
Endometriosis-Related Infertility – Minimal Causes
Endometriosis, a common gynecological condition, has been frequently associated with infertility. However, the question remains: can minimal endometriosis cause infertility? This comprehensive article aims to delve into the connection between endometriosis, particularly in its minimal stage, and fertility issues.
Table of contents
Defining Endometriosis
Endometriosis is a medical condition characterized by the growth of endometrium-like tissues outside the uterus. These tissues can adhere to various pelvic structures like the ovaries, fallopian tubes, and even the intestines and bladder, causing irritation, inflammation, and scar tissue formation.
Stages of Endometriosis
Endometriosis is categorized into four stages:
- Stage I (Minimal): Small endometriotic implants with no scar tissue.
- Stage II (Mild): More extensive implants, involving less than 2 inches of the abdomen, without scar tissue.
- Stage III (Moderate): Severe endometriosis with deep implants and possible formation of endometriotic cysts or ‘chocolate cysts’ in the ovaries.
- Stage IV (Severe): Numerous endometriotic implants, possibly large endometriotic cysts in the ovaries, and scar tissue formation around the reproductive organs.
Read More: Understanding How Endometriosis Can Cause
The Connection Between Endometriosis and Infertility
It’s estimated that 30% to 50% of women with endometriosis may experience infertility. Even in cases of minimal or mild endometriosis, the disease may still impact fertility in numerous ways, including:
- Distorted pelvic anatomy due to scar tissue and adhesions
- Inflammatory response causing a hostile environment for eggs, sperm, and embryos
- Altered immune system functionality
- Changes in the hormonal environment affecting egg quality and embryo implantation
However, it’s essential to note that endometriosis does not necessarily equate to infertility. Many women with endometriosis, even in severe stages, can conceive naturally or with fertility treatments.
Exploring the Question: Can Minimal Endometriosis Cause Infertility?
The impact of minimal endometriosis on fertility is a contentious subject. The disease, even at its earliest stage, can cause inflammation and subtle changes in the pelvic environment, potentially affecting fertility. However, many women with minimal endometriosis conceive without issues, leading some researchers to suspect that other factors, possibly genetic or immunological, might be at play in cases of endometriosis-associated infertility.
Diagnosing Endometriosis
Diagnosing endometriosis can be challenging, as many women with infertility migh experience no symptoms. The gold standard for diagnosis is a surgical procedure known as laparoscopy, allowing the doctor to visually inspect the pelvic organs for endometriotic lesions and scar tissue, and take samples for histopathology.
Read More: Life After Endometriosis Surgery: A Comprehensive Guide
Evaluating Fertility
Before initiating any fertility treatment, a comprehensive fertility evaluation is recommended. This includes hormonal and blood tests, an assessment of ovarian reserve, a sperm analysis for the male partner, and possibly a laparoscopy to confirm the presence and extent of endometriosis.
Read More: Pelvic Floor Physical Therapy: What you Need to Know
Treatment Options for Endometriosis-Related Infertility
The treatment approach for endometriosis-related infertility is multifaceted, depending on the stage of endometriosis, the woman’s age, and the presence of other fertility factors.
Surgical Treatment
For women with Stage I or II endometriosis, surgical removal of endometriotic tissue may improve pregnancy rates. However, for women aged 35 or older, other fertility treatments might be recommended in addition to surgery.
Medical Treatment
Medical treatments aim to suppress endometriosis growth by reducing estrogen levels. However, these treatments, including hormonal contraceptives and Gonadotropin-Releasing Hormone (GnRH) agonists, prevent pregnancy during use.
Assisted Reproductive Technology (ART)
In cases where pregnancy does not occur naturally or following surgery, ART methods such as Intrauterine Insemination (IUI) or In Vitro Fertilization (IVF) may be recommended. The success rates of these treatments vary depending on the woman’s age, ovarian reserve, and specific fertility issues.
Conclusion: Can Minimal Endometriosis Cause Infertility?
While minimal endometriosis can potentially affect fertility, it does not guarantee infertility. A comprehensive evaluation and personalized treatment plan can help women with endometriosis, even at minimal stages, to conceive successfully. However, further research is needed to fully understand the complex relationship between endometriosis and fertility.
References:
https://www.uptodate.com/contents/endometriosis-treatment-of-infertility-in-females
Understanding How Endometriosis Can Cause Bowel Problems
Endometriosis, a common health concern among women, can manifest itself in various ways, one of them being bowel problems. But how exactly can endometriosis cause bowel problems? This article will take you through the intricate connection between endometriosis and bowel problems, the symptoms to look out for, diagnostic procedures, and potential treatments.
Table of contents
What is Endometriosis?
Endometriosis is a health condition where the tissue similar to the type that lines the uterus, known as the endometrium, grows outside the uterus. This condition predominantly affects the reproductive organs such as the ovaries, fallopian tubes, and the external part of the uterus. However, it can also extend to other parts of the body including the bowels, rectum, and other pelvic organs.
Understanding Bowel Endometriosis
Bowel endometriosis is a form of endometriosis that affects the gastrointestinal tract, specifically the bowels. It can appear in two forms: superficial (on the surface of the bowel) and deep (penetrating the bowel wall).
Read More: Understanding Bowel Endometriosis
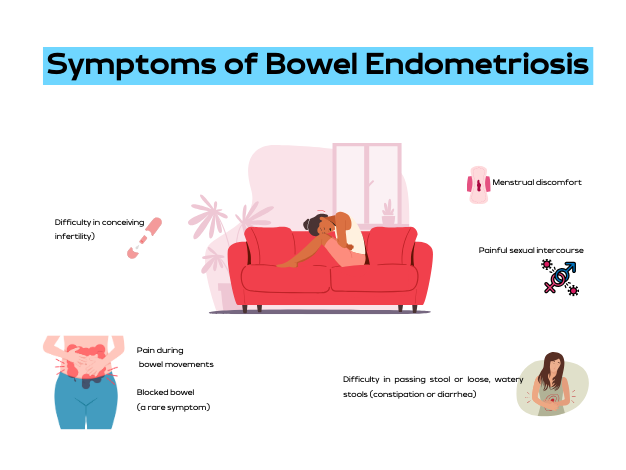
Symptoms of Bowel Endometriosis
The symptoms of bowel endometriosis can vary widely depending on the location of the lesion, its size, and how deep it is in the bowel wall. Some women may experience no symptoms. However, common symptoms include:
- Difficulty in passing stool or loose, watery stools (constipation or diarrhea)
- Pain during bowel movements
- Menstrual discomfort
- Painful sexual intercourse
- Difficulty in conceiving (infertility)
- Blocked bowel (a rare symptom)
It is noteworthy that these symptoms can often mimic other conditions like irritable bowel syndrome (IBS), but the two conditions are distinct. One distinguishing factor is that with bowel endometriosis, symptoms often worsen before and during the menstrual period.
Read More: Endometriosis and Painful Intercourse: Is it Really Just Endometriosis?
Causes of Bowel Endometriosis
The exact cause of bowel endometriosis is still under study. However, several factors have been linked to its occurrence. These include genetic predisposition, inflammation, and levels of estrogen, a female sex hormone.
The Prevalence of Endometriosis
Endometriosis affects approximately 10%-12% of women of childbearing age. The condition is often diagnosed in women who are in their 30s, although it can occur at any age.
Diagnosing Bowel Endometriosis
The diagnosis of bowel endometriosis starts with the doctor asking about your symptoms and medical history, followed by a physical examination of your pelvic area. The doctor may also recommend imaging tests to get more information on the location and size of any cysts or tissue damage related to endometriosis. These tests include:
- Transvaginal or transrectal ultrasound: This procedure involves the insertion of a wand-like device into your vagina or rectum. This device releases sound waves that create images of your organs.
- Magnetic resonance imaging (MRI): An MRI test provides detailed images of your organs and tissues using a magnetic field and radio waves.
- Laparoscopy: This surgical procedure involves making a small incision near your belly button and inserting a thin viewing tool called a laparoscope.
- Barium enema: This type of X-ray is used to see changes or defects in your large intestine (colon).
- Colonoscopy: They pass a tube with a camera on its tip through the anus into the colon to directly visualize the wall and take samples from inside the colon.
Read More: Colon Chronicles: Delving into Bowel Endometriosis
Treating Bowel Endometriosis
The treatment plan for bowel endometriosis will be personalized, taking into account your symptoms, medical history, age, and reproductive plans. Treatments can include:
- Surgery: The aim of surgery is to remove as many lesions as possible while preserving your organs and overall health.
- Hormone treatments: These medications control estrogen levels which can worsen the symptoms of bowel endometriosis.
- Counseling: Given the ongoing nature of bowel endometriosis and its impact on both physical and mental health, counseling may be recommended to provide emotional support.
The Prognosis for Bowel Endometriosis
There is currently no cure for endometriosis. However, treatments like surgery and hormone therapy can help manage the symptoms. It is also important to note that symptoms could return if treatment is halted, or they could recur on their own, especially in cases with deep lesions.
Endometriosis is a complex condition that can cause bowel problems and other health issues. If you suspect you have endometriosis and are experiencing bowel problems, it’s important to consult with a healthcare provider. Early diagnosis and treatment can help manage symptoms and improve your quality of life.
References:
https://www.webmd.com/women/endometriosis/bowel-endometriosis
https://www.endometriosis-uk.org/endometriosis-and-bowel
https://www.endofound.org/gastrointestinal-distress
ENDOMETRIOSIS AND CONSTIPATION

Anti-Mullerian Hormone & Endometriosis – What’s The Connection?
Endometriosis has been associated with a marker called Antimullerian hormone (AMH), which is a pivotal marker of ovarian reserve, and is commonly measured in women with endometriosis specifically in relation to fertility. There is debate among the community that your AMH level is what it is and it cannot change. I would challenge this notion though as I have seen people with endometriosis have significant increases after proper excision surgery, which is a point of debate. Recently, I had another patient send me lab work that demonstrated what some may call a low AMH, has confirmed endometriosis, but likely a surgery that was incomplete and is continuing to suffer ongoing symptoms. Though I have seen this change in my patients, I recognize this is only a small fraction of the people suffering, so it was time to review what the research says. This article aims to provide a review of the various studies conducted on this critical subject, exploring how endometriosis and AMH interact, the effect of surgical intervention on AMH levels, and the subsequent impact on fertility.
Table of contents
The Antimullerian Hormone (AMH): A Brief Overview
AMH, a hormone playing diverse roles during embryonic development and puberty, is produced by ovarian follicles smaller than 8 mm, hence linking ovarian reserve to AMH levels in the blood. The normal range for AMH hovers between 1 and 4 ng/mL. However, women’s AMH levels greatly vary based on factors like age, ethnic background, lifestyle, and genetics. Additionally, someone at the low end of range may still suffer problems despite them being “in range.”
AMH Testing in Reproductive Health
AMH testing is a crucial tool for evaluating female fertility. It can assist in:
- Assisting with understanding the prognosis of a woman’s response to assisted reproduction techniques (ART) such as in vitro fertilization (IVF)
- Confirming other markers of menopause
- Providing a more comprehensive evaluation when certain conditions are confirmed or suspected such as polycystic ovarian syndrome (PCOS), premature ovarian failure, and endometriosis
Endometriosis and AMH Levels
Endometriosis is a common culprit behind infertility, affecting nearly half of the women suffering from this ailment. This infertility arises from various factors, including inflammation in the reproductive tract, scar tissue-induced decreased blood supply to the ovaries, and pelvic anatomical distortions. Research reveals a significant correlation between endometriosis and lower than average AMH levels.
Some argue that surgical intervention of endometriosis often leads to a reduction in AMH levels, though many of us in the community may argue that this is a more nuanced topic and this highly depends on the skill of the surgeon, something that is often overlooked in endometriosis research. Various studies have attempted to decipher the impact of endometriosis surgery on AMH levels and fertility outcomes. A retrospective study conducted in 2016 found that preoperative AMH levels did not influence pregnancy rates after surgery. This is consistent with the literature we have on surgical impact, and thus the need for better research in the future. In my experience, this is the opposite of what I have seen, as many of us have seen when people get to the right surgeon.
Laparoscopic Cystectomy on AMH Levels
Laparoscopic ovarian cystectomy, a common surgical procedure to treat endometriomas, has been associated with decreased ovarian reserve. A study in 2019 demonstrated significantly lower AMH levels in women who underwent laparoscopic endometrioma cystectomy, especially in cases with bilateral cysts larger than 7 cm and stage 4 endometriosis.
Considerations: I want to highlight that we do not know the skill of the surgeon, but we do know that the skill of the surgeon matters. That being said, large endometriomas can often overtake ovarian tissue which is what happened to Christina. Hear her story here. This is why it is extremely important to find a knowledgeable surgeon that you feel comfortable with. If you need help finding a surgeon, you can start here.
Laparoscopic Endometriosis Surgery on AMH Levels
A literature review and meta-analysis of 19 studies conducted between 2010 and 2019 on the impact of laparoscopic endometriosis surgery on AMH levels post-surgery revealed a decline in AMH levels, extending beyond six months post-surgery. This decline was more pronounced in cases where surgery was performed on both sides of the body, compared to a single side.
Again, I would argue that we consider the quality of the research and the skill of the surgeon. Remember, ablation is different from excision and this may be another factor that is skewing results. I repeat this because, like many of us in the community, this is not our experience, thus I often read research with these things in mind. If many others in the community are also seeing this, there must be more to consider than what is presented. The bottom line is that we need better research.
AMH Levels Post-Surgery for Endometrioma
Several studies have observed that laparoscopic ovarian cystectomy results in a significant and progressive decrease in AMH levels post-surgery. However, other studies have noted that this decrease may only be temporary, with levels potentially returning to normal within a year. Another factor to consider is when the AMH was measured post-surgery and what other factors may have impacted the levels!
Certain studies have observed a temporary decrease in AMH levels following endometrioma ablation. However, this decrease did not persist beyond six months in most cases, suggesting a potential recovery of ovarian reserves.
Several studies have compared the decrease in AMH levels following ovarian cystectomy and endometrioma vaporization. The general consensus suggests a higher postoperative decline in AMH levels following cystectomy compared to vaporization, particularly in bilateral endometrioma cases.
This caught my attention and highlights my thoughts on how the surgery (excision) is being performed as to not compromise ovarian tissue. Using ablation, which is what the CO2 laser is referring to, may not compromise the ovarian tissue, but it also may not treat the disease. Paul Tyan, MD discusses this complex topic in our interview which you can find here.
The combined technique, involving partial cystectomy and ablation, has been shown to have less detrimental effects on the ovary, resulting in a lesser decline in AMH levels post-surgery.
The role of endometriosis surgery in improving pregnancy rates remains a topic of debate. Some studies suggest that surgery might improve the success rates of fertility treatment, while others highlight the risk of ovarian damage due to surgical intervention.
In conclusion, the Antimullerian hormone is a vital marker for assessing the impact of endometriosis and its surgical intervention on ovarian reserve and fertility. Understanding the complex relationship between AMH levels, endometriosis, and surgical intervention along with identifying gaps in the research can help medical professionals devise more effective treatment strategies, improve the quality of research studies which ultimately improves patient outcomes.
IRelated Reading:
- Does Endometriosis Cause Infertility? Covering the Basics
- Endometriosis and Pregnancy: Natural, Medical, & Surgical Options
References:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6603105/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7865255/
- https://drseckin.com/endometriosis-surgery-and-amh-levels/
Endometriosis and Inflammatory Bowel Disease: Distinguishing the Differences
Exploring the complex world of health and medical conditions can sometimes feel like navigating through a labyrinth. The similarities between certain conditions often blur the lines, making it challenging for individuals and even healthcare professionals to differentiate between them. This is notably true in the case of endometriosis and inflammatory bowel disease (IBD), two disorders that share several overlapping symptoms and characteristics. We’ve recently been discussing endometriosis and the bowel, this article aims to shed light on these conditions, highlighting the differences, similarities, and the challenges faced in their diagnosis.
Table of contents
Symptoms of Endometriosis
The signs and symptoms of endometriosis can vary greatly, making it a complex disease to diagnose. Some of the most common symptoms include dysmenorrhea (painful periods), dyspareunia (painful intercourse), chronic pelvic pain, and gastrointestinal symptoms like diarrhea, constipation, and abdominal pain. Because endometriosis symptoms often overlap with GI symptoms, getting a diagnosis in general can be tricky, but especially if it may be impacting the bowels which is estimated in about 5-12% of cases, whereas approximately 90% of those with endometriosis suffer from gastrointestinal symptoms. In many cases, these symptoms can be mistaken for other conditions, leading to delays in diagnosis.
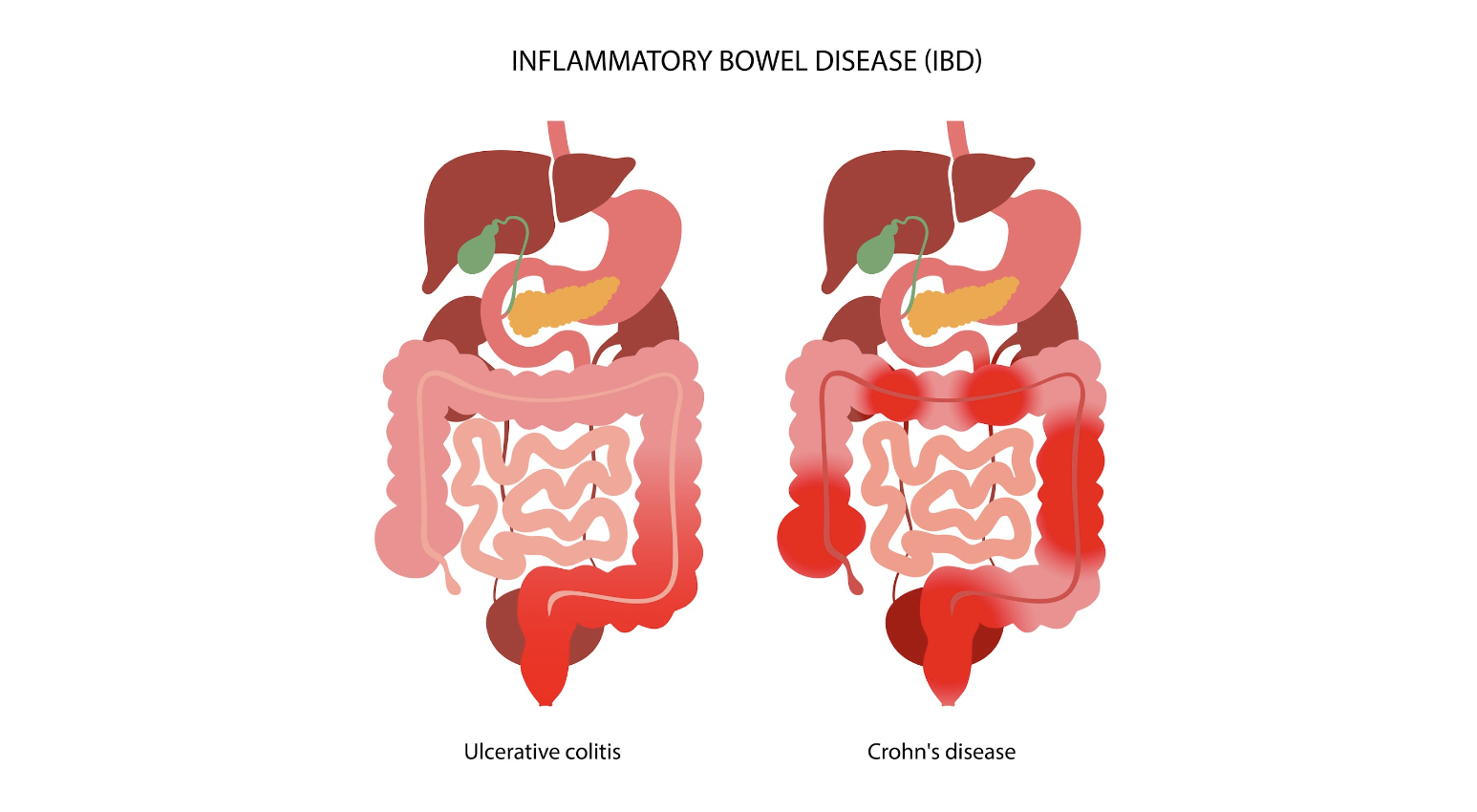
Inflammatory Bowel Disease: An Overview
Inflammatory bowel disease (IBD) is an umbrella term that encompasses two chronic autoimmune disorders: ulcerative colitis (UC) and Crohn’s disease (CD). These conditions are characterized by the chronic inflammation of the gastrointestinal tract, which can lead to a wide range of symptoms, including abdominal pain, diarrhea, weight loss, and fatigue.
The prevalence of IBD is highest in Europe, with reported cases reaching up to 505 per 100,000 for UC in Norway and 322 per 100,000 for CD in Italy. Like endometriosis, IBD can significantly impact an individual’s quality of life, necessitating long-term management strategies to control symptoms and prevent complications.
The Overlap: Endometriosis and IBD
Interestingly, endometriosis and IBD share several common traits, including immune dysregulation and overlapping clinical manifestations like abdominal pain and bowel-related symptoms. This overlap often poses a significant diagnostic challenge, as endometriosis can mimic IBD or vice versa, leading to delays or indeterminate diagnosis.
In fact, endometriosis has often been termed as having “IBD-like” features due to the similarities in symptoms and underlying pathophysiology. This has led to substantial interest in the potential link between these conditions, with several studies investigating the co-occurrence of endometriosis and IBD.
Investigating the Link: Endometriosis and IBD
To understand the potential link between endometriosis and IBD, numerous studies have been conducted, ranging from case reports and clinical series to epidemiological research. These studies have reported varying results, further highlighting the complexity of these conditions and the challenges associated with their diagnosis and management.
Case Reports and Clinical Series
Many case reports have been published that highlight the diagnostic challenges associated with endometriosis and IBD. For instance, several cases have been reported where an initial diagnosis of CD was later revised to intestinal endometriosis upon histopathological examination. Similarly, other case reports have documented instances where an initial diagnosis of UC was later confirmed to be appendiceal endometriosis.
Conversely, there have also been cases where an initial diagnosis of endometriosis was later revised to be CD upon histopathological examination. Additionally, several case reports have documented instances where both CD and endometriosis were diagnosed in the same patient.
Epidemiological Studies
In addition to case reports and clinical series, several epidemiological studies have investigated the co-occurrence of endometriosis and IBD. One such study, a nationwide Danish cohort study, reported a 50% increase in the risk of IBD in women with endometriosis compared to the general population. This increased risk persisted even more than 20 years after a diagnosis of endometriosis, suggesting a genuine association between the two conditions..
Another study, a retrospective cross-sectional study conducted in Israel, found that 2.5% of patients with endometriosis also had a diagnosis of IBD, compared to 1% in the general population. A recent Italian case-control study found that among 148 women with endometriosis, five had IBD, although this did not reach statistical significance.
The Challenge of Temporality
One of the critical aspects of evaluating the association between endometriosis and IBD is the issue of temporality, or the order in which the conditions are diagnosed. Many studies do not provide information on the temporal sequence of endometriosis and IBD, which poses a significant challenge in determining a cause-effect relationship between the two conditions.
Furthermore, the diagnosis of endometriosis often faces delays, with an average delay of seven years estimated between the onset of symptoms and definitive diagnosis. This delay further complicates the evaluation of the temporal relationship between endometriosis and IBD.
Distinguishing Between Endometriosis and IBD
Given the overlapping symptoms and shared characteristics of endometriosis and IBD, distinguishing between these conditions can be challenging. Both conditions can result in similar symptoms, such as abdominal pain and bowel-related symptoms, which can lead to misdiagnosis or delayed diagnosis.
In cases where endometriosis and IBD coexist, the symptoms can be atypical and cyclic, and fibrosis caused by chronic inflammation can lead to obstruction of the intestinal lumen. Therefore, it’s essential for healthcare professionals to consider both conditions when evaluating patients with such symptoms.
In cases of intestinal endometriosis, endoscopic biopsies may reveal IBD-like lesions. However, these lesions may represent an epiphenomenon of endometriosis rather than a true IBD. Hence, patients with concurrent IBD and endometriosis should be adequately followed up for the reassessment of IBD diagnosis over time.
The Role of Treatment in the Risk of IBD
The treatment of endometriosis could potentially influence the risk of developing IBD. For instance, oral contraceptives are a common treatment for endometriosis, and a meta-analysis of 14 studies suggested an increased risk of IBD among users of oral contraceptives. Additionally, non-steroidal anti-inflammatory drugs (NSAIDs), often used for pain relief in endometriosis, have been reported to increase the risk of IBD.
The Need for Further Research
Though existing research has shed some light on the association between endometriosis and IBD, there is still much to uncover. Further research is needed to better understand the temporal relationship between endometriosis and IBD in cases of co-occurrence and identify predictors that could be useful for evaluation and management of these patients.
Understanding these conditions and their potential links can not only improve diagnostic accuracy but also inform treatment strategies and improve the quality of life for those affected.
Distinguishing between endometriosis and inflammatory bowel disease can be a challenging task due to the overlapping symptoms and shared characteristics of these conditions. However, understanding the nuances of these conditions and the potential links between them can lead to improved diagnostic accuracy and more effective treatment strategies. As research progresses in this area, we hope to gain a better understanding of these complex conditions and continue to improve the lives of those affected.
Related Reading:
- Finding an Endometriosis Specialist: Your Guide to Effective Treatment
- Unraveling the Connection Between Endometriosis and Autoimmune Diseases
References:
- Parazzini F, Luchini L, Vezzoli F, Mezzanotte C, Vercellini P. Gruppo italiano perlo studio dell’endometriosi. Prevalence and anatomical distribution of endometriosisin women with selected gynaecological conditions: results from amulticentric Italian study. Hum Reprod 1994;9:1158–62.
- Bulun SE. Endometriosis. N Engl J Med 2009;360:268–79.
- Weed JC, Ray JE. Endometriosis of the bowel. Obstet Gynecol 1987;69:727–30.
- Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology 2012;142:46–54.
- Nielsen NM, Jorgensen KT, Pedersen BV, Rostgaard K, Frisch M. The co-occurrence of endometriosis with multiple sclerosis, systemic lupus erythematosus and Sjogren syndrome. Hum Reprod 2011;26:1555–9.

Understanding Neuroproliferative Vestibulodynia and the Connection with Endometriosis
Table of contents
A few weeks ago, we delved into the intricacies of vestibulodynia and its potential association with painful intercourse in individuals with endometriosis. We presented an overview of vestibulodynia subtypes in general and discussed one of the more common presentations we see in those with endometriosis – hormonally mediated vestibulodynia which in many is caused from the side effects of the birth control pill, which are offered as first line “treatments” for endometriosis. Today, we will focus on another subtype, neuroproliferative vestibulodynia (NPV), and the fascinating connections are are seeing in these two conditions, including the role of mast cells.
If you missed our previous discussion on painful sex and vestibulodynia, you can find the detailed information here.
Recent research endeavors have yielded valuable insights into the fundamental causes of these conditions, unveiling a shared mechanism involving neuroproliferation, characterized by an increase in nerve cells. Furthermore, an elevated presence of mast cells—integral components in immune function—has been observed both in endometriosis tissue and the vestibule of individuals diagnosed with neuroproliferative vestibulodynia (NPV).
Individuals diagnosed with NPV undergo a surgical procedure which is excised to remove the problematic tissue, sound familiar?
This surgical approach has demonstrated notable success in alleviating pain for individuals affected by NPV. Dr. Paul Yong, an OBGYN, endometriosis surgeon, and researcher based in Canada, addressed the parallels between these two conditions during his presentation titled ‘Neuroproliferative Dyspareunia’ at the ISSWSH’s annual conference in March 2022. Dr. Yong’s insights laid the foundation for subsequent research, with Dr. Irwin Goldstein initiated further exploration earlier this year. We were lucky enough to be able to speak directly with these two on our podcast iCarebetter: Endometriosis Unplugged, available on Spotify (linked here) and Apple Podcasts.
A Quick Overview
Vestibulodynia
Vestibulodynia is a condition characterized by pain in the vestibule, the area of tissue within the vulva that surrounds the opening of the vagina. This pain can be described as sharp, stinging, burning, or hypersensitive, and can occur spontaneously or be provoked by touch or pressure, and many people will report superficial dyspareunia (or pain upon insertion) which is not limited to penis in vagina sex. Vestibulodynia is a subcategory of a broader condition called vulvodynia, which refers to chronic pain in the vulva.
Endometriosis
On the other hand, endometriosis is a condition where tissue similar to the lining of the uterus grows outside the uterus, often causing pain and fertility issues. This condition can cause deep dyspareunia, or pain with deep vaginal penetration. Like vestibulodynia, the pain associated with endometriosis can be chronic and can significantly impact the quality of life.
The Concept of Neuroproliferative Dyspareunia
Both vestibulodynia and endometriosis can lead to pain during sexual intercourse and the term neuroproliferative dyspareunia, is in reference to the source of the pain. Both tissues have been shown to have neuroproliferation, or increased growth, of nerve endings in the areas affected by these conditions and we are now seeing an aberrant amount of mast cells as well also contributing to inflammation. This overgrowth of nerves, and presence of excessive mast cells, can lead to heightened sensitivity and pain during vaginal penetration, both superficially, as well as deep.
Neuroproliferation in Vestibulodynia
In the case of vestibulodynia, research has shown that there are too many nerve endings in the vestibule tissue. This overgrowth of nerves, or neuroproliferation, is still under investigation. However, it is believed that this could be due to a congenital birth defect, with the excess nerve endings developing very early. There are two types of neuroproliferative vestibulodynia: primary (congenital) and secondary (acquired). In primary vestibulodynia, individuals have experienced pain their entire lives though usually identified shortly after menses or with first attempts at penetration (sex, tampons, speculum exams) while in secondary or acquired vestibulodynia, pain develops later in life usually after an event such as an allergic reaction, chronic yeast infections or other infection, and there has typically been a period of normalcy prior to these event.
Neuroproliferation in Endometriosis
In endometriosis, nerve fibers have been found around endometriosis lesions in the pelvic peritoneum. These nerve fibers are more numerous in individuals with endometriosis compared to those without the condition. The increase in nerve fibers is believed to be driven by the immune response to infection or allergy, leading to nerve proliferation.
Symptoms of Neuroproliferative Vestibulodynia and Endometriosis
Vestibulodynia Symptoms
People with vestibulodynia typically experience pain at the entrance of the vagina, called the vestibule. This pain can be described in various ways, including as sharp, stinging, burning, or hypersensitive. This pain can also be classified by when it occurs, with provoked vestibulodynia referring to pain that occurs with touch or pressure, while unprovoked pain occurs spontaneously.
Endometriosis Symptoms
In endometriosis, the pain is typically experienced deeper within the pelvis, often during or after sexual intercourse. This deep dyspareunia can also be accompanied by other symptoms, such as painful periods (dysmenorrhea), painful bowel movements, and chronic pelvic pain to name a few.
For more signs and symptoms, check out our blog Endometriosis Signs and Symptoms: Everything You Need to Know.
Causes of Neuroproliferative Vestibulodynia and Endometriosis
Causes of Vestibulodynia
The exact causes of vestibulodynia are still being investigated. However, research suggests that the overgrowth of nerves in the vestibule tissue could be triggered by signaling from immune cells in the tissue. This could be due to a congenital birth defect, resulting in excess nerve endings developing very early, or it could be an acquired condition, developing later in life possibly due to infection or allergy.
Causes of Endometriosis
The causes of endometriosis are also not fully understood though we have began to shift away from the narrative that it is caused by retrograde menstruation, and towards a genetic basis. We hope that in the future with new research, we will be able to fully understand the cause (or causes) and have optimal treatment methods to address the heterogeneity of this disease.
You can read more about these theories in our blogs listed below:
- The History of Endometriosis: Unraveling the Theories and Advances [or lack thereof]
- Is Endometriosis Genetic? Understanding the Genetic Links in Endometriosis.
There has been limited research in the role of mast cells in endometriosis thus far, and Dr. Irwin Goldstein, MD has now successfully demonstrated in a case study of a patient with NPV, her endometriosis pathology also demonstrated similar findings, as well as a biopsy taken of her colon during a colonoscopy.
Thank you to Paul Yong, MD for this information, here is a comparison of endometriosis and NPV and common mechanisms in each.
| Endometriosis | NPV | |
| Prevalence | Approx 10% | Approx 10% |
| Diagnosis | Histological diagnosis(ectopic endometrial-like epithelium/stroma) | Clinical diagnosis (but normal vestibular histology consists of epithelium/stroma) NPV – mast cells and excessive nerve endings |
| Description of Dyspareunia | Deep | Superficial |
| Nerve Density | Increased local nerve density compared to controls | Increased local nerve density compared to controls |
| Neutrophins | Increased NGF expression by endometriosis stroma when higher nerve fibers | Increased NGF expression by immune cells in vestibulodynia in areas with more nerve fibers |
| Inflammation | Increased IL-1b expression by endometriosis when higher nerve fibres Endometriosis stromal cells, when stimulated by IL-1b, increase production of NGF and promote nerve fibre development in a PC12 2q13 polymorphism (adjacent to IL-1 family genes) Mast cells Tryptase | Increased IL-1b in tissues in vestibulodynia vs. controls; Not observed in another study (Eva) Vestibular fibroblasts from patients with vestibulodynia expressed more IL-1b compared to external vulvar fibroblasts and to controlsIL-1b and IL-1R antagonist gene polymorphism Mast cells Tryptase Heparanase |
References
- Mwaura, A. N., Marshall, N., Anglesio, M. S., & Yong, P. J. (2023). Neuroproliferative dyspareunia in endometriosis and vestibulodynia. Sex Med Rev. https://doi.org/10.1093/sxmrev/qead033
- Goldstein, S., Yee, A., & Goldstein, I. (2022). Severe Allergic, Inflammatory and Traumatic Reactions of the Vestibule Associated with Acquired Neuroproliferative Vestibulodynia. The Journal of Sexual Medicine, 19(8, Supplement 3), S3. https://doi.org/https://doi.org/10.1016/j.jsxm.2022.05.012
Bornstein, J., Goldstein, A. T., Stockdale, C. K., Bergeron, S., Pukall, C., Zolnoun, D., Coady, D., consensus vulvar pain terminology committee of the International Society for the Study of Vulvovaginal, D., International Society for the Study of Women’s Sexual, H., & International Pelvic Pain, S. (2016). 2015 ISSVD, ISSWSH, and IPPS Consensus Terminology and Classification of Persistent Vulvar Pain and Vulvodynia. J Sex Med, 13(4), 607-612. https://doi.org/10.1016/j.jsxm.2016.02.167

Postmenopausal Malignant Transformation of Endometriosis
Table of contents
Endometriosis is a pain and infertility producing condition which predominantly affects premenopausal women. Estimates suggest that up to 10% of women worldwide suffer from the condition during their reproductive years. While the incidence of postmenopausal endometriosis is considerably lower, studies have suggested that this may still be in the neighborhood of 2.5%. So it is a misconception that endo is exclusively a disease of younger women.
Further, although endometriosis is a benign disorder, there lies a risk of malignant transformation, at all ages. This article delves into the potential for malignant transformation of postmenopausal endometriosis.
Understanding Endometriosis and Menopause
Postmenopausal endometriosis refers to the occurrence or continuation of endometriosis symptoms after menopause, which typically occurs around age 50. This is defined as the cessation of menstrual cycles for twelve consecutive months. After this point, the ovaries produce minimal estrogen, a hormone which is generally considered essential for endo growth. So, without this hormone, or lowered levels, most cases of endometriosis naturally diminish. Yet, for some postmenopausal women, endometriosis can persist or even manifest anew.
The cause or causes of endometriosis in younger women are controversial and incompletely defined. Through uncertain but likely multifactorial mechanisms, endometriosis is characterized by the presence and growth of ectopic endometrial-like tissue outside the uterus. While one might assume that a hypoestrogenic state associated with menopause would alleviate endometriosis, this isn’t always the case.
In postmenopausal women, the causes of endometriosis are less clear. Some contributing factors include:
- Residual Disease: Endometriosis that began before menopause may continue after menopause due to residual disease and growth stimulated by factors other than estrogen or high sensitivity to low estrogen levels.
- Exogenous Estrogen: Hormone replacement therapy (HRT) can potentially stimulate the growth of endometrial cells. This may be particularly relevant for postmenopausal women who take estrogen-only HRT, which can reactivate endometrial implants or even initiate new growths.
- Endogenous Estrogen Conversion: Adipose (fat) tissue can produce estrogen by converting it from other hormones. Postmenopausal women with higher amounts of adipose tissue might produce enough estrogen to promote the growth of endo. Fat can also store xeno-estrogens from certain toxins and then slowly release them into circulation. The tissue microenvironment around endometriosis lesions also contributes to local estrogen production.
Malignant Transformation: A Rare but Possible Event
While endometriosis is overwhelmingly benign, studies have indicated that women with endometriosis have an increased risk of developing certain types of ovarian cancers, specifically clear cell and endometrioid carcinomas.
Some factors that might increase the risk include:
- Duration of Endometriosis: Prolonged presence of endometriosis lesions might increase the risk of malignant transformation. In general, cancer risk increases with age and it is well known that chronic inflammation contributes to formation of cancer. Endo is inflammatory in nature. Thus, if endo is still growing after menopause this means more time in an inflammatory state, hypothetically contributing to the risk.
- HRT Use: As mentioned, exogenous estrogen can stimulate endometriosis growth, potentially increasing the risk of malignant changes in existing lesions. This is not proven but may be a contributory factor which is very complicated due to individual variations in receptor activity and levels of estrogen.
- Genetic Factors: Some genetic mutations might predispose women to both deeply invasive endometriosis and ovarian cancer, and there is overlap. Epigenetic factors regulate which genes turn on an off during life and are influenced by environmental factors. There is also a potential cumulative effect in the number of active mutated genes over the years. Some of the key genetic factors include:
- PTEN: PTEN is a tumor suppressor gene. Its mutations have been identified in both endometriosis and endometrioid and clear cell ovarian cancers. Loss of PTEN function can lead to uncontrolled cell growth and might play a role in the malignant transformation of endometriosis.
- ARID1A: ARID1A mutations are frequently seen in endometriosis-associated ovarian cancers. This gene is involved in chromatin remodeling, and its mutation can lead to disruptions in DNA repair and subsequent malignant transformation.
- KRAS and BRAF: Mutations in these genes are known to play roles in the pathogenesis of various cancers. They’ve been identified in benign endometriotic lesions and might contribute to the early stages of malignant transformation.
- Inherited Genetic Mutations: Women with inherited mutations in BRCA1 and BRCA2 genes, known for their association with breast and ovarian cancers, might also have an increased risk of developing endometriosis and its subsequent malignant transformation.
Conclusions
Postmenopausal endometriosis, although less common than its premenopausal counterpart, cannot be overlooked. The absolute risk of malignant transformation, albeit very low, emphasizes the importance of regular monitoring and endo specialist consultations for postmenopausal women with endometriosis or its symptoms. When postmenopausal endometriosis is suspected or diagnosed, especially if it is invasive and there are unusual symptoms or pelvic masses, a consultation with a gynecologic oncologist is also prudent.
References
Bulun SE. Endometriosis. N Engl J Med. 2009;360(3):268-279.
Pearce CL, Templeman C, Rossing MA, et al. Association between endometriosis and risk of histological subtypes of ovarian cancer: a pooled analysis of case-control studies. Lancet Oncol. 2012;13(4):385-394.
Luca Giannella, Chiara Marconi, Jacopo Di Giuseppe, et al. Malignant Transformation of Postmenopausal Endometriosis: A Systematic Review of the Literature. Cancers (Basel) 2021 Aug 10;13(16):4026.
Luca Giannella, Chiara Marconi, Jacopo Di Giuseppe, et al. The association between endometriosis and gynecological cancers and breast cancer: a review of epidemiological data. Gynecol Oncol. 2011;123(1):157-163.
Sato N, Tsunoda H, Nishida M, et al. Loss of heterozygosity on 10q23.3 and mutation of the tumor suppressor gene PTEN in benign endometrial cyst of the ovary: possible sequence progression from benign endometrial cyst to endometrioid carcinoma and clear cell carcinoma of the ovary. Cancer Res. 2000;60(24):7052-7056.
Wiegand KC, Shah SP, Al-Agha OM, et al. ARID1A mutations in endometriosis-associated ovarian carcinomas. N Engl J Med. 2010;363(16):1532-1543.
Dinulescu DM, Ince TA, Quade BJ, Shafer SA, Crowley D, Jacks T. Role of K-ras and Pten in the development of mouse models of endometriosis and endometrioid ovarian cancer. Nat Med. 2005;11(1):63-70.
Saha R, Pettersson H, Svedberg P, et al. Endometriosis and the risk of ovarian and endometrial adenocarcinomas: a meta-analysis. BMJ Open. 2020;10(4):e034760.

The Hidden Connection Between Systemic Lupus and Endometriosis
Based on possible shared characteristics and pathogenesis the interconnectedness of various ailments becomes a focal point of research. Such is the relationship between endometriosis and lupus, two seemingly unrelated conditions that share intriguing parallels. This article aims to shed light on the increased risk of being diagnosed with endometriosis in patients suffering from Systemic Lupus Erythematosus or SLE. The purpose of unraveling connections is that this may lead to treatment discoveries.
Table of contents
Understanding Endometriosis
Endometriosis is a multifaceted disease that primarily affects women in their reproductive years. It is characterized by the abnormal growth of endometrial-like tissue outside the uterus, leading to chronic pelvic pain, and potential infertility.
The pathophysiology of endometriosis involves a systemic inflammatory response, influenced by female sex hormones that may subtly affect the maintenance of immunity or the development of autoimmune diseases.
Getting to Know Systemic Lupus Erythematosus (SLE)
SLE is a chronic, autoimmune disease that can affect various parts of the body, including the skin, joints, kidneys, heart, and lungs. It involves the immune system attacking the body’s own tissues, leading to inflammation and damage. Women, especially of childbearing age, are more frequently diagnosed with SLE than men. Other factors such as ethnicity, age of onset, and socioeconomic class significantly influence SLE incidence, with notable geographic differences observed.
Endometriosis and SLE: The Intriguing Association
Epidemiological studies suggest a solid link between endometriosis and female-dominant autoimmune diseases. However, not all studies support a significant association between endometriosis and SLE. The potential for spurious associations due to small study sizes and suboptimal control selection is high.
Unraveling the Connection: A Comprehensive Study
Given these inconsistencies, and accepting that the findings may not be applicable to all geo-ethnic populations, a large nationwide retrospective cohort study was conducted to assess the risk of endometriosis in women diagnosed with SLE. The study analyzed data from the Taiwan Longitudinal Health Insurance Research Database 2000 (n = 958,349) over a 13-year follow-up period (2000–2013).
Study Design and Population
The study adopted a retrospective cohort design with primary data sourced from the Taiwan National Health Insurance Research Database (NHIRD). The study cohort included women diagnosed with SLE between 1997 and 2013, and the index date was defined as the first diagnosis of SLE.
Assessed Outcome
The primary outcome was defined as the diagnosis of endometriosis. Given the lack of non-invasive diagnostic tools for endometriosis, the disease’s diagnosis was derived from clinical evidence or surgical intervention. Every effort was made to optimize parameters of non-surgical diagnosis of endo but surgical validation was lacking in a large number of subjects, representing a significant study weakness.
Results and Implications
The study, within stated limitations, found a statistically significant association between SLE and endometriosis, after controlling for age.
Conclusion: A Call for Further Research
The risk of endometriosis was found to be significantly higher in SLE patients compared to the general population in this study. This adds substantially to the overall body of evidence supporting an association. However, more research is needed to fully understand this association and to determine if it can be generalized across different geo-ethnic populations. Clearly, more basic science research is also critically needed to support epidemiologic associations.
Reference:
https://pubmed.ncbi.nlm.nih.gov/35922461/

Can endometriosis cause miscarriage? Understanding Endometriosis and Its Impact on Miscarriage
Endometriosis is a prevalent health condition, affecting approximately 10% of women worldwide. It is often associated with chronic pain and infertility, but its potential connection to miscarriage is not as widely recognized. This article aims to shed light on the link between endometriosis and miscarriage, drawing on recent scientific research and expert insights.
Table of contents
What is Endometriosis?
Endometriosis is a chronic condition where tissue similar to the lining of the uterus, known as endometrium, grows outside the uterus. This tissue can grow on the ovaries, fallopian tubes, or the lining of the pelvic cavity. Just as the inner lining of the uterus thickens, breaks down, and bleeds with each menstrual cycle, so too does the endometrial-like tissue outside the uterus. However, this displaced tissue has no way to exit the body, leading to various problems.
Read More: What causes endometriosis?
Pathogenesis of Endometriosis
Endometriosis develops in stages, with severity ranging from minimal to severe. The American Society for Reproductive Medicine groups endometriosis into four stages: minimal (Stage I), mild (Stage II), moderate (Stage III), and severe (Stage IV). The stages reflect the extent, location, and depth of endometrial-like tissue growth, as well as the presence and severity of adhesions and the presence and size of ovarian endometriomas.
Symptoms of Endometriosis
While some women with endometriosis may have no symptoms, others may experience:
- Painful periods
- Pain during intercourse
- Pain with bowel movements or urination
- Excessive bleeding
- Infertility
- Other signs and symptoms such as fatigue, diarrhea, constipation, bloating, or nausea
Read more: 20 Signs and Symptoms of Endometriosis
Endometriosis and Pregnancy Complications
Endometriosis has long been associated with infertility, with studies indicating that up to 50% of women with infertility have the condition. However, less is known about its impact on women who do conceive. Emerging research suggests that endometriosis may increase the risk of several pregnancy complications, including preterm birth, cesarean delivery, and miscarriage.
Read More: How Does Endometriosis Cause Infertility?
Endometriosis and Miscarriage: Understanding the Connection
Recent research has begun to explore the potential link between endometriosis and miscarriage. Miscarriage, also known as spontaneous abortion, is defined as the loss of a pregnancy before 20 weeks of gestation. It is estimated that about 10-20% of known pregnancies end in miscarriage. The actual number is likely higher, as many miscarriages happen so early in pregnancy that a woman might not even know she’s pregnant.
The Role of Inflammation
One theory proposes that the inflammation associated with endometriosis could interfere with the early stages of pregnancy. Endometriosis is characterized by chronic pelvic inflammation, which could potentially disrupt the implantation of the embryo or the development of the placenta.
The Impact of Surgical Treatment
Another factor to consider is the potential impact of surgical treatment for endometriosis. There have only been a few clinical trials and they do not indicate that surgical excision reduces the risk of miscarriage. However, there are two very large databases from Sweden and Scotland that suggest a benefit to removing known endometriosis to lower pregnancy loss risk. More research is required.
Hormonal Factors
Endometriosis can alter the hormonal environment of the uterus, which could potentially impact early pregnancy. More research is needed to fully understand how these hormonal changes might contribute to miscarriage risk.
Research Insights: Endometriosis and Miscarriage Risk
Several studies have investigated the link between endometriosis and miscarriage. A meta-analysis published in 2020 in the journal BioMed Research International found that women with endometriosis had a significantly higher risk of miscarriage compared to women without the condition. This risk was particularly pronounced in women who conceived naturally, rather than those with tubal infertility who conceived through assisted reproductive technology (ART).
Coping with Endometriosis and Miscarriage
The potential link between endometriosis and miscarriage can come as distressing news. However, it’s important to remember that many women with endometriosis have successful pregnancies. So, counseling and intervention really depend on the individual situation. With repeat losses, there are many potential reasons but it appears that endo can be one of them.
Read more: Find an Endometriosis Specialist for Diagnosis, Treatment, & Surgery.
Conclusion
Endometriosis is a complex condition that can impact various aspects of a woman’s health, including her fertility and pregnancy outcomes. While research suggests a potential link between endometriosis and miscarriage, many women with the condition have successful pregnancies. If you have endometriosis or suspect you have endo, and having difficulty conceiving or experiencing pregnancy losses, it’s crucial to seek consultation with an endometriosis specialist.
Reference:
https://pubmed.ncbi.nlm.nih.gov/33490243/

Epigenetics and Endometriosis Hereditary: Unraveling the Complex Web of Hereditary Implications
Endometriosis, a medical condition afflicting numerous women worldwide, continues to puzzle medical researchers due to its complex nature and the myriad of genetic and environmental factors contributing to its development. This article aims to dissect the convoluted genetic aspect of endometriosis, providing a comprehensive understanding of its hereditary implications.
Table of contents
- 1. Introduction to Endometriosis
- 2. The Puzzle of Endometriosis Hereditary
- 3. Theories on the Pathogenesis of Endometriosis
- 4. The Genetic/Epigenetic Theory: A Closer Look
- 5. Clinical Implications of the Genetic/Epigenetic Theory
- 6. Prevention and Treatment of Endometriosis: A Genetic/Epigenetic Perspective
- 7. Conclusion
1. Introduction to Endometriosis
Endometriosis is a condition characterized by the growth of endometrium-like tissue outside the uterus. This disease exhibits significant diversity in its manifestation, with the tissue appearing in various forms and locations. It has a significant impact on the quality of life of the affected individual, often causing pain, infertility, and other related complications.
2. The Puzzle of Endometriosis Hereditary
2.1 Hereditary Factors in Endometriosis
Endometriosis has been confirmed as a hereditary disease, with the risk of developing the condition significantly higher in first-degree relatives of affected women. Twin studies further corroborate this, showing a similar prevalence and age of onset in twins. Despite this, the exact genetic mechanisms contributing to endometriosis remain elusive and likely presents with an inheritance pattern that is multifactorial.
2.2 Genetic and Epigenetic Incidents in Endometriosis
Genetic and epigenetic incidents, both inherited and acquired, significantly contribute to the development of endometriosis. These incidents, which can cause changes in gene expression, are often triggered by environmental factors such as oxidative stress and inflammation. Familial clustering of endometriosis has been shown in an array of studies with similar findings. First-degree relatives are 5 to 7 times more likely to have surgically confirmed disease.
Familial endometriosis may be more severe than sporadic cases. This also supports the multifactorial inheritance of endometriosis and a genetic propensity as it may spread more severely to offspring or siblings. These women with familial inheritance may also have earlier age of onset and symptoms.
3. Theories on the Pathogenesis of Endometriosis
3.1 The Implantation Theory
The implantation theory, popularized by Sampson in 1927, suggests that endometriosis is caused by the implantation of endometrial cells in locations outside the uterus. This theory, while reasonable, fails to explain certain observations, such as the occurrence of endometriosis in men and women without endometrium.
3.2 The Metaplasia Theory
The metaplasia theory postulates that endometriosis is a result of metaplastic changes, a process where one type of cell changes into another type due to environmental stress. This theory, while accounting for some observations, is limited by the varying definitions of “metaplasia” and the disregard for genetic or epigenetic changes.
3.3 The Genetic/Epigenetic Theory
The genetic/epigenetic theory proposes that endometriosis results from a series of genetic and epigenetic incidents, both hereditary and acquired. This theory is compatible with all known observations of endometriosis, providing a comprehensive understanding of the disease’s pathogenesis.
4. The Genetic/Epigenetic Theory: A Closer Look
4.1 Genetic and Epigenetic Incidents: The Triggers of Endometriosis
According to the genetic/epigenetic theory, endometriosis is triggered by a series of genetic and epigenetic incidents. These incidents can be hereditary, transmitted at birth, or acquired later in life due to environmental factors such as oxidative stress and inflammation.
4.2 The Role of Redundancy in the Development of Endometriosis
Redundancy, where a task can be accomplished by multiple pathways, plays a significant role in the development of endometriosis. This redundancy can mask the effects of minor genetic and epigenetic changes, causing them to become visible only when a higher capacity is needed.
4.3 The Genetic/Epigenetic Theory and Endometriosis Lesions
Endometriosis lesions are clonal, meaning they originate from a single cell that has undergone genetic or epigenetic changes. The genetic/epigenetic theory proposes that these lesions can remain dormant for extended periods, similar to uterine myomas, and may only be reactivated by certain triggers such as trauma.
5. Clinical Implications of the Genetic/Epigenetic Theory
5.1 Understanding the Nature of Endometriosis Lesions
According to the genetic/epigenetic theory, most subtle or microscopic lesions are normal endometrium-like cells that would likely resolve without intervention. In contrast, typical, cystic, and deep lesions are benign tumors that do not recur after complete excision but may progress slowly or remain dormant for an extended period.
5.2 The Role of Factors in Endometriosis Hereditary
The genetic/epigenetic theory suggests that genetic and epigenetic defects inherited at birth may play a significant role in the development of endometriosis. These hereditary factors may not only contribute to the disease’s onset but also to associated conditions such as subfertility and pregnancy complications.
5.3 Variability in Endometriosis Lesions
The genetic/epigenetic theory explains that endometriosis lesions can vary significantly in their reaction to hormones and other environmental factors. This variability is due to the specific set of genetic and epigenetic changes present in each lesion.
6. Prevention and Treatment of Endometriosis: A Genetic/Epigenetic Perspective
6.1 Prevention of Genetic/Epigenetic Incidents
Preventing the genetic/epigenetic incidents that trigger endometriosis can be a complex task. However, reducing repetitive stress may be useful in this regard.
6.2 Treatment of Endometriosis
The genetic/epigenetic theory suggests that the treatment of endometriosis should focus on the complete excision of the lesions to prevent recurrence. However, it also proposes that less radical surgery may be sufficient in some cases where the surrounding fibrosis and outer cell layers are composed of normal cells with reversible changes.
7. Conclusion
While the genetic/epigenetic theory provides a comprehensive understanding of the pathogenesis of endometriosis, it remains a theory until disproven by new observations. Further research is needed to fully elucidate the genetic and epigenetic mechanisms contributing to endometriosis, paving the way for more effective prevention and treatment strategies. Despite the complexity and challenges, the pursuit of knowledge in this field continues, offering hope for a future where endometriosis can be effectively managed and potentially prevented.
Reference:
- Koninckx PR, Ussia A, Adamyan L, Wattiez A, Gomel V, Martin DC. Pathogenesis of endometriosis: the genetic/epigenetic theory. Fertil Steril. 2019 Feb;111(2):327-340. [PubMed]
- Simpson J, Elias S, Malinak L, et al. Heritable aspects of endometriosis: 1. Genetic studies. Am J Obstet Gynecol. 1980;137:327–331. [PubMed] [Google Scholar]
- Kennedy S, Hadfield R, Mardon H, Barlow D. Age of onset of pain symptoms in non-twin sisters concordant for endometriosis. Hum Reprod. 1996;11:403–405. [PubMed] [Google Scholar]
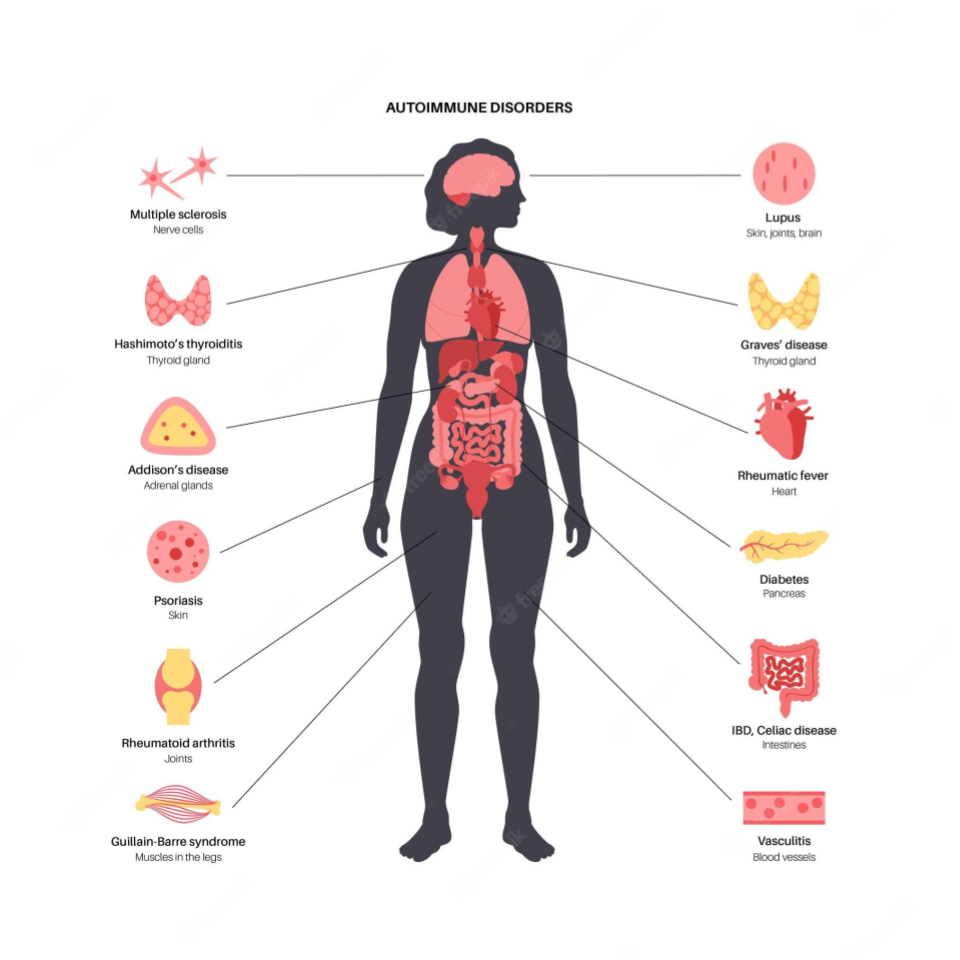
Unraveling the Connection Between Endometriosis and Autoimmune Diseases
Endometriosis causes pain, multiple bowel symptoms and infertility, among many other debilitating symptoms, in about 10% of women, mostly in the reproductive age range. Developing research has shown that there is a link to various autoimmune conditions.
Table of contents
- Understanding Endometriosis
- The Immune System’s Role
- Is Endometriosis an Autoimmune Disease?
- Systemic Lupus Erythematosus (SLE) and Endometriosis
- Sjögren’s Syndrome (SS) and Endometriosis
- Rheumatoid Arthritis (RA) and Endometriosis
- Autoimmune Thyroid Disorders (ATD) and Endometriosis
- Coeliac Disease (CLD) and Endometriosis
- Multiple Sclerosis (MS) and Endometriosis
- Inflammatory Bowel Disease (IBD) and Endometriosis
- The Bigger Picture
- The Path Ahead
Understanding Endometriosis
Endometriosis is a chronic gynecological disorder characterized by the presence of endometrial-like tissue growing outside the uterus. This means the cells look like those which line the inner part of the uterus but differ markedly in multiple ways at the molecular level. The more we find out the less it is clear what the origins are. However, they are likely partly genetic and partly based on other multiple influences of the environment on your body and genes.
The Immune System’s Role
Research suggests that abnormalities in the immune system may play a key role in the development of endometriosis. These abnormalities could prevent the immune system from effectively clearing ectopic endometrial cells, regardless of how they get there, allowing them to implant and grow outside the uterus. This hypothesis suggests that endometriosis might be, at least in part, an immunity-associated disorder.
Furthermore, endometriosis is often associated with a chronic inflammatory response, triggered by the presence of ectopic endometrial-like cells. This inflammation, coupled with the immune system’s inability to effectively remove ectopic cells, could partly explain the chronic pain often associated with endometriosis.
Is Endometriosis an Autoimmune Disease?
Autoimmune diseases occur when the immune system mistakenly attacks the body’s own cells, viewing them as foreign invaders. The link between endometriosis and autoimmune diseases is still being explored, but multiple studies suggest that women with endometriosis may have a higher risk for certain autoimmune diseases. It is not clear if endo carries a risk of developing autoimmune diseases or if the reverse is true or if they simply share common molecular mechanisms which results in both potentially occurring in any given individual. At this point it is important to stress that an “association” does not mean “cause”.
This review aims to delve into the current state of research on the association if endometriosis is an autoimmune disease. It presents key findings from population-based studies, discusses the potential implications, and highlights areas for future research.
Systemic Lupus Erythematosus (SLE) and Endometriosis
Systemic Lupus Erythematosus (SLE) is an autoimmune disease characterized by inflammation and damage to various body tissues, including the skin, joints, kidneys, and heart. Some studies have suggested a positive association between endometriosis and SLE.
One study suggested a seven-fold increase in the odds of having SLE among women with endometriosis. However, the study relied on self-reported diagnoses, which may introduce bias. A more recent cohort study found a more modest but still significant elevation in SLE risk among women with endometriosis.
Sjögren’s Syndrome (SS) and Endometriosis
Sjögren’s Syndrome (SS) is an autoimmune disorder characterized by dry eyes and mouth, often accompanied by other systemic symptoms. Several studies have investigated the potential link between SS and endometriosis.
A meta-analysis of three case-control studies found a 76% higher odds of SS in women with endometriosis. However, these studies had small sample sizes and wide confidence intervals, indicating a need for further research. Confidence intervals describe the range of results around a measurement which indicate how accurate the conclusion might be. The tighter it is among measurements the better.
Rheumatoid Arthritis (RA) and Endometriosis
Rheumatoid Arthritis (RA) is a chronic inflammatory disorder affecting many joints, including those in the hands and feet. Some studies have suggested a link between endometriosis and an increased risk of developing RA.
One meta-analysis, for example, found a 50% increased risk of RA among women with endometriosis. Again, the studies included in the analysis had limitations, including small sample sizes and wide confidence intervals.
Autoimmune Thyroid Disorders (ATD) and Endometriosis
Autoimmune thyroid disorders (ATDs), including Graves’ disease and Hashimoto’s thyroiditis, occur when the immune system attacks the thyroid gland, leading to either overactivity (hyperthyroidism) or underactivity (hypothyroidism) of the gland.
A meta-analysis of three case-control studies suggested a non-significant increase in the odds of ATD in women with endometriosis. However, the studies had high heterogeneity and low-quality scores, suggesting that further research is needed.
Coeliac Disease (CLD) and Endometriosis
Coeliac disease (CLD) is an autoimmune disorder where ingestion of gluten leads to damage in the small intestine. Some studies have suggested a possible link between endometriosis and CLD.
A meta-analysis of two case-control studies found a four-fold increase in the odds of CLD among women with endometriosis. Again, these studies had small sample sizes and wide confidence intervals, indicating a need for further research.
Multiple Sclerosis (MS) and Endometriosis
Multiple Sclerosis (MS) is a chronic disease that attacks the central nervous system. Current research on the association between MS and endometriosis is limited and inconclusive, with some studies suggesting a possible link while others finding no significant association.
Inflammatory Bowel Disease (IBD) and Endometriosis
Inflammatory bowel disease (IBD), including Crohn’s disease and ulcerative colitis, is characterized by chronic inflammation of the gastrointestinal tract. Some studies indicate a possible association between IBD and endometriosis.
One study found a 50% increase in the risk of IBD among women with endometriosis. However, the study had a small sample size and the confidence interval was wide, indicating a need for further research.
The Bigger Picture
While the evidence for an association between endometriosis and certain autoimmune diseases is compelling, it’s important to emphasize that correlation or association does not imply causation. Further research is needed to determine whether endometriosis actually increases the risk of developing autoimmune diseases or vice versa, or whether the two share common risk factors or underlying mechanisms.
The potential link between endometriosis and autoimmune diseases highlights the importance of a comprehensive approach to women’s health. For women with endometriosis, being aware of the potential increased risk of autoimmune diseases can inform their healthcare decisions and monitoring.
The Path Ahead
The intersection of endometriosis and autoimmune diseases is a complex and evolving field of research. Better understanding the relationship between these conditions could help improve diagnosis, treatment, and ultimately, the quality of life for patients with endometriosis.
By continuing to explore this connection, we are gaining new insights into the pathophysiology of endometriosis and autoimmune diseases, potentially leading to novel treatments and preventive strategies.
Reference:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6601386/

How Does Endometriosis Cause Infertility?
Endometriosis, a complex and often misunderstood condition, can significantly impact a woman’s fertility. Understanding the intricacies of this condition, its causes, and its effects on fertility can be vital in paving the way for effective treatment strategies.
Table of contents
An Introduction to Endometriosis
Endometriosis is a benign, estrogen-dependent disorder primarily affecting approximately one in ten cisgender women in their reproductive years. It may also have an impact on transgender men, where the condition may be present in a higher percentage. While it has been reported in cisgender men, it is exceedingly rare. Thus the fertility impact discussed here is that which specifically affects the uterus, Fallopian tubes and ovaries.
Endometriosis is characterized by the abnormal presence of endometrial-like tissue outside the uterus. This abnormally growing tissue is often found in the pelvic region, such as on the ovaries, fallopian tubes, and the outer surface of the uterus. Still, in some cases, it can extend beyond the pelvic area.
While endometriosis affects approximately 10-15% of cisgender women in their reproductive years, the condition is more prevalent in those struggling with infertility, affecting up to 25%-50% of this demographic. The exact cause of endometriosis remains a subject of research and debate, and its impact on fertility is multi-faceted and complex.
Understanding The Pathogenesis of Endometriosis
While the precise cause of endometriosis is still under debate, several theories have emerged over the years, trying to explain the pathogenesis of this condition.
Retrograde Menstruation
The oldest theory is retrograde menstruation, which suggests that during menstruation, some of the endometrial tissue flows backward, through the fallopian tubes, into the pelvic cavity instead of leaving the body. These endometrial cells then attach to the peritoneal surfaces, proliferate, and form endometriosis implants.
Coelomic Metaplasia and Metastatic Spread
Other theories suggest that cells in the peritoneum can transform into endometrial cells, a process known as coelomic metaplasia. Alternatively, endometrial tissue may spread through the bloodstream or lymphatic system to other parts of the body, a process known as metastatic spread. Both these theories could explain how endometriosis implants can be found in areas outside the pelvic region.
Altered Immunity
Another theory proposes that women with endometriosis have a compromised immune system, which fails to eliminate the endometrial cells that have migrated to the peritoneal cavity. This immune dysfunction may also contribute to the progression of the disease, as the immune system’s reactions may inadvertently promote the growth and proliferation of endometrial implants.
Stem Cells and Genetics
Recent research also suggests that stem cells and genetic factors may play a role in the development of endometriosis. Bone marrow-derived stem cells may differentiate into endometriosis cells, contributing to the formation of ectopic endometrial-like tissue.
Additionally, genetic predisposition may play a significant role in the development of endometriosis. People with a first-degree relative affected by the disease have a seven times higher risk of developing endometriosis.
Learn More: Current Knowledge on Endometriosis Etiology: A Systematic Review
How Does Endometriosis Cause Infertility?
Endometriosis can affect fertility through various mechanisms:
Effect on Gametes and Embryo
Endometriosis can impact the production and quality of oocytes (eggs), as well as sperm function and embryo health. The presence of endometriomas (cysts caused by endometriosis) and the inflammatory environment they create can negatively affect both oocyte production and ovulation.
Effect on Fallopian Tubes and Embryo Transport
Endometriosis can disrupt the fallopian tubes’ normal functioning and impact the embryo’s transport. The inflammation caused by endometriosis can impair tubal motility and cause abnormal uterine contractions, which can hinder the transportation of gametes (eggs and sperm) and embryos.
Effect on the Endometrium
Endometriosis can also impact the uterine lining or endometrium, which can lead to implantation failure. Research suggests that endometriosis can alter the gene expression in the endometrium, affecting its receptivity to implantation.
Read More: Learn More About the Connections Between Endometriosis and Infertility
Current Treatment Options for Endometriosis-Associated Infertility
The treatment of endometriosis-associated infertility is multi-faceted and can include expectant management, medical treatment, surgical treatment, and assisted reproductive technologies.
Expectant Management
While endometriosis significantly lowers fertility rates, some women with mild to moderate endometriosis can still conceive without any medical or surgical intervention. However, this approach may be more suitable for younger women with mild endometriosis and no other fertility issues.
Surgical Treatment
Surgery can be both diagnostic and therapeutic in the context of endometriosis. The goal of surgical treatment is to remove or reduce endometriosis implants and restore normal pelvic anatomy and reduce the inflammatory impact. This could potentially improve fertility, particularly in women with severe endometriosis.
Assisted Reproductive Technology
In vitro fertilization (IVF) is currently the most effective treatment for endometriosis-associated infertility. IVF can be particularly beneficial for women with severe endometriosis or those for whom other treatments have failed.
Medical Treatment
Medical treatment for endometriosis primarily targets reducing the severity of the disease and relieving symptoms. Hormonal medications such as combined oral contraceptives, progestins, danazol, and gonadotropin-releasing hormone agonists or antagonists (GnRH analogs) are commonly used. However, these medications have not shown any significant benefit in treating endometriosis-associated infertility.
Read More: Natural, Medical & Surgical Treatment of Endometriosis Infertility
Looking Towards The Future: Potential Treatments
As our understanding of endometriosis deepens, new potential treatment options are emerging, such as therapies targeting the abnormal gene expression and inflammation caused by endometriosis. Furthermore, stem cell therapies and genetic interventions hold promise for treating endometriosis-associated infertility in the future. As research continues, the hope is that these advancements will lead to more effective strategies for managing this complex condition and improving fertility outcomes in those with endometriosis.
Read More: How Do Endo Fertility Issues Impact the Mental Health of a Person?
Reference: Macer ML, Taylor HS, Obstet Gynecol Clin North Am. 2012 Dec;39(4):535-49.

Interstitial Cystitis and Endometriosis: Unraveling the Evil Twins Syndrome of Chronic Pelvic Pain
Table of contents
Introduction
Chronic pelvic pain (CPP) is a health condition that burdens millions of women worldwide. The complexity of diagnosing and treating CPP is often overwhelming due to the multitude of potential underlying causes and associated conditions. Two such conditions, often called the “Evil Twins” syndrome, are Interstitial Cystitis (IC) and Endometriosis, both commonly found in patients suffering from CPP. This article will explore these conditions’ prevalence, diagnosis, and treatment in patients with CPP.
Understanding Chronic Pelvic Pain
Chronic Pelvic Pain (CPP) is a prevalent health condition affecting an estimated 9 million women in the United States alone. It accounts for up to 40% of laparoscopies and 10% to 12% of all hysterectomies, indicating its significant impact on women’s health. The annual expenditure on diagnosing and treating CPP is nearly $3 billion.
The “Evil Twins”: Interstitial Cystitis and Endometriosis
Two conditions frequently associated with CPP are Interstitial Cystitis (IC) and Endometriosis. These conditions can present similar symptoms and coexist in patients, making the diagnosis and management of CPP even more challenging.
Interstitial Cystitis (IC)
Interstitial Cystitis, or bladder-originated pelvic pain, is a significant disorder related to CPP. The etiology of IC is multifactorial and progressive, involving bladder epithelial dysfunction, mast cell activation, and bladder sensory nerve upregulation. The exact prevalence of IC in the United States varies, with estimates ranging from 10 to 510 per 100,000 normal population. However, current research suggests that IC might be more prevalent than previously estimated.
Endometriosis
Endometriosis is another common condition among women with CPP, affecting more than half of the patients diagnosed with CPP. Symptoms include pain during sexual intercourse (dyspareunia), cyclical perimenstrual lower abdominal pelvic pain, symptom flares after sexual intimacy, and irritative voiding in case of urinary tract involvement. A definitive diagnosis of endometriosis requires visual confirmation of the lesion during laparoscopy and histologic confirmation of the presence of both ectopic endometrial glands and stroma.
The Overlap Between Interstitial Cystitis and Endometriosis
Research has demonstrated a high rate of overlap between IC and endometriosis in patients with CPP. This overlap poses challenges in diagnosis and treatment, as the presence of one condition does not preclude the existence of the other. Therefore, it is crucial to consider both conditions in the evaluation of patients with CPP.
Diagnosis of Interstitial Cystitis
The diagnosis of IC and endometriosis involves various tests and procedures, including the Potassium Sensitivity Test (PST), cystoscopy with hydrodistention, and laparoscopy.
Laparoscopy
Laparoscopy for direct visualization of endometriosis lesions and taking a biopsy is the gold standard for endometriosis diagnosis.
Read more: The Different Tests Used to Diagnose Endometriosis
Potassium Sensitivity Test (PST)
The PST is a diagnostic test developed to detect abnormal permeability of the bladder epithelium, a key factor in the pathophysiology of IC. Previous studies have validated the use of the PST in diagnosing IC, particularly at the early stages of the disease.
Cystoscopy with Hydrodistention
Cystoscopy with hydrodistention is a diagnostic procedure often used to confirm the presence of IC. The bladder is filled with sterile water under passive hydrostatic pressure, then slowly drained. The presence of submucosal petechial hemorrhages, or glomerulations, confirms the diagnosis of IC.
Biopsy
During cystoscopy under anesthesia, your provider may remove a sample of tissue (biopsy) from the bladder and the urethra for examination under a microscope. This is to check for bladder cancer and other rare causes of bladder pain.
Urine cytology
Your provider collects a urine sample and examines the cells to help rule out cancer.
Conclusion
This article highlights the complex interplay between IC and endometriosis in the context of CPP. It underscores the need for careful evaluation and simultaneous consideration of these conditions in patients with CPP. A multidisciplinary approach, including the use of PST and concurrent cystoscopy and laparoscopy, is crucial for accurate diagnosis and effective treatment of concurrent interstitial cystitis and endometriosis.

