Endometriosis Diet: Low FODMAP, a Comprehensive Guide
Table of contents
- Understanding the Low FODMAP Endometriosis Diet
- What are FODMAPs?
- Exploring the Impacts of FODMAPs
- Who Should Follow a Low FODMAP Endometriosis Diet?
- The Purpose of a Low FODMAP Endometriosis Diet
- How to Follow a Low FODMAP Diet
- The Effectiveness of Low FODMAP Endometriosis Diet Combined with Other Therapies
The Low FODMAP Diet, a revolutionary approach for managing symptoms associated with Irritable Bowel Syndrome (IBS), has gained substantial recognition and popularity in recent years. Developed by researchers at Monash University, this diet has offered hope to many individuals suffering from IBS, a common gastrointestinal disorder that affects the digestive system. So how can it help those with endometriosis? This article will focus on the diet itself, but a relatively recent systematic review of dietary approaches and endometriosis showed that the low FODMAP diet was most helpful in managing symptoms in those with endometriosis that complained of gastrointestinal symptoms and had good follow through in individuals who tried it.
Understanding the Low FODMAP Endometriosis Diet
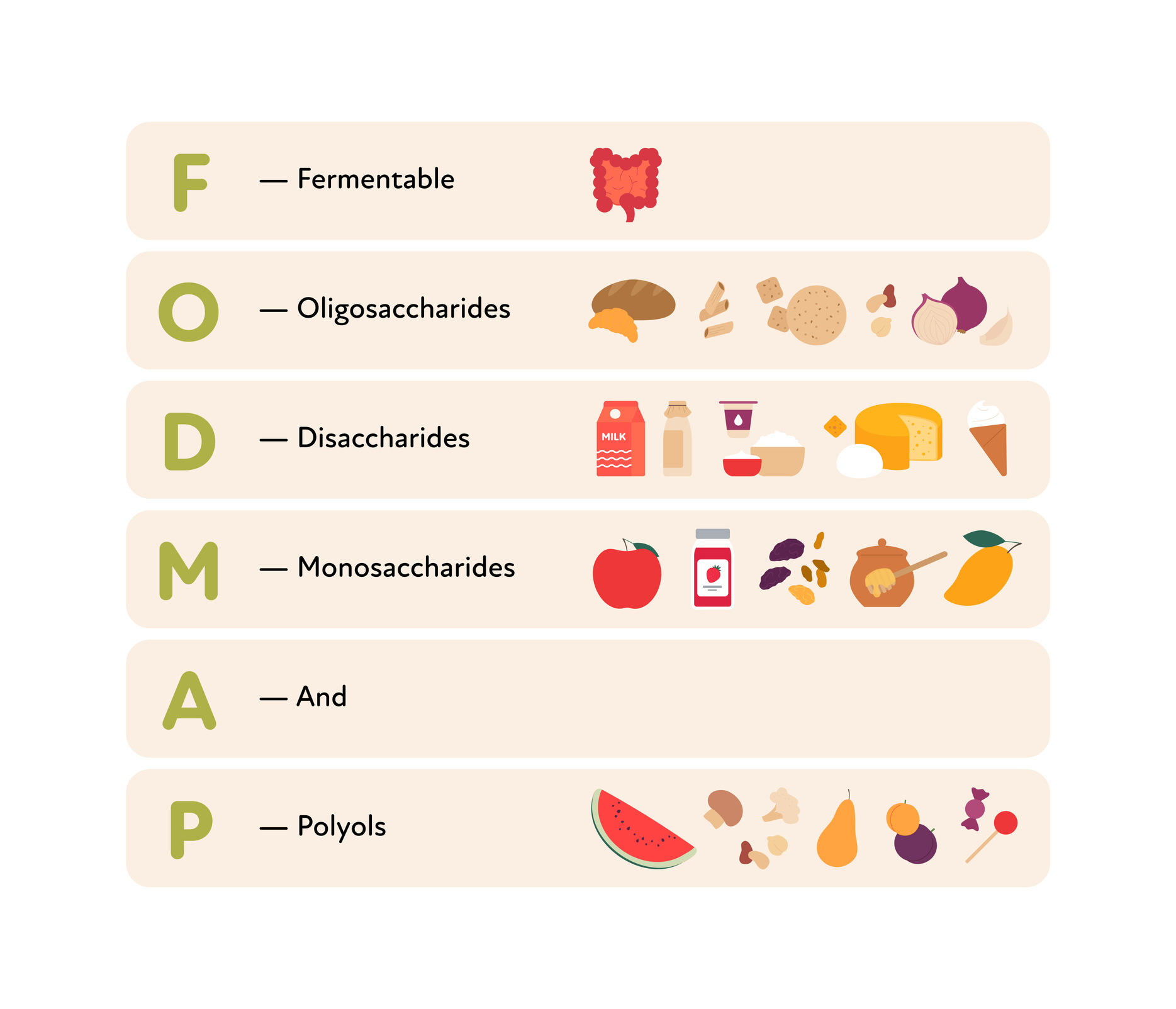
FODMAP is an acronym that stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. These are certain types of carbohydrates that are either poorly absorbed or not absorbed at all in your intestines and can trigger symptoms in individuals with IBS.
What are FODMAPs?
FODMAPs are naturally occurring sugars found in a wide range of foods and food additives. When consumed, these sugars move slowly through the small intestine, attracting water. As they reach the large intestine, they are fermented by gut bacteria, resulting in gas production. This extra gas and water cause the intestinal wall to stretch and expand, which can cause pain and discomfort, especially in people with IBS.
Types of FODMAPs
Here are the different types of FODMAPs and examples of foods where they can be found:
- Oligosaccharides: These include Fructans and Galacto-Oligosaccharides (GOS) found in foods such as wheat, rye, onions, garlic, and legumes.
- Disaccharides: Lactose is a disaccharide found in dairy products like milk, soft cheeses, and yogurts.
- Monosaccharides: Fructose is an example, found in honey, apples, and high fructose corn syrups.
- Polyols: These include Sorbitol and Mannitol, found in some fruits, vegetables, and used as artificial sweeteners.
Exploring the Impacts of FODMAPs
When FODMAPs are consumed, they move slowly through the small intestine, attracting water. As they reach the large intestine, gut bacteria use these FODMAPs as a fuel source, fermenting them and producing gas. This process is normal but can cause problems in people with IBS due to issues with motility (the speed at which contents move through the intestines) or a highly sensitive gut wall.
FODMAPs are found in a variety of foods, such as fruits, vegetables, bread, cereals, nuts, and legumes. It’s impossible to guess the FODMAP content of a food without careful laboratory analysis. Monash University has developed a mobile phone app, the Monash University FODMAP Diet App, which uses a simple traffic light system to indicate whether foods are low, moderate, or high in FODMAPs.
High FODMAP Foods and Low FODMAP Alternatives
Here’s a table showing some high FODMAP foods and their low FODMAP alternatives:
| High FODMAP Foods | Low FODMAP Alternatives |
|---|---|
| Vegetables: Artichoke, Asparagus, Cauliflower, Garlic, Green Peas, Mushrooms, Onion, Sugar Snap Peas | Aubergine/Eggplant, Beans (Green), Bok Choy, Green Capsicum (Bell Pepper), Carrot, Cucumber, Lettuce, Potato, Zucchini |
| Fruits: Apples, Apple Juice, Cherries, Dried Fruit, Mango, Nectarines, Peaches, Pears, Plums, Watermelon | Cantaloupe, Kiwi Fruit (Green), Mandarin, Orange, Pineapple |
| Dairy & alternatives: Cow’s Milk, Custard, Evaporated Milk, Ice Cream, Soy Milk (Made from Whole Soybeans), Sweetened Condensed Milk, Yoghurt | Almond Milk, Brie/Camembert Cheese, Feta Cheese, Hard Cheeses, Lactose-Free Milk, Soy Milk (Made from Soy Protein) |
| Protein sources: Most Legumes/Pulses, Some Marinated Meats/Poultry/Seafood, Some Processed Meats | Eggs, Firm Tofu, Plain Cooked Meats/Poultry/Seafood, Tempeh |
| Breads & Cereals: Wheat/Rye/Barley Based Breads, Breakfast Cereals, Biscuits and Snack Products | Corn Flakes, Oats, Quinoa Flakes, Quinoa/Rice/Corn Pasta, Rice Cakes (Plain), Sourdough Spelt Bread, Wheat/Rye/Barley Free Breads |
| Sugars, Sweeteners & Confectionery: High Fructose Corn Syrup, Honey, Sugar Free Confectionery | Dark Chocolate, Maple Syrup, Rice Malt Syrup, Table Sugar |
| Nuts & Seeds: Cashews, Pistachios | Macadamias, Peanuts, Pumpkin Seeds/Pepitas, Walnuts |
Who Should Follow a Low FODMAP Endometriosis Diet?
The Low FODMAP diet is specifically designed for individuals with medically diagnosed IBS. It is not recommended for people to self-diagnose and start this diet without the proper medical guidance. There are many conditions with symptoms similar to IBS, such as coeliac disease, inflammatory bowel disease, endometriosis, and bowel cancer. Therefore, it is crucial to get a clear diagnosis of IBS from a medical doctor before starting this diet.
The Purpose of a Low FODMAP Endometriosis Diet
The Low FODMAP diet is essentially a three-step diet used to manage symptoms of IBS, which can include abdominal pain, bloating, wind (farting) and changes in bowel habit (diarrhea, constipation, or both). The main goals of this diet are:
- Understand which foods and FODMAPs you tolerate and which ones trigger your IBS symptoms.
- Determine whether your IBS symptoms are sensitive to FODMAPs.
- Implement a less restrictive, more nutritionally balanced diet for the long term that only restricts foods that trigger your IBS symptoms.
How to Follow a Low FODMAP Diet
The Low FODMAP diet is a three-step diet, typically encompassing the following steps:
Step 1: Follow the Monash University Low FODMAP Diet by replacing high FODMAP foods in your diet with low FODMAP alternatives. This step usually lasts for 2-6 weeks.
Step 2: Continue your low FODMAP diet and complete a series of ‘FODMAP challenges’ to identify which FODMAPs you tolerate and which trigger symptoms.
Step 3: Relax dietary restrictions as much as possible, reintroduce well-tolerated foods and FODMAPs to your diet, and establish a ‘personalized FODMAP diet’ for the long term.
It is recommended to follow a Low FODMAP diet under the guidance of a dietitian who has specialty skills in managing IBS and using a FODMAP diet. Monash University’s FODMAP Dietitian Directory can be a useful resource to find such dietitians.
The Effectiveness of Low FODMAP Endometriosis Diet Combined with Other Therapies
The Low FODMAP diet has shown promising results in managing IBS symptoms. However, in some cases, the diet alone may not be sufficient, and other therapies may be required. One such therapy that has shown positive results in treating IBS is Gut Focused Hypnotherapy.
Understanding Gut Focused Hypnotherapy
Gut Focused Hypnotherapy is a type of treatment where patients are asked to visualize their gut as a perfectly slimy set of passages where all the digesting food slips through smoothly. This treatment has been proven to reduce symptoms of IBS by 70% in patients.
Combining Low FODMAP Diet and Gut Focused Hypnotherapy
Researchers at Monash University conducted a study combining the Low FODMAP diet and Gut Focused Hypnotherapy. The study resulted in a significant improvement in the overall and individual gut symptoms of the participants by the end of the six-week study.
Comparing the Low FODMAP Diet with Other IBS Diets
When comparing the Low FODMAP diet with other diets for IBS, it has been noted that the Low FODMAP diet seems to be superior to a gluten-free diet for patients with non-celiac gluten sensitivity. This is likely due to the comprehensive approach of the Low FODMAP diet, which considers all types of carbohydrates that could potentially trigger IBS symptoms.
The Low FODMAP diet has been shown to be effective in managing IBS symptoms, with studies showing improvement in pain, discomfort, bloating, and other GI symptoms. However, it is essential to follow this diet under the guidance of a trained dietitian and in conjunction with other therapies if necessary. As with any diet, the Low FODMAP diet should be personalized to fit the individual’s needs and tolerance levels.
If you are suffering from IBS-like symptoms and you have endometriosis or are just starting in your journey for a diagnosis, it may be worth seeking out professional guidance to see if the low FODMAP diet may be helpful. As a reminder – it is not going to treat your endometriosis and is used primarily for symptom management. It does not replace seeking out the root cause of both endometriosis and your GI dysfunction.
Disclaimer: This article is intended for informational purposes only and is not a substitute for professional medical advice. Always consult your doctor or a dietitian before making any changes to your diet.
References:
- https://www.monashfodmap.com/about-fodmap-and-ibs/
- https://www.monashfodmap.com/ibs-central/i-have-ibs/starting-the-low-fodmap-diet/
Molina-Infante, J., Serra, J., Fernandez-Banares, F., & Mearin, F. (2016). The low-FODMAP diet for irritable bowel syndrome: Lights and shadows. Gastroenterol Hepatol, 39(2), 55-65. https://doi.org/10.1016/j.gastrohep.2015.07.009

