
Understanding Neuroproliferative Vestibulodynia and the Connection with Endometriosis
A few weeks ago, we delved into the intricacies of vestibulodynia and its potential association with painful intercourse in individuals with endometriosis. We presented an overview of vestibulodynia subtypes in general and discussed one of the more common presentations we see in those with endometriosis – hormonally mediated vestibulodynia which in many is caused from the side effects of the birth control pill, which are offered as first line “treatments” for endometriosis. Today, we will focus on another subtype, neuroproliferative vestibulodynia (NPV), and the fascinating connections are are seeing in these two conditions, including the role of mast cells.
If you missed our previous discussion on painful sex and vestibulodynia, you can find the detailed information here.
Recent research endeavors have yielded valuable insights into the fundamental causes of these conditions, unveiling a shared mechanism involving neuroproliferation, characterized by an increase in nerve cells. Furthermore, an elevated presence of mast cells—integral components in immune function—has been observed both in endometriosis tissue and the vestibule of individuals diagnosed with neuroproliferative vestibulodynia (NPV).
Individuals diagnosed with NPV undergo a surgical procedure which is excised to remove the problematic tissue, sound familiar?
This surgical approach has demonstrated notable success in alleviating pain for individuals affected by NPV. Dr. Paul Yong, an OBGYN, endometriosis surgeon, and researcher based in Canada, addressed the parallels between these two conditions during his presentation titled ‘Neuroproliferative Dyspareunia’ at the ISSWSH’s annual conference in March 2022. Dr. Yong’s insights laid the foundation for subsequent research, with Dr. Irwin Goldstein initiated further exploration earlier this year. We were lucky enough to be able to speak directly with these two on our podcast iCarebetter: Endometriosis Unplugged, available on Spotify (linked here) and Apple Podcasts.
A Quick Overview
Vestibulodynia
Vestibulodynia is a condition characterized by pain in the vestibule, the area of tissue within the vulva that surrounds the opening of the vagina. This pain can be described as sharp, stinging, burning, or hypersensitive, and can occur spontaneously or be provoked by touch or pressure, and many people will report superficial dyspareunia (or pain upon insertion) which is not limited to penis in vagina sex. Vestibulodynia is a subcategory of a broader condition called vulvodynia, which refers to chronic pain in the vulva.
Endometriosis
On the other hand, endometriosis is a condition where tissue similar to the lining of the uterus grows outside the uterus, often causing pain and fertility issues. This condition can cause deep dyspareunia, or pain with deep vaginal penetration. Like vestibulodynia, the pain associated with endometriosis can be chronic and can significantly impact the quality of life.
The Concept of Neuroproliferative Dyspareunia
Both vestibulodynia and endometriosis can lead to pain during sexual intercourse and the term neuroproliferative dyspareunia, is in reference to the source of the pain. Both tissues have been shown to have neuroproliferation, or increased growth, of nerve endings in the areas affected by these conditions and we are now seeing an aberrant amount of mast cells as well also contributing to inflammation. This overgrowth of nerves, and presence of excessive mast cells, can lead to heightened sensitivity and pain during vaginal penetration, both superficially, as well as deep.
Neuroproliferation in Vestibulodynia
In the case of vestibulodynia, research has shown that there are too many nerve endings in the vestibule tissue. This overgrowth of nerves, or neuroproliferation, is still under investigation. However, it is believed that this could be due to a congenital birth defect, with the excess nerve endings developing very early. There are two types of neuroproliferative vestibulodynia: primary (congenital) and secondary (acquired). In primary vestibulodynia, individuals have experienced pain their entire lives though usually identified shortly after menses or with first attempts at penetration (sex, tampons, speculum exams) while in secondary or acquired vestibulodynia, pain develops later in life usually after an event such as an allergic reaction, chronic yeast infections or other infection, and there has typically been a period of normalcy prior to these event.
Neuroproliferation in Endometriosis
In endometriosis, nerve fibers have been found around endometriosis lesions in the pelvic peritoneum. These nerve fibers are more numerous in individuals with endometriosis compared to those without the condition. The increase in nerve fibers is believed to be driven by the immune response to infection or allergy, leading to nerve proliferation.
Symptoms of Neuroproliferative Vestibulodynia and Endometriosis
Vestibulodynia Symptoms
People with vestibulodynia typically experience pain at the entrance of the vagina, called the vestibule. This pain can be described in various ways, including as sharp, stinging, burning, or hypersensitive. This pain can also be classified by when it occurs, with provoked vestibulodynia referring to pain that occurs with touch or pressure, while unprovoked pain occurs spontaneously.
Endometriosis Symptoms
In endometriosis, the pain is typically experienced deeper within the pelvis, often during or after sexual intercourse. This deep dyspareunia can also be accompanied by other symptoms, such as painful periods (dysmenorrhea), painful bowel movements, and chronic pelvic pain to name a few.
For more signs and symptoms, check out our blog Endometriosis Signs and Symptoms: Everything You Need to Know.
Causes of Neuroproliferative Vestibulodynia and Endometriosis
Causes of Vestibulodynia
The exact causes of vestibulodynia are still being investigated. However, research suggests that the overgrowth of nerves in the vestibule tissue could be triggered by signaling from immune cells in the tissue. This could be due to a congenital birth defect, resulting in excess nerve endings developing very early, or it could be an acquired condition, developing later in life possibly due to infection or allergy.
Causes of Endometriosis
The causes of endometriosis are also not fully understood though we have began to shift away from the narrative that it is caused by retrograde menstruation, and towards a genetic basis. We hope that in the future with new research, we will be able to fully understand the cause (or causes) and have optimal treatment methods to address the heterogeneity of this disease.
You can read more about these theories in our blogs listed below:
- The History of Endometriosis: Unraveling the Theories and Advances [or lack thereof]
- Is Endometriosis Genetic? Understanding the Genetic Links in Endometriosis.
There has been limited research in the role of mast cells in endometriosis thus far, and Dr. Irwin Goldstein, MD has now successfully demonstrated in a case study of a patient with NPV, her endometriosis pathology also demonstrated similar findings, as well as a biopsy taken of her colon during a colonoscopy.
Thank you to Paul Yong, MD for this information, here is a comparison of endometriosis and NPV and common mechanisms in each.
| Endometriosis | NPV | |
| Prevalence | Approx 10% | Approx 10% |
| Diagnosis | Histological diagnosis(ectopic endometrial-like epithelium/stroma) | Clinical diagnosis (but normal vestibular histology consists of epithelium/stroma) NPV – mast cells and excessive nerve endings |
| Description of Dyspareunia | Deep | Superficial |
| Nerve Density | Increased local nerve density compared to controls | Increased local nerve density compared to controls |
| Neutrophins | Increased NGF expression by endometriosis stroma when higher nerve fibers | Increased NGF expression by immune cells in vestibulodynia in areas with more nerve fibers |
| Inflammation | Increased IL-1b expression by endometriosis when higher nerve fibres Endometriosis stromal cells, when stimulated by IL-1b, increase production of NGF and promote nerve fibre development in a PC12 2q13 polymorphism (adjacent to IL-1 family genes) Mast cells Tryptase | Increased IL-1b in tissues in vestibulodynia vs. controls; Not observed in another study (Eva) Vestibular fibroblasts from patients with vestibulodynia expressed more IL-1b compared to external vulvar fibroblasts and to controlsIL-1b and IL-1R antagonist gene polymorphism Mast cells Tryptase Heparanase |
References
- Mwaura, A. N., Marshall, N., Anglesio, M. S., & Yong, P. J. (2023). Neuroproliferative dyspareunia in endometriosis and vestibulodynia. Sex Med Rev. https://doi.org/10.1093/sxmrev/qead033
- Goldstein, S., Yee, A., & Goldstein, I. (2022). Severe Allergic, Inflammatory and Traumatic Reactions of the Vestibule Associated with Acquired Neuroproliferative Vestibulodynia. The Journal of Sexual Medicine, 19(8, Supplement 3), S3. https://doi.org/https://doi.org/10.1016/j.jsxm.2022.05.012
Bornstein, J., Goldstein, A. T., Stockdale, C. K., Bergeron, S., Pukall, C., Zolnoun, D., Coady, D., consensus vulvar pain terminology committee of the International Society for the Study of Vulvovaginal, D., International Society for the Study of Women’s Sexual, H., & International Pelvic Pain, S. (2016). 2015 ISSVD, ISSWSH, and IPPS Consensus Terminology and Classification of Persistent Vulvar Pain and Vulvodynia. J Sex Med, 13(4), 607-612. https://doi.org/10.1016/j.jsxm.2016.02.167

Endometriosis and Painful Intercourse: Is it Really Just Endometriosis?
Those with endometriosis oftentimes will experience pain and discomfort with intercourse, especially pain with deep thrusting, also known as deep dyspareunia. However, many people also experience a different type of pain that extends beyond intercourse – superficial dyspareunia or pain upon entrance. Many people will have been diagnosed with ‘vaginismus’ and oftentimes given dilators, told to “just relax” or “have a glass of wine,” which is terrible advice. While some may have vaginismus, or pelvic floor dysfunction, for many the culprit could be that birth control pill that was given to you and advertised as a treatment for your endometriosis. It is a mixed bag on how many people benefit from the use of oral contraceptive pills (OCPs), and they can be a helpful tool for many. That being said, one thing is certain: medications always have consequences – sometimes good, sometimes not good.
In today’s blog, we will discuss a condition called vestibulodynia, and we will specifically cover hormonally associated vestibulodynia which is a prevalent health concern that results in pain in the vestibule, the tissue within the vulva at the opening of the vagina which also surrounds the urethra. It’s a subcategory of a broader term, vulvodynia, which refers to chronic pain in the vulva. This article aims to provide an in-depth understanding of vestibulodynia, its causes, symptoms, and effective treatment methods.
Vestibulodynia vs Vulvodynia vs Vaginismus?
Vestibulodynia is a general term used to describe discomfort in the vestibule, a part of the vulva that sits at the entrance of the vagina. The vestibule is the transition point between external and internal, similar to the entrance of a building. Vulvodynia is the broader category that includes vestibulodynia but can be pain anywhere in the vulva and typically is present for longer than three months and has specific causes and associated factors. Vaginismus lies within these and often is a misdiagnosis, the term refers to a chronic muscle spasm upon penetration or attempted penetration. This is one of the oldest terms used and while some may have true vaginismus, in the case of endometriosis there are much more likely causes, such as the birth control pill and other hormonal suppressive agents.
Think about it – if you touch a hot stove, the muscles in your shoulder and arm reflexively pull you away. If a penis, speculum, finger, or tampon hit tissue that is painful and irritated, the surrounding muscles will tense reflexively because it is painful. So yes, there is a muscle spasm, but the cause of the spasm is the inflamed and painful vestibule, possibly due to consequences from the birth control pill. There are other causes of pain here, which we will cover in future blogs.
Subtypes of Vestibulodynia
Recent research has led to the identification of a few subtypes of vestibulodynia based on the root cause of the discomfort:
· Neuroproliferative vestibulodynia
· Hormonally-mediated vestibulodynia
· Inflammatory vestibulodynia
The vestibule tissue is fundamentally different from the skin around it, developing from a different part of the embryo. This biological difference is crucial to understanding the causes of pain specifically in the vestibule. In this post, we will be reviewing hormonally mediated vestibulodynia, and in upcoming posts we will discuss neuroproliferative vestibulodynia as there are some interesting new research in the connection between neuroproliferative vestibulodynia and endometriosis.
Causes of Vestibulodynia
The reason why some individuals develop vestibulodynia while others do not, is still under investigation. However, a 2014 study suggests that there may be a genetic risk factor for developing vestibulodynia when taking anti-androgen medication.
Hormonally-mediated vestibulodynia can be caused by several factors, times in life or medications that alter hormones and result in a suboptimal state. This could be during periods of amenorrhea (lack of a period) in young adults, medications including combined oral contraceptive pills, aromatase inhibitors used in breast cancer, and other hormonal suppressive medications as well as acne medications (Accutane and Spironolactone). Periods in life that result in reduced hormones including breastfeeding (lactational amenorrhea) and perimenopause through menopause which we describe as GSM (genitourinary syndrome of menopause). The vestibule tissue is particularly sensitive to a lack of hormone signals, so for those with endometriosis, while your birth control may be helping your painful periods, it maybe causing you to have painful intercourse.
Symptoms of Vestibulodynia
Pain.
Individuals with vestibulodynia typically experience discomfort at the entrance of the vagina, known as the vestibule. The pain in the vestibule can be described in many ways. People with hormonally-mediated vestibulodynia may describe their discomfort as burning, stinging, or tearing.
Provoked vestibulodynia refers to vestibular pain that occurs with touch or pressure, while unprovoked pain occurs spontaneously. Sometimes, it can be challenging to distinguish provoked from unprovoked pain before all triggers are recognized, especially when they are seemingly simple things like sitting or wearing tight clothing.
People often feel discomfort any time there is contact or pressure on the vestibule. This includes during vaginal penetration (dyspareunia), tampon use, and speculum exams. Day-to-day activities that put pressure on the vestibule, such as wearing tight clothing, sitting for long periods, or wiping with toilet paper, can also cause discomfort.
Urinary.
Because this tissue also impacts the urethra, for some, the primary symptoms are urinary in nature. Urinary urgency, frequency, or UTI-like feelings without an infection are common and some will even receive a diagnosis of interstitial cystitis/painful bladder syndrome, also very common to see in those with endometriosis.
Pelvic Floor Tightness
It is believed that pelvic floor dysfunction may develop in people with vestibulodynia due to a subconscious guarding response against discomfort (remember the stove analogy). However, chronic tightening of the pelvic floor muscles can create more discomfort. The muscles can accumulate knots (trigger points) and become shortened and weak. The weakness is because the muscles are not functioning optimally, please do not go and do kegels!
Additional symptoms of pelvic floor dysfunction can include feeling tension, discomfort, and burning in the hips, legs, lower back, and vulva, especially the vestibule. One can also experience urinary symptoms like frequency, urgency, and leakage, as well as bowel symptoms like constipation or discomfort with bowel movements.
Diagnosis of Vestibulodynia
The first step towards diagnosing vestibulodynia is a thorough history of your story by a knowledgeable provider. Your story holds crucial clues to your diagnosis. People with hormonally-mediated vestibulodynia may have discomfort that developed later in life after any of the associated factors discussed above, including starting a medication, surgery, breastfeeding, or menopause.
Then there should be a very specific examination of the pelvis, vulva, and vagina. In patients with hormonally-mediated vestibulodynia, the vestibule usually appears very red and irritated (erythema), but also pale (mucosal pallor). The provider should manually examine the pelvic floor muscles to determine if there is excess tension in the muscles.
A process called a Q-tip test is essential for mapping discomfort in the vulva. The provider will gently press a cotton swab to each part of the vulva while the patient reports their degree of discomfort at each spot. It is important that the provider touch each region of the vestibule, all the way around the vaginal opening. The physical exam is extremely important prior to using dilators as this may cause more irritation because the cause (or one cause) of the muscle tension is the vestibule and needs attention before dilators come into treatment.
Some specialists will check labs including total testosterone, free testosterone, and SHBG (sex hormone binding globulin), and many with hormonally mediated vestibulodynia show altered levels; though you do not need labs to confirm this diagnosis.
Treatment of Vestibulodynia
Fortunately, in the case of hormonally-mediated vestibulodynia, the standard treatment has a very high success rate. If vestibulodynia developed after starting a medication that is known to affect hormone levels, then patients should stop taking that medication. Stopping the medication is often not enough to help the vestibule tissue heal quickly because hormone levels might stay low for a long time after taking birth control pills.
Providers should prescribe a topical hormone gel to apply directly to the vestibule to restore the hormone signals to the tissue. The standard is 0.01-0.03% estrogen and 0.1% testosterone gel. The hormone gel is usually made by a compounding pharmacy. Custom compounded medications are especially helpful if someone is sensitive to a medication’s base, the inactive ingredients, and needs a different base.
Patients typically use the gel 1 to 2 times daily and start to notice improvement in 6 to 12 weeks. Some patients stop using the hormone gel once the offending medication has been stopped for a while, but many women choose to stay on this therapy.
Support for Vestibulodynia Patients
There are many societies with interests in female sexual dysfunctions in addition to ISSWSH. The National Vulvodynia Association (NVA) is a US-based association founded by patient advocates that focuses specifically on vulvodynia. They provide some educational materials for the public and fund research of vulvodynia. Tight Lipped is also a patient facing, grass-roots, advocacy group helping to change medical education around this condition.
There are many online support groups and communities of patients who support each other on social media. To find fellow patients locally, ask a provider if they know of another patient seeking community or any local groups to join.
Conclusion
Understanding and effectively managing vestibulodynia necessitates a comprehensive understanding of its causes, symptoms, and treatments. The information in this article seeks to bridge the gap between scientific research and the general public, providing evidence-based insights into this prevalent health concern. If you are experiencing symptoms of vestibulodynia, seek advice from a healthcare professional. There is a broad range of treatment options available, and you are not alone in your journey towards healing and managing this condition.
While this article provides a comprehensive overview of vestibulodynia, it is essential to remember that each individual’s experience with the condition can vary. Therefore, it’s crucial to consult with healthcare professionals and consider personal circumstances when making decisions regarding management and treatment.
Find a specialist: www.isswsh.org
Additional reading:
- Managing Endometriosis: What You Need to Know
- Understanding the Relationship between Sex and Endometriosis
- Finding an Endometriosis Specialist: Your Guide to Effective Treatment
References:
- Rubin, R. W. C. (2022). Hormonally mediated vestibulodynia. Accessed from https://www.prosayla.com/articles/hormonally-mediated-vestibulodynia
- Burrows LJ, Goldstein AT. The treatment of vestibulodynia with topical estradiol and testosterone. Sex Med. 2013 Aug;1(1):30-3. doi: 10.1002/sm2.4. PMID: 25356284; PMCID: PMC4184715.
Endometriosis Affects Sexual Function: What You Need to Know
Many people know endometriosis as a “menstrual” disease or associate it with painful periods and/or infertility; however, endometriosis impacts many aspects of one’s life, including sexual function and intimacy.. This article aims to shed light on the complex interplay between endometriosis and sexual dysfunction, highlighting the critical points from recent scientific findings and providing an empathetic and informative perspective for those affected by the condition.
Impact on Sexuality
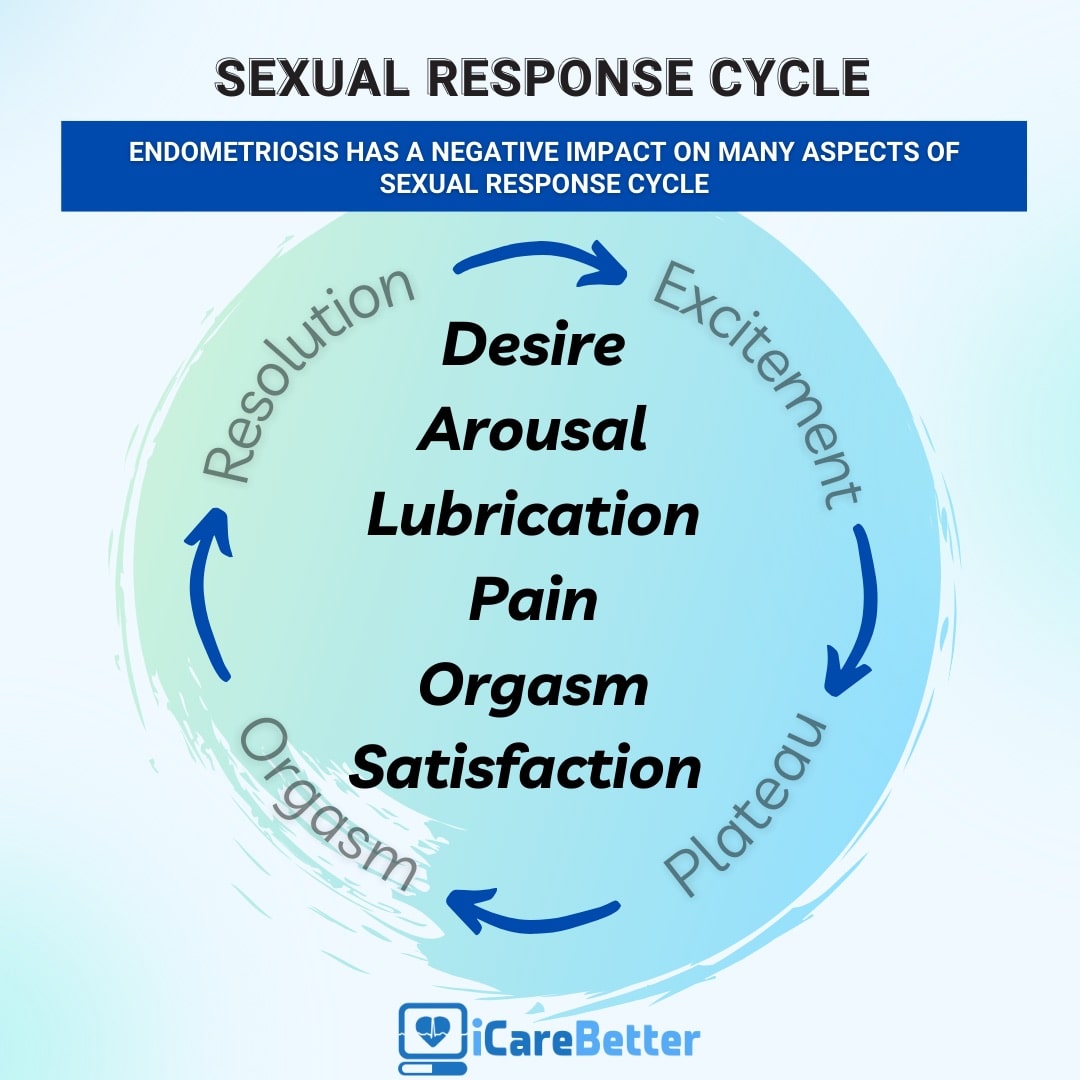
Endometriosis is notorious for causing severe pelvic pain, which is often exacerbated during menstruation. However, its effect extends beyond physical discomfort, with a significant impact on a woman’s sexual function. The correlation between endometriosis and sexual dysfunction is a compelling topic for scientific research, as it profoundly affects the quality of life of those living with this condition. One of the primary clinical manifestations of endometriosis is dyspareunia. What is important to know is that the lesions may directly cause deep dyspareunia (pain with deep thrusting), though the lesions as well as ‘treatments’ for endometriosis may also impact sexual functioning and leads to a decrease in sexual desire or arousal, resulting in a cycle of distress and avoidance of sexual intimacy.
Beyond Pain: Emotional and Psychological Effects
The effects of endometriosis on sexual function aren’t limited to physical symptoms. The condition can also trigger feelings of anxiety, distress, and guilt, affecting a woman’s self-esteem and overall mental health. Furthermore, the chronic nature of endometriosis and its association with infertility can impose additional psychological stress, further exacerbating sexual dysfunction. Over time, one may anticipate the pain, or have anxiety about what the sexual experience may be like, therefore causing reduced desire and arousal, or resulting in avoidance of sex or intimacy altogether.
Understanding the Prevalence of Sexual Dysfunction in Endometriosis
A significant proportion of women living with endometriosis experience some form of sexual dysfunction. However, the severity and type of dysfunction can vary greatly, influenced by factors such as the type and extent of endometriosis, individual pain tolerance, and psychological well being.
Several scientific studies have delved into the intricate relationship between endometriosis and sexual dysfunction. A systematic review of nine studies conducted between 2000 and 2016 found that around two-thirds of women with endometriosis experienced some form of sexual dysfunction. These dysfunctions extended beyond deep dyspareunia, encompassing issues like hypoactive sexual desire, arousal problems, and orgasmic disorders.
The Role of Deep Infiltrating Endometriosis (DIE)
Deep Infiltrating Endometriosis (DIE), a severe form of the disease, is often associated with a higher prevalence of sexual dysfunction. Studies focusing on patients with DIE have found a significant impairment in various aspects of sexual functioning, including satisfaction, frequency of intercourse, and orgasm.
The Multidimensional Nature of Human Sexuality
Human sexuality is a complex phenomenon, influenced by a multitude of physical, psychological, and relational factors. As such, sexual dysfunction in women with endometriosis is not solely a result of physical pain but can also be shaped by the individual’s mental health and the quality of their intimate relationships.
Psychological distress, often associated with chronic pelvic pain, can significantly affect sexual functioning. Women living with endometriosis often experience anxiety and depression, which can act as powerful inhibitors of the sexual response cycle.
The quality of intimate relationships plays a crucial role in shaping sexual function. Marital satisfaction, perceived partner support, and the degree of intimacy can significantly influence the sexual experiences of women living with endometriosis.
Addressing Sexual Dysfunction in Endometriosis: A Multidisciplinary Approach
Given the multifaceted nature of sexual dysfunction in endometriosis, a comprehensive and multidisciplinary approach is crucial for effective management. Such an approach extends beyond medical treatment for painful symptoms, encompassing psychological support and psychosexual therapy.
Your general gynecologist or endometriosis specialist may not necessarily be the person to also address your sexual dysfunction. This is a major area in which many providers are not trained in. ISSWSH, which stands for the International Society for the Study of Women’s Sexual Health, is an international, multidisciplinary organization that focuses on sexual health. Often, these people are the ones you want to see in regards to your sexual dysfunction. They include urologists, gynecologists, mental health professionals, physical therapists, nurse practitioners and more.
Psychological support is crucial in managing the mental health challenges associated with endometriosis. Therapists and psychologists can provide coping strategies for anxiety and depression, addressing feelings of guilt and distress associated with sexual dysfunction.
Empowerment Through Knowledge
Education and awareness are powerful tools in managing endometriosis and its impact on sexual function. By understanding the nature of the disease and its potential effects on their sexual health, women can seek appropriate help and take proactive steps towards improving their quality of life.
Endometriosis and its impact on sexual function is a complex issue, requiring a multifaceted, compassionate, and patient-centric approach. By acknowledging the physical, psychological, and relational aspects of sexual dysfunction, healthcare professionals can provide holistic support to those living with endometriosis, empowering them to navigate the challenges of this chronic condition and enhancing their overall quality of life.
Related reading:
- Endometriosis Pain after Orgasm: What You Need to Know
- Understanding the Relationship between Sex and Endometriosis
- What You Need to Know About Endometriosis and Intimacy
References:Barbara, G., Facchin, F., Buggio, L., Somigliana, E., Berlanda, N., Kustermann, A., & Vercellini, P. (2017). What Is Known and Unknown About the Association Between Endometriosis and Sexual Functioning: A Systematic Review of the Literature. Reprod Sci, 24(12), 1566-1576. https://doi.org/10.1177/1933719117707054

