideally you want a specialist who is not only a surgeon but also capable of guiding you through any additional treatment options you may need, mainstream and holistic. While a master excision surgeon and integrative endo specialist is hard to come by, many have a team that can fulfill your needs.
References:
Endometriosis: Etiology, pathobiology, and therapeutic prospects
Brassica Bioactives Could Ameliorate the Chronic Inflammatory Condition of Endometriosis
Diet and risk of endometriosis in a population-based case–control study
Emerging Drug Targets for Endometriosis
Updated Post: July 09, 2024

Can Endometriosis Grow Inside the Bladder
Endometriosis, a medical condition that affects many women worldwide, is often associated with the reproductive system. However, this disorder can manifest in other regions of the body, leading to a pertinent question:
Can Endometriosis Grow Inside the Bladder?
Yes, endometriosis can indeed grow inside the bladder, although this is less common than other locations. This condition, known as bladder endometriosis, affects approximately 1-2% of women with endometriosis.
In this article, we will explore the nature of endometriosis, its ability to affect the bladder, the related symptoms, causes, diagnosis, and available treatment options.
Understanding Endometriosis
Endometriosis is a gynecological condition where cells similar to the ones lining the uterus, known as endometrial-like cells, grow outside of the womb. These cells can attach themselves to various organs such as the ovaries, fallopian tubes, and in rare instances, the bladder. This phenomenon is known as bladder endometriosis.
Bladder Endometriosis: An Overview
Bladder endometriosis is a specific form of endometriosis where endometrial-like cells grow inside or on the surface of the bladder. These cells respond similarly to hormones as the cells within the womb, causing them to build up, break down, and bleed. However, being outside of the uterus, these cells have no way of exiting the body, leading to inflammation, pain, and scar tissue.
Bladder endometriosis is considered a rare form of the disorder, affecting only about 1 to 2% of patients with endometriosis. However, for those suffering from deep endometriosis (DE), a severe form of the condition, the prevalence increases to nearly 50%.
There are two types of bladder endometriosis:
- Superficial Endometriosis: Endometrial-like cells are found on the outer surface of the bladder.
- Deep Endometriosis: Endometrial-like cells infiltrate the bladder lining or wall. This infiltration can cause a nodule, potentially affecting the ureter.
Recognizing the Symptoms of Bladder Endometriosis
The symptoms of bladder endometriosis can vary, often aligning with the menstrual cycle and intensifying during or just before a period. However, many women may remain asymptomatic until the disease has progressed significantly.
Common symptoms of bladder endometriosis include:
- Bladder irritation
- Urgency to urinate
- Pain when the bladder is full
- Occasional presence of blood in the urine during menstruation
- In some cases, pain in the area of the kidneys
Identifying the Root Causes of Bladder Endometriosis
The exact cause of bladder endometriosis remains unknown. However, several theories have been proposed, including:
- Early Cell Transformation: Cells leftover from embryonic development may transform into endometrial-like cells.
- Surgery: Endometrial cells may spread to the bladder during pelvic surgeries, like a cesarean delivery or hysterectomy.
- Hematogenous/Lymphatic Spread: Endometrial-like cells might travel through the blood or lymph system to the bladder.
- Genetic Factors: Endometriosis has been observed to run in families, indicating a possible genetic link.
Diagnosing Bladder Endometriosis
Bladder endometriosis is diagnosed through a comprehensive evaluation involving a physical examination, medical history, and various diagnostic tests. These tests may include:
- Vaginal examination
- Ultrasound
- Urine sample analysis
- Cystoscopy and Laparoscopy
- CT and/or MRI scan
Bladder Endometriosis Treatment Options
The primary aim of bladder endometriosis treatment is to control symptoms and inhibit the growth of endometrial-like cells. Treatment options include:
Medication
Hormone therapy can slow the growth of endometrial-like cells, relieve pain, and help preserve fertility.
Surgery
Surgery is typically required for bladder endometriosis. The surgical options can vary depending on the severity and area affected. The areas affected by endometriosis can be excised to remove them.
Complications and Prognosis
If left untreated, bladder endometriosis could lead to kidney damage. However, surgery can prevent this complication. The condition doesn’t directly affect fertility, but if endometriosis is present in other parts of the reproductive system, conceiving might be challenging.
Endometriosis, including its bladder variant, is a chronic condition that can impact daily life. Yet, it can be effectively managed with proper treatment and a supportive healthcare team.
Final Thoughts
So, to answer the question, Can endometriosis grow inside the bladder? — yes, it can. However, through increased awareness, early diagnosis, and effective treatment strategies, bladder endometriosis can be managed, improving the quality of life for those affected.
References:
https://www.endometriosis-uk.org/endometriosis-and-bladder
Bladder Endometriosis symptoms
Endometriosis Symptoms And Treatments
https://www.healthline.com/health/womens-health/bladder-endometriosis
https://consultqd.clevelandclinic.org/urinary-tract-endometriosis-has-serious-health-implications/

Do Endometriomas Automatically Make You Stage 4?
Endometriosis, a complex and often painful condition, is characterized by the growth of endometrial-like tissue outside the uterus. This tissue, which differs molecularly and in behavior from the lining of the uterus, can cause severe discomfort and various health complications. One such complication is the formation of endometriomas, sometimes referred to as “chocolate cysts”, which predominantly affect the ovaries. They’re named for their dark, chocolate-like appearance, resulting from the accumulation of old blood within the cyst.
But does the presence of endometriomas automatically classify a patient as having stage 4 (also designated Stage IV) endometriosis? This primer delves into the stages of endometriosis, the nature of endometriomas, and the relationship between the two.
Understanding Endometriosis and Its Stages
Endometriosis is categorized into four stages according to the American Society of Reproductive Medicine (ASRM), with each stage reflecting the location, extent, and superficial vs deep endometriosis implants, presence and severity of adhesions, and the presence and size of ovarian endometriomas. The current revised ASRM system (rASRM) was adopted in 1996 and remains the most common staging system. Unfortunately, there is a lot of inter-observer variation, so reproducibility of the score is poor. It also is limited because it mixes visual staging and actual biopsy proven staging. So, one surgeon might call it one stage and another surgeon may arrive at a different stage. In addition, rASRM stages do not correlate well with degree of pain and does not fully consider presence and location of deeply infiltrating endometriosis (DIE).
For all of the above reasons, other staging systems have been introduced. The ENZIAN system, which more robustly considers the location and depth of DIE, was intended to supplement the rASRM system but due to numerous misunderstandings it is not widely used. The endometriosis fertility index (EFI) focused mainly on predicting pregnancy rates. The American Association of Gynecological Laparoscopists (AAGL) proposed a comprehensive system to try to address pain, infertility/subfertility, and surgical excision difficulty. However, it was only recently published in 2021, continues to have limitations of not addressing upper abdominal and extra-abdominal disease, and is not yet widely accepted.
So, we are left with the rASRM system in terms of best communicating surgical outcomes, treatment planning and comparing results. The Stages are based on a numerical score and are as follows:
Stage I: Minimal Endometriosis
In stage I, there are only a few small clumps of endometriosis tissue, also known as implants. These may be found in the tissue lining the abdomen or pelvis.
Stage II: Mild Endometriosis
In stage II, there are more implants than in stage I, which may be either superficial or deep, with mild adhesions. Stage II is typically characterized by more extensive endometriosis with deep implants present.
Stage III: Moderate Endometriosis
In stage III, deep implants of endometriosis tissue are present. Adhesions may be dense rather than filmy and thin. As a result, endometriosis at this stage is more widespread than in stage II.
Stage IV: Severe Endometriosis
Stage IV, or severe endometriosis, is typically associated with numerous deep endometriosis plaques, large endometriotic cysts on one or both ovaries and many dense adhesions. There is usually also extensive scar tissue in the abdomen and signs of intense inflammation and scarring or fibrosis.
Read More: Can Endometriosis Cause Bowel Issues?
The Nature of Endometriomas
Endometriomas are endometriosis cysts that primarily affect the ovaries. Endometriomas can occur on one ovary or both and affect between 20-40% of patients with endometriosis, many of whom also have stage III-IV disease. The origin of endometriomas is incompletely known, just like endometriosis in general, but likely multifactorial in principle.
Endometriomas and Stage 4 Endometriosis: The Connection
The question is, “Do endometriomas automatically make you stage 4?” The answer is not straightforward. The presence of ovarian endometriosis or an endometrioma of course contributes to the staging of endometriosis. Each ovary can contribute between 1 and 20 points, varying based on tiny implants to endometriomas greater than three centimeters in size. However, the presence of endometriomas alone does not automatically classify a patient as having stage 4 endometriosis, which requires 40 or more points. In addition to ovarian endometrioma, presence or absence of surrounding adhesions also contributes to the point total. Also, larger endometriomas are often associated with extensive deep pelvic disease. So, in general, small endometriomas may not mean Stage 4. But larger ones are quite likely to mean Stage 4 disease is present.
Read More: What Does Bowel Endometriosis Feel Like? Understanding the Pain and Symptoms
Treatment Options for Stage 4 Endometriosis and Endometriomas
The treatment of stage 4 endometriosis and endometriomas is complex and highly individualized. It depends on various factors, including the patient’s symptoms, age, desire for pregnancy, and overall health.
Treatment options for stage 4 endometriosis can include a combination of hormonal therapy, pain management, and surgery. While hormonal therapy may help control pain it is highly unlikely to shrink endometriomas, let alone resolve them, or effectively treat endometriosis. This is due to the relative resistance of endometriosis to progesterone and progestins and incomplete dependence on estrogen. There are major potential health risks and this should be part of the discussion with your chosen endometriosis specialist. Pain management strategies include over-the-counter and prescription medications, as well as physical modalities like pelvic floor therapy and transcutaneous electrical nerve stimulation (TENS) units. While this can help manage chronic pain associated with the condition this does not treat the root cause, which is endometriosis and resulting fibrosis.
Minimally invasive surgery under the care of an extremely well trained surgeon is the cornerstone of advanced endometriosis treatment. This is not surgery that should be undertaken by novices or most general gynecologists. The reason is mainly due to the fact that anatomy can be severely distorted, making surgery very challenging in terms of achieving excision while limiting complications which can be life threatening or at least very morbid.
Specifically regarding endometriomas, endometriomas require excision, not drainage. Draining is very ineffective and the endometrioma can soon recur. Ideally, any surgical spillage should be minimized because it is not just old blood but also potentially endo-related stromal stem cells, which can implant and grow elsewhere. Overall, the planning and timing of surgery varies significantly. Often decisions have to be made based on whether or not fertility is the main concern or pain, or both in equal degrees. Surgical planning is complex and requires a master surgeon for optimal outcomes. Especially for the management of Stage 4 endometriosis and endometriomas a highly trained and skilled endometriosis specialist and surgeon is mandatory for your success.
Read More: Life After Endometriosis Surgery: A Comprehensive Guide
References:
Risk factors for coexisting deep endometriosis for patients with recurrent ovarian endometrioma
Diagnosis and management of endometriosis

Endometriosis-Related Infertility – Minimal Causes
Endometriosis, a common gynecological condition, has been frequently associated with infertility. However, the question remains: can minimal endometriosis cause infertility? This comprehensive article aims to delve into the connection between endometriosis, particularly in its minimal stage, and fertility issues.
Defining Endometriosis
Endometriosis is a medical condition characterized by the growth of endometrium-like tissues outside the uterus. These tissues can adhere to various pelvic structures like the ovaries, fallopian tubes, and even the intestines and bladder, causing irritation, inflammation, and scar tissue formation.
Stages of Endometriosis
Endometriosis is categorized into four stages:
- Stage I (Minimal): Small endometriotic implants with no scar tissue.
- Stage II (Mild): More extensive implants, involving less than 2 inches of the abdomen, without scar tissue.
- Stage III (Moderate): Severe endometriosis with deep implants and possible formation of endometriotic cysts or ‘chocolate cysts’ in the ovaries.
- Stage IV (Severe): Numerous endometriotic implants, possibly large endometriotic cysts in the ovaries, and scar tissue formation around the reproductive organs.
Read More: Understanding How Endometriosis Can Cause
The Connection Between Endometriosis and Infertility
It’s estimated that 30% to 50% of women with endometriosis may experience infertility. Even in cases of minimal or mild endometriosis, the disease may still impact fertility in numerous ways, including:
- Distorted pelvic anatomy due to scar tissue and adhesions
- Inflammatory response causing a hostile environment for eggs, sperm, and embryos
- Altered immune system functionality
- Changes in the hormonal environment affecting egg quality and embryo implantation
However, it’s essential to note that endometriosis does not necessarily equate to infertility. Many women with endometriosis, even in severe stages, can conceive naturally or with fertility treatments.
Exploring the Question: Can Minimal Endometriosis Cause Infertility?
The impact of minimal endometriosis on fertility is a contentious subject. The disease, even at its earliest stage, can cause inflammation and subtle changes in the pelvic environment, potentially affecting fertility. However, many women with minimal endometriosis conceive without issues, leading some researchers to suspect that other factors, possibly genetic or immunological, might be at play in cases of endometriosis-associated infertility.
Diagnosing Endometriosis
Diagnosing endometriosis can be challenging, as many women with infertility migh experience no symptoms. The gold standard for diagnosis is a surgical procedure known as laparoscopy, allowing the doctor to visually inspect the pelvic organs for endometriotic lesions and scar tissue, and take samples for histopathology.
Read More: Life After Endometriosis Surgery: A Comprehensive Guide
Evaluating Fertility
Before initiating any fertility treatment, a comprehensive fertility evaluation is recommended. This includes hormonal and blood tests, an assessment of ovarian reserve, a sperm analysis for the male partner, and possibly a laparoscopy to confirm the presence and extent of endometriosis.
Read More: Pelvic Floor Physical Therapy: What you Need to Know
Treatment Options for Endometriosis-Related Infertility
The treatment approach for endometriosis-related infertility is multifaceted, depending on the stage of endometriosis, the woman’s age, and the presence of other fertility factors.
Surgical Treatment
For women with Stage I or II endometriosis, surgical removal of endometriotic tissue may improve pregnancy rates. However, for women aged 35 or older, other fertility treatments might be recommended in addition to surgery.
Medical Treatment
Medical treatments aim to suppress endometriosis growth by reducing estrogen levels. However, these treatments, including hormonal contraceptives and Gonadotropin-Releasing Hormone (GnRH) agonists, prevent pregnancy during use.
Assisted Reproductive Technology (ART)
In cases where pregnancy does not occur naturally or following surgery, ART methods such as Intrauterine Insemination (IUI) or In Vitro Fertilization (IVF) may be recommended. The success rates of these treatments vary depending on the woman’s age, ovarian reserve, and specific fertility issues.
Conclusion: Can Minimal Endometriosis Cause Infertility?
While minimal endometriosis can potentially affect fertility, it does not guarantee infertility. A comprehensive evaluation and personalized treatment plan can help women with endometriosis, even at minimal stages, to conceive successfully. However, further research is needed to fully understand the complex relationship between endometriosis and fertility.
References:
https://www.uptodate.com/contents/endometriosis-treatment-of-infertility-in-females

Diaphragmatic Endometriosis: An In-Depth Analysis
Diaphragmatic endometriosis is a chronic health condition that manifests when tissues akin to the endometrial lining start to grow outside the uterus. This exogenous growth of endometrial-like tissue can be found in various areas such as the ovaries, fallopian tubes, and bladder. However, endometriosis can also occur in less common areas like the diaphragm, organs in the upper abdomen, like the stomach, in the retroperitoneum like the lymph nodes and kidneys, and so on. Of these uncommon findings, finding some amount of endo on the diaphragm is perhaps most common.
Understanding the Diaphragm
The diaphragm is a large, dome-shaped muscle located beneath the lungs, responsible for the crucial function of respiration. Acting as a separation between the abdominal and thoracic (chest) cavities, its involuntary contraction and relaxation facilitate the breathing process. The diaphragm also has openings that allow important structures such as the esophagus and major blood vessels to pass through.
What is Diaphragmatic Endometriosis?
In most cases, diaphragmatic endometriosis affects the right side of the diaphragm. The endometrium-like tissue that builds up on the peritoneal surface of the diaphragm reacts to the menstrual cycle’s hormones in the same way it does in the uterus, which can cause a range of symptoms in the affected individuals.
Read More: Understanding How Endometriosis Can Cause
Symptoms of Diaphragmatic Endometriosis
The most common symptoms of diaphragmatic endometriosis include pain in the chest, upper abdomen, right shoulder, and arm. This pain typically occurs around the time of your period and may get worse when you take deep breaths or cough. In rare cases, if it grows through the diaphragm and involves the lungs, it can lead to a collapsed lung. This is known as catamenial pneumothorax. However, diaphragmatic endometriosis can often be asymptomatic while only small superficial implants are present. Hence, surgery usually involves at least looking at the diaphragms to document if there are any endo implants even if there are no symptoms in that area.
Causes of Diaphragmatic Endometriosis
The exact causes of diaphragmatic or other types of endometriosis remain unknown. However, it is plausible that endo cells from the pelvis can travel throughout the abdomen and up into the diaphragm. What makes them implant and grow there is unknown. Alternatively, there are other possible etiologies, such as lymphatic or blood stream spread to this area or direct transformation of stem cells or growth of embryologic remnants into endometriosis implants. This is all likely facilitated or repressed by genetic and genomic molecular signalling that is only now coming to be appreciated and unraveled.
Read More: What Does Bowel Endometriosis Feel Like? Understanding the Pain and Symptoms
Diagnosis of Diaphragmatic Endometriosis
Diagnosing diaphragmatic endometriosis can be challenging. Diagnosis often involves a combination of medical history, physical examination, and imaging tests such as a CT (computed tomography) scan or MRI (magnetic resonance imaging).
The most reliable way to diagnose diaphragmatic endometriosis is via minimally invasive laparoscopic or robotic surgery. Ideally, the surgeon who is excising endo in the pelvis can also remove diaphragmatic implants or have a surgeon available as part of the team, who can do so. In the much rarer event that endo is suspected to be inside the chest and/or growing on or in the lungs, a thoracic surgeon should be consulted.
Treatment of Diaphragmatic Endometriosis
Surgery is the main treatment for diaphragmatic endometriosis and this can usually be accomplished using minimally invasive laparoscopic or robotic surgery. Again, the excision surgeon or surgical team should be capable of removing endo from the diaphragms.
In some cases, endo is not suspected to be growing on the diaphragm. In that case, if the surgery cannot be safely accomplished by the surgeon or surgeons on the team, it is best to back out and not cause more harm than good. The diaphragm is very thin and it is rather easy to enter the chest as part of the excision. In expert hands, that is not a problem. However, going one step beyond diaphragmatic endo, if it is unclear whether or not the endo may be crossing into the chest cavity it is best to back out, re-evaluate with proper imaging and consultation and perform the surgery with a thoracic surgeon at a later date.
Complications of Diaphragmatic Endometriosis
In relatively rare cases, endometriosis of the diaphragm can lead to defects or holes forming in the diaphragm. Endo can then grow into the chest cavity and possibly involve the lungs. This can lead to life-threatening complications such as a collapsed lung during your period (catamenial pneumothorax) or significant bleeding into the chest, also compressing the lung.
Read More: Can Endometriosis on Ureter Cause Kidney Shooting Back Pain?
Conclusion
In conclusion, while it is relatively uncommon, endometriosis can indeed spread to your diaphragm. Under more rare circumstances it can even grow into the chest and lungs. Expert endometriosis consultation and care is always prudent. But if you are experiencing upper abdominal or chest symptoms as discussed this this article, it become crucial.
References
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6018178/

Can Ureteral Endometriosis Cause Kidney Shooting Back Pain?
Endometriosis is a common gynecological condition that affects many women during their reproductive years. While it typically manifests in the pelvic region, in some instances, it may invade other organs, including the urinary system. This article explores the question: Can endometriosis on the ureter cause kidney shooting back pain?
About Endometriosis
Endometriosis is a chronic disease characterized by the presence of endometrial-like tissue outside the womb. This could include the ovaries, fallopian tubes, and the lining of the pelvic cavity. In some extreme cases, endometrial tissue may also affect organs outside the pelvic cavity, such as the bladder, bowel, or kidneys.
Read More: Understanding Endometriosis: Unveiling the Common Symptoms and Their Impact
Understanding Ureteral Endometriosis
Ureteral endometriosis is an uncommon manifestation of the disease, accounting for about 1% of all endometriosis cases. It involves the ureters, the tubes that transport urine from the kidneys to the bladder. This condition can lead to urinary tract obstruction, resulting in hydronephrosis, which is the swelling of a kidney due to a build-up of urine.
The Kidney-Endometriosis Connection
The kidneys can be impacted when one or both of the ureters become affected by endometriosis. The section of the ureter that is usually affected sits below the pelvic area.
Symptoms of Kidney Endometriosis
Kidney endometriosis can be asymptomatic for several years. If a person who has undergone surgery to treat endometriosis has ongoing urinary problems such as pain and infections, it may suggest the presence of urinary tract or kidney endometriosis. Symptoms may include:
- Pain in the lower back that gets worse with a monthly menstrual cycle. That pain can also extend down through the legs.
- Blood in the urine that can co-occur with the menstrual cycle
- Difficulty urinating
- Recurrent urinary tract infections
Read More: Understanding How Endometriosis Can Cause
Diagnosis of Ureteral Endometriosis
The diagnosis of ureteral endometriosis relies heavily on clinical suspicion. As a result, they often misdiagnose patients with kidney cancer. This can lead to patients not receiving treatment on time, or receiving the wrong kind of treatment.
Read More: Life After Endometriosis Surgery: A Comprehensive Guide
Treatment Options
Kidney endometriosis can lead to kidney damage and even kidney failure if left untreated. However, the best approach is to treat the condition by removing endometriosis lesions with minimally invasive laparoscopic surgery.
The Silent Threat of Kidney Failure
One of the most concerning aspects of ureteral endometriosis is the silent threat of kidney failure. It is estimated that as many as 25% to 50% of nephrons are lost when there is evidence of ureteral endometriosis, and 30% of patients will have reduced kidney function at the time of diagnosis.
Impact on Kidney Health
The good news is that if one kidney isn’t functioning due to endometriosis, you can survive on the other kidney. So, if you find out you only have one fully-functioning kidney, it’s essential to take care of it.
Conclusion
In conclusion, while endometriosis is typically a pelvic condition, it can venture beyond and affect the urinary system, including the kidneys. This can lead to severe complications, including kidney failure. Therefore, it’s crucial for women with endometriosis to be aware of the potential symptoms and seek medical advice if they experience any signs of kidney problems. The early detection and treatment of ureteral endometriosis are crucial to preserving kidney function and overall health.
References:
https://drseckin.com/kidney-endometriosis/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3535807/