
Top Endometriosis Specialist in New York—Find Expert Care Near You Today!
Table of Contents
- New York’s Endometriosis Experts: Hope in the City That Never Sleeps
- Endometriosis Symptoms Checklist
- Advanced Endometriosis Treatment in New York City
- Best Endometriosis Surgeons in New York City
- Endometriosis Treatment Options New York: As Diverse as New York Itself
- Fertility Preservation and Treatment
- Living with Endometriosis in New York: Endometriosis Support
- Empowering Your Endo Journey in the City of Dreams
New York’s Endometriosis Experts: Hope in the City That Never Sleeps
Endometriosis affects millions of women worldwide, causing debilitating pain and potential fertility issues. For those living in or near New York City, finding a top endometriosis specialist is crucial for proper diagnosis and treatment. This comprehensive guide will help you navigate the process of locating expert care, understanding treatment options, and taking control of your health.
Living with endometriosis can be challenging, but with the right medical team by your side, relief is possible. New York City is home to some of the world’s leading endometriosis experts, offering hope and healing to those struggling with this complex condition. Moreover, New York’s specialists combine the latest endometriosis research, treatment, and community resources. Whether you’re experiencing symptoms for the first time or seeking more effective management of long-standing issues, this article will equip you with the knowledge to find the best care available. Finding expert care is a big step toward reclaiming your quality of life!
Endometriosis Symptoms Checklist
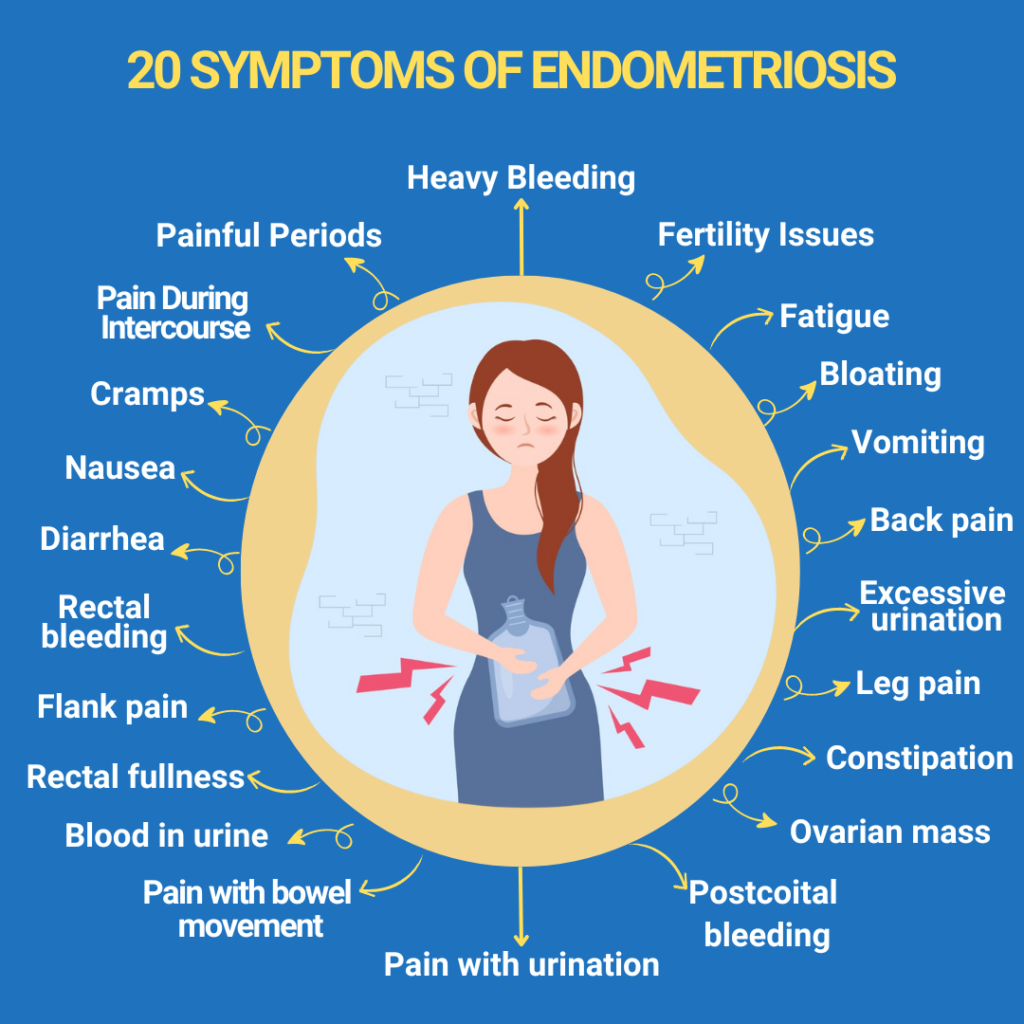
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus, often affecting the ovaries, fallopian tubes, and pelvic lining. This misplaced tissue responds to hormonal changes, leading to inflammation, pain, and potential scarring. The condition can have far-reaching effects on a woman’s quality of life, impacting everything from daily activities to intimate relationships and fertility.
Endometriosis Symptoms Checklist for Your Guidance:
- Heavy bleeding
- Fertility Issues
- Fatigue
- Bloating
- Vomiting
- Back pain
- Excessive urination
- Leg pain
- Constipation
- Ovarian mass
- Postcoital bleeding
- Pain with urination
- Pain with bowel movements
- Blood in urine
- Rectal fullness
- Flank pain
- Rectal bleeding
- Diarrhea
- Nausea
- Cramps
- Pain during intercourse
- Painful periods
It’s important to note that symptoms can vary widely between individuals, and some women may have few or no apparent symptoms despite having the condition. This variability makes accurate diagnosis crucial, highlighting the need for experienced specialists to recognize the subtle signs of endometriosis.
Advanced Endometriosis Treatment in New York City
New York City is recognized worldwide for its exceptional healthcare system, offering patients access to cutting-edge treatments and advanced research. This reputation for medical excellence is precious for those with complex conditions like endometriosis, who benefit from having a range of specialized care options nearby. In New York, renowned experts consistently push the boundaries of what’s possible in endometriosis treatment, often setting new standards for care. Patients here can access minimally invasive surgical options, advanced diagnostic imaging, and innovative pain management techniques that may not be widely available elsewhere.
Moreover, New York is home to many leading researchers actively working on understanding and treating endometriosis. For those impacted by endometriosis, this means better symptom management, faster recoveries, and potentially reduced recurrence rates. In addition, the collaborative environment among New York’s medical institutions allows for a holistic approach to patient care. Specialists, surgeons, pain management experts, and reproductive endocrinologists often work together to design individualized treatment plans.
Best Endometriosis Surgeons in New York City
New York City is home to numerous world-class specialists, making it an ideal location for those seeking expert endometriosis care. These surgeons often have extensive training in minimally invasive techniques, such as laparoscopic and robotic-assisted excision surgery, which can provide more effective symptom relief and lower recurrence rates than other methods. Leading surgeons also frequently collaborate with other specialists to offer comprehensive, individualized treatment plans tailored to each patient’s needs.
Among the best endometriosis surgeons in NYC are Dr. Andrea Vidali, Dr. Lora Liu, and Dr. Amanda Chu. They are known for their expertise and dedication to advancing care for patients with this complex condition. You can find more information about them and search for additional doctors in New York at iCareBetter. On this platform, you can find vetted top-notch doctors specializing in treating endometriosis and women’s pelvic pain worldwide.
Dr. Andrea Vidali

Dr. Andrea Vidali, a renowned endometriosis and reproductive immunology specialist, is celebrated for his minimally invasive excision surgery skills and personalized approach to fertility preservation. Through his comprehensive treatment plans, he has helped many women achieve successful pregnancies.
Dr. Lora Liu

Dr. Lora Liu is recognized for her precision in laparoscopic and robotic-assisted surgeries, providing endometriosis patients with effective and minimally invasive options to manage endometriosis. Her commitment to innovative techniques and compassionate approach to patient care make her a trusted figure in New York’s medical community. She is known for her collaborative, patient-centered methods, empowering individuals with endometriosis to reclaim their quality of life.
Dr. Amanda Chu, MD

Dr. Amanda Chu, MD, is a Board-Certified Gynecologic Surgeon specializing in minimally invasive techniques, particularly endometriosis excision surgery and treatment for pelvic endometriosis and fertility-related issues. Her expertise extends to multi-organ endometriosis and its impact on pain, fertility, and overall quality of life. Dr. Chu is dedicated to enhancing patient and provider education on endometriosis. Her focus areas include advanced robotic surgery, chronic pelvic pain management, and advanced hysteroscopy.
Endometriosis Treatment Options New York: As Diverse as New York Itself
Dr. Vidali is a Video-Vetted excision surgeon for endometriosis. His approach to endometriosis is holistic, addressing the disease and any potentially associated conditions. Currently, since we lack medical options for curing endometriosis, the primary treatment step is excision surgery. Additionally, Dr. Vidali utilizes hormonal contraception, preferably progestins—either orally or via IUDs—to manage bleeding or any adenomyosis-related factors, if present. He does not favor GnRH agonists or antagonists, as, in his experience, their risk and efficacy profiles are not superior to those of progestins, making them less desirable.
Dr. Liu, a Video-Vetted excision surgeon for endometriosis, believes that the etiology of endometriosis is complex and multifactorial, and she supports the Mullerianosis theory. However, other contributing factors also exist, including oxidative stress, inflammation, impaired immune response, genetics, and both endogenous and exogenous hormones, all of which play a role in the pathogenesis and proliferation of endometriosis.
Dr. Amanda Chu, a Video-Vetted excision surgeon for endometriosis, believes that the approach to endometriosis care is rooted in the understanding that no single theory thoroughly explains all cases of endometriosis. She believes that specific theories may apply more significantly to individual patients. While older concepts like retrograde menstruation and coelomic metaplasia remain valuable, Dr. Chu emphasizes the importance of ongoing research. She believes emerging insights into epigenetics and immune dysregulation will play a growing role in understanding and treating endometriosis.
Advanced Diagnostic Techniques
Accurate diagnosis is crucial for effective endometriosis treatment. Top specialists in New York utilize a range of advanced diagnostic techniques to identify and assess the extent of endometriosis, including:
- High-Resolution Imaging
Advanced imaging technologies, such as transvaginal ultrasound and MRI, can help visualize endometriotic lesions and assess the extent of the disease. These noninvasive methods are often used as initial screening tools.
- Laparoscopy
L laparoscopy is considered the gold standard for endometriosis diagnosis. It allows doctors to inspect the pelvic cavity for endometriosis tissue and samples visually. This minimally invasive surgical procedure can also remove lesions and adhesions.
- Biomarker Testing
Emerging research explores the use of blood and tissue biomarkers to aid endometriosis diagnosis. While yet to be widely available, some specialized centers may offer these cutting-edge tests as part of their diagnostic toolkit.
Innovative Treatment Approaches in New York
New York’s top endometriosis specialists offer a range of treatment options, from conservative management to advanced surgical techniques. Some of the innovative approaches available include:
- Minimally Invasive Excision Surgery
Laparoscopic and robotic surgeries are considered the gold standard for treating endometriosis. This technique involves carefully removing endometriotic lesions while preserving healthy tissue and organs. Skilled surgeons can often perform complex procedures using minimally invasive techniques, leading to faster recovery and less scarring.
- Robotic-Assisted Surgery
Some specialists use robotic-assisted surgical systems to enhance precision and control during endometriosis excision. This technology can be particularly beneficial for complex cases or when operating in difficult-to-reach areas.
- Hormone Therapy
Advanced hormone therapies, including newer progestin-only options, can help manage symptoms in some cases. Specialists can tailor hormone treatments to patients’ unique needs and medical history.
- Integrative Approaches
Many top endometriosis centers in New York offer integrative care options, combining traditional medical treatments with complementary therapies like acupuncture, pelvic floor physical therapy, and nutritional counseling to address the multifaceted nature of endometriosis.
Fertility Preservation and Treatment
For women with endometriosis who hope to conceive, fertility preservation and treatment are crucial considerations. New York’s leading endometriosis specialists often work closely with reproductive endocrinologists to offer:
- Fertility assessments and counseling
- Egg freezing and fertility preservation options
- Assisted reproductive technologies like IVF
- Surgical interventions to improve fertility outcomes
By addressing both endometriosis and fertility concerns simultaneously, these integrated approaches can help maximize a woman’s chances of achieving a successful pregnancy.
Living with Endometriosis in New York: Endometriosis Support
Living with endometriosis can be isolating, but connecting with others who understand your experience can be incredibly empowering. New York offers several support groups and advocacy organizations for endometriosis patients, including:
- Endometriosis Foundation of America
- NYC Endometriosis Support Group
Additionally, you can find valuable information and resources on the iCareBetter website. Our blog, forum, and published articles offer significant insights about endometriosis and its specialists.
To adapt to city life with Endo, try flexible commuting options, consider an anti-inflammatory diet (easy with NYC’s healthy food options), and focus on gentle exercise like yoga or walks in Central Park. These lifestyle adjustments and community resources can make managing endometriosis in the city more accessible.
Empowering Your Endo Journey in the City of Dreams
Finding a top endometriosis specialist in New York is crucial to reclaiming your health and quality of life. With access to world-class medical care, innovative treatments, and supportive communities, women with endometriosis have more options than ever before. By arming yourself with knowledge, seeking expert care, and advocating for your needs, you can take control of your endometriosis journey and work towards a future free from debilitating pain and limitations.
If you are struggling with endometriosis and seeking proper care, don’t navigate this journey alone! Visit iCareBetter to connect with top endometriosis specialists in New York who can provide personalized treatment options and support. Empower yourself with the knowledge and resources you need for better health—take the first step toward a brighter future today!
Remember, every woman’s experience with endometriosis is unique, and finding the right specialist may take time. Don’t be discouraged if your first appointment doesn’t provide all the answers—perseverance and self-advocacy are keys to finding the care you deserve. With the right team by your side, relief and healing are possible, opening the door to a brighter, pain-free future.
References:
https://www.dukehealth.org/treatments/obstetrics-and-gynecology/endometriosis-and-pelvic-pain

How to Become an Endometriosis Expert: Training Path
Table of contents
Due to the condition’s complexity and growing awareness, doctors who can diagnose and treat endometriosis are in high demand. To provide efficient patient care, doctors must complete advanced medical education and develop surgical expertise. These specialists need extensive training to handle this challenging condition.
Becoming an endometriosis specialist requires meeting strict standards. Experts must excel in advanced training courses and perfect their surgical techniques. They also need to keep up with new diagnostic methods and treatment options. This piece outlines the essential steps doctors should take to become recognized experts in endometriosis care.
Educational Requirements for Endometriosis Expertise
To become experts in endometriosis, specialists need extensive training and specialized education beyond standard qualifications. This helps practitioners become skilled at specific techniques and procedures.
Medical degree and gynecology specialization
Endometriosis expertise starts with medical school completion and obstetric gynecology specialization. Doctors need a complete understanding of reproductive medicine and pelvic health conditions. Not all gynecologists have advanced training to work with endometriosis, so specialists need extra intense training to manage it efficiently.
Advanced training in endometriosis diagnosis and treatment
Advanced training helps doctors become skilled in multiple aspects of endometriosis care. The complete training model has the following:
- Diagnostic imaging techniques and interpretation
- Surgical management of the disease
- Hormonal treatment protocols
- Pain management strategies
- Reproductive medicine expertise
- Psychosomatic medicine understanding
- Post-surgical treatment planning
Specialists must complete training at certified endometriosis centers. They work directly with patients and learn different treatment approaches. This specialized training prepares doctors to deliver complete care to their patients.
Surgical skills development
Surgical expertise is crucial for endometriosis specialists. Training programs must help doctors become skilled at laparoscopic or robotic excision of endometriosis. Surgeons need to develop proficiency in several specific techniques.
Advanced Surgical Skills:
- Surgical preparation by imaging studies
- Comprehensive assessment of the pelvic and abdominal organs during the surgery
- Removal of deep infiltrating endometriosis
- Parametrial dissection techniques
- Ureterolysis and ureteral procedures
- Rectal surgery techniques
- Nerve-sparing deep pelvic preparation
- Endometriomas
- Recto-vaginal septum endometriosis
Surgical training combines simulation-based learning with supervised practical experience. Specialists enhance their skills through workshops and specialized courses. At the end of their training, doctors must excel in minimally invasive surgical techniques for removing endometriosis lesions.
Critical Components of Endometriosis Training
Healthcare providers need training in specialized areas to become skilled at endometriosis care. These professionals must build their expertise in diagnostic and treatment approaches that work for better patient outcomes.
Diagnostic techniques (clinical examination, imaging, surgery)
Medical professionals need several examination methods to diagnose accurately. Laparoscopic visualization with histological confirmation remains the gold standard for diagnosis. Healthcare specialists should become skilled at the following:
- Transvaginal ultrasound (TVUS) – This method shows 93% sensitivity and 96% specificity when detecting endometriomas.
- Magnetic Resonance Imaging (MRI): This technique demonstrates 90-92% sensitivity and 91-98% specificity in identifying lesions.
- Laparoscopic examination – This procedure enables direct visualization and allows doctors to perform biopsies.
Medical management approaches
Medical management training emphasizes hormonal therapies and pain management protocols. Endometriosis specialists master several treatment options. Doctors must carefully monitor their patients’ responses and side effects.
Surgical techniques for different types of endometriosis
Surgical expertise includes procedures that doctors customize for each unique case. Doctors need to master both conservative and advanced surgical techniques. They must pay special attention to profoundly infiltrating endometriosis (DIE), which requires specialized surgical approaches.
Fertility preservation and reproductive medicine
Medical specialists need substantial training in fertility preservation because endometriosis affects a woman’s ability to conceive.
Completing required training
Doctors must complete specialized training at certified endometriosis centers to meet certification requirements. This training allows them to work with a variety of cases. The training process helps practitioners:
- Learn comprehensive surgical skills for removal of endometriosis lesions regardless of location and depth
- Become skilled at ultrasound techniques and interpretation
- Develop expertise in MRI interpretation
- Learn pain management protocols
- Study hormonal treatment options
Maintaining proficiency through continuing education
Ongoing Education Requirements: Medical and surgical proficiency just needs continuous professional development. Specialists must participate in educational activities to stay current with advancing medical knowledge. The continuing education process has:
- Participating in specialized workshops and masterclasses
- Attending professional conferences
- Engaging in clinical research
- Completing required continuing medical education (CME) credits
- Tracking certification maintenance through learning portals
Building Expertise Through Clinical Experience
Clinical experience is the lifeblood of expertise in endometriosis treatment. Medical professionals need hands-on practice and must learn continuously from all professional channels.
Working at specialized endometriosis centers
Specialized centers deliver complete care through teams of medical professionals. These teams include gynecologic surgeons, urologists, general surgeons, physical therapists, pain experts, fertility doctors, dietitians, and psychologists. Practitioners get unique opportunities to handle complex cases while working with experienced experts. Research shows that patient outcomes improve and complication rates decrease when surgeons perform endometriosis surgeries with a high volume of cases.
Attending conferences and workshops
Endometriosis experts enhance their expertise by participating in major international conferences. Key events include:
- AAGL annual conference
- World Congress on Endometriosis
- European Endometriosis Congress
- ESHRE Annual Meetings
- ASRM Annual Congress
These scientific gatherings offer insights into molecular fingerprints, complex surgery techniques, and emerging treatment approaches. Experts can find learning opportunities throughout the year at conferences worldwide.
Networking with other endometriosis specialists
Through these connections, specialists can:
- Share clinical experiences
- Work together on research projects
- Mentor younger members
- Promote high standards of ethical investigation
Conclusion
Doctors need thorough education, specialized training, and hands-on experience to become skilled at treating endometriosis. Their path requires expertise in advanced diagnostic techniques, surgical procedures, and medical management strategies. These specialists must show proficiency in multiple disciplines, from reproductive medicine to pain management, and stay updated with emerging treatment approaches.
Specialists can improve their endometriosis care through certification programs, clinical research, and professional networking. Time invested in specialized centers combined with participation in international conferences and professional networks helps doctors become pioneering experts in endometriosis treatment. This dedication benefits patient care through better diagnostic accuracy, improved treatment outcomes, and higher quality care for this complex condition.

Through the Looking Glass: Reflecting on 2023
Embarking on the journey of self-reflection is not just a personal endeavor; for us at iCareBetter, it’s a collective celebration of progress, community, and collaboration. As we bid farewell to 2023, a year marked by challenges and triumphs, it’s time to take a look into the past year and reflect on all that has been accomplished. Join us as we navigate through the areas of growth, community involvement, projects, and meaningful collaborations that shaped our year. In this special blog post, we’re excited to share the insights gained from our podcast endeavors and offer a sneak peek into the thrilling developments that await us in 2024. Let’s rewind, recap, and anticipate the exciting narrative that continues to unfold in the ever-evolving story of iCareBetter.
About iCareBetter
iCareBetter is an innovative platform dedicated to helping patients with endometriosis and chronic pelvic pain find compassionate and skilled experts. All experts on iCareBetter have shown knowledge and expertise in the treatment of endometriosis and chronic pelvic pain.
Vision
Our vision is to reduce the symptom-to-effective treatment of endometriosis to less than a year. Studies show that patients with endometriosis spend an average of 7.5 years to have an official diagnosis. Moreover, even after the diagnosis, patients will have to spend several years with multiple failed treatment attempts. After the long delays in diagnosis and treatment, they might be lucky enough to receive effective treatment from an expert.
Mission
Our mission is to improve access to high-quality specialized care for those with endometriosis. iCareBetter wants to combat the issue of patients living in confusion, pain, and isolation. To that end, we hope to connect as many patients to the right experts as early as possible. And we hope that this will ensure timely diagnosis and effective treatment.
To read more about why iCareBetter was built and the inspiration behind it, check out our blog here and listen to episode 1 of the podcast here, where Saeid and Jandra give you a behind the scenes look into what inspired them.
What happened in 2023?
In 2023, iCareBetter grew in many ways, including new avenues to provide education along with collaboration from the community. Here are some of the highlights!
- We started a podcast! iCareBetter: Endometriosis Unplugged is hosted by Jandra Mueller, DPT, MS a pelvic floor physical therapist and endometriosis patient. The podcast is available on Spotify, Apple Podcasts, and Youtube.
- We had 19 weekly episodes in season one
- Listeners joined from all over the world, reaching 22 countries
- We brought on a team to help with new content on social media creating a more visually appealing platform, community engagement, and followers.
- We now have 211 providers on our website available and ready to help those suffering from endometriosis and we are continuing to grow!
- Our blog content is now consistent with twice weekly posts bringing you updates on all things endometriosis.
What To Expect in 2024
While 2023 was a big year for iCareBetter, we hope to continue the growth and expand our providers across the globe. Our hope is to increase our collaboration with medical specialists, researchers, and advocates. There are some exciting things to come in 2024 including a new season of iCareBetter: Endometriosis Unplugged as well as some other projects that will be announced in 2024.
We hope you have found our resources helpful either for yourself or a loved one, and hope you continue to share the love and spread the word about Endometriosis. All of us here at iCareBetter wish you a safe and happy new year.

Cheers to 2024!
Do you or a loved one have Endometriosis? Here are some blogs that may help you get started on your journey.
- Endometriosis Signs and Symptoms: Everything You Need to Know
- Endometriosis Facts & Myths: Dispelling the Misconceptions

Women’s Health Research and the White House Initiative
Merry Christmas and Happy Holidays! It’s time for some good news when it comes to researching ‘women’s diseases.’
Women’s health has long been an area that has been overlooked and understudied in medical research. Despite making up more than half of the population, women have historically been underrepresented in clinical trials and medical studies, leading to significant gaps in knowledge and understanding of women’s health issues. However, recent developments, such as the establishment of the White House Initiative on Women’s Health Research, are changing the landscape and paving the way for a new era of research and innovation in women’s health.
Table of contents
The Historical Underrepresentation of Women in Research
For decades, women’s health needs were considered a low priority in the scientific and medical fields. During the 1970s, when the women’s health movement emerged as part of the larger women’s movement, it became apparent that women were significantly underrepresented in medical and scientific research. At that time, there were few women working in medicine and science, and the lack of representation had serious implications for the understanding and treatment of women’s health conditions.
One significant example of the cautious approach towards including women in research was the Food and Drug Administration’s policy in 1977, which recommended excluding women of childbearing potential from early-stage drug trials. This policy was a response to the tragic consequences of the drug thalidomide, which caused severe birth defects in thousands of babies born to women who had taken the drug during pregnancy. While the intention was to protect women from potential harm, it resulted in a lack of data on how drugs specifically affected women.
The Shift Towards Inclusion and Advocacy
As awareness grew about the exclusion of women from research studies, advocacy groups and activists began to protest for change. They argued that individual women should be allowed to make informed decisions about participating in research and that excluding women limited their access to potentially life-saving treatments. The Public Health Service Task Force on Women’s Health Issues, in their 1985 report, called for long-term research on how behavior, biology, and social factors affect women’s health, further highlighting the need for inclusion.
In response to these concerns, the National Institutes of Health (NIH) established a policy in 1986 that encouraged the inclusion of women in studies. This policy, published in the NIH Guide for Grants and Contracts in 1987, urged researchers to include women and minorities in their studies and provided guidelines for doing so. The policy was further reinforced in 1989 when NIH announced that research solicitations should prioritize the inclusion of women and minorities.
The Founding of the White House Initiative on Women’s Health Research
In 1990, the Congressional Caucus for Women’s Issues requested an investigation into NIH’s implementation of guidelines for the inclusion of women in research studies. The subsequent report by the General Accounting Office (now known as the Government Accountability Office) highlighted inconsistencies in applying the inclusion policy and the need for improved communication. As a result, the Office of Research on Women’s Health (ORWH) was established in 1991 to monitor and promote the inclusion of women in research.
Under the leadership of Dr. Bernadine Healy, the first female NIH Director, the Women’s Health Initiative was launched in 1991. This initiative consisted of clinical trials and an observational study involving over 150,000 postmenopausal women. The trials aimed to investigate the effects of hormone therapy but was stopped due to incorrect interpretation of the data resulting in the majority of women stopping their hormone therapy overnight, literally. We are still dealing with the consequences of this today.
Legislation and Policies to Ensure Inclusion
While the inclusion of women in research was initially an NIH policy, it became federal law in 1993 through the NIH Revitalization Act. This act included provisions requiring the inclusion of women and minorities in clinical research funded by NIH. The law mandated that NIH ensure the inclusion of women and minorities and that trials be designed to analyze whether variables affect women and minorities differently. It also emphasized that cost should not be a reason for exclusion and called for outreach efforts to recruit diverse populations for clinical studies.
Since the establishment of the ORWH, the office has monitored adherence to inclusion policies and guidelines. Researchers receiving NIH funding are required to report on the sex, race, and ethnicity of participants enrolled in clinical trials. These reports contribute to the ongoing efforts to promote inclusivity and address health disparities among different populations.
Improving Women’s Health Through Research
The White House Initiative on Women’s Health Research, announced by President Biden and led by First Lady Jill Biden, signifies a renewed commitment to advancing women’s health research. The initiative aims to galvanize the federal government, private sector, and philanthropic communities to close research gaps, address health disparities, and pioneer the next generation of discoveries in women’s health.
Under this initiative, concrete recommendations will be delivered to the Biden-Harris Administration within 45 days, outlining actions to improve research on women’s health and maximize investments in this field. Priority areas of focus will be identified to ensure transformative outcomes, ranging from heart attacks in women to menopause and beyond. The initiative also seeks to engage stakeholders from the scientific, private sector, and philanthropic communities to drive innovation and foster collaborative partnerships.
By prioritizing research on women’s health, we can gain a deeper understanding of conditions and diseases that predominantly affect women, such as endometriosis, cardiovascular disease, and Alzheimer’s disease. This knowledge will enable healthcare providers to better prevent, diagnose, and treat these conditions, ultimately improving the lives of millions of women.
The establishment of the White House Initiative on Women’s Health Research and the ongoing efforts to promote inclusion in medical research mark significant milestones in addressing the historical underrepresentation of women in studies. Through policies and legislation, initiatives like the Women’s Health Initiative, and the monitoring of adherence to inclusion guidelines, progress is being made to close research gaps and improve women’s health outcomes.
Research plays a crucial role in understanding the unique aspects of women’s health and developing effective treatments and interventions. By prioritizing and investing in research on women’s health, we can empower women, healthcare providers, and researchers to make informed decisions and advancements that will positively impact the health and well-being of women across the nation. The White House Initiative on Women’s Health Research is a vital step towards achieving this goal and creating a future where women’s health is fully understood, supported, and prioritized.
What you can do!
The Initiative is accepting written comments and input, we urge everyone to get involved.
You can send in either a word document or PDF file to WomensHealthResearch@who.eop.gov
Related reading:
- Endometriosis Signs and Symptoms: Everything You Need to Know
- Endometriosis Facts & Myths: Dispelling the Misconceptions
- Why was iCareBetter built?
References:
- https://www.whitehouse.gov/briefing-room/statements-releases/2023/11/13/fact-sheet-president-joe-biden-to-announce-first-ever-white-house-initiative-on-womens-health-research-an-effort-led-by-first-lady-jill-biden-and-the-white-house-gender-policy-council/
- https://www.whitehouse.gov/gpc/briefing-room/2023/11/17/launch-of-white-house-initiative-on-womens-health-research/
- https://www.whitehouse.gov/briefing-room/speeches-remarks/2023/11/13/remarks-by-president-biden-and-first-lady-jill-biden-establishing-the-first-ever-white-house-initiative-on-womens-health-research/
- https://orwh.od.nih.gov/toolkit/recruitment/history#:~:text=Inclusion%20Becomes%20Law&text=In%201993%2C%20Congress%20wrote%20the,as%20Subjects%20in%20Clinical%20Research.
Current Research in Endometriosis
Endometriosis affects roughly 190 million women and girls (assigned female at birth) worldwide. Despite its significant impact on the health of the individual due to both the disease and overlapping pain conditions, research funding for endometriosis lags behind other common diseases. However, we are starting to see small improvements. For example, in 2020, research funding by the NIH (National Institutes for Health) for endometriosis was 14 million dollars (US) and in 2022 nearly doubled at 27 million, and it is estimated for 2023 and 2024 to be approximately 29 million dollars.
The economic burden of endometriosis on the U.S. alone, in terms of medical care and lost productivity, is estimated to be around $78-120 billion annually. These figures underscore the urgent need for more research funding and better treatment options for endometriosis. Which is what we have been seeing more recently, research focused on other aspects of the disease and co-morbidities and not just drugs aimed at suppressing hormones.
Researchers have started to look more broadly and dive deeper into some areas that have only been superficially explored such as the impact of the microbiome and genetic studies. While the media has seemed overly excited about the findings and what this means now, this new research may be the stepping stones we need to better understand the variations of this disease and future treatments for managing endometriosis along with the overlapping symptoms.
This article aims at reviewing the new research in endometriosis.
Please note that this is a brief overview of some of the research, not opinions or endorsements from the iCareBetter team. More extensive research is needed in these areas before any conclusions can truly be drawn.
Here’s what researchers have been studying recently:
- Dichloroacetate. Researchers from the University of Edinburgh found that treatment with dichloroacetate reduced the size of endometriosis lesions and decreased lactate production, which has been associated with endometriosis manifestation in earlier studies.
- Cannabis. The Western Sydney University in Australia is investigating the potential benefits of medical cannabis for endometriosis treatment. The double-blind randomized controlled trial will evaluate whether medicinal cannabis can counter symptoms like pain caused by endometriosis against a placebo. This of course would not be focused on a treatment for endo, but as pain management.
- Immune system. It’s been recognized for many years that endometriosis and the immune system are intricately linked. Recent studies have found an overexpressed protein on endometriotic cells which may help drug development. Startup Fimmcyte is developing an antibody that labels endometriosis cells for clearance by the immune system, which could provide a much-needed non-hormonal therapy for women with endometriosis.
- Pelvic floor therapy. Studies have shown that pelvic floor therapy could be key to tackling endometriosis-induced pain, or identifying overlapping pain conditions. In addition to helping manage chronic pelvic pain, pelvic floor therapy has been effective in relieving pain through exercise, movements, and manual therapies that target the pelvic area. Read more about pelvic floor physical therapy from our recent blog here.
- Endometriosis and other inflammatory diseases. Recent research suggests that endometriosis may be linked to other inflammatory and pain-inducing diseases. A study by Celmatix and 23andMe, among others, found that endometriosis may be linked to 11 conditions, including migraine, back, and multisite chronic pain (MCP), and inflammatory conditions like asthma and osteoarthritis.
- Biotech and Endometriosis. Several ongoing studies aim to improve our understanding of endometriosis at the genetic level. The Research OutSmarts Endometriosis (ROSE) study is investigating the causes of endometriosis and aims to develop improved diagnostics and treatments for women with the condition.
Despite the challenges faced by researchers and patients alike, these recent developments in endometriosis research are a beacon of hope. As our understanding of this complex condition deepens, we edge closer to more effective treatments and perhaps, one day, a cure for endometriosis. One thing is certain though, endometriosis may be due to several factors which may need different targets. The expanding research into these topics may not seem relevant now, but may pave the way to better understanding of the variations of the disease, resulting in a wider array of therapies in addition to surgery for both treatment as well as symptom management.
Related Reading:
- Genetic Study On Patients With Confirmed or Suspected Endometriosis; Next Gen Jane
- Unraveling the Connection Between Endometriosis and Autoimmune Diseases
- The Hidden Connection Between Endometriosis and Systemic Lupus Erythematosus
- Genetics and Epigenetics of Endometriosis: Unraveling the Complex Web of Hereditary Implications
References:
- Endometriosis Clinical Trials – Mayo Clinic Research
- Giudice, L.C., Horne, A.W. & Missmer, S.A. Time for global health policy and research leaders to prioritize endometriosis. Nat Commun 14, 8028 (2023). https://doi.org/10.1038/s41467-023-43913-9

Your Guide to Supporting a Loved One Through the Holidays: The Ultimate Endometriosis Resource List Updated and Revised
Table of contents
The holiday season can be a joyous time filled with festivities, but for individuals navigating the challenges of endometriosis, it can also present unique hurdles. Supporting a loved one with endometriosis during this time involves not only empathy but also understanding the complexities of the disease. To aid both those directly affected and their support systems, a plethora of resources are available, ranging from insightful blogs and informative books to engaging movies and podcasts. These tools not only offer a wealth of knowledge about endometriosis but also provide a platform for individuals seeking a better understanding of the condition or those desiring to support their loved ones effectively.
In this guide, we will explore a curated selection of resources, offering both emotional support, educational insights, and even some ideas for your holiday shopping list to help individuals navigate the holiday season with a heightened awareness of endometriosis and a supportive approach to those impacted by this often misunderstood condition.
Understanding Endometriosis
For those of you unfamiliar with our blog, endometriosis is a chronic disease that primarily affects women (XX) of reproductive age. It involves the growth of endometrial-like tissue (the tissue that lines the inside of the uterus) outside of the uterus, leading to inflammation and pain, particularly during menstruation, though many other symptoms may be present.
For more information on symptoms of endometriosis, read our blog 20 Signs and Symptoms of Endometriosis.
Despite being a common condition, endometriosis is often misdiagnosed or overlooked, leading to many women suffering in silence. However, with the right information, supportive community, and access to informed medical providers, it is possible to manage the condition and lead a fulfilling life.
Podcasts on Endometriosis
Podcasts are an excellent way of gaining insights and information about endometriosis in a convenient and accessible format. Here are some podcasts that delve into various aspects of the disease, from personal stories to expert opinions:
- “iCareBetter: Endometriosis Unplugged”: Hosted by yours truly, is a video podcast (Spotify & Youtube) that focuses on expert interviews and patient stories with a few bonus episodes of specialists who treat conditions that often coexist with those with endometriosis. We have completed season 1 and hope to have season 2 coming in 2024!
- “In Sixteen Years of Endometriosis”: Hosted by two witty best friends who share their personal journey with the disease, this podcast offers a blend of humor, vulnerability, and accurate information.
- “The Cycle”: This podcast features stories of people living with endometriosis from around the world, providing practical ways to cope with the disease.
For more podcasts about endo, check out our previous blog here.
Books about Endometriosis
Reading about endometriosis can provide a comprehensive understanding of the disease. Here are some books written by medical experts and those living with the condition:
- “Beating Endo: How to Reclaim Your Life from Endometriosis”: Written by Iris Kerin Orbuch, MD, and Amy Stein, DPT, this book provides actionable insights into understanding and managing the disease.
- “Heal Endo”: By Katie Edmonds, (F)NTP provides a book that is patient focused with a more indepth understanding of the science balanced by actionable items that range from surgery to dietary and lifestyle changes.
- “The Endometriosis Health and Diet Program”: Authored by Dr. Andrew S. Cook, MD, FACOG, and Danielle Cook, MS, RD, CDE, this book focuses on treating endometriosis holistically, offering a comprehensive program tailored to individual needs.
- “Know Your Endo: An Empowering Guide to Health and Hope With Endometriosis”: Authored by Jessica Murnane, this book provides tools and strategies to manage chronic pain associated with endometriosis.
- “The Endo Patient’s Survival Guide: A Patient’s Guide to Endometriosis & Chronic Pelvic Pain”: This book by Andrew S. Cook, MD, FACOG, Libby Hopton, MS, and Danielle Cook, MS, RD, CDE, is a companion guide for patients, offering insights into diagnosis, treatment options, and achieving optimal relief.
Videos and Documentaries about Endometriosis
Visual content can help in understanding complex information about endometriosis. Several documentaries and movies have been produced to increase awareness about the disease.
- “Below the Belt”: A documentary from Shannon Cohn who created “Endo What?” focuses on the journey of several women seeking an endometriosis diagnosis and the challenges they face. “Below the belt” is not only an empowering film for educating the masses, it has become a tool for legislative change. A must see for everyone.
- “All about NINA”: A drama highlighting the experience of a woman, Nina Geld, managing her life with endometriosis.
- “Endo what?”: A documentary featuring women living with endometriosis and experts discussing treatment options.
- “The painful truth”: This film focuses on endometriosis and adenomyosis, another related condition.
- “A thousand needles”: A short documentary about the impact of endometriosis on a woman’s life.
- “End-o”: A short film showcasing the life of a young woman, Jaq, living with endometriosis.
- “The resilience of women in pain”: This short film focuses on Rose, a woman suffering from endometriosis and chronic illness, and her journey towards resilience.
Your Endo Shopping List: Comfort Tools for Loved Ones
In case you need to do some last minute shopping and want to show your loved ones you understand, here are some essential items that have proven useful for many. While these tools may not be able to stop this awful disease, they may provide some degree of comfort and relief when things get bad. Whether you are prepping for surgery, or just need some handy tools, here are some of my favorite items.
- Wedge Pillow. This is a must for those preparing for surgery during recovery. I only found this at my 3rd (and hopefully last) surgery and it was a game changer. When your belly is full of air, tender, and you don’t feel like moving (or sitting up at the very least), this helps to provide relief for recovering in bed or on the couch and is great if you are a side or back sleeper.
- Heating pads. This is probably the number one item most endo warriors have – likely at home and work. They are always handy to have wherever you are, and for a more personalized gift, ETSY.COM has some amazing endo swag (including heating pads).
- My Obi Apollo. This is a TENS unit with heat and multiple programs to help with cramps and reduce pain. To learn more about how TENS may be helpful, check out our blog here.
- Squatty Potty. Everyone should have one. This is the gift that no one really wants, but secretly is so happy when they get one. It is essential for optimal toileting for everyone, but especially if you have endometriosis. Constipation and pelvic floor dysfunction are two issues the majority of those with endometriosis suffer from and this tool can make a world of a difference for toileting….
Until recently, endometriosis was not a term most people were familiar with, unless you are suffering. It is amazing how this is shifting and so many more people are familiar with the term, but may not understand how impactful this disease is to one’s life. Finding the right surgeon is key to address the lesions, but having tools to help in the meantime is crucial. More importantly, your loved one will most appreciate the effort you made to educate yourself about their disease, especially during the stress the holidays may bring. Give them the gift of understanding and empathy this year, and maybe something to help their pain in the meantime.
Please note: We do not have financial affiliations with any of these products listed above.
Related Reading:
- Find an Endometriosis Specialist for Diagnosis, Treatment, & Surgery
- Endometriosis Facts & Myths: Dispelling the Misconceptions
- What You Need to Know About Endometriosis Excision Surgery
- Managing Endometriosis: What You Need to Know.

Preparing for the Holidays: Tips for Managing Flares
Table of contents
As the holiday season approaches, individuals grappling with endometriosis or other chronic illnesses are contemplating how to sidestep discomfort and flare-ups. Despite our concerted efforts to prevent or mitigate the frequency and intensity of flares associated with endometriosis, the truth remains that flare-ups are inevitable.
The holiday season holds the promise of joy, connections, and quality time with loved ones for many, but for others, it may bring stress, indulgence, worry, temptation, or even apprehension. The prospect of navigating gatherings, grappling with uncomfortable inquiries, or being compelled to make challenging food choices after diligently avoiding certain items for an extended period can be disheartening. Although flares may be an inherent part of the journey at any given time, holidays are no exception. The good news is that there are strategies available to effectively manage or minimize flares during these festive times!
Managing endometriosis or any chronic illness during the holiday season can present unique challenges, but there are strategies to help minimize flares and make the most of the festive season. Here are some tips:
Plan and Pace Yourself
- Plan your activities and commitments wisely. Don’t overcommit to events or tasks.
- Prioritize what’s most important to you and conserve your energy for those activities.
Communicate Openly
- Communicate with friends and family about your condition. Let them know your limitations and needs.
- Be open about your health concerns, so they can better understand and support you during gatherings.
- Or have a script of what you may want to say to those you do not want to share this information with such as: “Thank you for asking, though I’d prefer not to share those details right now, thank you for understanding.”
For a list of resources for yourself or others, check these out:
Choose Your Events
- Select events that align with your energy levels and health status.
- It’s okay to decline invitations or leave early if you’re not feeling well.
Mindful Eating
- Food is more than just its ingredients and nutrients, food is a major part of many of our cultures, enjoy it!
- Remember, stressing about trigger foods may be just as triggering as enjoying some of your favorite dishes.
- Consider bringing a dish that aligns with your dietary restrictions to ensure there’s something you can comfortably eat.
- Eat prior to going to events to avoid overindulging in foods that may be a trigger for your symptoms.
Rest and Relaxation
- Schedule breaks for rest and relaxation. Give yourself permission to step away from activities and take time for self-care.
- Incorporate relaxation techniques such as deep breathing or meditation to manage stress.
Create a Comfortable Space:
- If attending gatherings, find a comfortable spot to rest if needed.
- Consider bringing a cushion, heating pad, or any other items that provide comfort during flare-ups.
Be Kind to Yourself
- Understand that flares may still happen despite your best efforts. Be kind to yourself and acknowledge that it’s okay to take a step back when needed.
Stay Connected
- Stay connected with supportive friends or online communities. Sharing experiences and tips with others who understand what you’re going through can be comforting.
Use your toolbox!
- For many, you have gathered your individual tools that have worked well for you in the past, don’t forget about these!
- Connect with your providers, if you haven’t seen your providers in a while, it may be helpful to touch base with your mental health therapist, nutritionist, or physical therapist.
- Maybe you opt for that less intense workout to give your body a break.
Remember, everyone’s experience with endometriosis is unique, so tailor these tips to your specific needs and preferences. It’s essential to prioritize your well-being and enjoy the holiday season in a way that works best for you.
For more on this topic, check out our blog Managing Endometriosis: What You Need to Know.
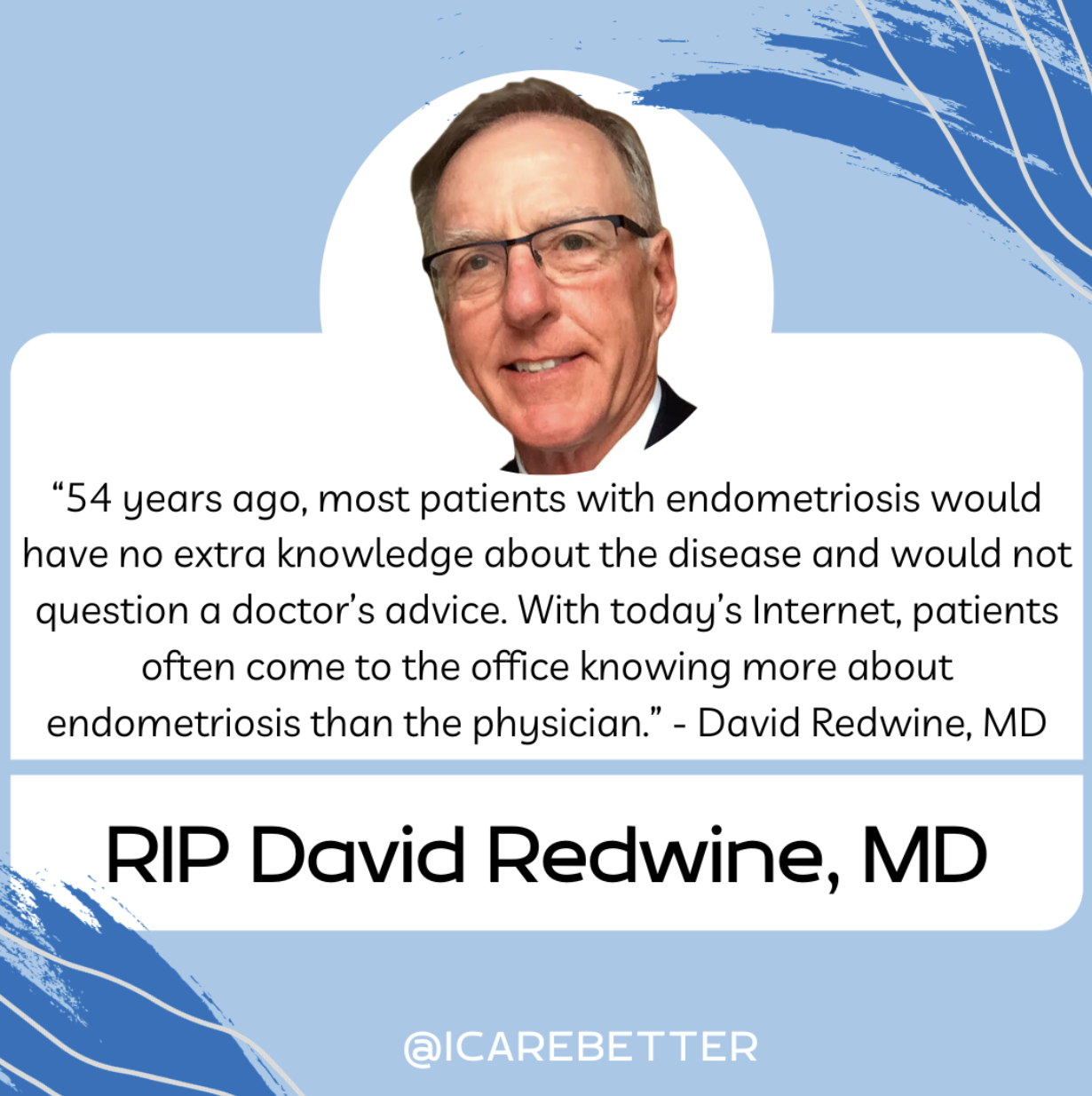
Dr. David Redwine Obituary : A Modern Hero in Endometriosis Research and Excision Surgery
The recent death of David Redwine has undoubtedly left many with sadness and devastation. Our thoughts are with his friends, family, colleagues, and the endometriosis community as a whole. The world of gynecology has been significantly influenced and transformed by the groundbreaking work of Dr. David Redwine, a significant contributor to those suffering from this disease. A modern hero in this community in his contributions to endometriosis research, excision surgery, and fighting alongside patients and advocating for better answers and better care. His innovative approaches and relentless pursuit of knowledge have positioned him as a leading advocate for patients with endometriosis, a debilitating condition that affects millions of women worldwide.
Table of contents
Who is David Redwine?
A formidable figure in the medical community, Dr. David Redwine has devoted his career to understanding and treating endometriosis. His profound commitment to research and patient care has made him a renowned authority in the field.
Redwine’s Contribution to the Understanding of Endometriosis
Endometriosis is a complex and often misunderstood condition. Dr. Redwine’s research has been instrumental in challenging established theories and introducing new perspectives on the origins and treatment of the disease.
Challenging Sampson’s Theory
One of the most significant contributions of Dr. Redwine has been his challenge to the widely accepted Sampson’s Theory of endometriosis. The theory, proposed by Dr. John Sampson in the 1920s, suggests that endometriosis is caused by retrograde menstruation, where menstrual blood containing endometrial cells flows back through the fallopian tubes and into the pelvic cavity. Redwine questioned the validity of this theory, arguing that if retrograde menstruation were indeed the cause of endometriosis, there should be ample microscopic evidence of refluxed endometrial cells attaching to the pelvic lining and subsequently proliferating. Yet, such evidence is conspicuously lacking. While modern day understanding by experts support alternative theories and are moving toward more plausible explanations, Dr. Redwine is largely to thank for this movement.
Proposing an Embryonic Origin
In place of Sampson’s Theory, Redwine proposed that endometriosis originates from an embryonic source. He argued that endometriosis is derived from mesoderm, the middle layer of the three embryonic layers, and is a result of abnormal differentiation and migration of cells during embryonic formation of the female reproductive tract. This theory suggests that endometriosis is a congenital condition that can manifest later in life under the influence of hormones and other factors.
The Concept of Mulleriosis
To further elucidate the embryonic origin of endometriosis, Redwine introduced the concept of ‘Mulleriosis.’ This term embraces a wider perspective, encompassing all pathologies associated with abnormal development of the Mullerian ducts, the precursor structures to the female reproductive organs.
Redwine’s Innovations in Endometriosis Surgery
Dr. Redwine has not only helped reshape our understanding of endometriosis but also revolutionized its treatment. He is a staunch advocate for excision surgery, a procedure that aims to completely remove endometriosis lesions. While early surgeries also focused on excision surgery, though lacking the precision and advanced technology we have today, the introduction of ablation surgery in the 70’s has complicated research findings, surgical outcomes, and the overall role of surgery in the treatment of this disease resulting in a further push towards hormonal suppression and the fight against Big Pharma.
The Importance of Excision Surgery
Whereas traditional first-line therapies often rely on hormonal therapy or less thorough surgical methods, Redwine emphasizes the importance of excision surgery in effectively treating endometriosis. Through extensive research and practice, he has demonstrated that excision surgery can significantly alleviate symptoms and improve the quality of life for patients with endometriosis.
The Concept of Cure
Contrary to the prevalent belief that endometriosis is incurable, Redwine insists that the disease can be effectively treated through excision surgery. He defines ‘cure’ as the complete absence of the disease, as proven by follow-up laparoscopy. While this topic may be nuanced to a degree and there are cases of regrowth, those of who have undergone a true excision surgery, and those that perform skilled excision surgery understand the difference of persistent pain vs. incomplete technique.
Redwine’s Advocacy for Patients with Endometriosis
In addition to his clinical and research work, Dr. David Redwine is a passionate advocate for patients with endometriosis. He strongly believes in empowering patients with knowledge about their condition and available treatment options.
Redwine is committed to educating both the medical community and the public about endometriosis. He regularly delivers lectures and presentations, sharing his insights and the latest research findings. His dedication to education aims to foster a more informed and empathetic understanding of endometriosis.
As a fervent advocate for patient-centered care, Redwine emphasizes the need to listen to patients’ experiences and concerns. He argues that an effective treatment approach should consider not only the physical manifestations of the disease but also its impact on a patient’s mental and emotional well-being.
You Will Be Missed!
Dr. David Redwine’s pioneering work in endometriosis research, excision surgery, and patient advocacy has had a profound impact on the understanding and treatment of the disease. His unwavering dedication to advancing knowledge and improving patient care serves as an inspiration for both medical professionals and patients alike. Dr. Redwine’s contributions will undoubtedly continue to shape the future of endometriosis care and research, despite his recent passing. His name will always be known in this community for the significant contributions he has made and the patients whom he has helped whether directly, or indirectly.
Rest in peace Dr. Redwine, you will be missed.
Endometriosis and the Microbiome: Insights and Emerging Research
Table of contents
- Understanding Endometriosis
- The Human Microbiome and Its Role in Health and Disease
- The Microbiome-Endometriosis Connection: An Emerging Field of Research
- Microbiome and the Inflammatory Response in Endometriosis
- The Gut Microbiome and Estrogen Levels
- The Microbiome as a Diagnostic and Therapeutic Target
- Conclusion
Endometriosis is a multifaceted, heterogenous, inflammatory condition that impacts 10%-15% of women (XX) in their reproductive years, most commonly associated with chronic pelvic pain and infertility.
Over the years, numerous theories have been proposed to explain its pathogenesis, but none have conclusively clarified its origins. Recently, however, researchers have begun investigating the complex interplay between endometriosis and the human microbiome. This article aims to provide an in-depth exploration of the current research into the relationship between endometriosis and the microbiome, with a particular focus on gut health, inflammation, and pathogenesis.
Understanding Endometriosis
Endometriosis is marked by the growth of endometrial-like tissue found outside of the uterine cavity. This tissue is commonly found implanted over visceral and peritoneal surfaces within the abdominopelvic cavity, but can extend to the connective tissue and organs throughout the body. The condition can lead to severe dysmenorrhea, pelvic pain, and subfertility among a number of other symptoms and manifestations, significantly impairing a person’s quality of life.4
Read more: What causes endometriosis?
The Human Microbiome and Its Role in Health and Disease
The human microbiome comprises microorganisms that colonize our bodies and play crucial roles in nutrient metabolism and various physiological functions. The composition and balance of these microbial communities can significantly influence our health. For instance, the gut microbiota synthesizes vitamins B12 and K, maintains intestinal mucosal integrity, promotes angiogenesis and epithelial repair, and modulates immune functions.5
Disruptions in gut microbiota composition, a state known as dysbiosis, can contribute to the development and progression of numerous diseases, including inflammatory bowel diseases, arthritis, psoriasis, neuropsychiatric diseases, and even malignancies.4 Given that endometriosis is a chronic inflammatory disease potentially triggered by altered immune functions and increased angiogenesis, there is a growing interest in investigating the role of microbiota dysbiosis in the pathogenesis and pathophysiology of endometriosis.1,4
The Microbiome-Endometriosis Connection: An Emerging Field of Research
Recent studies have commenced exploring whether microbiome composition is altered in women with endometriosis. For instance, one study identified significant differences in the microbial community structure between those with and without endometriosis.1,5 This study found that the abundance of Acinetobacter, Pseudomonas, Streptococcus, and Enhydrobacter significantly increased, while the abundance of Propionibacterium, Actinomyces, and Rothia significantly decreased in the endometriosis group.5
Another study focused on the microbiota of extracellular vesicles in the peritoneal fluid.4,5 These vesicles, small structures made of bilayered lipid membranes released by cells, carry proteins, nucleic acids, and lipids, and play a key role in immune function, inflammatory reactions, and disease development. Like other cells, bacteria can release extracellular vesicles that modulate host-cell immune responses and other health conditions. The study found significant differences in the microbial community of these vesicles between women with and without endometriosis.5
Highlighting the complex relationship between the microbiome and endometriosis, several studies have shown an increased bacterial colonization of menstrual blood and endometrial tissue in women with endometriosis compared to control subjects.5 A study on rhesus monkeys demonstrated that altered composition of the intestinal microflora and intestinal inflammation are associated with endometriosis. While we know animal comparison is not exactly like humans, the reproductive tract of rhesus monkeys closely resembles humans in both the form and function.7
Read more: Endo-Fighting Microbiome Optimization: Research-based Tips
Microbiome and the Inflammatory Response in Endometriosis
Endometriosis is known to trigger an inflammatory response within the body, characterized by increased production of pro-inflammatory cytokines, autoantibodies, growth factors, oxidative stress, and alterations in T-cell and natural killer cell reactivity.1 This dysregulated immune response potentially creates an immunosuppressive environment that enables the growth of these endometriosis lesions.1
Recent studies suggest that gut microbiome-derived extracellular vesicles could play a critical role in this process.5 These vesicles, ranging from 20 to 400 nm in diameter, can traverse the intestinal barrier, enter the systemic circulation, and potentially influence the peritoneal environment. They may carry a cargo of proteins, nucleic acids, and lipids that can influence immune function, inflammatory responses, and the development of diseases like endometriosis.
One study demonstrated that extracellular vesicles from women with endometriosis carry unique cargo that can influence inflammation, angiogenesis, and proliferation.5 Another study identified specific proteins in the exosomes of peritoneal fluid samples from patients with endometriosis, suggesting a role of exosomes in the diagnosis and treatment of endometriosis.5
The Gut Microbiome and Estrogen Levels
The gut microbiome is a significant regulator of estrogen levels, influencing estrogen metabolism and hence potentially affecting estrogen-dependent diseases like endometriosis.3 In postmenopausal women, fecal microbiota richness and levels of fecal Clostridia taxa have been associated with systemic estrogen levels. Therefore, gut dysbiosis leading to abnormal circulating levels of estrogen could potentially play a role in the development of endometriosis or the associated symptoms.3
The Microbiome as a Diagnostic and Therapeutic Target
The alterations in microbiota composition associated with endometriosis may provide valuable diagnostic markers for the disease. For instance, one study has proposed a microbiota-based model that can distinguish infertile patients with and without endometriosis.1 Another study has found that specific bacterial species are enriched in the endometrium and peritoneal fluid of patients with endometriosis.2
On the therapeutic front, the modulation of gut microbiota through dietary interventions, prebiotics, probiotics, or fecal microbiota transplantation could potentially represent a novel treatment approach for endometriosis.4 However, more research is needed to explore the potential of these strategies and to understand the precise mechanisms through which the microbiota influences endometriosis development and progression.
Read More: Integrative Therapies for Endometriosis
Conclusion
The complex relationship between the microbiome and endometriosis is still in its early stages of investigation. Recent studies indicate that alterations in microbiota composition may be associated with endometriosis. These insights not only enhance our understanding of endometriosis pathogenesis but also open up new possibilities for the diagnosis and treatment of this prevalent condition.
As our understanding of the microbiome continues to grow, so does the potential for novel, integrative health strategies that target this complex ecosystem. Further research is required to confirm the observed associations and to elucidate the mechanisms underlying the microbiome-endometriosis connection. Such research holds the promise of ushering in a new era in our approach to endometriosis, one that acknowledges the intricate interplay between our bodies and the microbes that inhabit them.
While there are limitations in the current usefulness of this research, we do know that the immune system is involved with regulating the disease. An important question remains: are the microbiota changes seen in those with endo the chicken or the egg?
References:
- Leonardi, M., Hicks, C., El-Assaad, F., El-Omar, E., & Condous, G. (2020). Endometriosis and the microbiome: a systematic review. BJOG, 127(2), 239-249. https://doi.org/10.1111/1471-0528.15916
- Oishi, S., Mekaru, K., Tanaka, S. E., Arai, W., Ashikawa, K., Sakuraba, Y., Nishioka, M., Nakamura, R., Miyagi, M., Akamine, K., & Aoki, Y. (2022). Microbiome analysis in women with endometriosis: Does a microbiome exist in peritoneal fluid and ovarian cystic fluid? Reprod Med Biol, 21(1), e12441. https://doi.org/10.1002/rmb2.12441
- Svensson, A., Brunkwall, L., Roth, B., Orho-Melander, M., & Ohlsson, B. (2021). Associations Between Endometriosis and Gut Microbiota. Reprod Sci, 28(8), 2367-2377. https://doi.org/10.1007/s43032-021-00506-5
- Jiang, I., Yong, P. J., Allaire, C., & Bedaiwy, M. A. (2021). Intricate Connections between the Microbiota and Endometriosis. Int J Mol Sci, 22(11). https://doi.org/10.3390/ijms22115644
- Lee, S. R., Lee, J. C., Kim, S. H., Oh, Y. S., Chae, H. D., Seo, H., Kang, C. S., & Shin, T. S. (2021). Altered Composition of Microbiota in Women with Ovarian Endometrioma: Microbiome Analyses of Extracellular Vesicles in the Peritoneal Fluid. Int J Mol Sci, 22(9). https://doi.org/10.3390/ijms22094608
- Wei, W., Zhang, X., Tang, H., Zeng, L., & Wu, R. (2020). Microbiota composition and distribution along the female reproductive tract of women with endometriosis. Ann Clin Microbiol Antimicrob, 19(1), 15. https://doi.org/10.1186/s12941-020-00356-0
- Burns, K. A., Pearson, A. M., Slack, J. L., Por, E. D., Scribner, A. N., Eti, N. A., & Burney, R. O. (2021). Endometriosis in the Mouse: Challenges and Progress Toward a ‘Best Fit’ Murine Model. Front Physiol, 12, 806574. https://doi.org/10.3389/fphys.2021.806574

Endo-Fighting Microbiome Optimization: Research-based Tips
Table of contents
Endometriosis is partly caused by, and causes, inflammation. The origin or genesis of this
inflammation is probably multifactorial but recent research suggests that the microbiome, the
community of microorganisms living in or on the human body, plays an important role through
inflammatory pathways. Dysbiosis, which means an imbalance or impairment of the microbiota,
is observed in endometriosis, and is thought to both contribute to and result from endo.
Studies have focused on the gut, peritoneal fluid, and female reproductive tract microbiota to
identify specific microbiome signatures associated with endometriosis. The gut microbiome, in
particular, has been extensively studied. Changes in bacterial composition, such as increased
levels of Proteobacteria and decreased levels of Lactobacilli, have been observed in the gut of
endometriosis patients. Other body sites, including the peritoneal fluid and female reproductive
tract, also show altered microbiota in endometriosis.
The dysbiosis observed in endometriosis is believed to contribute to the disease through
various mechanisms. One theory suggests that bacterial contamination, particularly with
Escherichia coli, in the menstrual blood may lead to inflammation and immune activation in the
peritoneal cavity, contributing to endometriosis development. Dysbiosis can also affect
estrogen metabolism, through dysfunction of the so called “estrobolome”. This can lead to
increased levels of circulating estrogen and a hyper-estrogenic state, which promotes
endometriosis. Additionally, dysbiosis-induced epigenetic changes and immune modulation
may play a role in direct endometriosis pathogenesis.
Research on the microbiome in endometriosis is still in its early stages, but it holds promise for
potential diagnostic and therapeutic approaches. Microbiome testing could potentially be used
as a non-invasive tool for detecting endometriosis, complementing current imaging modalities.
The technology for doing this is already here and you can get it ordered. However, the meaning
of the results is still not well understood in any given individual. So, it’s complicated.
Beyond testing, manipulating the microbiome through interventions like probiotics, antibiotics,
or dietary modifications may offer new treatment options for endometriosis. To the extent that
you can diversify your microbiome and get it to a healthier state, this is something that can be
done with little risk or cost today. Options available to you are covered below, most of which
are focused on the bacterial part of your microbiome.
Future studies will explore the role of different types of microorganisms, beyond bacteria, such
as viruses and fungi, and utilize advanced analytical methods like shotgun metagenomics and
metabolomics to gain a more comprehensive understanding of the microbiome in
endometriosis. Newer technologies like this are significantly accelerating gains in knowledge.
Meanwhile, emerging understanding of the bidirectional relationship between endometriosis
and the microbiome has implications for potential treatment strategies available today.
Antibiotics
Antibiotics could be used to target specific bacteria associated with dysbiosis in
endometriosis, especially if you are diagnosed with small intestinal bacterial overgrowth (SIBO).
Animal studies have shown that treatment with antibiotics can reduce the size of endometriotic
lesions and associated inflammation. In humans, we know that chronic endometritis (infection
of the uterine cavity) seems to play a role in development of endo. However, this requires
expert guidance. It’s critical to exercise caution with antibiotic use to avoid disrupting healthy
commensal (good bacteria) microbiota and contributing to antimicrobial resistance. You don’t
want to grow a bug that might be resistant to multiple antibiotics down the line.
Probiotics
Probiotics are live bacteria that can have beneficial effects on your microbiome
health and diversity when consumed. Studies in animal models have demonstrated that certain
probiotic strains, such as Lactobacillus gasseri, can suppress the development and growth of
endometriotic lesions. Probiotics may modulate the immune response and restore a healthier
microbiota composition, potentially mitigating the inflammatory processes associated with
endometriosis. However, again, this requires expert guidance because, for example, it could
lead to ineffectiveness against or exacerbation of SIBO. This is partly because there are at least
three different general types of SIBO, based on what type of gas is produced by the
microbiome.
Prebiotics
Prebiotics are basically food substances that selectively promote the growth of
beneficial bacteria in the gut. By providing a favorable environment for beneficial bacteria,
prebiotics can help restore a healthy microbiota balance. An example of a prebiotic shown to
be beneficial in SIBO treatment is partially hydrolyzed guar gum (PHGG). Further research is
needed to investigate the potential roles of prebiotics in endometriosis treatment, but it could
be a gamechanger for simple treatment of various intestinal disorders, leaky gut and so on.
Dietary Modifications
Diet can hugely influence the composition and activity of the
microbiome. Consuming a diet rich in fiber and plant-based foods, which are known to support
a diverse and healthy microbiota, may have beneficial effects on endometriosis. Low FODMAPs
diets, which restrict fermentable carbs, can help. Omega-3 polyunsaturated fatty acids (PUFAs),
found in fatty fish, flaxseeds, and chia seeds, have shown anti-inflammatory properties and
have been associated with a lower incidence of endometriosis. Incorporating these dietary
changes, among many others, may help modulate the microbiome and reduce inflammation.
Immunomodulation
The microbiome has profound effects on the immune system, and
targeting the immune response could be a potential avenue for endometriosis treatment.
Modulating the immune system through therapies such as immune-suppressing medications or
immune-modulating agents may help regulate the inflammatory processes associated with
endometriosis. The idea here is to keep it as natural as possible, but sometimes prescription
medications may turn out to be necessary.
Please keep in mind that these treatment implications are based on current research, primarily
in the lab and animal models, and further studies are needed to validate their effectiveness and
safety in humans. Additionally, personalized approaches considering an individual’s specific
microbiota composition and disease characteristics may be necessary for optimal treatment
outcomes. It is exciting research in development and will be part of upcoming revolutionary
advances which take us far beyond hormonal manipulation for endo management. Since these
approaches are exploring the root cause of endo, treatments will likely be therapeutic as
opposed to simply something that reduces symptoms, which is the case with today’s hormonal
therapies.
The best part is that with proper expert guidance, much of the above can be used today
because, in most cases, the risk and cost are relatively low.
References:
Uzuner, C., Mak, J., El-Assaad, F., & Condous, G. (2023). The bidirectional relationship between
endometriosis and microbiome. Frontiers in Endocrinology, 14, 1110824. doi:
10.3389/fendo.2023.1110824
Moreno, I., Franasiak, J. M., & Endometrial Microbiome Consortium. (2020). Endometrial
microbiota—new player in town. Fertility and Sterility, 113(2), 303-304. doi:
10.1016/j.fertnstert.2019.10.031

Managing Stress with Endometriosis: A Guide for Patients
Endometriosis is a chronic condition that affects approximately 10% of women between 15-50 and other genders. This condition is characterized by the growth of tissue similar to endometrium outside of the uterus, leading to painful menstrual cramps, heavy bleeding, and infertility. Living with endometriosis can be extremely challenging due to its physical and emotional toll on an individual. Stress can exacerbate symptoms of endometriosis and make coping with the condition even more difficult. In this blog post, we will discuss the effects of stress on endometriosis and provide some tips on managing stress for individuals with this condition.
Stress is a common issue that affects patients with endometriosis. When you experience stress, your body releases the hormone cortisol, which can trigger inflammation and potentially exacerbate endometriosis symptoms. Stress also affects our immune system, making fighting diseases and infections harder for our bodies. To help manage stress, it’s essential to develop healthy coping mechanisms. Some practical techniques include meditation, yoga, deep breathing, or guided imagery.
Exercise is another effective way to manage stress and improve endometriosis symptoms. Physical activity has been shown to release endorphins, which are natural painkillers, and reduce inflammation. However, it’s essential to be cautious when exercising if you have endometriosis. High-impact activities like running or jumping can trigger pain and discomfort. Instead, try low-impact exercises like swimming, walking, or cycling.
It’s also essential to pay attention to what you eat when managing endometriosis and stress. A diet rich in anti-inflammatory foods can help reduce inflammation and improve endometriosis symptoms. Include foods like leafy greens, berries, fatty fish, and nuts in your diet to provide your body with the necessary nutrients. Avoid caffeine, sugar, and processed foods that can exacerbate inflammation and trigger hormonal imbalances.
Getting enough sleep is also essential for managing stress and endometriosis. Lack of sleep can lead to fatigue, mood swings, and anxiety. Try to establish a regular sleep schedule and avoid using electronic devices before bed, as they can disrupt your sleep pattern. Creating a relaxing bedtime routine, like taking a warm bath or reading a book in bed, can help promote a peaceful sleep environment and reduce stress.
Finally, seeking support from others can help alleviate stress and improve endometriosis symptoms. Talking to a therapist can provide you with tools to manage stress and emotional challenges. Joining a support group or online community can also help you connect with other people who experience similar challenges and find comfort in sharing experiences.
Living with endometriosis can be challenging, but managing stress can help alleviate symptoms and improve the overall quality of life. Incorporating healthy habits like exercise, a nutritious diet, and stress-reducing activities into your everyday routine can reduce anxiety and inflammation and promote physical and emotional wellness. Remember that you are not alone in this journey, and seeking support from others can help alleviate stress and provide you with the necessary tools to manage endometriosis.
Read more: Managing Endometriosis
The Importance of Endometriosis Awareness Month
Table of contents
Every March, the world comes together to recognize and raise awareness for endometriosis. This global health issue affects hundreds of millions of humans worldwide yet is rarely discussed due to a lack of education and knowledge. Endometriosis Awareness Month allows us to learn more about this debilitating condition and how it impacts those who suffer from it.
What is Endometriosis
Endometriosis is a chronic disorder affecting up to 10% of women worldwide. Endometriosis can impact other genders as well. This disease occurs when tissue similar to the lining of the uterus grows outside the uterus and on other organs in the body, such as the ovaries, bladder, bowels, and abdomen. While endometriosis can occur at any age, it most commonly impacts women between 15-50 years old.
Common Symptoms
The most common symptom of endometriosis is pelvic pain. This pain can range from mild cramping or discomfort to severe period pain lasting days or weeks. Other symptoms include heavy periods (with large clots), painful bowel movements or urination during menstrual cycles, painful sex, fatigue, and infertility. Unfortunately, these symptoms are often misdiagnosed as menstrual cramps or irritable bowel syndrome (IBS).
Endometriosis Treatment Options and Management Strategies
Endometriosis cannot be cured, but treatment options are available to help manage its symptoms. These include surgical removal of endometrial growths, hormone therapy, pain management, and dietary changes. Additionally, lifestyle modifications like stress reduction techniques and exercise can help alleviate some symptoms of endometriosis.
Endometriosis Awareness Month is important in educating everyone about this chronic disorder that affects hundreds of millions globally. We must learn more about endometriosis so that those suffering from this condition can get the proper diagnosis and care they need. Together we can make a difference in raising awareness for this disease!

