
The Definitive Guide: Finding the Right Pelvic Pain Doctor
Persistent, unrelenting pelvic pain can be an agonizing and debilitating experience, significantly impacting one’s quality of life. However, navigating the intricate landscape of healthcare providers and specialists can be daunting, especially when seeking relief from this complex condition. This comprehensive guide aims to shed light on the various specialists equipped to address pelvic pain, empowering individuals to make informed decisions and receive the care they deserve.
Table of contents
Understanding Pelvic Pain: A Multifaceted Condition
Pelvic pain is a broad term encompassing discomfort or aching sensations within the lower abdominal region, extending from the navel down to the pubic area. This condition can manifest in various forms, ranging from acute, short-lived episodes to chronic, persistent pain lasting six months or longer. The underlying causes of pelvic pain are diverse, often stemming from an intricate interplay between the reproductive, digestive, urinary, and musculoskeletal systems.
Exploring the Spectrum of Pelvic Pain Specialists
When it comes to addressing pelvic pain, a multidisciplinary approach is often required, involving collaboration among various medical professionals. Each specialist brings unique expertise and perspectives, tailoring treatment plans to the specific needs of the individual.
1. Gynecologists: Guardians of Reproductive Health
Gynecologists are medical doctors specializing in the diagnosis and treatment of conditions affecting the female reproductive system. These professionals are well-versed in addressing pelvic pain stemming from conditions such as endometriosis, ovarian cysts, uterine fibroids, and pelvic inflammatory disease (PID). While gynecologists can provide valuable insights and treatment options, they may not be equipped to handle complex or chronic cases of pelvic pain that extend beyond the reproductive system.
2. Urologists: Experts in Urinary and Male Reproductive Health
Urologists are medical specialists dedicated to the diagnosis and treatment of conditions related to the urinary tract and male reproductive system. For individuals experiencing pelvic pain associated with conditions like interstitial cystitis, chronic prostatitis, or urinary tract infections, a urologist’s expertise can be invaluable. Additionally, urologists play a crucial role in addressing pelvic pain in men, an often overlooked aspect of this condition.
3. Gastroenterologists: Navigating Digestive System Disorders
The digestive system can be a significant contributor to pelvic pain, with conditions like irritable bowel syndrome (IBS), diverticulitis, and inflammatory bowel diseases (IBD) frequently manifesting as lower abdominal discomfort. Gastroenterologists, specialists in the diagnosis and treatment of digestive system disorders, can be instrumental in identifying and managing pelvic pain originating from the gastrointestinal tract.
4. Pelvic Pain Specialists: The Comprehensive Approach
While the aforementioned specialists offer valuable insights and expertise within their respective domains, individuals suffering from chronic or complex pelvic pain may benefit from the comprehensive care provided by a pelvic pain specialist. These medical professionals have undergone extensive training in diagnosing and treating a wide range of pelvic pain conditions, taking a holistic approach that considers the intricate interplay between various bodily systems.
Pelvic pain specialists are uniquely equipped to address conditions such as vulvodynia, pudendal neuralgia, hypertonic pelvic floor dysfunction, and persistent genital arousal disorder (PGAD). They employ a multidisciplinary approach, collaborating with other specialists, physical therapists, and mental health professionals to develop personalized treatment plans tailored to each individual’s needs.
Factors to Consider When Choosing a Pelvic Pain Doctor
When seeking medical care for pelvic pain, it is crucial to consider several factors to ensure a positive and effective experience.
1. Expertise and Experience
Evaluate the doctor’s level of expertise and experience in treating pelvic pain conditions. Inquire about their training, certifications, and the number of patients they have treated with similar conditions. Experienced pelvic pain doctors often have a deeper understanding of the complexities involved and may be better equipped to provide comprehensive care.
2. Bedside Manner and Communication
A compassionate and attentive bedside manner can significantly impact the patient-doctor relationship and the overall treatment experience. Look for a pelvic pain doctor who actively listens to your concerns, provides clear explanations, and fosters an environment of trust and open communication.
3. Treatment Approach
Inquire about the doctor’s treatment philosophy and approach to managing pelvic pain. Some may favor a more conservative approach, starting with lifestyle modifications and medications, while others may recommend interventional procedures or surgery when appropriate. Ensure that the doctor’s treatment approach aligns with your preferences and values.
4. Accessibility and Convenience
Consider the doctor’s office location, hours of operation, and availability for appointments. If you require frequent visits or have mobility limitations, choosing a conveniently located practice can make a significant difference in your overall experience.
5. Insurance Coverage and Costs
Before committing to a particular doctor or treatment plan, verify your insurance coverage and understand the associated costs. Inquire about the practice’s billing policies, out-of-pocket expenses, and any available financial assistance programs to ensure that the treatment is accessible and affordable.
Finding the Right Pelvic Pain Doctor Near You
With the abundance of healthcare providers and specialists available, finding the right pelvic pain doctor in your area can be a daunting task. Fortunately, several resources can aid in your search:
- Referrals from Primary Care Physicians: Your primary care physician or gynecologist may be able to provide recommendations for reputable pelvic pain specialists in your area.
- Online Directories and Reviews: Utilize online directories and review platforms to research pelvic pain doctors in your vicinity. Read patient reviews and ratings to gain insights into the doctor’s expertise, bedside manners, and overall patient satisfaction.
- Hospital and Medical Center Websites: Many hospitals and medical centers have dedicated sections on their websites featuring profiles of their physicians, including pelvic pain specialists. These profiles often provide information about the doctor’s qualifications, areas of expertise, and contact information.
- Professional Organizations: Organizations such as the International Pelvic Pain Society (IPPS), the International Society for the Study of Sexual Health (ISSWSH), and the American Urogynecologic Society (AUGS) maintain directories of pelvic pain specialists, which can be a valuable resource in your search.
- Support Groups and Online Communities: Connecting with others who have experienced pelvic pain can provide invaluable insights and recommendations for finding the right doctor. Participate in online support groups or local community organizations to tap into this collective knowledge.
Remember, finding the right pelvic pain doctor may require patience and perseverance. Don’t hesitate to seek second or third opinions until you find a healthcare provider who understands your needs and with whom you feel comfortable.
Preparing for Your Appointment: Empowering Yourself
Once you have identified a potential pelvic pain doctor, it is essential to prepare for your appointment to ensure a productive and informative consultation. Here are some tips to help you get the most out of your visit:
- Keep a Detailed Pain Journal: Document your pelvic pain experiences, including the location, intensity, duration, and any potential triggers or alleviating factors. This information can provide valuable insights to your doctor and aid in accurate diagnosis and treatment planning.
- Compile Medical Records: Gather all relevant medical records, including test results, imaging scans, and previous treatments or medications. Providing your doctor with a comprehensive medical history can facilitate a more informed assessment.
- Prepare a List of Questions: Write down any questions or concerns you may have regarding your condition, treatment options, potential side effects, or lifestyle modifications. An open and honest dialogue with your doctor can lead to a better understanding and more effective treatment plans.
- Consider Bringing a Support Person: Having a trusted friend or family member accompany you to your appointment can provide emotional support and an additional set of ears to help you remember important details discussed during the consultation.
- Be Open and Honest: Pelvic pain can be a sensitive and personal topic, but it is crucial to be open and honest with your doctor about your symptoms, concerns, and any relevant personal or medical history. This transparency can help your doctor provide the most appropriate and effective care.
Conclusion: Embracing a Collaborative Journey
Navigating the complexities of pelvic pain can be a challenging and often frustrating experience. However, by understanding the various specialists available and their areas of expertise, you can take an active role in your healthcare journey. Remember, finding the right pelvic pain doctor may require patience and perseverance, but the rewards of receiving personalized, comprehensive care and relief from your symptoms are invaluable.
Embrace a collaborative approach with your healthcare provider, actively participate in your treatment plan, and don’t hesitate to seek second or third opinions if necessary. With the right support and guidance, you can regain control over your health and reclaim the quality of life you deserve.
REFERENCES:
https://pelvicrehabilitation.com/pelvic-doctor-specialized
https://www.pelvicpaindoc.com/blog/pelvic-pain-specialist-vs-ob-gyn-whats-the-difference
https://www.cvmus.com/blog/female-patient-guide-pelvic-pain-specialists
https://nyulangone.org/doctors/condition/pelvic-pain
http://www.medparkhospital.com/en-US/disease-and-treatment/pelvic-pain

Understanding Laparoscopic Surgeries and Scar Management
In an era where medical advancements continually push boundaries, laparoscopic procedures have emerged as a game-changer, offering patients a minimally invasive approach to various surgical interventions. These cutting-edge techniques have revolutionized the way we perceive and experience surgical treatments, minimizing trauma and promoting faster recovery times.
Table of contents
- The Laparoscopic Advantage: A Paradigm Shift in Surgical Approach
- Scarring Concerns: Addressing a Common Apprehension
- Scar Formation: Understanding the Healing Process
- Factors Influencing the Appearance of Scars
- Scar Management Strategies for Laparoscopic Surgeries
- Embracing the Benefits: Laparoscopic Surgeries and Beyond
- Exploratory Laparoscopy: A Diagnostic Marvel
- Minimizing Risks and Maximizing Benefits
- Laparoscopy Recovery Time: A Quicker Comeback
- The Future of Minimally Invasive Procedures
- Embracing a New Era of Surgical Excellence
The Laparoscopic Advantage: A Paradigm Shift in Surgical Approach
Conventional open surgeries, while effective, often left patients grappling with significant scarring, prolonged recovery periods, and increased discomfort. Laparoscopic surgeries, on the other hand, have ushered in a new era of minimally invasive procedures, harnessing the power of advanced imaging and precision instruments.
Rather than relying on large incisions, laparoscopic surgeries employ specialized tools and a slender, illuminated instrument called a laparoscope. This remarkable device, equipped with a miniature camera, is inserted through a small incision, enabling surgeons to visualize the internal organs and perform intricate procedures with unparalleled precision.
Scarring Concerns: Addressing a Common Apprehension
Despite the numerous benefits of laparoscopic surgeries, one concern that often weighs on patients’ minds is the potential for scarring. While the incisions made during these procedures are significantly smaller than those of traditional open surgeries, the formation of scars remains a possibility.
However, it is essential to understand that scarring is a natural part of the body’s healing process and is not necessarily an indication of complications or improper surgical technique. In fact, the minimally invasive nature of laparoscopic surgeries often results in less noticeable scarring compared to open procedures.
Scar Formation: Understanding the Healing Process
To appreciate the intricacies of scar management, it is crucial to comprehend the underlying mechanisms of wound healing. When the skin is injured, the body initiates a complex cascade of events to repair the damaged tissue.
The healing process involves several phases, including inflammation, proliferation, and remodeling. During the proliferation phase, new blood vessels form, and collagen fibers are deposited, laying the foundation for scar tissue formation.
Factors Influencing the Appearance of Scars
While scarring is an inevitable consequence of any surgical procedure, several factors can influence the appearance and severity of scars. These include:
- Genetics: An individual’s genetic makeup plays a significant role in determining their propensity for scarring. Some individuals may be more prone to developing hypertrophic or keloid scars, which are characterized by excessive collagen production and raised thickened scar tissue.
- Age: Younger individuals generally have a more robust healing response, which can contribute to more pronounced scarring. As individuals age, their healing capabilities may diminish, potentially resulting in less visible scars.
- Skin Tone: Individuals with darker skin tones may be more susceptible to developing hyperpigmented scars, which can appear darker or lighter than the surrounding skin.
- Wound Healing Factors: Various factors, such as infection, poor nutrition, and underlying medical conditions, can impair the wound healing process and potentially lead to abnormal scarring.
Scar Management Strategies for Laparoscopic Surgeries
While scarring is an inevitable part of the healing process, there are several strategies that can be employed to minimize the appearance of scars following laparoscopic surgeries:
1. Surgical Technique and Incision Placement
Experienced surgeons skilled in laparoscopic techniques often place incisions in strategic locations, such as natural skin creases or areas where scarring is less noticeable. Additionally, careful tissue handling and meticulous surgical techniques can minimize trauma and promote optimal healing.
2. Postoperative Care and Scar Massage
Proper postoperative care is crucial for promoting optimal scar healing. Adhering to your surgeon’s instructions regarding wound care, activity restrictions, and follow-up appointments can significantly impact the appearance of scars.
Scar massage, a technique involving gentle massaging of the scar tissue, can help break down collagen fibers and improve the texture and appearance of scars over time.
3. Topical Treatments and Silicone Sheeting
Various topical treatments, such as silicone-based gels or sheeting, can be applied to scars to help hydrate and flatten them. These products create an occlusive environment, which can promote collagen remodeling and improve scar appearance.
4. Laser Therapy and Injectables
For more stubborn or hypertrophic scars, laser therapy or injectable treatments like corticosteroids may be recommended. These advanced techniques can help reduce scar thickness, improve texture, and address issues like hyperpigmentation or redness.
5. Sun Protection
Protecting scars from excessive sun exposure is crucial, as UV radiation can exacerbate hyperpigmentation and potentially worsen scar appearance. Diligent use of broad-spectrum sunscreen and protective clothing can help minimize these effects.
Embracing the Benefits: Laparoscopic Surgeries and Beyond
While scarring is an inevitable part of any surgical procedure, the minimally invasive nature of laparoscopic surgeries often results in less noticeable scarring compared to traditional open procedures. By understanding the factors influencing scar formation and employing appropriate scar management strategies, patients can optimize their healing outcomes and embrace the numerous benefits that laparoscopic surgeries have to offer.
From faster recovery times and reduced discomfort to improved cosmetic results, laparoscopic surgeries represent a significant advancement in the field of medicine. As technology continues to evolve, we can expect even more innovative approaches to minimize scarring and enhance patient outcomes.
Exploratory Laparoscopy: A Diagnostic Marvel
In addition to its surgical applications, laparoscopy has proven invaluable as a diagnostic tool, enabling physicians to explore and visualize internal organs with remarkable clarity. This exploratory laparoscopy approach has revolutionized the way various conditions are diagnosed and treated, particularly in cases where traditional imaging techniques may not provide sufficient information.
One of the primary advantages of exploratory laparoscopy is its ability to directly visualize organs and tissues, allowing for a more accurate and comprehensive assessment. This can be especially beneficial in diagnosing conditions such as:
- Abdominal or pelvic pain of unknown origin
- Suspected endometriosis or other gynecological conditions
- Gastrointestinal disorders, including inflammatory bowel diseases
- Liver or gallbladder abnormalities
- Potential adhesions or scar tissue formation from previous surgeries
By providing a direct visual examination, exploratory laparoscopy can help identify the underlying cause of symptoms, guide treatment decisions, and even facilitate immediate intervention if necessary.
Minimizing Risks and Maximizing Benefits
While laparoscopic procedures, including exploratory laparoscopy, are generally considered safe and minimally invasive, it is essential to acknowledge and address potential risks. These may include:
- Bleeding or injury to surrounding organs or structures
- Infection at the incision site or within the abdominal cavity
- Adverse reactions to anesthesia or medications
- Potential for conversion to open surgery in case of complications
To mitigate these risks, it is crucial to choose experienced and skilled surgeons who are well-versed in laparoscopic techniques. Additionally, adhering to pre-operative instructions, disclosing relevant medical history, and following post-operative care guidelines can contribute to a smoother recovery process.
Laparoscopy Recovery Time: A Quicker Comeback
One of the most significant advantages of laparoscopic procedures, including exploratory laparoscopy, is the relatively shorter recovery time compared to traditional open surgeries. While recovery times can vary depending on the specific procedure and individual factors, patients typically experience:
- Reduced postoperative pain and discomfort
- Shorter hospital stays, often discharged within a day or two
- Faster return to normal activities and work
- Quicker resumption of regular diet and routine
It is important to note that recovery times can be influenced by factors such as the complexity of the procedure, the patient’s overall health, and adherence to postoperative instructions. However, in general, laparoscopic surgeries offer a more streamlined recovery process, allowing patients to resume their normal lives more quickly.
The Future of Minimally Invasive Procedures
As medical technology continues to advance, the field of laparoscopic surgery and minimally invasive procedures is poised for even greater advancements. Ongoing research and innovation are paving the way for:
- Robotic-assisted laparoscopic surgeries, enhancing precision and control and better visualization of endometriosis lesions
- Smaller and more advanced laparoscopic instruments
- Improved imaging and visualization techniques
- Incorporation of artificial intelligence and machine learning for surgical planning and guidance
- Development of novel scar management therapies and techniques
These advancements aim to further minimize scarring, reduce recovery times, and improve overall patient outcomes, solidifying the role of laparoscopic procedures as a preferred choice for a wide range of surgical interventions.
Embracing a New Era of Surgical Excellence
The rise of laparoscopic surgeries and minimally invasive procedures represents a significant milestone in the field of medicine, offering patients a path to improved surgical outcomes, faster recovery times, and reduced scarring. As we continue to embrace these cutting-edge techniques, it is essential to stay informed, seek guidance from experienced healthcare professionals, and prioritize personalized care and scar management strategies.
By combining technological advancements with a deep understanding of the healing process and scar formation, we can unlock a new era of surgical excellence, where minimally invasive procedures become the norm, and patients can confidently embark on their journey towards optimal health and well-being.
REFERENCES:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9358567
https://www.allaboutwomenmd.com/knowledge-center/what-is-laparoscopic-surgery.html

How to Find an Expert Endometriosis Specialist?
Table of contents
The Endometriosis Enigma
For countless individuals grappling with the perplexing condition of endometriosis, the journey toward finding a knowledgeable and compassionate specialist can be an arduous one. This chronic disorder, characterized by the growth of endometrial-like tissue outside the uterus, often evades timely diagnosis and effective treatment. The debilitating symptoms, encompassing excruciating pelvic pain, heavy menstrual bleeding, and even infertility, can severely impact one’s quality of life.
Navigating the labyrinth of healthcare professionals can be a daunting task, especially when faced with the frustrating reality that many gynecologists lack the specialized training and expertise to accurately identify and manage endometriosis. The absence of a dedicated medical specialty solely focused on this condition further compounds the challenge.
The Pursuit of Expertise
Fortunately, amidst this landscape of uncertainty, a select group of medical professionals have dedicated their careers to unraveling the complexities of endometriosis. These esteemed authorities, often based in larger metropolitan areas or affiliated with teaching hospitals, have emerged as beacons of hope for those seeking relief from the relentless grip of this enigmatic condition.
However, the quest to locate these specialists can be akin to finding a needle in a haystack. With no official designation or certification process, the onus falls squarely on the patient to navigate the intricate web of resources and recommendations.
Leveraging Support Networks
One of the most invaluable resources in this arduous journey is the collective wisdom of endometriosis support groups and online communities. These platforms not only serve as a sanctuary for shared experiences but also as a treasure trove of insights, enabling individuals to tap into the collective knowledge of those who have walked the path before them.
By engaging with these support networks, patients can gain access to a wealth of information, including recommendations for reputable specialists, insights into their treatment approaches, and firsthand accounts of experiences with various healthcare providers.
Consulting Primary Care Physicians
While primary care physicians may not possess the specialized expertise required to treat endometriosis, they can serve as invaluable allies in the quest for specialized care. These healthcare professionals often maintain a network of referrals and can provide guidance on navigating the complexities of the healthcare system.
Harnessing Online Resources
In the digital age, the power of online resources cannot be understated. Organizations such as the Endometriosis Foundation of America and the American Society for Reproductive Medicine offer comprehensive databases and referral services, enabling patients to identify specialists in their vicinity who specialize in the diagnosis and treatment of endometriosis.
Additionally, endometriosis-focused blogs, forums, and social media platforms can serve as valuable repositories of information, providing insights into the experiences of others who have navigated similar journeys.
Vetting Potential Specialists
Once a list of potential specialists has been curated, the process of vetting and selecting the most suitable healthcare provider begins. This critical phase involves a multifaceted approach, encompassing both objective and subjective evaluations.
Key considerations include:
- Expertise and Experience: Assessing the specialist’s specific training, certifications, and extensive experience in treating endometriosis, particularly in complex cases or those involving fertility challenges.
- Treatment Approach: Evaluating the specialist’s philosophical alignment with your preferences and needs, whether it be a focus on medication, surgical interventions, or a holistic, multidisciplinary approach.
- Collaborative Mindset: Determining the specialist’s willingness to engage in a collaborative partnership, valuing your input, addressing your concerns, and fostering an environment of open communication.
- Compassion and Empathy: Gauging the specialist’s ability to exhibit genuine compassion, empathy, and understanding towards the unique challenges and experiences associated with endometriosis.
- Reputation and Reviews: While acknowledging that reputation alone should not be the sole determinant, seeking insights from others who have experienced the specialist’s care can provide valuable context.
Embracing Second Opinions
In the realm of endometriosis care, the pursuit of a second opinion should be viewed not as a sign of doubt but rather as a proactive step toward ensuring the most comprehensive and personalized treatment plan. By consulting multiple specialists, patients can gain a broader perspective, compare treatment philosophies, and ultimately make an informed decision that aligns with their individual needs and goals.
Preparing for the Appointment
Once a specialist has been selected, thorough preparation is key to maximizing the value of the consultation. Gathering comprehensive medical records, documenting symptoms and their impact on daily life, and articulating specific concerns and questions can facilitate productive dialogue and enable the specialist to gain a holistic understanding of the patient’s unique circumstances.
Advocating for Yourself
Throughout this journey, it is imperative for individuals to embrace the role of an active advocate for their own health and well-being. While endometriosis specialists possess invaluable expertise, no one understands the nuances of one’s experiences better than the individual themselves.
Cultivating the confidence to voice concerns, ask probing questions, and respectfully challenge recommendations that do not align with personal beliefs or goals is an essential component of forging a truly collaborative partnership with a healthcare provider.
Embracing a Holistic Approach
While the pursuit of an endometriosis specialist is a critical step, it is essential to recognize that addressing this complex condition often requires a multidisciplinary, holistic approach. Incorporating complementary therapies, lifestyle modifications, and emotional support can enhance the effectiveness of medical interventions and promote overall well-being. By embracing a comprehensive and individualized treatment plan, patients can optimize their chances of achieving lasting relief and regaining control over their lives.
Perseverance and Resilience
The journey towards finding an endometriosis specialist is rarely a linear one. It may be punctuated by setbacks, disappointments, and moments of frustration. However, it is essential to cultivate a mindset of perseverance and resilience, recognizing that the ultimate goal – finding a compassionate and knowledgeable healthcare partner – is worth the effort.
By remaining steadfast in their pursuit, individuals can navigate the challenges with grace and determination, ultimately emerging victorious in their quest for comprehensive care and a better quality of life.
In conclusion, the path to finding an endometriosis specialist is a winding and often arduous one, but it is a journey that holds the promise of relief, understanding, and empowerment. By leveraging the collective wisdom of support networks, harnessing the power of online resources, and embracing a proactive and collaborative approach, individuals can navigate this quest with confidence and emerge victorious in their pursuit of comprehensive care.
REFERENCES:
https://www.endofound.org/preparing-to-see-a-doctor
https://www.everydayhealth.com/endometriosis/finding-endometriosis-expert-what-you-need-know
https://www.elanzawellness.com/post/how-to-find-an-endometriosis-specialist-in-the-us

Decoding the Mystery of Scar Endometriosis
Endometriosis, a perplexing condition where endometrial-like tissue is found outside the uterus, manifests in various forms. Among them is scar endometriosis, a rare yet distressing subtype that warrants heightened awareness and understanding. This is often a consequence of surgical procedures. Scar endometriosis can profoundly impact an individual’s quality of life, necessitating prompt diagnosis and effective management.
Table of contents
- Introduction
- Etiology: Unveiling the Root Causes
- Clinical Manifestations: Recognizing the Signs
- Diagnostic Approach: Piecing Together the Puzzle
- Treatment Strategies: Alleviating the Burden
- Preventive Measures: Minimizing the Risk
- Psychological Impact and Support
- Fertility Considerations
- Emerging Treatments and Research Frontiers
- Multidisciplinary Care: A Collaborative Approach
- Patient Education and Advocacy
- Conclusion
Introduction
Scar endometriosis, an extrapelvic manifestation of endometriosis, is characterized by the growth of endometrial-like tissue within or around a surgical scar. While its incidence is relatively low, ranging from 0.03% to 1.08% of endometriosis cases, the symptoms can be just as debilitating and the diagnosis challenging. This article delves into the intricacies of scar endometriosis, shedding light on its causes, symptoms, diagnosis, and treatment options, empowering individuals to navigate this intricate condition with knowledge and confidence.
Etiology: Unveiling the Root Causes
The precise etiology of scar endometriosis remains a subject of ongoing research and debate. However, several theories have been proposed to explain its development:
- Iatrogenic Transplantation: This widely accepted theory suggests that during surgical procedures, endometriosis cells inadvertently become implanted within the surgical incision or scar tissue. This phenomenon is particularly common in obstetric and gynecological surgeries, such as cesarean sections, hysterectomies, and laparoscopic procedures.
- Lymphatic or Vascular Dissemination: Similar to other forms of endometriosis found in the body, these cells may travel through lymphatic or vascular channels, eventually seeding and proliferating within surgical scars or distant sites.
- Metaplastic Transformation: This theory proposes that specialized cells within the surgical scar undergo metaplastic changes, transforming into endometrial-like cells under the influence of specific hormonal or environmental factors.
While these theories provide plausible explanations, the exact mechanisms underlying scar endometriosis remain elusive, underscoring the need for further research to unravel the complexities of this condition.
Clinical Manifestations: Recognizing the Signs
The clinical manifestations of scar endometriosis can vary, making early recognition a challenge. However, certain symptoms may raise suspicion and prompt further investigation:
- Cyclical Pain: One of the hallmark symptoms is cyclical pain or discomfort at the surgical scar site, often coinciding with menstrual periods. This pain can range from mild to severe and may radiate to adjacent areas.
- Swelling or Lump: Many people with scar endometriosis report the presence of a palpable lump or swelling at the scar site. This lump may fluctuate in size and tenderness throughout the menstrual cycle.
- Cyclical Bleeding: In some cases, patients may experience cyclical bleeding or discharge from the surgical scar, further indicating the presence of endometriosis.
- Dysmenorrhea and Pelvic Pain: Scar endometriosis can coexist with pelvic endometriosis, leading to additional symptoms such as dysmenorrhea (painful periods) and chronic pelvic pain, especially if endometriosis has been left untreated.
It is crucial to note that the absence of cyclical symptoms does not necessarily exclude the possibility of scar endometriosis, as some cases may present with non-cyclical pain or discomfort.
Diagnostic Approach: Piecing Together the Puzzle
Diagnosing scar endometriosis can be challenging due to its non-specific symptoms and the need for a multidisciplinary approach. The diagnostic process typically involves the following steps:
- Medical History and Physical Examination: A thorough medical history, including details of previous surgeries, menstrual patterns, and associated symptoms, is essential. During the physical examination, healthcare professionals may palpate the surgical scar site for any palpable masses, nodules, or tenderness.
- Imaging Modalities: Various imaging techniques can aid in the diagnosis and assessment of scar endometriosis:
- Ultrasonography: Ultrasound is often the initial imaging modality employed, as it can detect hypoechoic or heterogeneous lesions with irregular borders at the scar site.
- Magnetic Resonance Imaging (MRI): MRI provides detailed information about the extent and depth of the lesion, aiding in surgical planning.
- Computed Tomography (CT) Scan: While less commonly used, CT scans can help differentiate scar endometriosis from other conditions, such as hernias or malignancies.
- Biopsy and Histopathological Examination: Ultimately, a definitive diagnosis requires a biopsy or surgical excision of the lesion, followed by histopathological examination. The presence of endometrial glands and stroma within the scar tissue confirms the diagnosis of scar endometriosis.
It is essential to note that a multidisciplinary team including gynecologists, radiologists, and pathologists may be necessary to establish an accurate diagnosis and develop an appropriate treatment plan.
Treatment Strategies: Alleviating the Burden
The management of scar endometriosis aims to alleviate symptoms, prevent recurrence, and preserve fertility when desired. The treatment approach is multifaceted and tailored to each individual’s unique circumstances:
- Surgical Intervention: Wide surgical excision with clear margins is the ideal treatment for scar endometriosis. This procedure involves the complete removal of the endometriosis lesion(s), including any affected surrounding tissue or muscle layers. In cases of extensive involvement, abdominal wall reconstruction with mesh reinforcement may be recommended.
- Hormonal Therapy: While not a definitive treatment, hormonal therapies such as oral contraceptives, progestins, or gonadotropin-releasing hormone (GnRH) agonists can provide temporary symptom relief, and some research shows that these therapies may suppress the growth of lesions. However, these medications may have side effects and do not address the underlying lesion.
- Combined Approach: In some cases, a combined approach involving surgical excision followed by adjuvant hormonal therapy may be recommended and may reduce the risk of recurrence.
- Pain Management: Effective pain management strategies, including the use of non-steroidal anti-inflammatory drugs (NSAIDs) or other analgesics, may be necessary to alleviate discomfort associated with scar endometriosis.
It is crucial to engage in shared decision-making with healthcare professionals, weighing the risks and benefits of each treatment option to determine the most appropriate course of action.
Preventive Measures: Minimizing the Risk
While the complete prevention of scar endometriosis may not be feasible in all cases, certain measures can be taken to reduce the risk of its development:
- Meticulous Surgical Technique: During surgical procedures, particularly those involving the uterus or pelvic region, strict adherence to meticulous surgical techniques is paramount. This includes minimizing the risk of cell seeding, proper handling of surgical specimens, and thorough irrigation of the surgical site.
- Containment of Tissue Biopsies: The use of endo-bags or containment devices during laparoscopic procedures can help prevent the inadvertent dissemination of endometriosis cells into the surgical field.
- Careful Wound Closure: Ensuring proper closure of the peritoneum and fascial layers during abdominal surgeries can help minimize the risk of endometriosis cell implantation within the surgical site.
- Postoperative Monitoring: Regular follow-up and vigilance for any signs or symptoms of scar endometriosis in the postoperative period can aid in early detection and prompt management.
While these preventive measures cannot guarantee the complete elimination of scar endometriosis, they can contribute to reducing the risk and promoting better outcomes for patients undergoing surgical procedures.
Psychological Impact and Support
Scar endometriosis can have a profound impact on an individual’s psychological well-being, often leading to feelings of frustration, anxiety, and diminished self-esteem. The chronic pain, discomfort, and potential impact on fertility can take a toll on mental health, underscoring the importance of holistic care and support.
Healthcare professionals should be attuned to the psychological needs of patients with scar endometriosis and provide access to counseling, support groups, or mental health resources as needed. Building a strong support system and fostering open communication can empower an individual to cope with the challenges of this condition more effectively.
Fertility Considerations
For individuals desiring fertility, the impact of scar endometriosis on fertility is a significant concern. While the condition itself may not directly affect fertility, the presence of pelvic endometriosis or the surgical interventions required for treatment can potentially impact fertility outcomes.
In such cases, a multidisciplinary approach involving reproductive endocrinologists and fertility specialists may be necessary. Fertility preservation techniques, such as egg or embryo freezing, may be considered for people undergoing extensive surgical procedures. Ongoing monitoring and tailored treatment plans can help optimize fertility outcomes for those affected by scar endometriosis.
Emerging Treatments and Research Frontiers
While current treatment modalities for scar endometriosis have shown promising results, ongoing research efforts aim to further enhance our understanding and management of this condition. Some emerging areas of interest include:
- Targeted Therapies: The development of targeted therapies that selectively inhibit the growth or proliferation of endometriosis could potentially offer more effective and less invasive treatment options.
- Stem Cell Therapy: Preliminary research explores the potential of stem cell therapy in regenerating or repairing damaged tissue, potentially reducing the need for extensive surgical interventions.
- Genetic and Molecular Studies: Investigating the genetic and molecular mechanisms underlying scar endometriosis could provide insights into its pathogenesis and pave the way for personalized treatment strategies.
- Improved Diagnostic Techniques: Ongoing efforts to refine imaging modalities and develop novel biomarkers could enhance the accuracy and timeliness of scar endometriosis diagnosis.
As research continues to advance, the future holds promise for more effective, personalized, and minimally invasive approaches to managing scar endometriosis.
Multidisciplinary Care: A Collaborative Approach
Scar endometriosis often requires a multidisciplinary approach involving various healthcare professionals, each contributing their expertise to ensure comprehensive care. This collaborative team may include:
- Gynecologists: Gynecologists play a pivotal role in diagnosing, treating, and managing scar endometriosis, as well as addressing any associated pelvic endometriosis or fertility concerns.
- Radiologists: Radiologists are essential in interpreting imaging studies and guiding the diagnostic process, particularly in cases where surgical intervention is being considered.
- Pathologists: Pathologists provide crucial insights by examining tissue samples and confirming the diagnosis of scar endometriosis through histopathological analysis.
- Surgeons: Surgical specialists, such as general surgeons or plastic surgeons, may be involved in the surgical management of scar endometriosis, particularly in cases requiring complex reconstructive procedures or mesh reinforcement.
- Pain Management Specialists: Chronic pain associated with scar endometriosis may necessitate the involvement of pain management specialists to develop effective pain control strategies.
- Mental Health Professionals: Psychologists, counselors, or therapists can provide invaluable support in addressing the psychological impact of scar endometriosis and promoting overall well-being.
Effective communication and collaboration among this multidisciplinary team are essential to ensure comprehensive, coordinated care tailored to each patient’s unique needs.
Patient Education and Advocacy
Empowering patients through education and advocacy is crucial in addressing the challenges posed by scar endometriosis. Healthcare professionals should prioritize providing accurate and up-to-date information to patients, fostering a better understanding of the condition, its implications, and available treatment options.
Patient support groups and advocacy organizations play a vital role in raising awareness, promoting research, and advocating for improved access to care and resources. These platforms can also serve as a valuable source of support, allowing individuals with scar endometriosis to connect, share experiences, and gain strength from one another. By fostering a collaborative approach between healthcare professionals, patients, and advocacy groups, we can collectively work towards improving the quality of life for those affected by scar endometriosis and advancing our understanding of this complex condition.
Conclusion
Scar endometriosis, a rare and often overlooked manifestation of endometriosis, presents unique challenges in diagnosis and management. However, by raising awareness, promoting early recognition, and embracing a multidisciplinary approach, we can better support everyone affected by this condition.
Through meticulous surgical techniques, targeted therapies, and ongoing research, we can strive to alleviate the physical and emotional burdens associated with scar endometriosis. Additionally, fostering open dialogue, patient education, and advocacy efforts can empower an individual to navigate this journey with knowledge, support, and resilience. By unraveling the enigma of scar endometriosis, we can pave the way for more effective treatments, improved quality of life, and a deeper understanding of this intricate condition, ultimately providing hope and solace to those affected.
REFERENCES:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2851454
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10024799
https://www.shreeivfclinic.com/endometriosis/scar-endometriosis
https://casereports.bmj.com/content/2014/bcr-2014-206693
https://www.mdpi.com/2296-3529/9/2/20

Does Removing Endometriosis and Fibroid Tumor Increase the Chances of Pregnancy?
Table of contents
- Overview of Endometriosis and Fibroids
- Endometriosis and Infertility
- Fibroids and Fertility
- Endometriosis and Pregnancy Outcomes
- Fibroids and Pregnancy Outcomes
- Treatment Options for Fertility Preservation
- Fertility Outcomes After Surgery
- Pregnancy Monitoring and Management
- Non-Surgical Treatment Options
- Emerging Treatments and Future Directions
- Emotional and Psychological Support
- Conclusion
Overview of Endometriosis and Fibroids
Endometriosis and uterine fibroids are prevalent gynecological conditions that can profoundly impact a woman’s reproductive health and fertility. Endometriosis, affecting approximately 10% of individuals assigned female at birth (AFAB), occurs when endometrial-like tissue is found outside of the uterus, primarily in the abdominopelvic cavity. Fibroids, on the other hand, are non-cancerous growths made up of fibrous tissue and smooth muscle cells that develop in or around the uterus. They may also be called uterine myomas or leiomyomas and affect an estimated 20–40% of AFABs, often during their childbearing years.
While these conditions are distinct, they share some common characteristics, including the potential to cause infertility and pregnancy complications. This article aims to provide a comprehensive understanding of the effects of endometriosis and fibroids on pregnancy, as well as the various treatment options available to maintain fertility.
Endometriosis and Infertility
Endometriosis is a leading cause of infertility, responsible for approximately 50% of infertility cases. The condition can impair fertility by obstructing the fallopian tubes, disrupting the hormonal milieu, causing inflammation, and altering endometrial development, thereby reducing the chances of successful embryo implantation.
However, it’s important to note that many individuals with endometriosis can still conceive naturally or with the assistance of fertility treatments. The impact of endometriosis on fertility may depend on the severity and location of the endometrial lesions.
Fibroids and Fertility
While fibroids are generally non-cancerous, their presence can affect fertility in several ways. Submucosal fibroids, which protrude into the uterine cavity, can significantly reduce the chances of successful embryo implantation and pregnancy rates during assisted reproductive technologies (ART) such as in vitro fertilization (IVF).
Intramural fibroids, which grow within the uterine muscle wall, can also impair fertility by distorting the uterine cavity and disrupting the hormonal environment necessary for successful implantation and placentation.
Endometriosis and Pregnancy Outcomes
People with endometriosis may face an increased risk of certain adverse pregnancy outcomes, including:
- Placental abnormalities (placenta previa, placental abruption)
- Preterm birth
- Pregnancy-induced hypertension/preeclampsia
- Cesarean delivery
The risk of these complications may be influenced by factors such as the severity of endometriosis, the presence of infertility, and the use of fertility treatments. However, many individuals with endometriosis can have successful, uncomplicated pregnancies.
Fibroids and Pregnancy Outcomes
Fibroids can also impact pregnancy outcomes in various ways. Individuals with fibroids may be at an increased risk of:
- Placental abnormalities (placental abruption, placenta previa)
- Preterm labor and delivery
- Fetal malpresentation (breech presentation)
- Cesarean delivery
- Postpartum hemorrhage
The risk of these complications may be influenced by factors such as the size, number, and location of the fibroids. Large fibroids, or those located in the uterine cavity, may pose a greater risk to the pregnancy.
Treatment Options for Fertility Preservation
For individuals with endometriosis or fibroids who desire future fertility, surgery or removal of the endometriosis lesions and/or fibroid(s) may be recommended to improve their chances of conception and reduce the risk of pregnancy complications.
Endometriosis Surgery
While there is no one-size-fits all approach to addressing endometriosis, surgical excision or removal of the lesions is thought to be the ideal approach to addressing the lesions directly. This minimally invasive surgery aims to remove the lesions while preserving the uterus and ovaries, allowing for future fertility.
Fibroid Removal
For individuals with fibroids who wish to maintain their fertility, a myomectomy may be recommended. This surgical procedure involves the removal of fibroids while preserving the uterus. Depending on the size, number, and location of the fibroids, myomectomies can be performed through various approaches, including:
- Hysteroscopic myomectomy (for submucosal fibroids)
- Laparoscopic myomectomy (for intramural or subserosal fibroids)
- Abdominal myomectomy (for larger or multiple fibroids)
The choice of approach depends on factors such as the size and location of the fibroids, as well as the surgeon’s expertise and the patient’s preferences.
Fertility Outcomes After Surgery
Studies have shown that those who undergo endometriosis excision or myomectomy for fibroid removal can achieve pregnancy rates ranging from 50-60%. However, it’s important to note that these procedures do not guarantee fertility, and the success rates may vary depending on factors such as age, severity of the condition, and the presence of other infertility factors.
Pregnancy Monitoring and Management
For those with endometriosis or fibroids who become pregnant, close monitoring and specialized care may be recommended to mitigate potential risks and ensure the best possible outcomes for both the mother and the baby.
This may involve regular ultrasound examinations to monitor fetal growth and placental function, as well as close monitoring for signs of preterm labor or other complications. In some cases, additional interventions or precautions may be necessary, such as bed rest, medication, or early delivery.
Non-Surgical Treatment Options
While surgical tumor removal is often the preferred option for those seeking to preserve fertility, there are also non-surgical treatment options available for managing endometriosis and fibroids. These include:
Endometriosis:
- Hormonal therapies (e.g., birth control pills, GnRH agonists)
- Anti-inflammatory medications
- Complementary therapies (e.g., dietary modifications, exercise)
Fibroids:
- Gonadotropin-releasing hormone (GnRH) agonists
- Selective progesterone receptor modulators (SPRMs)
- Uterine artery embolization (UAE)
- Magnetic resonance-guided focused ultrasound (MRgFUS)
These non-surgical options may be used to manage symptoms, reduce tumor size, or provide temporary relief before pursuing fertility treatments or tumor removal surgery.
Emerging Treatments and Future Directions
Research is ongoing to develop new and improved treatment options for endometriosis and fibroids, with a particular focus on preserving fertility and minimizing the risk of adverse pregnancy outcomes.
Some areas of active research include:
- Novel hormonal therapies and targeted therapies for endometriosis
- Improved surgical techniques for myomectomy and endometriosis excision
- Non-invasive tumor removal methods (e.g., MRgFUS, UAE)
- Preventative strategies to reduce the risk of endometriosis and fibroid development
As our understanding of these conditions continues to evolve, it is hoped that more effective and less invasive treatment options will become available, improving the quality of life and reproductive outcomes for individuals affected by endometriosis and fibroids.
Emotional and Psychological Support
The journey through endometriosis, fibroids, and infertility can be emotionally and psychologically challenging for many. It’s essential to recognize and address the emotional impact of these conditions, as well as the stress and anxiety that can accompany fertility treatments and pregnancy complications.
Support groups, counseling, and mental health resources can be invaluable in helping individuals cope with the emotional and psychological aspects of their condition and treatment. Healthcare providers should be mindful of these needs and provide appropriate referrals and support services as needed.
Conclusion
Endometriosis and fibroids are common gynecological conditions that can have a significant impact on fertility and pregnancy outcomes. While these conditions can pose challenges, there are various surgical and non-surgical options and treatment strategies available to help individuals achieve their desired family size while mitigating potential risks.
By working closely with their healthcare providers, people with endometriosis or fibroids can develop personalized treatment plans that address their individual needs and preferences. With proper management and care, those suffering from these conditions can successfully navigate pregnancy and achieve their dreams of parenthood.
REFERENCES:
https://www.webmd.com/women/uterine-fibroids/what-if-i-have-uterine-fibroids-while-pregnant
https://www.acfs2000.com/fibroids-and-endometriosis.html
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3608270
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9187594

Navigating the Road to Recovery: A Comprehensive Guide to Endometriosis Surgery Aftercare
The journey towards relief from endometriosis often involves surgical intervention, but the road to recovery can be a winding one. While endometriosis surgery offers hope for alleviating debilitating symptoms, the post-operative phase demands patience, diligence, and a steadfast commitment to self-care. This comprehensive guide aims to equip you with the knowledge and strategies necessary to navigate the recovery process with confidence and ease.
Table of contents
- Understanding the Endometriosis Surgery Landscape
- Preparing for the Post-Operative Journey
- The First Few Days: Taking It Slow
- The Weeks Ahead: Gradual Progress and Patience
- Returning to Normal Activities: Listening to Your Body
- Embracing a Holistic Approach to Recovery
- Addressing Potential Complications and Recurrence
- Fertility Considerations After Endometriosis Surgery
- Embracing a Positive Mindset and Self-Care
- Endometriosis Surgery Recovery: A Transformative Journey
Understanding the Endometriosis Surgery Landscape
Endometriosis, a chronic condition characterized by the growth of endometrial-like tissue outside the uterus, can wreak havoc on an individual’s quality of life. When medications and lifestyle modifications fail to provide adequate relief, surgical intervention may become a viable option. Minimally invasive approaches are now the go-to approaches for endometriosis surgery.
Laparoscopy: A Minimally Invasive Marvel
Laparoscopy, a minimally invasive procedure, is the preferred approach for endometriosis surgery. This technique involves making small incisions in the abdomen and inserting a laparoscope—a slender camera—to visualize and remove endometrial lesions or scar tissue. Laparoscopy offers numerous advantages, including reduced recovery time, minimal scarring, and a lower risk of complications.
Robotic Surgery: A More Advanced Approach
While you may hear mixed opinions on whether robotic surgery is better or worse than a laparoscopic approach, it appears that robotics are the way of the future. Providers using a robotic approach have to undergo more extensive surgical training, but the outcomes may be superior. While the operative time, or time and anesthesia, can be longer than laparoscopic surgeries, the visualization is undoubtedly better. Endometriosis can present with some hard-to-see or hard-to-recognize lesion types, and using this approach may be a better way to visualize those hard-to-see lesions to remove them.
Laparotomy: The Open Approach
This is an older approach that has been replaced with minimally invasive approaches, but you may still occasionally see someone undergo a laparotomy. In cases of extensive endometriosis or when laparoscopy is not feasible, laparotomy, an open surgical procedure, may be recommended. Laparotomy involves a larger incision in the abdomen, allowing for better visualization and access to deeply infiltrating endometriosis lesions. While more invasive, laparotomy may be necessary in certain circumstances.
Preparing for the Post-Operative Journey
Before embarking on the recovery path, it is crucial to lay the groundwork for a smooth transition. Your healthcare provider will provide specific instructions tailored to your unique situation, but here are some general guidelines:
- Arrange Transportation: Have a trusted friend or family member available to drive you home after the procedure, as you will be unable to operate a vehicle immediately following surgery.
- Stock Up on Essentials: Ensure your pantry and refrigerator are stocked with easily digestible foods, such as soups, broths, yogurt, and fruits, as well as plenty of fluids to stay hydrated.
- Prepare for Medication Management: Discuss any necessary medication adjustments with your healthcare provider, including pain relievers, antibiotics, and laxatives to aid in post-operative recovery.
- Create a Comfortable Environment: Arrange your living space to minimize unnecessary movement and exertion, ensuring easy access to essential items and a comfortable resting area.
The First Few Days: Taking It Slow
The initial days following endometriosis surgery are crucial for initiating the healing process. During this time, it is essential to prioritize rest and follow your healthcare provider’s instructions diligently:
- Manage Pain and Discomfort: Take prescribed pain medications as directed to alleviate discomfort and promote healing. Applying a heating pad or ice pack to the incision site can also provide relief.
- Stay Hydrated and Nourished: Consume plenty of fluids and easily digestible foods to support your body’s recovery efforts. Avoid heavy, greasy, or spicy meals that may cause digestive discomfort.
- Embrace Gentle Movement: While rest is essential, light movement, such as short walks around the house, can aid in circulation and prevent complications like blood clots.
- Monitor Incision Sites: Keep an eye on your incision sites for signs of infection, such as redness, swelling, or pus drainage. Follow your healthcare provider’s instructions for proper wound care.
The Weeks Ahead: Gradual Progress and Patience
As the days turn into weeks, your body will continue its healing journey. During this phase, it is important to strike a balance between rest and gentle activity, while adhering to your healthcare provider’s recommendations:
- Increase Activity Levels Gradually: After the initial recovery period, you can gradually increase your activity levels, starting with light exercises like walking or gentle stretching. Listen to your body and avoid overexertion.
- Manage Expectations: Recovery timelines can vary significantly based on the extent of the surgery, your overall health, and individual healing rates. Be patient and celebrate small victories along the way.
- Attend Follow-up Appointments: Keeping scheduled follow-up appointments with your healthcare provider is crucial for monitoring your progress and addressing any concerns or complications that may arise.
- Seek Support: The recovery process can be emotionally and physically taxing. Reach out to loved ones, support groups, or mental health professionals for encouragement and guidance during this journey.
Returning to Normal Activities: Listening to Your Body
As you continue to heal, the desire to resume your normal routine may become increasingly strong. However, it is essential to listen to your body and follow your healthcare provider’s advice regarding the appropriate timeline for returning to various activities:
- Work and School: Depending on the nature of your job or studies, you may be able to return to work or school within two weeks of the surgery. However, if your responsibilities involve physical labor or strenuous activity, a longer recovery period may be necessary.
- Exercise and Sports: Low-impact exercises like walking or light yoga can typically be resumed within a few weeks, but strenuous activities and high-impact sports should be avoided until your healthcare provider gives the green light.
- Intimate Relationships: It is generally recommended to abstain from sexual activity for at least six weeks after endometriosis surgery to allow for proper healing. Discuss any concerns with your healthcare provider.
- Travel and Vacations: While short trips may be possible within a few weeks, it is advisable to postpone extended travel or vacations until you have fully recovered, typically within 6-8 weeks after the surgery.
Embracing a Holistic Approach to Recovery
Recovery from endometriosis surgery extends beyond physical healing; it encompasses emotional and mental well-being as well. Embracing a holistic approach can enhance your overall recovery experience:
- Prioritize Stress Management: Chronic stress can hinder the healing process. Incorporate relaxation techniques like deep breathing exercises, meditation, or gentle yoga into your routine to promote a calm and peaceful mindset.
- Seek Emotional Support: Endometriosis can take a toll on mental health, and the recovery process can be emotionally taxing. Lean on your support system, join support groups, or consider seeking professional counseling to navigate the emotional challenges.
- Nourish Your Body: A balanced diet rich in whole foods, antioxidants, and anti-inflammatory nutrients can aid in the healing process and promote overall well-being. Consult with a nutritionist or dietitian for personalized dietary recommendations.
- Stay Positive and Patient: Recovery from endometriosis surgery is a journey, and setbacks or slower progress than anticipated can be disheartening. Maintain a positive mindset, celebrate small victories, and trust in the healing process.
Addressing Potential Complications and Recurrence
While endometriosis surgery aims to alleviate symptoms and improve quality of life, it is important to be aware of potential complications and the possibility of recurrence:
- Recognizing Signs of Complications: Be vigilant for signs of infection, excessive bleeding, or worsening pain, and promptly report any concerns to your healthcare provider. Especially around the incision sites, look for abnormal redness, swelling, heat, or pain.
- Managing Recurrence Risk: Endometriosis can recur after surgery, even with the best surgery. However, the persistence of endometriosis can occur when not all lesions are removed. Discuss long-term management strategies with your healthcare provider.
- Exploring Alternative Treatments: If endometriosis symptoms persist or recur despite surgery, explore alternative treatment options such as hormonal therapy, pain management techniques, or complementary therapies in consultation with your healthcare provider.
Fertility Considerations After Endometriosis Surgery
For many individuals with endometriosis, preserving fertility is a significant concern. Endometriosis surgery can potentially improve fertility outcomes, but it is crucial to have an open dialogue with your healthcare provider about your goals and options:
- Timing for Conception: Depending on the extent of the surgery and your overall health, your healthcare provider may recommend waiting a specific period before attempting conception to allow for complete healing.
- Assisted Reproductive Technologies: In cases of moderate to severe endometriosis, assisted reproductive technologies (ART), such as in vitro fertilization (IVF), may be recommended to improve pregnancy chances.
- Fertility Preservation Options: If you are considering future fertility but are not ready for conception immediately after surgery, discuss fertility preservation options like egg freezing with your healthcare provider.
Embracing a Positive Mindset and Self-Care
The recovery journey after endometriosis surgery can be physically and emotionally challenging, but embracing a positive mindset and prioritizing self-care can make a significant difference:
- Celebrate Small Victories: Recovery is a process, and every milestone, no matter how small, deserves celebration. Acknowledge and appreciate your progress, even on days when it may seem insignificant.
- Practice Self-Compassion: Be kind and patient with yourself throughout the recovery process. Healing takes time, and setbacks are a natural part of the journey. Treat yourself with the same compassion you would extend to a loved one.
- Engage in Enjoyable Activities: While rest is essential, engaging in low-impact activities that bring you joy and relaxation can boost your mood and overall well-being. Read a book, listen to music, or indulge in a favorite hobby that doesn’t strain your recovery.
- Seek Professional Support: If you find yourself struggling with anxiety, depression, or other mental health concerns during the recovery process, don’t hesitate to seek professional support from a therapist or counselor.
Endometriosis Surgery Recovery: A Transformative Journey
Recovering from endometriosis surgery is a transformative journey that requires patience, perseverance, and a commitment to self-care. While the road may be winding, embracing a positive mindset, following your healthcare provider’s guidance, and listening to your body’s needs can pave the way for a successful recovery and improved quality of life. Remember, every person’s journey is unique, and with the right support and strategies, you can navigate this path with resilience and emerge stronger on the other side.
REFERENCES:
https://my.clevelandclinic.org/health/treatments/4620-endometriosis-surgery
https://www.healthline.com/health/endotough/surgery-for-endometriosis

Understanding Bladder Endometriosis and Its Treatment
Bladder endometriosis is a medical condition that affects a significant number of women worldwide. It involves the growth of endometrial-like tissue on or in the bladder. This article aims to provide an understanding of bladder endometriosis, how it is diagnosed, and the surgical procedures involved in its treatment.
Table of contents
What is Bladder Endometriosis?
Bladder endometriosis is a subtype of endometriosis, a condition in which cells similar to those that make up the lining of the uterus (endometrium) grow outside of it. In bladder endometriosis, these cells grow in or on the bladder. This can lead to various symptoms, including urinary frequency, pain during urination, and even blood in the urine.
Read More: https://icarebetter.com/can-endometriosis-be-treated-without-surgery/
Epidemiology and Etiology
Bladder endometriosis is relatively uncommon, occurring in approximately 1-2% of all women with endometriosis. It is most frequently diagnosed in women of reproductive age, with an average age of diagnosis around 35 years. Studies have suggested that heritability may play a role in the development of bladder endometriosis, with some women having a family history of the condition.
The exact cause of bladder endometriosis is still being researched. However, four main theories have been proposed:
- The embryonal theory suggests that bladder endometriosis originates from Müllerian remnants in the vesicouterine/vesicovaginal septum.
- The migratory or metastatic theory suggests it is an extension of an adenomyotic nodule of the anterior uterine wall.
- The transplantation theory posits that it results from the implantation of regurgitated endometrium.
- The iatrogenic theory suggests it occurs after pelvic surgery, such as cesarean delivery or hysterectomy.
Symptoms of Bladder Endometriosis
The symptoms of bladder endometriosis can vary from person to person, but often include one or more of the following:
- Frequent urination: The need to urinate often is a common symptom.
- Dysuria: This is a term for pain or discomfort during urination.
- Hematuria: This refers to blood in the urine, which may be visible or detected on a urine test.
- Lower abdominal pain: Some patients may experience pain in the lower abdomen, often worsening during menstruation.
- Recurrent urinary tract infections: Some women may have frequent UTIs.
Read More: https://icarebetter.com/can-endometriosis-grow-inside-the-bladder/
Diagnosis of Bladder Endometriosis
Diagnosing bladder endometriosis can be a complex process, as the symptoms can mimic other conditions such as recurrent cystitis or bladder infections. Various diagnostic modalities are used in the preoperative assessment of bladder endometriosis. These include:
- Transabdominal and transvaginal ultrasound: These are the initial investigations of choice for suspected bladder endometriosis due to their immediate availability and easy access.
- Magnetic resonance imaging (MRI): This imaging technique can not only delineate the morphologic abnormalities of bladder endometriosis but can also potentially identify other common sites.
- Cystoscopy: This procedure allows doctors to view the inside of the bladder and urethra using a thin, lighted instrument.
- CT urogram or MRI urogram: These tests involve injecting intravenous contrast material (a type of dye) into the urinary bladder to obtain images of the urinary tract.
Treatment of Bladder Endometriosis
The treatment of bladder endometriosis typically involves surgery, as medical management is often not effective for this condition. There are several surgical options, including:
- Transurethral resection: This procedure involves the removal of the endometriotic tissue through the urethra using a special instrument.
- Partial cystectomy: This procedure involves the removal of a part of the bladder that is affected by endometriosis.
- Laparoscopic surgery: This is a minimally invasive procedure where small incisions are made in the abdomen to remove the endometriotic tissue.
It’s important to note that the choice of treatment depends on various factors, including the size and location of the endometriotic lesions, the woman’s age, and the presence of other associated conditions.
Long-term Outcomes and Recurrence
Studies have shown that surgical treatment of bladder endometriosis can lead to good results in terms of pain relief and improvement in urinary symptoms. However, endometriosis is a chronic condition, and there is a risk of recurrence. The overall recurrence rate of symptoms is about 30% for combined therapies and about 35% for hormonal treatment alone. Regular follow-up visits are essential to monitor for any signs of recurrence and to manage any ongoing symptoms.
Read More: https://icarebetter.com/can-endometriosis-on-ureter-cause-kidney-shooting-back-pain/
Conclusion
Bladder endometriosis is a challenging condition that requires a comprehensive approach to diagnosis and treatment. It is crucial for women to be aware of the symptoms and to seek medical advice if they are experiencing any urinary problems or pelvic pain. With appropriate treatment, most women with bladder endometriosis can achieve significant relief from their symptoms and improve their quality of life.
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3016174/
https://karger.com/uin/article/89/3/249/322520/Diagnosis-and-Treatment-of-Bladder-Endometriosis
https://academic.oup.com/humrep/article/25/4/884/701431
How to Prevent Endometrioma Cysts
Endometrioma cysts, often dubbed as ‘chocolate cysts’ or “endometrioma”, pose a significant health issue for many women worldwide. Understanding how to prevent endometrioma cysts is crucial for maintaining optimal reproductive health. This comprehensive, empathetic guide will walk you through the essentials of endometrioma prevention, demystifying complex medical terms and offering practical advice.
Table of contents
- Understanding Endometrioma
- Symptoms of Endometrioma
- Causes of Endometrioma
- Who is at Risk?
- How is Endometrioma Diagnosed?
- Why Endometrioma Causes Health Problems
- Preventing Endometrioma: An Overview
- Hormonal Control
- Lifestyle Factors
- Medical Management
- Surgical Treatment
- Complementary and Alternative Medicine (CAM) Therapies
Understanding Endometrioma
Endometrioma, a form of endometriosis, is a condition where tissue similar to the lining of the uterus grows outside the uterus, primarily on the ovaries. This growth often results in cysts filled with blood and tissue products, referred to as ‘chocolate cysts’ due to their dark, chocolate-like appearance. Understanding this condition is the first step in learning how to prevent endometrioma cysts.
Symptoms of Endometrioma
Endometrioma can manifest in a variety of symptoms, some of which are debilitating. Common symptoms include severe menstrual cramps, chronic pelvic pain, discomfort during intercourse, painful bowel movements or urination during menstruation, and fertility issues. In some cases, endometrioma may be asymptomatic, discovered only during a routine check-up or fertility assessment.
Causes of Endometrioma
The exact cause of endometrioma remains a subject of ongoing research. Some theories suggest retrograde menstruation, genetic factors, hormonal imbalances, and immune system dysfunctions. Surgical procedures in the abdominal area may also inadvertently transport endometrial tissue to other parts of the body, leading to endometrioma.
Who is at Risk?
While any woman who menstruates can develop endometrioma, certain factors increase the risk. These include a family history of endometriosis.
How is Endometrioma Diagnosed?
Doctors diagnose endometrioma through several methods, including pelvic examinations, imaging tests like ultrasounds or MRIs, and laparoscopy – a surgical procedure that allows for the visual inspection of pelvic organs. A definitive diagnosis often requires a biopsy, where a small sample of tissue is examined under a microscope.
Why Endometrioma Causes Health Problems
Endometrioma can lead to several health problems, including persistent pain, inflammation, and fertility issues. These cysts can grow, bleed, and cause scarring, leading to complications such as blocked fallopian tubes, adhesions (tissues that bind organs together), and issues with the intestines and bladder.
Preventing Endometrioma: An Overview
While endometrioma cannot be primarily prevented, certain interventions can reduce the risk of progression and recurrence after surgery. These interventions mainly focus on removing the endometriomas through surgery, lowering estrogen levels in the body, and increasing the impact of progesterone-like hormones.
Hormonal Control
Hormonal birth control methods, such as pills, patches, or rings with lower doses of estrogen, can help regulate the menstrual cycle and slow the progression of endometrioma. Intrauterine devices (IUDs) that release hormones may also be beneficial in reducing pain and bleeding.
Lifestyle Factors
Maintaining a healthy lifestyle can influence natural estrogen levels and potentially reduce the risk of endometrioma regrowth and progression. Regular exercise helps decrease body fat, which in turn lowers estrogen levels. Limiting alcohol and caffeine intake can also help, as excessive consumption of either can raise estrogen levels.
Medical Management
For those not trying to conceive, hormonal birth control is often the first line of treatment to manage symptoms.
Surgical Treatment
Excision surgery is usually considered the gold standard and the only treatment that truly removes the endometrioma lesions. The procedure involves removing the endometrioma while preserving as much healthy ovarian tissue as possible. Following surgery, hormonal treatment is typically resumed unless pregnancy is desired.
Complementary and Alternative Medicine (CAM) Therapies
In addition to conventional treatments, some individuals find relief from endometrioma symptoms through complementary and alternative medicine (CAM) therapies. These can include acupuncture, chiropractic, dietary changes, herbs, or supplements. It’s essential to discuss these approaches with your healthcare provider to ensure they’re safe and suitable for your specific needs.
In conclusion, while endometrioma cannot be prevented, understanding the condition, its risk factors, and potential treatments allows women to better manage their reproductive health. Regular check-ups, open communication with healthcare providers, and proactive lifestyle changes are all crucial in dealing with endometrioma and mitigating its effects on one’s life.
References:
https://my.clevelandclinic.org/health/diseases/22004-ovarian-endometrioma
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7754428/
Chocolate Cysts: Everything You Need To Know
Management of ovarian endometrioma
https://www.womenshealth.gov/a-z-topics/endometriosis

Endometriosis Supportive Therapy: Can Endometriosis Be Treated Without Surgery?
Endometriosis is an extremely painful chronic condition, which often also leads to infertility or subfertility, that affects about ten percent of women worldwide. It is characterized by growth of endometrial-like tissue, which normally lines the inside of the uterus, outside of the uterus on pelvic organs, the abdomen, bowel, and beyond. This tissue is not the same as the endometrium, characterized by very different behavior and unique molecular profiles.
Eventually, personalized “theranostic” (therapy and diagnostic) tools will exploit these unique molecular profiles and lead to far better diagnosis, therapy and monitoring approaches. Research is accelerating in this area, which is already very pervasive in other diseases such as cancer and various immuno-inflammatory conditions. Meanwhile, the only therapies that are available to actually treat endometriosis, not just masking of symptoms, are hormonal options and excisional surgery. However, there are major limitations to the argument that hormonal therapies work very well to treat endo rather than simply reduce symptoms. That leaves surgery.
So, in a word, “can endometriosis be treated without surgery?”, the answer is a resounding NO! That is not to say that hormonal and other treatments, including anti-inflammatory and perhaps anti-histamine agents (e.g. Zyrtec), both mainstream and integrative-holistic, don’t help. They might. Let’s unpack this a little bit to give you a roadmap of the options.
Table of contents
Understanding Endometriosis
The exact cause of endometriosis is technically unknown, but we know it is influenced by genetic, genomic, hormonal, immunologic and environmental epigenetic factors. In other words, it is “multi-factorial”. This means the reason you may have endo could be different from why your friend or even your sister does. Endo can also behave very differently because different factors are probably in play in different people. This makes a “standard treatment” hard, if not impossible, to recommend to any given patient. This is changing with the advent of endometriosis bio-molecular pathway research, which will lead to highly individualized targeted treatments. But this is not part of what is available today.
Diagnosis of Endometriosis
Diagnosing endometriosis is very challenging, because the symptoms can mimic other conditions. This is part of the reason that diagnosis is often delayed by 5-10 years and intentional or inadvertent gaslighting is rampant, depending on which specialist was consulted. The doctor may be looking at you through a general practice medical lens, or intestinal, urologic, neurologic or other lenses in forming their opinions.
Rule # 1 is to listen to the patient. This is almost never done to an appropriate extent. Why? Because today’s medical system limitations often lead to five-to-ten-minute visits with a semi-interested and overworked provider who is likely under-informed regarding endometriosis.
When rule #1 is broken, an appropriate evaluation and testing is not likely to be done. Ideally, a clinical suspicion leads to testing that may include ultrasound or MRI, various blood tests, testing for associated conditions and so on. None of these will reliably lead to a diagnosis of endo but can lead to appropriate specialist referrals to get to the root cause of pain, such as endo.
Rule #2 in medicine, in general, is to get a diagnosis before recommending treatment. This is because treatments can be ineffective when treating the wrong condition or, worse, can lead to complications and side effects. Unfortunately, in the author’s strong opinion, this is often violated specifically in endometriosis treatment. A common standard is to offer hormonal therapy to patients to see if it might work because the diagnosis might be endometriosis and endo is, in part, fueled by hormones. This may or may not be reasonable depending upon individual circumstances and choices.
This brings us to rule #3, that we’ll cover next, which proposes that patients should be offered treatment options to select from after informed consent about the potential risks vs the potential benefits based on the best possible scientific evidence. This is not always done very well and certainly depends on the “trust factor” with your selected specialist(s), since scientific evidence is subject to interpretation. Most patients do not realize this.
Conventional Treatment of Endometriosis
Traditional treatment for endometriosis often involves medication or surgery. Medications can include anti-inflammatory pain relievers and hormonal therapies. In the near future medications will include targeted biomolecular non-hormonal therapies, but they are not here yet. Pain relievers are mainly a symptom reducing band-aid and are not intended to treat, so we will not discuss them here either. They can certainly help in overall management, but we will focus on “treatment” in this article.
Hormones aim to either shut down ovarian function (in other words, cut off estrogen) or at least regulate the menstrual cycle, and progesterone analogs, to potentially reduce the growth of endometriosis tissue.
Surgery is used for definitive diagnosis of endo as well as treatment by removing any lesions or implants that are found. In some cases, the two modalities can be used hand in hand, but the order in which they are used, and the nature of the proposed hormonal therapy are important considerations.
Hormonal Treatment
International guidelines are very confusing and inconsistent regarding hormonal therapy for endometriosis. Because of this, recommendations can vary between practitioners. We won’t delve into all these options here, but the following are excellent summary articles on this important topic.
The important points to consider are as follows:
- The ONLY way currently to definitively diagnose endometriosis is through biopsy, usually performed during surgery.
- Starting treatment that can cause extreme side effects and potential long-term harm without first getting a definitive diagnosis seems imprudent. So, if a practitioner offers hormones because they “think” you have endo based on history, examination and perhaps some scans, at least get a second opinion from an endometriosis specialist. This approach is within international guidelines but can cause you a world of misery and potential harm if not managed in expert hands.
- Hormone therapy for endo boils down to either reducing estrogen levels or eliminating estrogen altogether or increasing progestational agent levels to try to medically eliminate endo lesions. Reducing estrogen levels is not possible since there are different types of estrogen, different sources of estrogen and endo lesions themselves can influence local production of estrogen.
- Endometriosis cells differ from endometrial cells that are found in the uterus by being relatively resistant to synthetic progestin or natural micronized progesterone therapy.
- Hormonal therapy is known to reduce pain when endometriosis is the cause. However, studies have shown that pain relief is possible but hormonal therapy fails to significantly retard the growth of endometriosis tissue when objectively tested in pathology laboratories. Further, hormonal therapy cannot eliminate scar tissue or fibrosis caused by endo and this fibrosis by itself can be a cause for pain.
- While unproven, under some circumstances it may be prudent to use less toxic hormonal therapy options to potentially reduce the risk of endo recurrence after surgery.
Surgical Treatment
When symptoms, history, physical exam, scans and laboratory evidence all point to endometriosis as a strong possibility to be the root cause of pain, and/or infertility, minimally invasive surgery should be considered to find out for sure. If endo is diagnosed, then medical hormonal therapy may make sense as part of a highly individualized treatment plan under the guidance of an endo specialist.
The caveat to considering endometriosis surgery is that there are, of course, potential risks and complications even though it is minimally invasive. These risks can be minimized in the hands of an expert surgeon, but they should be considered in a risk-benefit discussion.
More importantly, assuming you have identified an expert endo excision surgeon, surgery is the cornerstone to current effective treatment. While incompletely proven, for many reasons, it appears that excision of endo lesions and scar tissue (fibrosis) rather than burning them away (fulguration) is a better and safer approach. To discover more about surgical considerations, consider the following articles.
Integrative Holistic View of Endometriosis
Since the cause of endo is incompletely understood, but highly multifactorial, and because the reason endo is present in any given individual may vary, either surgery or hormonal therapy or both may fail. Failure is relative. In other words, failure may be defined as no immediate pain improvement, persistent subfertility, or it may mean recurrence years later. These are very different scenarios, requiring different approaches. Also, it’s important to consider whether or not associated conditions have been addressed, such as SIBO or other microbiome irregularities, other inflammatory immune-modulated disease and so on. Finally, pelvic floor physical therapy is not just a symptom band-aid but a critical co-treatment for pelvic floor function before and after surgery. These topics are all beyond the scope of this article, but you can discover more by reading the following articles.
If expert excision surgery and supportive hormonal therapy, when used, fails to alleviate pain then supportive pain management can still improve quality of life. This can be mainstream pain and anti-inflammatory medications like non-steroidal anti-inflammatory (NSAID), nerve block injections, electrical stimulation modalities and/or more holistic approaches including acupuncture, acupressure, mind-body biofeedback approaches such as HeartMath, herbals, aromatherapy and more.
Kicking it up a notch, here is something you do not see covered much other than in a very superficial manner. It is not rocket science but is not simplistic at the potential treatment level either. However, it is something you can implement in a proactive way at any point in your journey. Specifically, this is the impact of nutrition and lifestyle choices, as well as well-selected and targeted supplements, but drilled down a lot further than simply eating right, exercising and de-stressing.
Upcoming bio-molecular therapies will target specific biological pathways that we are now beginning to better understand. Many pathways are already identified, many not. The problem is that there are no mainstream medical therapies, yet which can target these pathways safely and effectively. We know from other related genomically modulated inflammatory diseases, like cancer and auto-immune disorders, that these treatments take a while to develop and offer safely. Meanwhile, many of the genomic, metabolic and epigenetic abnormalities that influence endo are known or at least partly known. With few exceptions, while it is too early to safely use pharmaceutical agents to modulate these abnormalities, nutrients, specific exercise, toxin avoidance, and even state of mind can affect the same pathways abnormalities without risk.
Nutrigenomics and Epigenetics
How do toxins or stress adversely affect your health, while healthy diet and exercise positively influence your health? In large part, relatively new sciences like metabolomics and genomics, and their derivatives, explain this. You are born with your genes and, so far, you can’t alter that deck of cards. Some genes may be “bad” and increase your risk of endo, as well as other diseases. However, not everyone with some bad genes develops disease. The most famous examples are identical twins who inherited the exact same genetics yet might look a little different (e.g. eye or hair color) and often get different diseases. Why?
Anything and everything you eat, drink, get exposed to via skin or breathing, or even think about or emote, can affect your genes through epigenetics. This means these substances and neurochemicals, good or bad, can turn genes on and off. Of course, it is infinitely more complex than that and multiple genes affect one process in many cases. However, you can actively modulate your inflammatory and oxidative state. Do we know what veggie or what thought or what toxin turns what specific gene on or off? No. But we do know how these gene-controlled pathways synergize and work together to create health or facilitate disease.
Conclusion
Surgery is a cornerstone to definitive diagnosis of endo and serves as very important part of treatment. The path to success is a correct diagnosis, attention to detail and a highly individualized treatment plan. This can only be carried out in consultation with endometriosis specialists in medical and surgical management.
Unfortunately, it is not easy to find someone or a team that can fit your needs, but it is a crucial step forward to seek out the best you can. The more complex your situation (e.g. possible advanced disease or repeat surgery) the more you need an excision surgeon with master surgeon skills. Ideally you want a specialist who is not only a surgeon but also capable of guiding you through any additional treatment options you may need, mainstream and holistic. While a master excision surgeon and integrative endo specialist is hard to come by, many have a team that can fulfill your needs.
References:
Endometriosis: Etiology, pathobiology, and therapeutic prospects
Brassica Bioactives Could Ameliorate the Chronic Inflammatory Condition of Endometriosis
Diet and risk of endometriosis in a population-based case–control study
Emerging Drug Targets for Endometriosis
Updated Post: July 09, 2024

How to Treat Bowel Endometriosis: A Comprehensive Guide
Bowel endometriosis, a complex and severe variant of endometriosis, is a condition best navigated with a deep understanding of its details. This guide aims to shed light on the various aspects of bowel endometriosis, from its origins to symptoms, diagnostic approaches, and treatment options, to empower those affected.
Table of contents
What is Bowel Endometriosis?
Endometriosis, a chronic health disorder predominantly affecting women in their reproductive years, is characterized by the growth of endometrial-like tissue, which usually lines the uterus in regions outside the uterus. This misplaced tissue prompts an inflammatory reaction, leading to distressing symptoms. When this aberrant tissue growth takes place on or inside the bowels, the condition is referred to as bowel endometriosis.
How Common is Bowel Endometriosis?
While the exact prevalence of bowel endometriosis remains uncertain, it’s estimated to occur in 5-15% of all endometriosis cases. Predominantly, it manifests on the rectum or sigmoid colon but can also affect the appendix or small intestine.
Read More: https://icarebetter.com/endometriosis-and-inflammatory-bowel-disease-distinguishing-the-differences/
Recognizing the Symptoms
Symptoms of bowel endometriosis may not always be apparent, especially in the early stages of the disease. However, as the condition progresses, women may experience discomfort associated with their menstrual cycle, sexual intercourse, bowel movements, and even infertility.
Symptoms commonly associated with bowel endometriosis include:
- Painful Bowel Movements: This is often accompanied by constipation or diarrhea.
- Rectal Bleeding: This symptom, which is more uncommon, usually occurs during menstruation.
- Infertility: Some women may experience difficulty conceiving.
- Pelvic Pain: Chronic pelvic pain is a common symptom associated with endometriosis, often more severe during menstruation or ovulation.
- Painful Intercourse: This is often due to the endometriosis lesion causing a distortion of the pelvic anatomy.
It’s important to note that bowel endometriosis can sometimes mimic symptoms of other gastrointestinal conditions, like irritable bowel syndrome (IBS), making it challenging to diagnose.
Diagnosing Bowel Endometriosis
A comprehensive diagnosis of bowel endometriosis usually involves a combination of physical examination, medical history analysis, and advanced imaging techniques. The diagnostic process may include:
- Physical Examination: This includes a manual check for growths in the rectum or vagina.
- Imaging Tests: These can include ultrasound, MRI, colonoscopy, and barium enema.
- Laparoscopy: This surgical procedure is considered the gold standard for diagnosing endometriosis, as it allows for visual examination of the uterus, ovaries, and other pelvic structures. And surgeons can take samples for histopathology evaluations.
Read More: Understanding Bowel Endometriosis
Treating Bowel Endometriosis: An Overview
Treatment for bowel endometriosis is complex and multifaceted. It requires a personalized approach, taking into account the severity of the disease, the patient’s age, fertility goals, and personal preferences. The primary treatment options include:
- Hormonal Therapy: This involves medications that control estrogen levels, which can influence the progression of endometriosis. These medications can help manage pain and other symptoms.
- Pain Management: Over-the-counter or prescription nonsteroidal anti-inflammatory drugs (NSAIDs) may be recommended to help alleviate pain.
- Surgery: Surgical interventions aim to remove as much endometrial tissue as possible while preserving organ function.
Surgical Treatment Options
Surgery is typically the primary treatment for bowel endometriosis, particularly for severe cases. The goal of surgery is to remove endometrial implants without compromising the functionality of the organs involved. There are three main surgical options:
- Segmental Bowel Resection: This involves removing the section of the bowel affected by endometriosis and reconnecting the healthy portions. This option is often recommended for larger areas of endometriosis.
- Rectal Shaving: This procedure involves shaving off the endometriosis from the top of the bowel without removing any portion of the intestines. It’s often used for smaller areas of endometriosis.
- Disc Resection: In this procedure, a surgeon cuts out a small disk where the endometriosis lesions appear and then closes the remaining hole.
Understanding the Risks of Surgery
Surgery for bowel endometriosis is a complex procedure associated with certain risks. These can include short-term complications such as infection, leakage of bowel content during the postoperative healing phase, peritonitis, and septicaemia. Long-term risks might include bowel dysfunction, characterized by frequency, urgency, and incontinence.
Read More: Finding an Excision Specialist: What you Need to Know
Hormone Treatment Options
Although hormonal treatments cannot halt the progression of endometriosis, they can help manage symptoms. Hormonal treatments for bowel endometriosis can include birth control pills, progestin injections, or, less favorably, gonadotropin-releasing hormone (GnRH) agonists.
Read more: What are the long-term side effects of Lupron?
Managing Symptoms and Quality of Life
Bowel endometriosis can significantly impact the quality of life of those affected. However, with appropriate treatment and management strategies, many women affected by this condition can lead fulfilling lives. Communication with your healthcare team, lifestyle modifications, and psychological support can all contribute to improving the quality of life.
Conclusion
Understanding how to treat bowel endometriosis is crucial for managing this complex and often painful condition. With the right approach, it’s possible to mitigate symptoms, improve fertility outcomes, and enhance the quality of life for those affected. If you suspect you have bowel endometriosis, it’s important to speak with a healthcare provider who can guide you through the diagnostic process and treatment options. With the right knowledge and resources, you can navigate this challenging condition and find a path to improved health and well-being.
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4229526/
https://weillcornell.org/news/what-is-bowel-endometriosis
https://www.webmd.com/women/endometriosis/bowel-endometriosis
https://www.healthline.com/health/womens-health/bowel-endometriosis
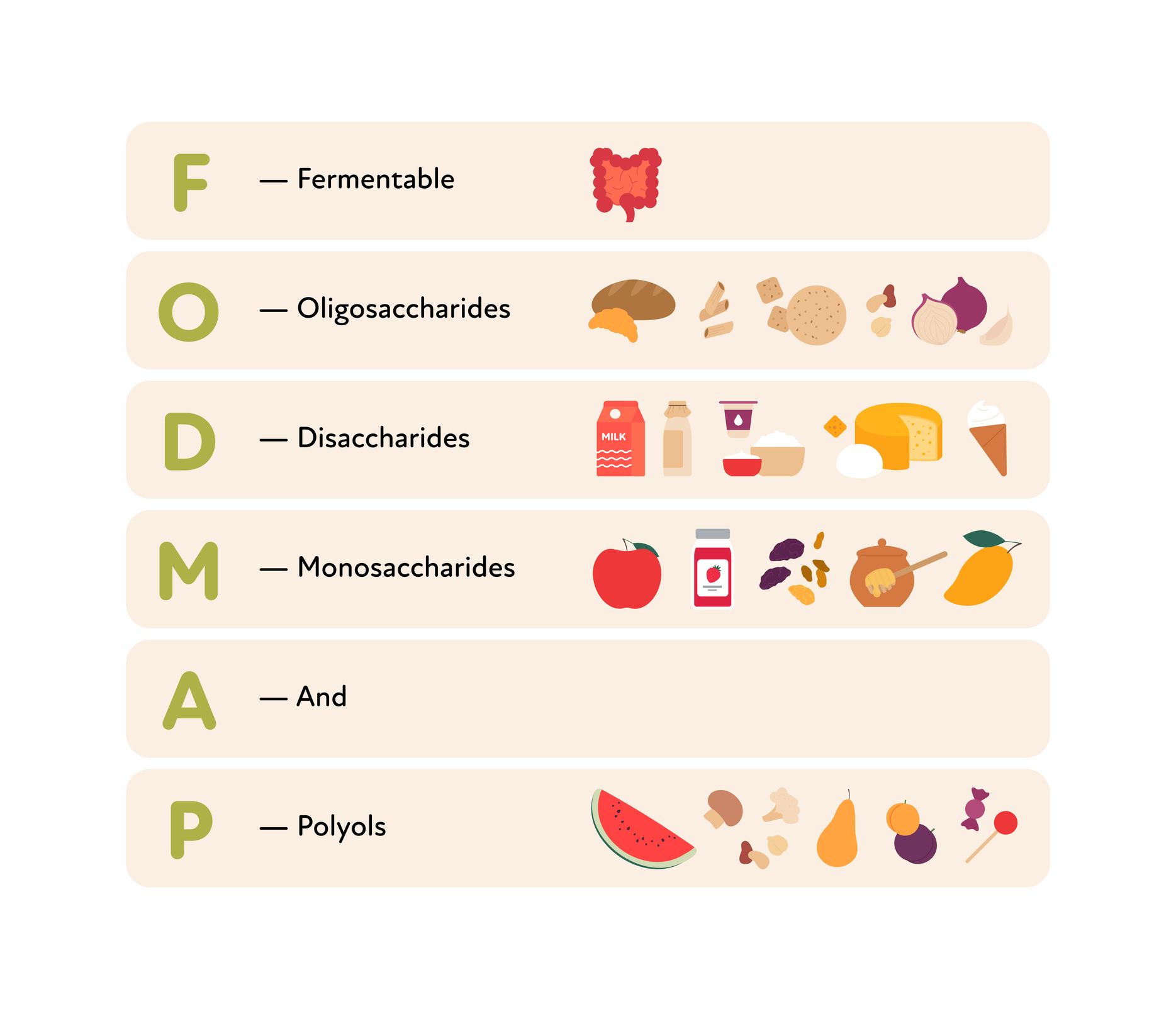
Endometriosis Diet: Low FODMAP, a Comprehensive Guide
Table of contents
- Understanding the Low FODMAP Endometriosis Diet
- What are FODMAPs?
- Exploring the Impacts of FODMAPs
- Who Should Follow a Low FODMAP Endometriosis Diet?
- The Purpose of a Low FODMAP Endometriosis Diet
- How to Follow a Low FODMAP Diet
- The Effectiveness of Low FODMAP Endometriosis Diet Combined with Other Therapies
The Low FODMAP Diet, a revolutionary approach for managing symptoms associated with Irritable Bowel Syndrome (IBS), has gained substantial recognition and popularity in recent years. Developed by researchers at Monash University, this diet has offered hope to many individuals suffering from IBS, a common gastrointestinal disorder that affects the digestive system. So how can it help those with endometriosis? This article will focus on the diet itself, but a relatively recent systematic review of dietary approaches and endometriosis showed that the low FODMAP diet was most helpful in managing symptoms in those with endometriosis that complained of gastrointestinal symptoms and had good follow through in individuals who tried it.
Understanding the Low FODMAP Endometriosis Diet
FODMAP is an acronym that stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. These are certain types of carbohydrates that are either poorly absorbed or not absorbed at all in your intestines and can trigger symptoms in individuals with IBS.
What are FODMAPs?
FODMAPs are naturally occurring sugars found in a wide range of foods and food additives. When consumed, these sugars move slowly through the small intestine, attracting water. As they reach the large intestine, they are fermented by gut bacteria, resulting in gas production. This extra gas and water cause the intestinal wall to stretch and expand, which can cause pain and discomfort, especially in people with IBS.
Types of FODMAPs
Here are the different types of FODMAPs and examples of foods where they can be found:
- Oligosaccharides: These include Fructans and Galacto-Oligosaccharides (GOS) found in foods such as wheat, rye, onions, garlic, and legumes.
- Disaccharides: Lactose is a disaccharide found in dairy products like milk, soft cheeses, and yogurts.
- Monosaccharides: Fructose is an example, found in honey, apples, and high fructose corn syrups.
- Polyols: These include Sorbitol and Mannitol, found in some fruits, vegetables, and used as artificial sweeteners.
Exploring the Impacts of FODMAPs
When FODMAPs are consumed, they move slowly through the small intestine, attracting water. As they reach the large intestine, gut bacteria use these FODMAPs as a fuel source, fermenting them and producing gas. This process is normal but can cause problems in people with IBS due to issues with motility (the speed at which contents move through the intestines) or a highly sensitive gut wall.
FODMAPs are found in a variety of foods, such as fruits, vegetables, bread, cereals, nuts, and legumes. It’s impossible to guess the FODMAP content of a food without careful laboratory analysis. Monash University has developed a mobile phone app, the Monash University FODMAP Diet App, which uses a simple traffic light system to indicate whether foods are low, moderate, or high in FODMAPs.
High FODMAP Foods and Low FODMAP Alternatives
Here’s a table showing some high FODMAP foods and their low FODMAP alternatives:
| High FODMAP Foods | Low FODMAP Alternatives |
|---|---|
| Vegetables: Artichoke, Asparagus, Cauliflower, Garlic, Green Peas, Mushrooms, Onion, Sugar Snap Peas | Aubergine/Eggplant, Beans (Green), Bok Choy, Green Capsicum (Bell Pepper), Carrot, Cucumber, Lettuce, Potato, Zucchini |
| Fruits: Apples, Apple Juice, Cherries, Dried Fruit, Mango, Nectarines, Peaches, Pears, Plums, Watermelon | Cantaloupe, Kiwi Fruit (Green), Mandarin, Orange, Pineapple |
| Dairy & alternatives: Cow’s Milk, Custard, Evaporated Milk, Ice Cream, Soy Milk (Made from Whole Soybeans), Sweetened Condensed Milk, Yoghurt | Almond Milk, Brie/Camembert Cheese, Feta Cheese, Hard Cheeses, Lactose-Free Milk, Soy Milk (Made from Soy Protein) |
| Protein sources: Most Legumes/Pulses, Some Marinated Meats/Poultry/Seafood, Some Processed Meats | Eggs, Firm Tofu, Plain Cooked Meats/Poultry/Seafood, Tempeh |
| Breads & Cereals: Wheat/Rye/Barley Based Breads, Breakfast Cereals, Biscuits and Snack Products | Corn Flakes, Oats, Quinoa Flakes, Quinoa/Rice/Corn Pasta, Rice Cakes (Plain), Sourdough Spelt Bread, Wheat/Rye/Barley Free Breads |
| Sugars, Sweeteners & Confectionery: High Fructose Corn Syrup, Honey, Sugar Free Confectionery | Dark Chocolate, Maple Syrup, Rice Malt Syrup, Table Sugar |
| Nuts & Seeds: Cashews, Pistachios | Macadamias, Peanuts, Pumpkin Seeds/Pepitas, Walnuts |
Who Should Follow a Low FODMAP Endometriosis Diet?
The Low FODMAP diet is specifically designed for individuals with medically diagnosed IBS. It is not recommended for people to self-diagnose and start this diet without the proper medical guidance. There are many conditions with symptoms similar to IBS, such as coeliac disease, inflammatory bowel disease, endometriosis, and bowel cancer. Therefore, it is crucial to get a clear diagnosis of IBS from a medical doctor before starting this diet.
The Purpose of a Low FODMAP Endometriosis Diet
The Low FODMAP diet is essentially a three-step diet used to manage symptoms of IBS, which can include abdominal pain, bloating, wind (farting) and changes in bowel habit (diarrhea, constipation, or both). The main goals of this diet are:
- Understand which foods and FODMAPs you tolerate and which ones trigger your IBS symptoms.
- Determine whether your IBS symptoms are sensitive to FODMAPs.
- Implement a less restrictive, more nutritionally balanced diet for the long term that only restricts foods that trigger your IBS symptoms.
How to Follow a Low FODMAP Diet
The Low FODMAP diet is a three-step diet, typically encompassing the following steps:
Step 1: Follow the Monash University Low FODMAP Diet by replacing high FODMAP foods in your diet with low FODMAP alternatives. This step usually lasts for 2-6 weeks.
Step 2: Continue your low FODMAP diet and complete a series of ‘FODMAP challenges’ to identify which FODMAPs you tolerate and which trigger symptoms.
Step 3: Relax dietary restrictions as much as possible, reintroduce well-tolerated foods and FODMAPs to your diet, and establish a ‘personalized FODMAP diet’ for the long term.
It is recommended to follow a Low FODMAP diet under the guidance of a dietitian who has specialty skills in managing IBS and using a FODMAP diet. Monash University’s FODMAP Dietitian Directory can be a useful resource to find such dietitians.
The Effectiveness of Low FODMAP Endometriosis Diet Combined with Other Therapies
The Low FODMAP diet has shown promising results in managing IBS symptoms. However, in some cases, the diet alone may not be sufficient, and other therapies may be required. One such therapy that has shown positive results in treating IBS is Gut Focused Hypnotherapy.
Understanding Gut Focused Hypnotherapy
Gut Focused Hypnotherapy is a type of treatment where patients are asked to visualize their gut as a perfectly slimy set of passages where all the digesting food slips through smoothly. This treatment has been proven to reduce symptoms of IBS by 70% in patients.
Combining Low FODMAP Diet and Gut Focused Hypnotherapy
Researchers at Monash University conducted a study combining the Low FODMAP diet and Gut Focused Hypnotherapy. The study resulted in a significant improvement in the overall and individual gut symptoms of the participants by the end of the six-week study.
Comparing the Low FODMAP Diet with Other IBS Diets
When comparing the Low FODMAP diet with other diets for IBS, it has been noted that the Low FODMAP diet seems to be superior to a gluten-free diet for patients with non-celiac gluten sensitivity. This is likely due to the comprehensive approach of the Low FODMAP diet, which considers all types of carbohydrates that could potentially trigger IBS symptoms.
The Low FODMAP diet has been shown to be effective in managing IBS symptoms, with studies showing improvement in pain, discomfort, bloating, and other GI symptoms. However, it is essential to follow this diet under the guidance of a trained dietitian and in conjunction with other therapies if necessary. As with any diet, the Low FODMAP diet should be personalized to fit the individual’s needs and tolerance levels.
If you are suffering from IBS-like symptoms and you have endometriosis or are just starting in your journey for a diagnosis, it may be worth seeking out professional guidance to see if the low FODMAP diet may be helpful. As a reminder – it is not going to treat your endometriosis and is used primarily for symptom management. It does not replace seeking out the root cause of both endometriosis and your GI dysfunction.
Disclaimer: This article is intended for informational purposes only and is not a substitute for professional medical advice. Always consult your doctor or a dietitian before making any changes to your diet.
References:
- https://www.monashfodmap.com/about-fodmap-and-ibs/
- https://www.monashfodmap.com/ibs-central/i-have-ibs/starting-the-low-fodmap-diet/
Molina-Infante, J., Serra, J., Fernandez-Banares, F., & Mearin, F. (2016). The low-FODMAP diet for irritable bowel syndrome: Lights and shadows. Gastroenterol Hepatol, 39(2), 55-65. https://doi.org/10.1016/j.gastrohep.2015.07.009

Finding an Excision Specialist: What you Need to Know
Table of contents
Finding a true excision specialist is difficult for many reasons, including the paucity of skilled surgeons and the financial burden that may come with when you find one that is a good fit for you. So, the first step is to find the right surgeon and the second step is determining how to navigate the financial implications. It’s important not to do it the other way around because initial botched surgery and treatment can make it that much more difficult to find relief. Surgery is never easier the second or third time around.
There are a small handful of carefully monitored sites with very helpful information and a listing of qualified surgeons based mainly on patient outcomes feedback, none better than Nancy’s Nook. While there may be a few others that share patient experiences and some information, most are not well monitored or refereed, and thus, information and surgeon leads must be viewed with caution. Nancy Petersen has a vested personal interest in endometriosis and a deep understanding of the disease based on her work for many years with Dr. David Redwine, a pioneer in the field. Thus the information which is refereed by Nancy and her hand-picked editors forms a solid base. However, patient feedback, while important, is not the only way to determine who to pick as your surgeon.
The degree of a surgeon’s true technical skills is not easy to judge, especially if you are in the majority of not being medically trained yourself. Review of resumes and asking questions such as where did you go to school or train or how many cases do you do leaves a lot to be desired. It is simply not an accurate reflection, although knowing the surgeon’s background and pedigree can help. So, what else can be done to help find the right surgeon for you?
iCarebetter was created to help those in need find a specialist with a bit more objective information than patient recommendations alone. iCarebetter includes surgeons who are video-vetted by a peer review process. This means that acknowledged experts review surgical videos submitted by surgeons who wish to be vetted and are objectively either verified or not as possessing a high level of surgical capabilities. Of course, this does not reflect total patient management and bedside manner and more subjective skills. However, you want someone who can get the surgery properly done at the highest possible level for your needs. There is something to be said about a surgeon who is not afraid of showing other, perhaps better, surgeons what they’ve got, so to speak.
Additional related reading: Why was iCarebetter built?
Not too long ago, it used to be that when you showed up to your appointment and asked the surgeon what type of surgery they perform, you typically would hear ablation or excision. More recently, many more have adopted excision as the preferred method, or at least talk that way. But outcomes are variable among those receiving “excision surgery,” why? This article will help you better understand some of the key takeaways in finding the right surgeon for you. Some are simply not at a high enough skill level to help you, and others do not walk the talk.
Additional related reading: Laparoscopy: A Common Treatment for Endometriosis
Excision vs. Ablation
Excision is the removal of tissue diseased with endo, whereas ablation is the burning or fulguration of endo lesions and surrounding tissue and organs, usually using electrocautery. Research shows both may be effective for superficial endometriosis and not near delicate structures such as bowel and ureters; however, it is usually not possible to accurately determine which are superficial or deep infiltrating lesions based on looking at them.
While some patients do symptomatically improve with ablation surgery, clinically, it is recommended that excision is the preferred method because you really cannot know if a lesion invades deeper into the tissue, until you remove it. It is likely that those who have benefited from ablation surgery probably only had superficial lesions, and those who did not improve likely had more extensive endometriosis that was missed or not fully eradicated. While this is clinically accepted, we need more research to confirm this and show it truly is the preferred method. The problem with designing an accurate research study for this question is that the skill of surgeons participating in clinical trials is highly variable, so the results can be completely wrong because it almost entirely depends on surgical skill. More importantly, one size does not fit all, and everyone is different. Hence, a truly expert surgeon who can determine and act appropriately on findings and nuances is critical to your personal success.
Important Terms and Approaches
- Wide excision is a term you may hear which means that there is a wide margin of tissue that is removed to ensure that only healthy tissue remains. There is no consensus on this topic. Some surgeons will adopt wide excision, while others will remove the individual lesions, perhaps leaving micro-diseased tissue behind that is difficult to visualize during surgery. These areas may develop endometriosis in the future. In an expert’s hands, it is a judgment call as to how wide any given area of excision should be. There is a balance of too much and not enough, and this requires a high level of expertise to optimize benefits and minimize harm.
- Combination of excision and ablation. The other consideration when it comes to excision surgery is that some surgeons adopt a combination of excision and ablation. Some tissue will be excised for histological confirmation of the disease, but then many lesions may be ablated instead of excised. This generally does not make sense unless the surgeon simply does not believe that excision is better. The only exception is the ablation of tiny lesions on sensitive areas, such as the ovarian surface, where fertility preservation is a concern.
- Incomplete removal of lesions. Most general gynecologic surgeons will not be able to excise very many lesions and will handle them by fulguration or ablation. Some surgeons may be able to excise the majority of lesions but do not have extensive training to remove all lesions. Hopefully, your surgeon will advise you of their limitations prior to rather than after your incomplete surgery. However, in some cases, endometriosis is not suspected prior to surgery, and a general gynecologist, who is most often not trained in higher-level excision techniques, is caught by surprise. In that case it is better to biopsy, prove that endo exists, and refer to a specialist rather than poorly perform an incomplete surgery.
Complete excision, especially in a difficult case where there is a lot of disease or perhaps in case of distorted anatomy due to repeat surgery, will only occur with a surgeon who has been additionally trained not just in MIGS (minimally invasive gynecologic surgery) but in endo excision per se. The main surgeon has to be an expert because it is never possible to predict how much endo there is, even if imaging scans are negative. Beyond that, if the main surgeon is not trained to perform bowel or urologic surgery, then a well-coordinated team is mandatory. The problem is that this coordination is not too tightly organized in many centers. Ask questions about who can do what, if any required supporting surgeons are in surgery from the beginning or “on call” when needed. The latter does not often work out too well because of other commitments that might be conflicting.
What if I Cannot Afford to see an Excision Specialist?
It is true that many of the surgeons that specialize in excision surgery are out-of-network providers. However, in the past couple of years there have been more surgeons that do take insurance and hopefully, with legislative efforts and more education, this trend will continue to grow.
That being said, there is a good reason why many do not take insurance, and even if you have the option of an in-network provider, it may not be the right surgeon for you. Currently, there is no difference in the coding when undergoing laparoscopic or robotic surgery for endometriosis that discriminates between ablation versus excision. Ablating lesions takes far less skill, time and effort than excision does. Meaning, that an in-network surgeon who performs an ablation surgery that takes one hour will get paid the same as an in-network surgeon who does an excision surgery that takes four hours. Becoming a trained excision specialist costs money to the provider to undergo extra training to be able to perform these types of procedures, and even more training to become an expert in robotics.
Until our payment, insurance, and coding systems catch up to what is required, we will likely not see a dramatic shift in those who take insurance.
Aside from the financial difference, those who are in-network may not be able to spend the amount of time you may want during office visits to discuss the details of your surgery and your overall case as those who are out-of-network. Out-of-network doctors are usually able to provide longer visits to address your concerns in depth instead of the standard 15-20 minutes you typically get with your regular OBGYN. Some choose cost over this important treatment planning time, but there are many people who value a personalized approach which takes more time over the cost of the surgery. It is not just excision surgery that will get you to where you want to be, and this personalized treatment planning includes very important discussion about pre-operative and post-operative healing options.
Whatever you choose, you want to feel comfortable with your surgeon and find the right fit for you.
Other Considerations: Some Tips on Navigating the System
- Change your insurance provider. I know this is easier said than done, but for those with HMOs who are only allowed to stay within a small network, it may be worthwhile to talk to your employer, or partner (if applicable), or do some research on what other insurances are available to you. PPO plans include their list of in-network providers but also often provide some reimbursement for out-of-network providers, especially if their surgeons are not at the skill level that you need or are not within a reasonable geographic range. Open enrollment is typically once a year, or when you change jobs, or due to other qualifying life-changing events. So consider this as an option that may allow you to have more latitude and choice when planning for surgery.
- Work with your insurance company. This does not always work, and is time-consuming, but can have a big payoff at the end. There have been patients who have communicated and worked with their insurance companies when there is no available specialist around to cover your out-of-network provider services. While this has worked for some, be ready for a time commitment and likely many phone calls to get to the person who can help you.
- Ask the doctor you have selected. Some excision specialists have been helping patients with this insurance negotiation conundrum for many years. Because of that, some have teams that help you get an exception and lower your out of pocket costs tremendously.
- Adopt a new perspective. Lastly, this will not necessarily save you money, but looking at your surgery as an investment in your health may make it seem more doable. We often do not think twice about financing $30-$40k on a car or the thousands of dollars we spend on “stuff,” but we often hesitate when it comes to our health. Without health, nothing else matters. For many, excision surgery has been life-changing, and thinking of paying for your surgery as an investment in your health, may be the best thing for you. Again, while upfront costs may seem high, a concerted effort to find the right surgeon, advocate for yourself, and ideally find a surgeon’s office that can help you negotiate and advocate can lead to lower final out-of-pocket costs than you might think.
Whatever route you take, it needs to be the best route for you, with a full understanding of the pros and cons. Take your time when finding the right surgeon, and don’t rush into something you are not comfortable with.
Additional reading: 7 Ways to Prepare For First Endometriosis Specialist Appointment

