
Integrative Therapies for Endometriosis
Table of contents
While there is no known cure for endometriosis, several mainstream treatment options can help manage the symptoms and improve quality of life. These are primarily focused on surgery and hormonal therapy. Research is ongoing to find additional multidisciplinary treatment options on the basis of immunomodulation, anti-inflammatory therapy, and molecular pathway signal alteration. Absent curative mainstream therapy, an approach that has gained popularity in recent years to help reduce symptoms and treat some underlying endo pathology, is “integrative therapy,” which adds a holistic natural component.
What is Integrative Therapy?
Integrative therapy is an approach to healthcare that takes into account the whole person, including their physical, emotional, and spiritual health. It involves combining conventional medical treatment with complementary therapies such as nutrition, supplementation, botanicals, acupuncture, massage, yoga, and much more. Integrative therapy aims to address the underlying causes of a person’s health concerns rather than simply treating the symptoms. While it often employs some aspects of Eastern medicine, it is not the same as “alternative therapy,” which can be ineffective, costly, and even dangerous in some situations. This overview article only scratches the surface of available options and is not meant to be authoritative in scope or depth.
Some of the complementary therapies that may be used in integrative therapy for endometriosis include:
Acupuncture
Everybody has heard of this, but briefly, acupuncture is a form of Traditional Chinese Medicine that involves the insertion of extremely thin needles into specific points along body pathways called meridians. These meridians and acupoints are close to where we know peripheral nerves course through your body. It has been used for centuries to treat a wide range of conditions, including chronic pain, headaches, anxiety, and infertility.
Acupuncture is believed to work by stimulating the body’s natural healing mechanisms, promoting the flow of energy, or Qi, throughout the body. It could also have an effect on the nerves from a mainstream perspective. In the context of endometriosis, acupuncture is thought to help by reducing inflammation and promoting the relaxation of the pelvic muscles, which can reduce pain and improve fertility.
One thing is for sure; it is not just a placebo effect. A systematic review published in the Cochrane Library in 2018 evaluated the effectiveness of acupuncture in treating pelvic pain associated with endometriosis. The review included seven randomized controlled trials involving a total of 527 participants. The authors found that acupuncture was associated with a statistically significant reduction in pain intensity compared to no acupuncture or sham acupuncture.
Another systematic review published in the Journal of Obstetrics and Gynecology in 2021 evaluated the effectiveness of acupuncture in treating endometriosis-related dysmenorrhea. The review included 17 randomized controlled trials involving a total of 1232 participants. The authors found that acupuncture was associated with a statistically significant reduction in pain intensity and duration compared to no acupuncture or sham acupuncture. They concluded that acupuncture might be a safe and effective therapy for managing endometriosis-related dysmenorrhea.
While the evidence for the effectiveness of acupuncture in treating endometriosis is promising, it is important to note that acupuncture is not a cure for endometriosis. Acupuncture may help to manage pain and other symptoms associated with the condition, but it does not address the underlying disease process other than helping reduce inflammation. Therefore, it should be used as part of a comprehensive treatment plan that includes conventional medical treatment as well as lifestyle modifications and other complementary therapies.
Acupressure
Acupressure is a related form of traditional Chinese medicine that involves applying pressure to specific points on the body to promote healing and reduce pain. Acupressure points that are commonly used in the treatment of endometriosis include the lower abdomen, lower back, and inner ankle. These points are believed to help regulate menstrual flow, reduce inflammation, and promote relaxation.
A randomized controlled trial published in the Journal of Complementary and Alternative Medicine in 2013 evaluated the effects of acupressure on pain and quality of life in women with endometriosis. The study included 60 participants who received either acupressure or a placebo. The authors found that acupressure was associated with a statistically significant reduction in pain intensity and an improvement in quality of life.
Another study published in the Journal of Obstetrics and Gynaecology Research in 2018 evaluated the effects of acupressure on menstrual pain and quality of life in women with endometriosis. The study included 62 participants who received either acupressure or a placebo. The authors found that acupressure was associated with a statistically significant reduction in menstrual pain intensity and an improvement in quality of life.
Massage Therapy
Massage therapy is a complementary therapy that involves the manipulation of soft tissues in the body, such as muscles and tendons, to promote relaxation and reduce pain. It has been used for centuries to treat a variety of conditions, including chronic pain, anxiety, and depression. We are talking about massage that is in addition to
Endometriosis can cause significant pain and discomfort, particularly during menstruation. Massage therapy can help ease tension in the pelvic muscles and reduce pain. A systematic review published in the Journal of Nursing Scholarship in 2019 evaluated the effectiveness of massage therapy in reducing pain and improving the quality of life in patients with endometriosis. The review included 13 studies involving a total of 602 participants. The authors found that massage therapy was associated with a statistically significant reduction in pain intensity and duration and improvements in quality of life and anxiety levels.
Massage therapy may also be beneficial for reducing stress and anxiety, which are common symptoms of endometriosis. Chronic pain can cause significant emotional distress, and massage therapy has been shown to be effective in reducing anxiety levels and promoting relaxation. A randomized controlled trial published in the Journal of Psychosomatic Obstetrics and Gynecology in 2018 evaluated the effects of massage therapy on anxiety levels in women with endometriosis. The study included 60 participants who received either massage therapy or no treatment. The authors found that massage therapy was associated with a statistically significant reduction in anxiety levels compared to no treatment.
In addition to its potential benefits for reducing pain and anxiety, massage therapy may also help to improve circulation and promote lymphatic drainage, which can help to reduce inflammation and promote healing. A review published in the Journal of Manual and Manipulative Therapy in 2016 evaluated the effectiveness of massage therapy for managing chronic pelvic pain, including endometriosis. The authors concluded that massage therapy might be a safe and effective therapy for managing chronic pelvic pain, mainly when used with other therapies.
Mind-Body Techniques
Meditation, yoga, Tai chi, and others are complementary therapies that can be used in the treatment of endometriosis to help manage physical, emotional, and mental support. These techniques focus on the connection between the mind and the body and are designed to help individuals learn how to use their thoughts and emotions to promote healing and reduce pain.
Endometriosis is often associated with significant emotional and mental distress, including anxiety, depression, and stress. Mind-body techniques can help to manage these symptoms by promoting relaxation and reducing stress levels. A systematic review published in the journal Obstetrics and Gynecology Clinics of North America in 2020 evaluated the effectiveness of mind-body therapies for managing chronic pain, including endometriosis. The review included 20 studies involving a total of 1126 participants. The authors found that mind-body therapies, including meditation, yoga, and Tai chi, were associated with statistically significant reductions in pain intensity, pain duration, and stress levels.
Meditation is a mind-body technique that involves focusing the mind on a particular object or thought to promote relaxation and reduce stress levels. A randomized controlled trial published in the journal Pain Medicine in 2018 evaluated the effects of mindfulness meditation on pain and quality of life in women with endometriosis. The study included 20 participants who received either mindfulness meditation or no treatment. The authors found that mindfulness meditation was associated with a statistically significant reduction in pain intensity and an improvement in quality of life.
Yoga is a mind-body technique that combines physical postures, breathing exercises, and meditation to promote relaxation and reduce stress levels. A randomized controlled trial published in the journal Obstetrics and Gynecology in 2018 evaluated the effects of yoga on pain and quality of life in women with endometriosis. The study included 90 participants who received either yoga or no treatment. The authors found that yoga was associated with a statistically significant reduction in pain intensity and improved quality of life.
Tai chi is a mind-body technique that involves slow, gentle movements and deep breathing exercises to promote relaxation and reduce stress levels. A systematic review published in the journal Pain Medicine in 2015 evaluated the effectiveness of Tai chi for managing chronic pain, including endometriosis. The review included ten studies involving a total of 494 participants. The authors found that Tai chi was associated with statistically significant reductions in pain intensity and duration and stress levels.
Diet and Nutrition
Diet modification can directly impact inflammation, hormone balance, and immune system function. While no specific diet has been shown to cure endometriosis, dietary changes, and nutritional supplements may be beneficial in reducing inflammation and pain associated with the condition.
Inflammation is a key factor in the development and progression of endometriosis. Certain foods and nutrients can contribute to inflammation in the body, while others have anti-inflammatory properties that can help to reduce inflammation. Omega-3 fatty acids, found in fatty fish such as salmon and mackerel, as well as in flaxseeds and chia seeds, have been shown to have potent anti-inflammatory effects. Magnesium, found in leafy greens, nuts, and whole grains, can also help to reduce inflammation and muscle tension. Vitamin D, found in fatty fish, eggs, and fortified dairy products, may help to regulate immune system function and reduce inflammation. Overall, the most anti-inflammatory antioxidant diet is whole-food plant-based.
Hormone balance is another important consideration in the management of endometriosis. Certain foods can help to balance hormones, while others can disrupt hormone balance and exacerbate symptoms. Phytoestrogens, found in foods such as soy products, flaxseeds, and lentils, can help to balance estrogen levels and reduce symptoms of endometriosis. On the other hand, foods high in saturated and trans fats, such as red meat and processed foods, can increase inflammation and disrupt hormone balance.
A systematic review published in the journal Nutrients in 2021 evaluated the effectiveness of dietary interventions for managing endometriosis. The review included 17 studies involving a total of 1311 participants. The authors found that dietary interventions, such as increasing intake of fruits and vegetables, omega-3 fatty acids, and phytoestrogens, and decreasing intake of saturated and trans fats, were associated with improved pain and quality of life, and other symptoms of endometriosis.
Supplements
Similar to diet, supplements may be beneficial in managing endometriosis by reducing inflammation, promoting hormonal balance, and supporting immune system function. While it is best to focus on transitioning to an anti-inflammatory, antioxidant diet, targeted supplementation may enhance the effect in some cases.
A randomized controlled trial published in the Journal of Reproductive Medicine in 2013 evaluated the effects of omega-3 fatty acids on pain and quality of life in women with endometriosis. The study included 59 participants who received either omega-3 fatty acids or a placebo. The authors found that omega-3 fatty acids were associated with a statistically significant reduction in pain intensity and improved quality of life.
A systematic review published in the European Journal of Obstetrics, Gynecology, and Reproductive Biology in 2017 evaluated the effectiveness of magnesium for managing menstrual pain, including endometriosis-related pain. The review included 13 studies involving a total of 1870 participants. The authors found that magnesium was associated with a statistically significant reduction in menstrual pain intensity and duration.
The study mentioned above also evaluated the effectiveness of vitamin D for managing menstrual pain, including endometriosis-related pain. The review included five studies involving a total of 238 participants. The authors found that vitamin D was associated with a statistically significant reduction in menstrual pain intensity and duration. Vitamin D supplementation is often essential because even in sunbelt areas of the world, up to 30% of the population is deficient.
It is important to note that supplements can have side effects and may interact with other medications, so it is essential to consult with a healthcare provider before using supplements for endometriosis.
Herbal Medicine
Herbal medicine, also known as herbalism, is the use of plants or plant extracts to treat or prevent disease. Many herbs have anti-inflammatory and pain-relieving properties, making them useful in managing endometriosis. While further research is needed to understand the effectiveness of herbal medicine for endometriosis fully, many women have reported positive outcomes from using herbal remedies as a complementary therapy.
Turmeric is one herb that has been suggested to effectively reduce inflammation and pain associated with endometriosis. Turmeric contains a compound called curcumin, which has potent anti-inflammatory effects. A randomized controlled trial published in the journal Complementary Therapies in Medicine in 2013 evaluated the effects of curcumin on pain and quality of life in women with endometriosis. The study included 67 participants who received either curcumin or a placebo. The authors found that curcumin was associated with a statistically significant reduction in pain intensity and an improvement in quality of life.
Ginger is another herb that has been suggested to be effective in reducing inflammation and pain associated with endometriosis. Ginger contains compounds called gingerols and shogaols, which have anti-inflammatory and pain-relieving effects. A randomized controlled trial published in the journal Pain in 2014 evaluated the effects of ginger on pain and menstrual symptoms in women with endometriosis. The study included 70 participants who received either ginger or a placebo. The authors found that ginger was associated with a statistically significant reduction in pain intensity and an improvement in menstrual symptoms.
Chasteberry, also known as vitex, is an herb that has been suggested to be effective in regulating hormones and reducing symptoms of endometriosis. Chasteberry contains compounds that can help to balance estrogen and progesterone levels, which can help to reduce inflammation and pain. A systematic review published in the journal Complementary Therapies in Medicine in 2018 evaluated the effectiveness of chasteberry for managing endometriosis-related pain. The review included six studies involving a total of 596 participants. Chasteberry was associated with a statistically significant reduction in pain intensity and duration compared to no treatment in this study.
Just as in the case of supplements, work with an expert in the field to avoid interactions with prescription medications.
Aromatherapy
Aromatherapy is a form of complementary therapy that involves using essential oils to promote health and well-being. Essential oils are concentrated plant extracts that are believed to have therapeutic properties. They can be used in several ways, such as inhaled, applied topically, or added to a bath.
While there is limited scientific research on the effectiveness of aromatherapy for endometriosis, some women with the condition have reported that it has helped to manage their symptoms. Aromatherapy may be particularly helpful for managing emotional symptoms, such as anxiety and depression, which are all too common.
A short list of essential oils that may be helpful for women with endometriosis includes Lavender, Clary sage, Rose, Peppermint, and Eucalyptus.
When using aromatherapy, it is important to dilute the essential oils with a carrier oil, such as coconut oil or almond oil, as they can be irritating to the skin when used undiluted. Aromatherapy should also be used with caution in women who are pregnant or breastfeeding, as some essential oils may not be safe for use during pregnancy or while breastfeeding.
Hyperbaric Oxygen Therapy (HBOT)
The theory behind using HBOT for endometriosis is that the increased oxygen levels in the body may help to reduce inflammation and promote the healing of damaged tissues. Some preliminary studies have suggested that HBOT may be effective in reducing pain and improving quality of life in women with endometriosis, although larger studies are needed to confirm these findings.
It is important to note that HBOT is not currently approved by the U.S. Food and Drug Administration (FDA) for the treatment of endometriosis, and it should only be used under the guidance of a qualified healthcare provider. There are also some risks associated with HBOT, including ear pain, sinus pressure, and oxygen toxicity, which can be serious in rare cases.
Summary
By addressing both the physical and emotional aspects of endometriosis, integrative therapy can help women to achieve a better quality of life and attach some of the suspected root causes of endo as well. This can include improvements in energy levels, sleep quality, and overall sense of well-being.
Integrative therapy is not a replacement for conventional medical treatment for endometriosis but rather a complementary approach that can be used in conjunction with conventional treatments to achieve better outcomes.
In conclusion, endometriosis is a complex condition that requires a multidisciplinary approach to treatment. Integrative therapy offers a promising addition to managing the symptoms of endometriosis by combining conventional medical treatments with complementary therapies that address the physical, emotional, and spiritual aspects of care.
Your endometriosis specialist can help guide you to practitioners who may be best suited for applying integrative therapies to endometriosis. It is ideal if you can find a specialist who is also certified in some aspect of East-West integrative medicine. These are hard to find but are out there.
Get in touch with Dr. Steve Vasilev
More articles from Dr. Steve Vasilev:
Endometriosis And Menopause; Everything You Need To Know
How to tell the difference between endometriosis and ovarian cancer
What would happen to the signs and symptoms of endometriosis after menopause?
References:
Manheimer E, Cheng K, Linde K, Lao L, Yoo J, Wieland S, Berman BM. Acupuncture for treatment of infertility: a systematic review. Obstet Gynecol. 2008;111(4):904-911. doi: 10.1097/AOG.0b013e31816a4c2c. PMID: 18378763.
Fernández-Martínez E, Onieva-Zafra MD, Parra-Fernández ML, et al. Effects of Massage on Pain, Anxiety, and Quality of Life in Patients With Endometriosis: A Systematic Review. J Nurs Scholarsh. 2019;51(6):614-623. doi:10.1111/jnu.12516
Soares TR, de Melo NH, de Lima Martins F, et al. The effectiveness of yoga in pain, menstrual disturbances, quality of life, and inflammatory markers in women with endometriosis: a systematic review. Complement Ther Clin Pract. 2021;44:101368. doi:10.1016/j.ctcp.2021.101368
Mira T, Mira N, Canadas D. Nutrition and endometriosis: therapeutic strategies. Biomed Res Int. 2015;2015:191461. doi: 10.1155/2015/191461. PMID: 26064937; PMCID: PMC4445933.
De Leo V, Musacchio MC, Cappelli V, Massaro MG, Morgante G, Petraglia F. Combined nutraceutical approach in the management of endometriosis-related pain. Minerva Ginecol. 2018;70(3):246-253. doi: 10.23736/S0026-4784.17.04057-9. PMID: 29243440.
Pan J, Dai Q, Zhang J, et al. Omega-3 fatty acids intake and risk of endometriosis: a systematic review and meta-analysis. Nutrients. 2018;10(10):1542. doi:10.3390/nu10101542
Sesti F, Caponecchia L, Pietropolli A, et al. Magnesium in the gynecological practice: a literature review. Magnes Res. 2017;30(1):1-7. doi: 10.1684/mrh.2017.0415. PMID: 28498078.
Amr MF, El-Mogy MM, Shams T, Vieira KSR, El-Masry SA. Vitamin D and Its Association with Endometriosis and Menstrual Pain: A Systematic Review and Meta-Analysis. J Clin Med. 2018;7(10):356. doi:10.3390/jcm7100356
Zhai B, Zheng W, Qi X, Tang K, Qin A, Lu J. The effectiveness of herbal medicine in the treatment of endometriosis: A systematic review. Complement Ther Med. 2017;34:81-96. doi: 10.1016/j.ctim.2017.07.006. PMID: 28917372.
Gottfried SF, Long B, Wittlake WA. Hyperbaric oxygen therapy for endometriosis: a systematic review. Undersea Hyperb Med. 2018;45(1):27-37. PMID: 29698797.
Kim TH, Lee HH, Ahn JY, et al. Effect of aromatherapy on symptoms of dysmenorrhea in college students: A randomized placebo-controlled clinical trial. J Obstet Gynaecol Res. 2018;44(6):1048-1054. doi: 10.1111/jog.13631. PMID: 29603750.
Gómez-Caravaca AM, Gómez-Romero M, Arráez-Román D, Segura-Carretero A, Fernández-Gutiérrez A. Advances in the analysis of bioactive compounds in functional foods. Curr Med Chem. 2011;18(33):5289-5302. doi: 10.2174/092986711798184194. PMID: 22023624.
Hwang JH, Han SM, Kwon YK. Short-term effects of aromatherapy massage on women with primary dysmenorrhea: a randomized controlled trial. J Altern Complement Med. 2009;15(7):731-738. doi: 10.1089/acm.2008.0368. PMID: 19552560.
de Sousa DP, de Almeida Soares Hocayen P, Andrade LN, Andreatini R. A systematic review of the anxiolytic-like effects of essential oils in animal models. Molecules. 2015;20(10):18620-18660. doi: 10.3390/molecules201018620. PMID: 26473827.
Han Y, Fan A, Bi X, Zhang Y, Wang S. The effect of hyperbaric oxygen therapy on endometriosis: A systematic review and meta-analysis. Medicine (Baltimore). 2019;98(49):e18199. doi:10.1097/MD.0000000000018199
Liu JP, McIntosh H, Lin H. Chinese herbal medicines for endometriosis. Cochrane Database Syst Rev. 2006;(4):CD006568. doi: 10.1002/14651858.CD006568. PMID

Endometriosis: What to Do After Diagnosis
Table of contents
If you’ve been diagnosed with endometriosis, you may wonder what your next steps should be. Here’s a quick overview of some things you can do after receiving a diagnosis of endometriosis.
Educate Yourself About Endometriosis
One of the best things you can do after an endometriosis diagnosis is to educate yourself about the condition. Knowledge will help you better understand your symptoms and give you an idea of available treatments. You can also ask questions about your diagnosis to your doctor or another healthcare provider.
Find an Endometriosis Doctor
When treating and managing endometriosis, all doctors are not the same. If you have or suspect you might have endometriosis, you should never just walk into the office of a random obstetrics/gynecology (OB-GYN) surgeon.
However, it can be tricky to find an endometriosis specialist who is highly skilled and follows the best treatment practices for this disorder. To learn more about endometriosis, read this article that introduces the condition, signs and symptoms, causes, complications, and treatments.
With so many myths about endometriosis (endo) – it’s essential to separate facts from fiction. Arm yourself with research and a solid foundation of knowledge to help you simplify the process and to get in touch with a trusted endo expert. Please keep reading to find out why using an endo expert is important, red flags your doctor/surgeon is not the right fit, and how to find an endometriosis specialist near you.
Talk to Your Doctor About Endometriosis Treatment Options
There is no cure for endometriosis, but there are treatments that can help lessen your symptoms and improve your quality of life. Some common treatments for endometriosis include excision surgery, medications for symptom management, and lifestyle changes. Talk to your doctor about which treatment or combination of options may be right for you.
Make Lifestyle Changes
Specific lifestyle changes can help lessen the symptoms of endometriosis. These include regular exercise, managing stress, and eating a healthy diet rich in fruits, vegetables, whole grains, and lean protein. Making these changes can help improve your overall health and well-being.
Join a Support Group
It can be helpful to talk to other women dealing with endometriosis. There are many online and in-person support groups available for women with endometriosis. Joining one of these groups can help you feel less alone and provide you with valuable information and support from others who understand what you’re going through.
If you’ve been diagnosed with endometriosis, you’re not alone. And there are things you can do to manage your symptoms and improve your quality of life. Educate yourself about the condition, talk to your doctor about treatment options, make lifestyle changes, and join a support group if possible. These steps will help you better cope with your diagnosis and live a fuller life despite having endometriosis.

Understanding and Finding Relief from Endometriosis Cramps
If you’re living with endometriosis, you’ve likely experienced the intense cramping and pain that comes along with it. Endometriosis is a chronic condition that can seriously impact your life with pain, cramps, and other symptoms. But there are ways to find relief and get back to living your life. Let’s review endometriosis cramps and how you can relieve endometriosis cramps.
Table of contents
What is Endometriosis?
Endometriosis is a chronic condition in which tissue similar to the lining inside the uterus grows outside of it. This tissue growth can cause severe pain and inflammation during menstruation and throughout the month. Common symptoms include painful periods, cramps, heavy bleeding, pelvic pain, infertility, and fatigue.
Endometriosis Cramps
Endometriosis cramps are most commonly present in the lower abdomen or pelvis. Patients describe the cramps as sharp and stabbing, severe gnawing or throbbing, and feel like their insides are being pulled down. Cramps might start before the period and last several days. Common causes of cramps include stress, inadequate sleep, and inflammatory foods such as alcohol and red meat.
Finding Support for Endo Pain Management
Living with chronic pain can be difficult for anyone, but resources are available for those with endo pain management needs. Local support groups are excellent options for those seeking community support from individuals who understand firsthand what they are going through. Many online communities also exist where individuals can share their experiences and offer support to one another while learning more about managing their condition on a daily basis. It’s important to remember that you don’t have to suffer alone if you are living with endo pain management needs—there are plenty of resources out there ready to help!
Managing Endometriosis Cramps
Getting rid of endometriosis cramps needs treating endometriosis and its inflammation. Besides excision surgery and medical management of endometriosis, which are the pillars of endometriosis care, lifestyle modification might have some benefits. Lifestyle habits that might be beneficial include regular exercise, stress management techniques like yoga or meditation, dietary changes such as avoiding processed foods or foods high in sugar or fat, getting enough sleep every night, and taking time for self-care each day. Please consult your doctor for the appropriate care for your cramps.
Endometriosis is a common chronic condition affecting many people worldwide each year. While there is no cure yet for this condition, there are ways to manage its symptoms, such as endo cramps through lifestyle changes, medication options as prescribed by your doctor, or even surgery if necessary. Additionally, online resources and local support groups provide invaluable community support for those living with this condition, so they don’t have to go through it alone! Whether you’re just beginning your journey towards finding relief from endo cramping or have been dealing with this issue for years, you deserve access to resources and care that will help make your life easier!

Patients Use These Strategies to Manage Endometriosis Flare-Ups
Endometriosis is a chronic condition that affects millions of women, causing pain and discomfort. Flare-ups are especially difficult and can be debilitating. Flare-up occurs when the symptoms become exacerbated. Flares amplify symptoms of the disease and ultimately decline after a while. Fortunately, some patients have found ways to cope with flare-ups to manage the pain and other symptoms. Let’s look at some strategies that others use for dealing with endometriosis flare-ups. Please notice that none of these discussions are medical tips.
Table of contents
What Causes Endometriosis Flare-Ups?
Flare-ups often occur when there is a trigger, such as hormonal imbalance, physical activity, stress levels, or certain environmental factors like heat or humidity. These triggers can lead to an increase in pain and discomfort for those affected by endometriosis.
Practice Relaxation Techniques
It can be hard to relax when you’re in the middle of an endometriosis flare-up. But relaxation techniques like meditation and deep breathing can help reduce stress levels and give your mind and body a much-needed break from the pain. If you’re feeling overwhelmed or anxious, try taking some slow breaths or focusing on an object in front of you until your mind calms down. You can also practice progressive muscle relaxation by tensing one muscle group at a time before releasing it. This relaxation will help release tension throughout your body while also helping to lower your heart rate and blood pressure.
Manage Your Stress Levels
Stress is known to trigger endometriosis flare-ups, so it’s important to find ways to manage your stress levels. Exercise is a great way to reduce stress and provide numerous other health benefits, such as improved mood, better sleep quality, and increased energy levels. Yoga is another great option as it combines physical activity with relaxation techniques which can be beneficial for managing endometriosis flare-ups. Other stress management strategies include talking about your feelings with someone who understands what you’re going through or writing in a journal about how you’re feeling.
Take Time for Yourself
When dealing with an endometriosis flare-up, it’s also important to take time for yourself, even if it’s just a few minutes each day! Do something that makes you happy, whether listening to music, reading a book, or watching your favorite movie – whatever brings you joy! Taking time out for yourself will give your mind and body a chance to rest and recharge.
Endometriosis flare-ups can be difficult, but some patients have found ways to cope with them that can make them more manageable. Taking some time out for yourself, practicing relaxation techniques such as meditation or yoga, exercising regularly, managing stress levels effectively, and talking about how you feel are all effective strategies for dealing with endometriosis flare-ups. By taking these steps consistently, people with endometriosis might manage their flares up more easily!

What to Expect Before and After Endometriosis Surgery
Endometriosis is a condition that affects millions of people worldwide. As a result, many patients opt for endometriosis surgery to manage the symptoms and reduce the discomfort associated with the disease. If you’re considering endometriosis surgery, you may have questions about what to expect before and after the procedure. Let’s dive into the details.
Table of contents
What Happens Before Endometriosis Surgery?
Your doctor will likely perform some tests before scheduling your surgery, including imaging tests such as an ultrasound or MRI and hormone tests to check your estrogen levels. Your doctor will also take a medical history and discuss your current symptoms to better understand how your endometriosis has progressed. It’s essential, to be honest about medications, allergies, and other health conditions that could affect your treatment options or surgical outcome. There will also be a physical exam, including a pelvic exam. Your doctor tries to learn your body and pinpoint any tumors, pain, or abnormality during this physical exam. The result of that physical exam might guide the surgery strategy.
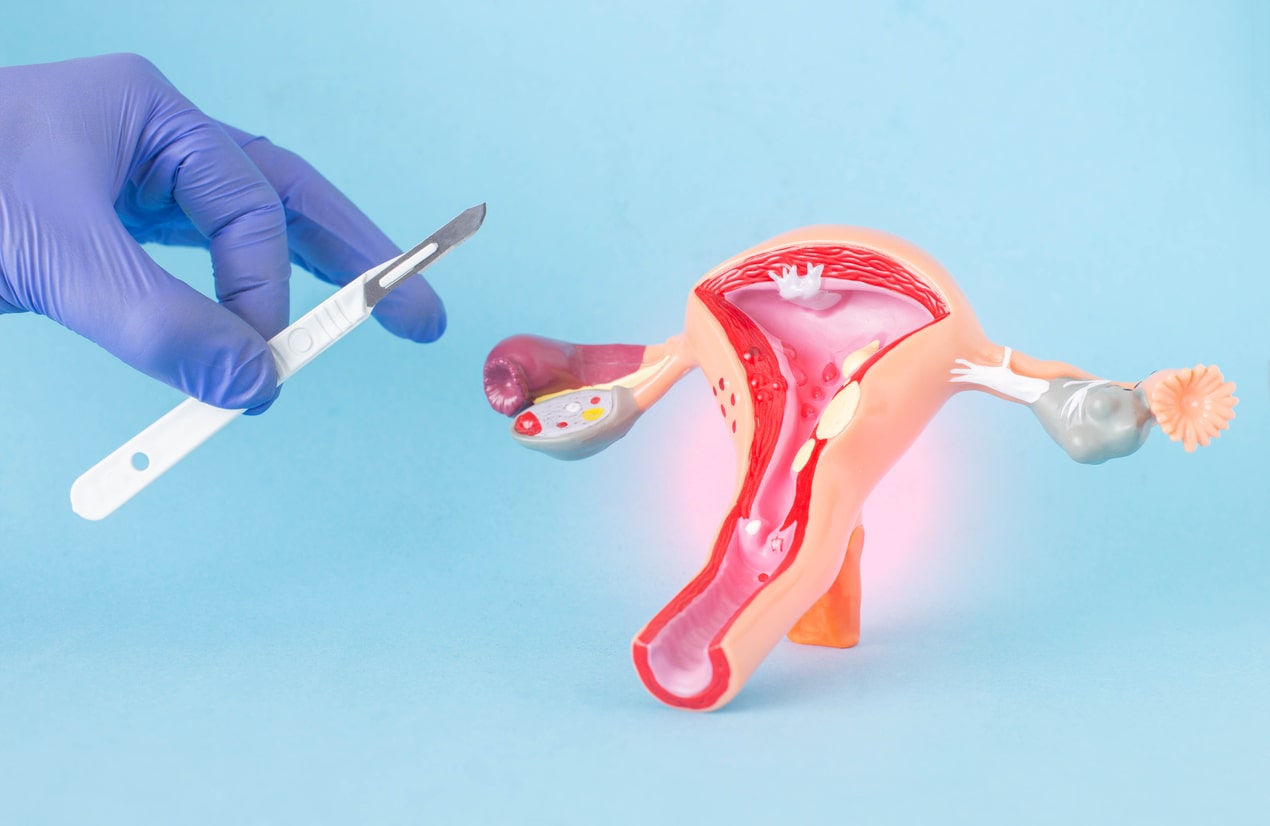
What Happens During Endometriosis Surgery?
This surgery often needs general anesthesia, so doctors put you to sleep during the surgery. Endometriosis surgery is typically performed laparoscopically or with a robot. That means your surgeon will make three to four small incisions in the abdomen and pelvic area. Then they insert a surgical tool with a tiny camera to help them see inside your body during the procedure. The primary goal of endometriosis surgery is to remove any areas of abnormal tissue or scarring caused by endometriosis growth while preserving healthy tissue as much as possible. Depending on the severity of your condition, the surgeon may remove specific organs partially or entirely to reduce pain and improve fertility outcomes. Your surgeon should discuss these possibilities and ask for your consent before surgery.
What Happens After Endometriosis Surgery?
After your surgery, it’s important to rest for several days or weeks so your body can heal properly. Your doctor may prescribe medications to help manage pain or inflammation during the post-surgical period. You must take these medications exactly as prescribed to minimize potential complications. You should also avoid strenuous activities such as heavy lifting or running during recovery; instead, with your doctor’s permission, stick with light exercises like walking or yoga until your doctor clears you for more demanding activity levels.
Endometriosis is a common condition among patients, but it doesn’t have to impede their quality of life. With modern treatments such as endometriosis surgery, patients can find relief from their symptoms while still preserving healthy tissues whenever possible. It’s crucial for those considering endometriosis surgery to understand what happens before, during, and after the procedure to know what steps they need to take to ensure successful recovery afterward. With proper preparation and informed decision-making about treatment options, you can have less anxiety during this period and get back on track with living your life after surgery.

Managing Endometriosis: What You Need to Know
Table of contents
Endometriosis is a common condition that occurs when tissue similar to the interior layer of the uterus grows outside the uterus. These pathologic tissues respond to hormones, nutrition, lifestyle, and stress level. Endometriosis can cause pain, fatigue, other symptoms, and infertility. Fortunately, there are several ways to manage endometriosis and reduce its effects on your life. Let’s look at what you need to know about managing endometriosis.
Can endometriosis be cured completely?
Hormonal Therapy for Endometriosis Management
Hormonal therapy is one of the most common treatments for endometriosis management. Hormones like progestins and birth control pills work by suppressing ovulation and reducing estrogen levels in the body, which helps reduce the growth of endometriosis tissue. While this treatment may not be suitable for everyone, it can effectively reduce pain and other symptoms associated with endometriosis. But it is not a cure or a permanent solution. You might feel better if you take hormonal therapy, and endometriosis symptoms most likely come back whenever you stop the medication.
Surgery for Endometriosis Management
Surgery may sometimes be the best choice to treat endometriosis and alleviate its symptoms. Endometriosis surgeons use laparoscopes or robots to remove most endometriosis and adhesions or cysts. After surgery, your doctor may also prescribe hormonal therapy to help keep the condition under control. Your endometriosis surgeon might also recommend physical therapy before or after surgery to help manage symptoms and regain your functions.
Physical Therapy for the Management of Endometriosis
Physical therapists can have a significant impact on your life with endometriosis. They can help you know your body better and understand your limitations. A physical therapist or occupational therapist might be a great resource if you have any pelvic area spasms or movement limitations because of endometriosis pain.
Physical Therapy Before Excision Surgery for Endometriosis
Physical Therapy after excision surgery
Questions to Ask Your Physical Therapist When you have endometriosis
Dietary Changes for Endometriosis Management
Making dietary changes can also help manage endometriosis symptoms and reduce inflammation in your body. Eating fruits and vegetables—especially those rich in antioxidants—can help reduce inflammation and improve overall health. Avoiding processed foods and refined sugars can also help lessen symptoms associated with this condition. You need a dietitian to help you with this dietary planning.
Lifestyle Changes for Endometriosis Management
More body fat can mean higher estrogen and higher inflammation levels. Therefore, some healthy changes in your lifestyle to optimize the fat storage in your body can positively impact endometriosis management and symptoms. These changes can mean more physical activity or less junk food, or else. You are the best person to decide what lifestyle you should pursue. Moreover, a healthy lifestyle can improve your mental health and quality of life.
People with endometriosis should talk to their doctor about treatment options that are right for them to manage their condition effectively. In many cases, combining hormonal therapy, surgery, lifestyle, physical therapy, and dietary changes can help reduce pain and other symptoms associated with this condition. The goal should be for you to live a fuller life free from endometriosis effects. With proper management strategies, people with endometriosis can live healthier lives despite their diagnosis!
Find the best endometriosis specialists around the world!

Endometriosis Excision Surgery: What You Need to Know About
Endometriosis is a gynecological condition that affects approximately 10% of women between 15-55. It can cause chronic pain, infertility, and other issues. It happens when a similar tissue to tissue that lines the uterus grows outside of the uterus. One way to manage endometriosis is through endometriosis excision surgery. Let’s take a deeper look into what this surgery involves.
Table of contents
The Procedure
Endometriosis excision surgery is a procedure in which a gynecologist uses specialized tools and techniques to remove endometriosis tissue from the pelvis, abdomen, and other regions. Excision means removing the tissue from organs near the uterus, such as the ovaries, fallopian tubes, bladder, rectum, or intestines. The doctor will remove any adhesions (scar tissue) causing pelvic pain or threatening fertility. The surgery requires an outpatient surgery center or a hospital operating room.
Benefits of Endometriosis Excision Surgery
Endometriosis excision surgery aims to reduce or eliminate the pain caused by endometriosis growths, improve fertility outcomes for those who want children, and prevent new growths from developing. In some cases, patients can experience improved symptoms after just one procedure; however, some patients may need multiple surgeries. This need for repeat surgeries depends on the surgeon’s experience, disease behavior and severity, and some unknown factors.
Precautions to Take Before Surgery
Before undergoing endometriosis excision surgery, you should speak with your doctor about any concerns about anesthesia or other risks associated with the procedure. Additionally, depending on the severity of your condition and your treatment goals (fertility vs. symptom relief), other treatments may need to be considered before considering surgical intervention.
Talk with your doctor first to ensure that endometriosis excision surgery is right for your needs. If you have questions about this procedure or any other treatments available for managing endometriosis symptoms, don’t hesitate to reach out to your healthcare provider today! They will help you determine if endo excision surgery is a good option.
Have you considered endometriosis excision surgery? What is your most burning question about endometriosis excision surgery?

A Guide to Endometriosis Surgery and Its Success Rate
Endometriosis is a condition in which tissue similar to the uterine lining grows outside the uterus. Endometriosis can cause pain, heavy bleeding, and infertility. Women seeking relief from endometriosis symptoms and want to maintain their fertility consider surgery an option. This guide will discuss the types of endometriosis surgery available and their success rates.
Table of contents
Types of Endometriosis Surgery
Two types of endometriosis surgery are available: minimally invasive (laparoscopy and robotics) and open abdominal surgery. In a minimally invasive procedure, a thin tube with a camera and tiny surgical instruments are inserted into the abdomen through small incisions in the belly area. During the minimally invasive procedure, surgeons can remove or destroy endometriosis tissue with lasers or other tools. Open abdominal surgery involves making a wide incision in the abdomen to access any affected areas directly and remove them surgically. Most top surgeons with significant experience prefer minimally invasive surgeries with laparoscopy or robotics.
Success Rates
The success rate of endometriosis surgeries depends on factors such as the severity of symptoms, type of procedure performed, and experience of the surgeon performing the procedure, etc. Patients can achieve complete or partial relief in complaints in up to 93.2% of cases with surgery. And 65% of those wishing for pregnancy but were unsuccessful in the past, could conceive after surgery. Some experts believe success rate increases when additional treatments such as hormone therapy or medications are used following surgery to reduce recurrence risk. But hormonal therapy after surgery is not an option if you plan to conceive right after recovery. Minimally invasive surgery is superior to open surgeries because it results in lower risk of surgical complications, such as bleeding, infection and damage to other abdominal organs. Minimally invasive procedure also offers faster recovery compared to open surgery.
Endometriosis can cause significant physical discomfort and emotional distress for individuals living with it. However, fortunately, some treatments can relieve painful symptoms while still allowing to maintain fertility if desired. Surgery is one such treatment option and provides varying levels of success depending on factors such as experience level, the severity of the disease, and the type of procedure used. Studies have found that up to 93% of patients report partial or complete decreased pain after undergoing endometriosis surgery. And 65% of patients achieved pregnancy after surgery. Talk with your doctor if you think you are suffering from this condition. Discuss testing options and treatment plans, including surgical interventions, so that you can take control of your health today!
Featured specialists:

Laparoscopy: A Common Treatment for Endometriosis
Endometriosis is a common condition that mainly affects women of reproductive age. It occurs when tissue similar to the uterine lining grows outside the uterus, typically on other organs in the pelvic area. One of the most common treatments for endometriosis is laparoscopy, a minimally invasive surgical procedure used to diagnose and treat the disorder. Let’s take a closer look at what this procedure entails.
Table of contents
How Laparoscopy Works
During a laparoscopy, your doctor will insert a thin, lighted tube called a laparoscope through small incisions in your belly. The laparoscope allows your doctor to see inside your abdomen and pelvis and identify areas of endometriosis tissue growth. In some cases, they may also use laparoscopic tools to remove any abnormal tissue growth they find during this process.
This procedure can be performed in several ways. Your doctor may perform it under general anesthesia, where you are completely asleep during the operation. Depending on what your doctor finds during the laparoscopy, they may perform additional procedures, such as removing cysts or scarring caused by endometriosis.
Recovery from Laparoscopy
The recovery time after a laparoscopic surgery depends on several factors, including how extensive the procedure was and how long it took to complete. Most people return home within 24 hours after having this done and can expect to recover fully within two to six weeks with minimal pain or discomfort afterward. You should follow all your doctor’s post-operative instructions, including taking medications as prescribed and avoiding strenuous activities like heavy lifting until your healthcare provider clears you to resume normal activities.
Laparoscopies can be an effective way to diagnose and treat endometriosis in women of reproductive age. This minimally invasive surgical procedure involves inserting thin, lighted tubes into incisions on your belly to identify areas of endometrial tissue growth that could be causing pain and other symptoms. While recovery time varies depending on the procedure’s extent, most people can return home within 24 hours and resume their normal activities within two weeks or so with minimal pain or discomfort afterward. If you think you may have endometriosis, talk to your healthcare provider about whether laparoscopy works for you!

Endometriosis Surgery Risks
Endometriosis is a condition that affects millions of women around the world. Endometriosis occurs when tissue similar to the tissue found in the uterus grows outside the uterus. This can create intense pain and other health complications, such as infertility. While surgery may be an option for some, it is essential to understand the risks associated with endometriosis surgery before making a decision.
Table of contents
Types of Surgery for Endometriosis
Several types of surgeries exist to treat endometriosis, including minimally invasive (laparoscopy or robotics) and open surgery (laparotomy.) Minimally invasive surgery typically involves making small incisions in the abdomen so that a camera can be inserted into the body to view abnormal endometriosis growths or lesions. Laparotomy involves a larger incision and allows for more extensive examination and treatment. Almost all top endometriosis surgeons worldwide prefer minimally invasive surgery vs. open surgery.
Risks Associated With Endometriosis Surgery
As with any surgery, there are risks associated with endometriosis surgery. These include bleeding, infection, and nerve damage due to surgery or anesthesia during the procedure. During surgical procedures, there is also a risk of harm to surrounding organs such as the bladder or bowels. Additionally, there is a risk that a surgeon will not remove all of the endometriosis tissue during surgery. This incomplete removal could lead to recurrent symptoms or disease if not appropriately addressed by your doctor post-surgery.
Other Treatment Options for Endometriosis
Suppose you are concerned about undergoing surgery for your endometriosis. In that case, other treatment options are available such as hormone therapy or medications used to reduce pain and inflammation caused by endometrial growths or lesions. Additionally, lifestyle changes such as exercise and diet might help reduce endometriosis’s associated symptoms without requiring surgery. Speak with your doctor about other options that may work best for you before deciding on any procedure related to your endometriosis diagnosis.
Find the best endometriosis specialists around the world:
Endometriosis Surgery Costs: Everything You Need to Know
Endometriosis is a chronic gynecological disorder that affects many women. One of the treatments for endometriosis is surgery, which can be expensive. This post will discuss what endometriosis surgery costs and how you can manage these costs.
Table of contents
Endometriosis Surgery
Endometriosis surgery needs minimally invasive tools such as laparoscopy and robotics. The endometriosis surgery usually includes a general anesthetic to reduce pain and discomfort during the procedure. Surgery removes endometrial tissue, scar tissue, and other growths from around the uterus and other organs in the pelvic region. This type of surgery can cost anywhere from $2,500 to $7,500. The cost depends on where you perform the surgery, how severe your endometriosis is, and how long it takes to complete the procedure.
How You Can Manage Endometriosis Surgery Cost?
Other options are available if you don’t have insurance coverage or if your insurance does not cover the cost of endometriosis surgery. Some hospitals offer payment plans or discounts if you pay all or part of your bill upfront. You may also qualify for financial aid programs or grants provided by local organizations or charities that help cover medical expenses for those with limited incomes. Additionally, some states assist with Medicaid programs that can help cover some or all of your medical costs related to endometriosis treatment.
It would be best if you spoke with your doctor about your options before deciding which route to take in terms of paying for endometriosis surgery. Your doctor can recommend a hospital that offers discounted rates or a payment plan that makes it easier for you to manage costs associated with treatment. Many healthcare providers also offer free consultations so you can discuss possible treatment options without any additional cost upfront.
Taking care of your body should never come at a heavy price tag — but unfortunately, endometriosis surgery can be costly. That doesn’t mean there aren’t ways to manage those costs, though! From payment plans to financial aid programs and even grants from local organizations, plenty of resources are available if you need help paying for endometriosis-related medical expenses. Talk with your doctor about your options before making any decisions. With the right resources, getting the care you need shouldn’t feel out of reach!
What is your experience about dealing with surgery costs and finding resources?
Featured Specialists

Physical Therapy After Excision Surgery
Table of contents
Why do You Get a Referral for Physical Therapy After Excision Surgery?
- Endometriosis is a chronic condition and it takes almost 10 years to diagnose the condition in most cases.
- The women suffer from severe pain and disability before they are really diagnosed with endometriosis. Pain leads to muscle guarding and spasms which leads to further limitation in mobility and function.
- Muscle guarding can also affect fascial mobility. Fascia covers our body from head to toe, it covers the muscles and organs and connects muscle to muscle and muscle to organ. Any fascial restrictions can affect the mobility of the organ and body and also function.
- Decreased mobility can affect the circulation and lymphatic draining. Many women present with blood stasis and swelling of pelvic region- vulva, discoloration and sometimes itching.
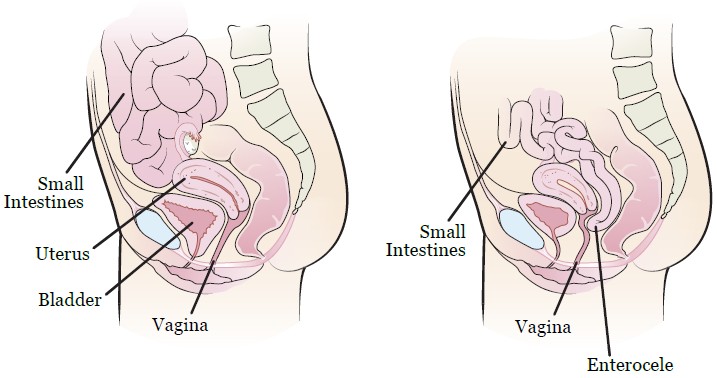
- Some women with endometriosis can present with the descend of a small intestine between uterus and rectum and it pushes the wall of vagina, it is called “enterocele”.
- Surgery can lead to scar tissue and muscle guarding which can affect the normal biomechanical movement.
- Many women have pain and pelvic floor dysfunction after surgery which can affect the function.
How does Fascial Mobility Affect the Pelvic Floor Function?
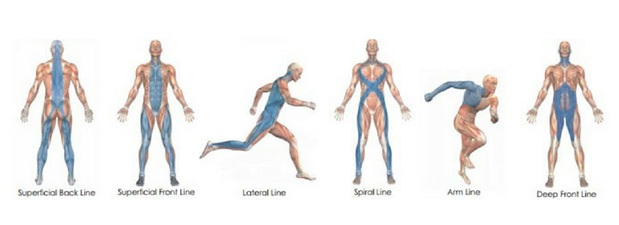
- Facia lines from Amygornall.com
- The abdominal fascial restrictions from guarding can affect the mobility of the fascia of the large and small intestine. Scar tissue after surgery can also affect the abdominal fascial mobility.
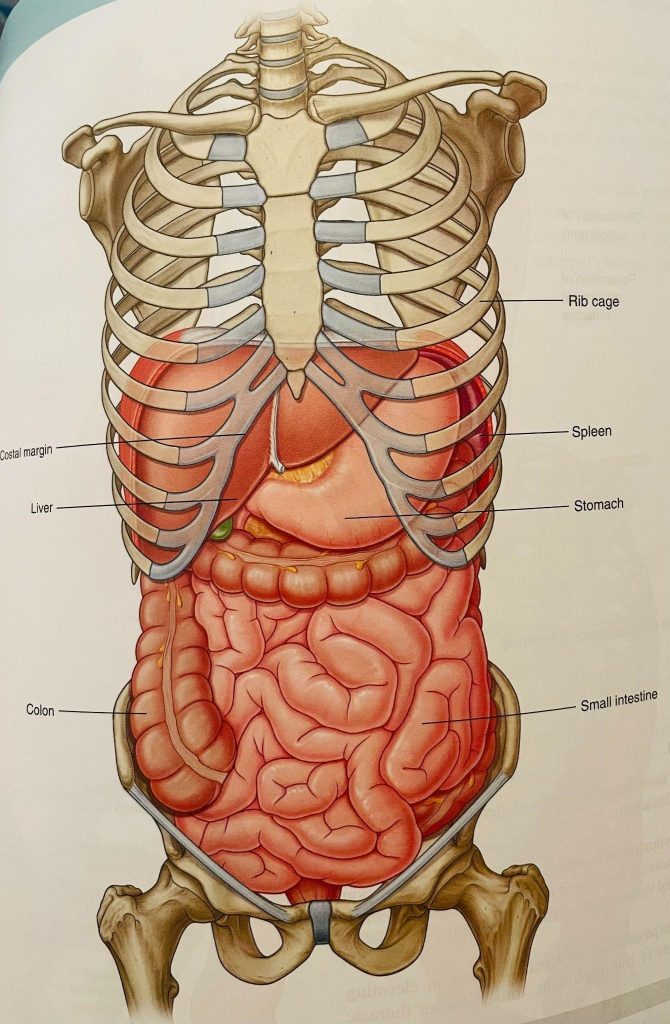
- This is image is taken from Grey’s Anatomy
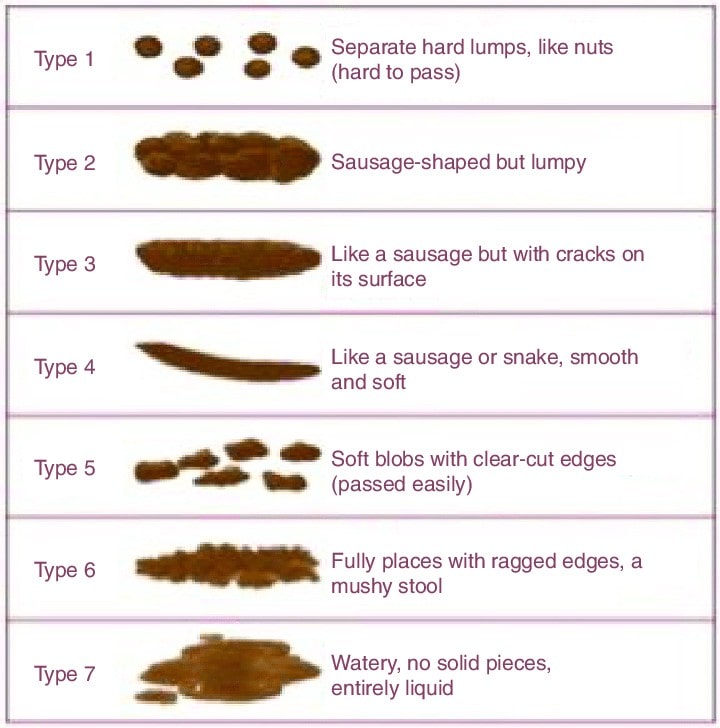
- The restrictions of the fascia around cecum (ascending colon on right side) and sigmoid colon (descending colon on left side) can affect bowel movement- many women have constipation, diarrhea, pain after bowel movement, bloating, and food intolerance. Constipation is defined as
- Small palates, hard stools, straining
- Not able to empty bowels completely
- Less than 3 spontaneous bowel movements a week
- The patient has to do manual maneuver to pass the stool
- Straining with stools can lead to pelvic floor dysfunction and increase the risk of prolapse
- Bristol stool scale helps to understand the consistency of stool and relation to constipation. As if you have bowel movement everyday does not mean you are not constipated. Bristol stool scale 1-2 is considered as constipation, 3-4 is considered as normal bowel movement as long as the person is not straining while doing bowel movement, 5-7 is considered as diarrhea
The restrictions of fascia around the bladder can cause
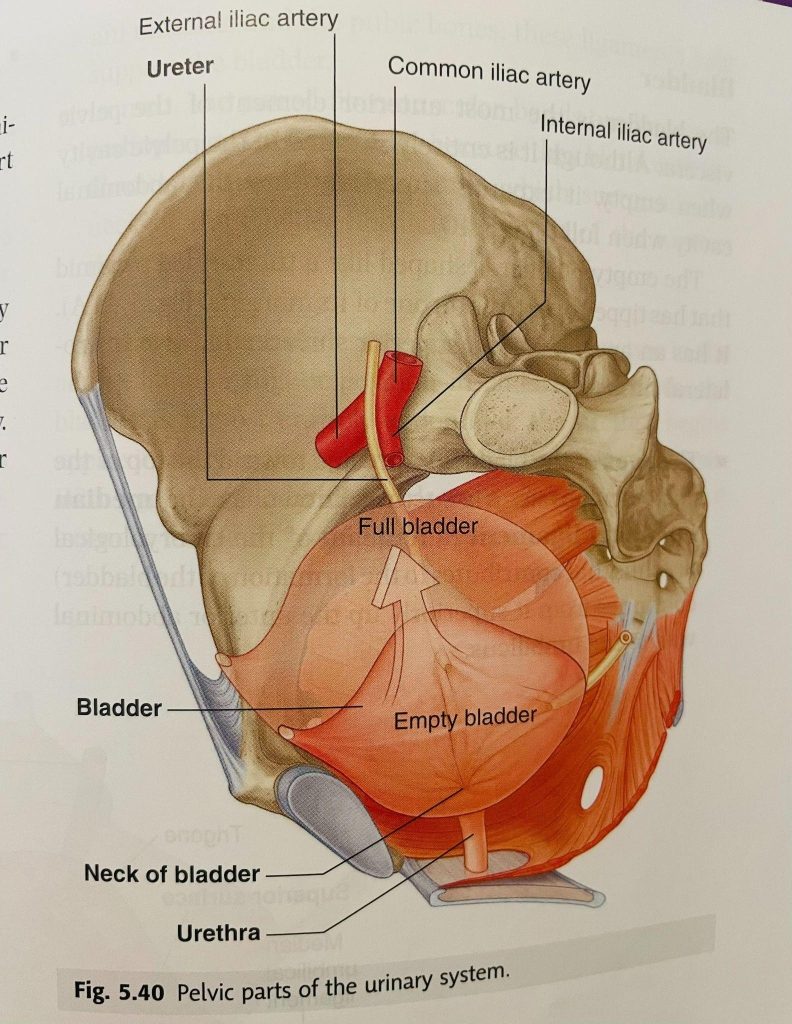
The image is taken from Grey’s Anatomy
- Increase in urinary urgency and frequency
- Bladder fascia shares the fascia with pelvic floor through urethra and it can cause stress/urge or both urinary incontinence.
- Bladder fascia also shares the fascia with obturator foramen where obturator internus muscle attaches. Obturator internus muscle is one of the major rotator muscles of the hip. Restrictions of bladder fascia can affect the mobility/mechanics of the hip and also can cause pain. Many women with hip pain without any pathology might have a connection to the bladder fascia. They always have one of the bladder symptoms such as urgency/frequency/burning of urination or incontinence.
- Anatomically small intestine sits on the bladder. The small intestine moves up and allows the bladder to fill. If the fascial mobility of the small intestine is limited or if the small intestine has descended, the bladder does not get enough room to fill and that leads to increase in urgency and frequency.
- The image is taken from Sloan Kettering Institute – research
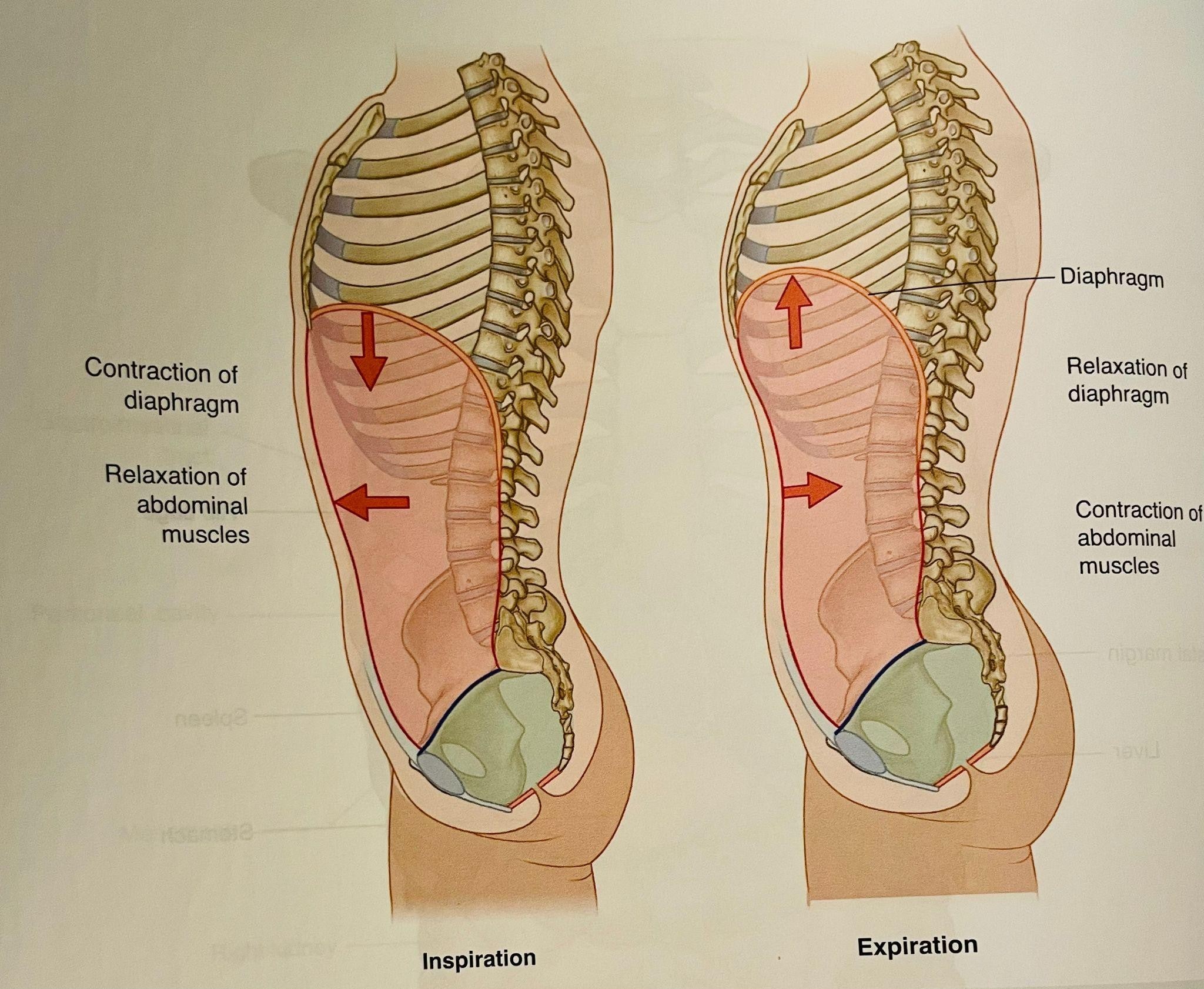
- The diaphragm and pelvic floor work as a piston during the breathing. When we breathe in, the diaphragm moves down along with the pelvic floor and when we breathe out they both move up. Breathing mechanics is very important for pressure mechanics- that means it provides stability, keeps the organ continence, pelvic floor function, lymphatic draining, and reduces the strain on joints. The factors can affect the breathing mechanics
- Abdominal fascial restrictions
- Shallow breathing from pain
- Decreased mobility of fascia of diaphragm/pelvic floor
- The image is taken from Grey’s Anatomy
- The restriction of fascia can affect the circulation and lymphatic drainage. Many women have pelvic congestion and also swelling of vulva and itching.
How can Physical Therapy help?
Goals of Physical Therapy are
- Reduction of pain
- Improve posture
- Improve mobility of muscle/fascia and organ to improve biomechanics and movement of the body
- Improve circulation and lymphatic drainage
The Physical Therapist have to perform detailed evaluation on fascial mobility, joint mechanics, muscle guarding pattern, posture, any swelling or signs of congestion, bowel and bladder function, sexual function, pelvic floor muscle function, lumbar spine/sacroiliac joint mobility and stability, breathing mechanics, load transfer, and central sensatization. I have found great success with fascia mobilization on abdomen/chest wall/diaphragm, and around the abdominal organ/pelvic floor muscles to reduce pain, improve mobility, circulation, breathing mechanics, bowel/bladder function and overall well being.
About the author
The author of this article, Neha Golwala, PT, DPT is a vetted endometriosis physical therapist. With more than 10 years of experience, she works at Zuppa Physical Therapy P.C. in New York. Neha uses manual therapy techniques including myofascial release, joint mobs, and neurominetic energy. She is an expert in the development of posture awareness and connecting mind to body to recover from injuries and prevent injuries and improve performance.

