
Does Endometriosis Cause Bowel Problems
Endometriosis, a chronic medical condition that affects up to 10% of women worldwide, has a significant impact on various aspects of a woman’s life, including her bowel health. This article will explore the question:
“Does endometriosis cause bowel problems?”
and delve into the symptoms, causes, diagnosis, and treatment of this condition.
Table of contents
- What is Endometriosis?
- Endometriosis and Bowel Problems
- Recognizing the Symptoms
- Bowel Endometriosis: Causes and Risk Factors
- Diagnosing Bowel Endometriosis
- Treatment Options for Bowel Endometriosis
- Post-Surgery Recovery and Follow-up
- The Impact of Delayed Treatment
- The Importance of Specialist Care
- Conclusion
What is Endometriosis?
Endometriosis is a medical condition in which tissue resembling the endometrium, the lining of the uterus, grows outside of the uterus. This tissue can grow on various organs, including the ovaries, fallopian tubes, bladder, and even the bowel.
Endometriosis and Bowel Problems
Endometriosis can affect the bowel in various ways, leading to numerous digestive issues. Specifically, endometriosis can grow on or inside the bowel walls, causing symptoms that are often mistaken for other conditions like Irritable Bowel Syndrome (IBS).
Superficial and Deep Bowel Endometriosis
Bowel endometriosis can present in two forms:
- Superficial Bowel Endometriosis: This is when endometriosis is found on the surface of the bowel.
- Deep Bowel Endometriosis: This form of endometriosis penetrates the bowel wall.
In some cases, rectovaginal nodules can start as superficial endometriosis and progress to infiltrate the bowel wall.
Read More: Can Endometriosis Cause Bowel Issues?
Recognizing the Symptoms
The symptoms of bowel endometriosis are similar to those of IBS. However, they can vary with the menstrual cycle, worsening in the days before and during a period. Some common symptoms include:
- Pain with defecation (dyschezia)
- Deep pelvic pain during sex (dyspareunia)
- Rectal bleeding during a period
If you experience these symptoms, it’s crucial to discuss them with your doctor. They may choose to use several techniques for diagnosis, such as a vaginal examination, ultrasound, sigmoidoscopy, laparoscopy, CT, or MRI scan.
Bowel Endometriosis: Causes and Risk Factors
While the definitive cause of endometriosis remains unknown, several potential contributing factors include hormonal imbalances, immune system problems, and genetic factors. Researchers have also found links to genes and stem cells, inflammation, and estrogen levels.
Read More: What Does Bowel Endometriosis Feel Like? Understanding the Pain and Symptoms
Diagnosing Bowel Endometriosis
Diagnosing bowel endometriosis can be challenging due to its similarities with other conditions like IBS. In addition to a physical examination and medical history review, doctors may suggest imaging tests such as transvaginal or transrectal ultrasound, magnetic resonance imaging (MRI), laparoscopy, or barium enema.
Treatment Options for Bowel Endometriosis
The treatment for bowel endometriosis typically involves a combination of painkillers, hormone treatments, and surgeries, depending on the severity of the symptoms. Surgery is usually recommended for bowel endometriosis, with the surgical options varying based on the severity of the condition and the areas affected.
There are three main surgery options for bowel endometriosis:
- The affected segment of the bowel is removed, and the bowel is rejoined (re-anastomosis).
- For smaller areas of endometriosis, the disc of affected bowel is cut away, followed by the closure of the hole in the bowel.
- Affected areas can be “shaved” off the bowel, leaving the bowel intact.
Post-Surgery Recovery and Follow-up
Recovery after any surgery varies depending on the individual. After laparoscopic bowel surgery, you can generally expect to go home within four days. Bowel function may be altered after surgery, particularly with a full resection (re-anastomosis). This does improve over time, although watching your diet to see which food aggravate or improve the situation may be helpful.
The Impact of Delayed Treatment
If bowel endometriosis is not treated properly and promptly, the disease may progress, and quality of life significantly decreases. Small lesions on the bowel can eventually progress and become full-thickness lesions that cause obstruction and may require major bowel surgery.
The Importance of Specialist Care
Because bowel endometriosis deals with your gastrointestinal system, it’s usually not solely treated by a general gynecologist. A collaborative care approach between an endometriosis expert, gastroenterologist, and/or general surgeon may be necessary to treat your bowel endometriosis from all angles.
Read More: Finding an Excision Specialist: What you Need to Know
Conclusion
Understanding the link between endometriosis and bowel problems is vital for improving diagnosis and treatment outcomes. If you’re experiencing symptoms of bowel endometriosis, it’s important to discuss them with your doctor and consider seeing a specialist. In doing so, you’ll be taking an important step towards managing your symptoms and improving your quality of life.
References:
https://www.endometriosis-uk.org/endometriosis-and-bowel
https://www.webmd.com/women/endometriosis/bowel-endometriosis
https://www.everydayhealth.com/endometriosis/bowel-endometriosis/
Endometriosis and constipation
https://drseckin.com/bowel-endometriosis/

Endometriosis Supportive Therapy: Can Endometriosis Be Treated Without Surgery?
Endometriosis is an extremely painful chronic condition, which often also leads to infertility or subfertility, that affects about ten percent of women worldwide. It is characterized by growth of endometrial-like tissue, which normally lines the inside of the uterus, outside of the uterus on pelvic organs, the abdomen, bowel, and beyond. This tissue is not the same as the endometrium, characterized by very different behavior and unique molecular profiles.
Eventually, personalized “theranostic” (therapy and diagnostic) tools will exploit these unique molecular profiles and lead to far better diagnosis, therapy and monitoring approaches. Research is accelerating in this area, which is already very pervasive in other diseases such as cancer and various immuno-inflammatory conditions. Meanwhile, the only therapies that are available to actually treat endometriosis, not just masking of symptoms, are hormonal options and excisional surgery. However, there are major limitations to the argument that hormonal therapies work very well to treat endo rather than simply reduce symptoms. That leaves surgery.
So, in a word, “can endometriosis be treated without surgery?”, the answer is a resounding NO! That is not to say that hormonal and other treatments, including anti-inflammatory and perhaps anti-histamine agents (e.g. Zyrtec), both mainstream and integrative-holistic, don’t help. They might. Let’s unpack this a little bit to give you a roadmap of the options.
Table of contents
Understanding Endometriosis
The exact cause of endometriosis is technically unknown, but we know it is influenced by genetic, genomic, hormonal, immunologic and environmental epigenetic factors. In other words, it is “multi-factorial”. This means the reason you may have endo could be different from why your friend or even your sister does. Endo can also behave very differently because different factors are probably in play in different people. This makes a “standard treatment” hard, if not impossible, to recommend to any given patient. This is changing with the advent of endometriosis bio-molecular pathway research, which will lead to highly individualized targeted treatments. But this is not part of what is available today.
Diagnosis of Endometriosis
Diagnosing endometriosis is very challenging, because the symptoms can mimic other conditions. This is part of the reason that diagnosis is often delayed by 5-10 years and intentional or inadvertent gaslighting is rampant, depending on which specialist was consulted. The doctor may be looking at you through a general practice medical lens, or intestinal, urologic, neurologic or other lenses in forming their opinions.
Rule # 1 is to listen to the patient. This is almost never done to an appropriate extent. Why? Because today’s medical system limitations often lead to five-to-ten-minute visits with a semi-interested and overworked provider who is likely under-informed regarding endometriosis.
When rule #1 is broken, an appropriate evaluation and testing is not likely to be done. Ideally, a clinical suspicion leads to testing that may include ultrasound or MRI, various blood tests, testing for associated conditions and so on. None of these will reliably lead to a diagnosis of endo but can lead to appropriate specialist referrals to get to the root cause of pain, such as endo.
Rule #2 in medicine, in general, is to get a diagnosis before recommending treatment. This is because treatments can be ineffective when treating the wrong condition or, worse, can lead to complications and side effects. Unfortunately, in the author’s strong opinion, this is often violated specifically in endometriosis treatment. A common standard is to offer hormonal therapy to patients to see if it might work because the diagnosis might be endometriosis and endo is, in part, fueled by hormones. This may or may not be reasonable depending upon individual circumstances and choices.
This brings us to rule #3, that we’ll cover next, which proposes that patients should be offered treatment options to select from after informed consent about the potential risks vs the potential benefits based on the best possible scientific evidence. This is not always done very well and certainly depends on the “trust factor” with your selected specialist(s), since scientific evidence is subject to interpretation. Most patients do not realize this.
Conventional Treatment of Endometriosis
Traditional treatment for endometriosis often involves medication or surgery. Medications can include anti-inflammatory pain relievers and hormonal therapies. In the near future medications will include targeted biomolecular non-hormonal therapies, but they are not here yet. Pain relievers are mainly a symptom reducing band-aid and are not intended to treat, so we will not discuss them here either. They can certainly help in overall management, but we will focus on “treatment” in this article.
Hormones aim to either shut down ovarian function (in other words, cut off estrogen) or at least regulate the menstrual cycle, and progesterone analogs, to potentially reduce the growth of endometriosis tissue.
Surgery is used for definitive diagnosis of endo as well as treatment by removing any lesions or implants that are found. In some cases, the two modalities can be used hand in hand, but the order in which they are used, and the nature of the proposed hormonal therapy are important considerations.
Hormonal Treatment
International guidelines are very confusing and inconsistent regarding hormonal therapy for endometriosis. Because of this, recommendations can vary between practitioners. We won’t delve into all these options here, but the following are excellent summary articles on this important topic.
The important points to consider are as follows:
- The ONLY way currently to definitively diagnose endometriosis is through biopsy, usually performed during surgery.
- Starting treatment that can cause extreme side effects and potential long-term harm without first getting a definitive diagnosis seems imprudent. So, if a practitioner offers hormones because they “think” you have endo based on history, examination and perhaps some scans, at least get a second opinion from an endometriosis specialist. This approach is within international guidelines but can cause you a world of misery and potential harm if not managed in expert hands.
- Hormone therapy for endo boils down to either reducing estrogen levels or eliminating estrogen altogether or increasing progestational agent levels to try to medically eliminate endo lesions. Reducing estrogen levels is not possible since there are different types of estrogen, different sources of estrogen and endo lesions themselves can influence local production of estrogen.
- Endometriosis cells differ from endometrial cells that are found in the uterus by being relatively resistant to synthetic progestin or natural micronized progesterone therapy.
- Hormonal therapy is known to reduce pain when endometriosis is the cause. However, studies have shown that pain relief is possible but hormonal therapy fails to significantly retard the growth of endometriosis tissue when objectively tested in pathology laboratories. Further, hormonal therapy cannot eliminate scar tissue or fibrosis caused by endo and this fibrosis by itself can be a cause for pain.
- While unproven, under some circumstances it may be prudent to use less toxic hormonal therapy options to potentially reduce the risk of endo recurrence after surgery.
Surgical Treatment
When symptoms, history, physical exam, scans and laboratory evidence all point to endometriosis as a strong possibility to be the root cause of pain, and/or infertility, minimally invasive surgery should be considered to find out for sure. If endo is diagnosed, then medical hormonal therapy may make sense as part of a highly individualized treatment plan under the guidance of an endo specialist.
The caveat to considering endometriosis surgery is that there are, of course, potential risks and complications even though it is minimally invasive. These risks can be minimized in the hands of an expert surgeon, but they should be considered in a risk-benefit discussion.
More importantly, assuming you have identified an expert endo excision surgeon, surgery is the cornerstone to current effective treatment. While incompletely proven, for many reasons, it appears that excision of endo lesions and scar tissue (fibrosis) rather than burning them away (fulguration) is a better and safer approach. To discover more about surgical considerations, consider the following articles.
Integrative Holistic View of Endometriosis
Since the cause of endo is incompletely understood, but highly multifactorial, and because the reason endo is present in any given individual may vary, either surgery or hormonal therapy or both may fail. Failure is relative. In other words, failure may be defined as no immediate pain improvement, persistent subfertility, or it may mean recurrence years later. These are very different scenarios, requiring different approaches. Also, it’s important to consider whether or not associated conditions have been addressed, such as SIBO or other microbiome irregularities, other inflammatory immune-modulated disease and so on. Finally, pelvic floor physical therapy is not just a symptom band-aid but a critical co-treatment for pelvic floor function before and after surgery. These topics are all beyond the scope of this article, but you can discover more by reading the following articles.
If expert excision surgery and supportive hormonal therapy, when used, fails to alleviate pain then supportive pain management can still improve quality of life. This can be mainstream pain and anti-inflammatory medications like non-steroidal anti-inflammatory (NSAID), nerve block injections, electrical stimulation modalities and/or more holistic approaches including acupuncture, acupressure, mind-body biofeedback approaches such as HeartMath, herbals, aromatherapy and more.
Kicking it up a notch, here is something you do not see covered much other than in a very superficial manner. It is not rocket science but is not simplistic at the potential treatment level either. However, it is something you can implement in a proactive way at any point in your journey. Specifically, this is the impact of nutrition and lifestyle choices, as well as well-selected and targeted supplements, but drilled down a lot further than simply eating right, exercising and de-stressing.
Upcoming bio-molecular therapies will target specific biological pathways that we are now beginning to better understand. Many pathways are already identified, many not. The problem is that there are no mainstream medical therapies, yet which can target these pathways safely and effectively. We know from other related genomically modulated inflammatory diseases, like cancer and auto-immune disorders, that these treatments take a while to develop and offer safely. Meanwhile, many of the genomic, metabolic and epigenetic abnormalities that influence endo are known or at least partly known. With few exceptions, while it is too early to safely use pharmaceutical agents to modulate these abnormalities, nutrients, specific exercise, toxin avoidance, and even state of mind can affect the same pathways abnormalities without risk.
Nutrigenomics and Epigenetics
How do toxins or stress adversely affect your health, while healthy diet and exercise positively influence your health? In large part, relatively new sciences like metabolomics and genomics, and their derivatives, explain this. You are born with your genes and, so far, you can’t alter that deck of cards. Some genes may be “bad” and increase your risk of endo, as well as other diseases. However, not everyone with some bad genes develops disease. The most famous examples are identical twins who inherited the exact same genetics yet might look a little different (e.g. eye or hair color) and often get different diseases. Why?
Anything and everything you eat, drink, get exposed to via skin or breathing, or even think about or emote, can affect your genes through epigenetics. This means these substances and neurochemicals, good or bad, can turn genes on and off. Of course, it is infinitely more complex than that and multiple genes affect one process in many cases. However, you can actively modulate your inflammatory and oxidative state. Do we know what veggie or what thought or what toxin turns what specific gene on or off? No. But we do know how these gene-controlled pathways synergize and work together to create health or facilitate disease.
Conclusion
Surgery is a cornerstone to definitive diagnosis of endo and serves as very important part of treatment. The path to success is a correct diagnosis, attention to detail and a highly individualized treatment plan. This can only be carried out in consultation with endometriosis specialists in medical and surgical management.
Unfortunately, it is not easy to find someone or a team that can fit your needs, but it is a crucial step forward to seek out the best you can. The more complex your situation (e.g. possible advanced disease or repeat surgery) the more you need an excision surgeon with master surgeon skills. Ideally you want a specialist who is not only a surgeon but also capable of guiding you through any additional treatment options you may need, mainstream and holistic. While a master excision surgeon and integrative endo specialist is hard to come by, many have a team that can fulfill your needs.
References:
Endometriosis: Etiology, pathobiology, and therapeutic prospects
Brassica Bioactives Could Ameliorate the Chronic Inflammatory Condition of Endometriosis
Diet and risk of endometriosis in a population-based case–control study
Emerging Drug Targets for Endometriosis
Updated Post: July 09, 2024

Can Endometriosis Cause Bowel Issues?
Endometriosis is a common but often under-recognized condition, primarily affecting women between 15-50. It results from the growth of tissue similar to the endometrium (the lining of the uterus) outside the uterus. This article explores the question: Can endometriosis cause bowel issues?
Table of contents
- Understanding Endometriosis
- Endometriosis and Bowel Involvement
- Causes of Endometriosis
- Symptoms of Bowel Endometriosis
- Diagnosing Bowel Endometriosis
- Misdiagnosis of Bowel Endometriosis
- Treatment for Bowel Endometriosis
- Coping with Bowel Endometriosis
- The Importance of Early Detection
- Conclusion
- Additional Information
Understanding Endometriosis
Endometriosis is a condition where tissue, similar to the kind that lines the uterus (the endometrium), grows outside the uterus. This condition usually affects the ovaries, fallopian tubes, and the tissue lining the pelvis. However, in some cases, it can also affect other organs, including the bowel.
Endometriosis and Bowel Involvement
When endometriosis affects the bowels, it typically occurs in two forms:
- Superficial: The endometriosis tissue is located on the surface of the bowel.
- Deep: The endometriosis tissue passes through the bowel wall.
In both cases, doctors usually find a small mass of tissue, known as a lesion, on the bowel wall. More rarely, these lesions can penetrate into the muscular layer of the bowel.
Read More: Endometriosis and Inflammatory Bowel Disease: Distinguishing the Differences
Causes of Endometriosis
While the definitive cause of endometriosis remains unknown, several contributing factors have been identified. These include hormonal imbalances, immune system problems, and genetic factors.
Symptoms of Bowel Endometriosis
The symptoms of bowel endometriosis can vary, depending on the location and size of the lesion, and how deep it is within the bowel wall. These symptoms often mimic those of irritable bowel syndrome (IBS), but there are key differences.
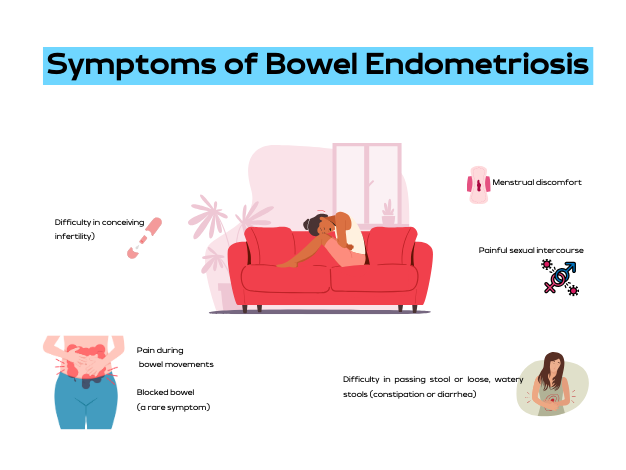
Some of the common symptoms include:
- Trouble pooping or loose, watery stools (constipation or diarrhea)
- Pain during bowel movements
- Menstrual discomfort
- Painful sex
- Difficulty getting pregnant (infertility)
- Blocked bowel (this is a rare symptom)
Diagnosing Bowel Endometriosis
Diagnosing bowel endometriosis can be challenging due to its similarities with other conditions. However, if you have other endometriosis symptoms, such as painful periods, painful sex, lower back pain, or abdominal bloating and discomfort, it’s critical to talk to your doctor.
Read More: Understanding Bowel Endometriosis
Misdiagnosis of Bowel Endometriosis
Unfortunately, bowel endometriosis is often misdiagnosed as irritable bowel syndrome or other gastrointestinal diseases. This is because the symptoms of bowel endometriosis can mirror those of IBS, Crohn’s disease, and appendicitis.
Read More: Finding an Excision Specialist: What you Need to Know
Treatment for Bowel Endometriosis
Treatment for bowel endometriosis is usually tailored to the patient’s symptoms and medical history. The most common treatments include surgery, hormone treatments, and counseling.
Coping with Bowel Endometriosis
Bowel endometriosis is a challenging condition to live with. It not only affects your physical health but also your mental well-being. Many patients have found some symptom relief through lifestyle changes, including dietary adjustments and regular exercise.
The Importance of Early Detection
Given the potential complications of bowel endometriosis, early detection and treatment are crucial. If you experience bowel issues alongside painful menstruation, it’s essential to consult with a healthcare professional.
Conclusion
The question, “Can endometriosis cause bowel issues?” is undoubtedly answered with a resounding yes. However, with timely detection, appropriate treatment, and necessary lifestyle changes, it’s possible to manage the symptoms and lead a healthy life.
Additional Information
This article is a comprehensive exploration of how endometriosis can impact bowel health. It’s essential to remember that while this condition can cause significant discomfort and health issues, effective treatments are available. If you suspect you have endometriosis, don’t hesitate to reach out to a healthcare provider.
References:
https://www.webmd.com/women/endometriosis/bowel-endometriosis
https://www.endofound.org/gastrointestinal-distress
https://maidenlanemedical.com/endometriosis/endometriosis-and-constipation/
https://drseckin.com/bowel-endometriosis/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4604671/
Understanding How Endometriosis Can Cause Bowel Problems
Endometriosis, a common health concern among women, can manifest itself in various ways, one of them being bowel problems. But how exactly can endometriosis cause bowel problems? This article will take you through the intricate connection between endometriosis and bowel problems, the symptoms to look out for, diagnostic procedures, and potential treatments.
Table of contents
What is Endometriosis?
Endometriosis is a health condition where the tissue similar to the type that lines the uterus, known as the endometrium, grows outside the uterus. This condition predominantly affects the reproductive organs such as the ovaries, fallopian tubes, and the external part of the uterus. However, it can also extend to other parts of the body including the bowels, rectum, and other pelvic organs.
Understanding Bowel Endometriosis
Bowel endometriosis is a form of endometriosis that affects the gastrointestinal tract, specifically the bowels. It can appear in two forms: superficial (on the surface of the bowel) and deep (penetrating the bowel wall).
Read More: Understanding Bowel Endometriosis
Symptoms of Bowel Endometriosis
The symptoms of bowel endometriosis can vary widely depending on the location of the lesion, its size, and how deep it is in the bowel wall. Some women may experience no symptoms. However, common symptoms include:
- Difficulty in passing stool or loose, watery stools (constipation or diarrhea)
- Pain during bowel movements
- Menstrual discomfort
- Painful sexual intercourse
- Difficulty in conceiving (infertility)
- Blocked bowel (a rare symptom)
It is noteworthy that these symptoms can often mimic other conditions like irritable bowel syndrome (IBS), but the two conditions are distinct. One distinguishing factor is that with bowel endometriosis, symptoms often worsen before and during the menstrual period.
Read More: Endometriosis and Painful Intercourse: Is it Really Just Endometriosis?
Causes of Bowel Endometriosis
The exact cause of bowel endometriosis is still under study. However, several factors have been linked to its occurrence. These include genetic predisposition, inflammation, and levels of estrogen, a female sex hormone.
The Prevalence of Endometriosis
Endometriosis affects approximately 10%-12% of women of childbearing age. The condition is often diagnosed in women who are in their 30s, although it can occur at any age.
Diagnosing Bowel Endometriosis
The diagnosis of bowel endometriosis starts with the doctor asking about your symptoms and medical history, followed by a physical examination of your pelvic area. The doctor may also recommend imaging tests to get more information on the location and size of any cysts or tissue damage related to endometriosis. These tests include:
- Transvaginal or transrectal ultrasound: This procedure involves the insertion of a wand-like device into your vagina or rectum. This device releases sound waves that create images of your organs.
- Magnetic resonance imaging (MRI): An MRI test provides detailed images of your organs and tissues using a magnetic field and radio waves.
- Laparoscopy: This surgical procedure involves making a small incision near your belly button and inserting a thin viewing tool called a laparoscope.
- Barium enema: This type of X-ray is used to see changes or defects in your large intestine (colon).
- Colonoscopy: They pass a tube with a camera on its tip through the anus into the colon to directly visualize the wall and take samples from inside the colon.
Read More: Colon Chronicles: Delving into Bowel Endometriosis
Treating Bowel Endometriosis
The treatment plan for bowel endometriosis will be personalized, taking into account your symptoms, medical history, age, and reproductive plans. Treatments can include:
- Surgery: The aim of surgery is to remove as many lesions as possible while preserving your organs and overall health.
- Hormone treatments: These medications control estrogen levels which can worsen the symptoms of bowel endometriosis.
- Counseling: Given the ongoing nature of bowel endometriosis and its impact on both physical and mental health, counseling may be recommended to provide emotional support.
The Prognosis for Bowel Endometriosis
There is currently no cure for endometriosis. However, treatments like surgery and hormone therapy can help manage the symptoms. It is also important to note that symptoms could return if treatment is halted, or they could recur on their own, especially in cases with deep lesions.
Endometriosis is a complex condition that can cause bowel problems and other health issues. If you suspect you have endometriosis and are experiencing bowel problems, it’s important to consult with a healthcare provider. Early diagnosis and treatment can help manage symptoms and improve your quality of life.
References:
https://www.webmd.com/women/endometriosis/bowel-endometriosis
https://www.endometriosis-uk.org/endometriosis-and-bowel
https://www.endofound.org/gastrointestinal-distress
ENDOMETRIOSIS AND CONSTIPATION

Colon Chronicles: Delving into Bowel Endometriosis
In our recent blog, we highlighted the significance of addressing bowel endometriosis, a condition prone to misdiagnosis. Whether individuals have struggled with lifelong bowel issues or are suddenly facing disruptions, determining what’s considered normal can be perplexing. The “normal” range spans anywhere from three times a day to as infrequent as three times per week. In many sources, the focus is typically limited to frequency and to some degree consistency; however, there’s an overall scarcity of information on what defines normalcy.
Table of contents
ICYMI: Understanding Bowel Endometriosis
This ambiguity is particularly challenging for those with endometriosis, where gastrointestinal symptoms vary widely, making it tough to discern what’s amiss. About 90% of endometriosis cases involve some form of gastrointestinal symptoms, often leading to an IBS (irritable bowel syndrome) diagnosis, which essentially offers a label for persistent symptoms without an identifiable cause. The usual next step in diagnostics is often a colonoscopy, a key tool for identifying or ruling out certain diseases. This article explores the nuances of bowel endometriosis, with a primary focus on the role and precision of colonoscopy in diagnosing this condition.
Bowel endometriosis is considered to be deep infiltrating endometriosis and can lead to a variety of symptoms which we discussed in the previous blog, but is often concerning if not diagnosed timely and may risk more complex surgeries including resection if the disease is not properly addressed.
Related Reading: How to Get an Endometriosis Diagnosis
The Role of Colonoscopy – Is it helpful?
A colonoscopy is a diagnostic procedure commonly used to examine the inner lining of the large intestine (colon and rectum). It involves the use of a long, flexible tube called a colonoscope, which has a small camera attached to its end. This tool allows physicians to visualize the interior of the colon to identify any abnormal conditions or changes.
In the context of bowel endometriosis, a colonoscopy can potentially detect signs of endometrial tissue growth within the bowel. However, its effectiveness and accuracy in diagnosing this condition have been subjects of ongoing research and debate. Aside from its ability to detect endometriosis, there is also consideration of the provider performing the procedure and their level of knowledge of endometriosis.
The use of colonoscopy in diagnosing bowel endometriosis has been a topic of considerable discussion among medical professionals. Given the invasive nature of the procedure and the often non-specific symptoms of bowel endometriosis, the role and necessity of colonoscopy in its diagnostic process have been questioned.
However, several case studies and research findings suggest that colonoscopy can indeed play a crucial role in identifying bowel endometriosis. In particular, it has been found to be effective in detecting endometriosis growth in the bowel, with certain colonoscopic findings such as eccentric wall thickening, polypoid lesions, and surface nodularities often being associated with endometriosis.
Evaluating the Accuracy of Colonoscopy for Diagnosing Bowel Endometriosis
While the potential of colonoscopy in detecting bowel endometriosis has been recognized, its accuracy in doing so has been the subject of extensive research. A number of studies have sought to evaluate the sensitivity, specificity, and predictive values of colonoscopy in diagnosing this condition.
One such study was conducted by Milone M et al., who performed a prospective observational study that included women diagnosed with deep pelvic endometriosis. The study aimed to evaluate the accuracy of colonoscopy in predicting intestinal involvement in deep pelvic endometriosis.
The results of the study suggested that colonoscopy did have the potential to detect bowel endometriosis, with a number of cases accurately diagnosed through the procedure. However, the overall sensitivity, specificity, and predictive values of colonoscopy were found to be variable, indicating room for improvement in its diagnostic accuracy.
In another study conducted by Marco Milone and his team, the researchers also found that while colonoscopy could indeed identify bowel endometriosis, its accuracy was not optimal. The study elucidated that the presence of colonoscopic findings of intestinal endometriosis in deep pelvic endometriosis was quite low, indicating that routine colonoscopy may not be justified for all women with deep pelvic endometriosis.
A Case Study: Bowel Endometriosis and Colonoscopy
To illustrate the potential role of colonoscopy in diagnosing bowel endometriosis, let’s consider a case study involving a 45-year-old woman who presented with abdominal pain in her left lower quadrant. This woman underwent a colonoscopy, which revealed a submucosal tumor-like lesion in her sigmoid colon.
Upon further examination using magnifying endoscopy, the lesion was found to contain sparsely distributed round pits – a finding that was suggestive of endometrial glands and stroma (the histological definition of endometriosis). This discovery led to a biopsy of the lesion, the results of which confirmed the presence of intestinal endometriosis.
This case study serves to highlight how colonoscopy, when combined with other diagnostic methods like magnifying endoscopy and biopsy, can aid in the detection and diagnosis of bowel endometriosis.
The Future of Bowel Endometriosis Diagnosis
While the role and accuracy of colonoscopy in diagnosing bowel endometriosis have been explored, research in this area is ongoing. The development and refinement of diagnostic methods are crucial for improving the detection and treatment of bowel endometriosis.
In parallel with the innovations in medical technology, new diagnostic methods such as magnifying chromoendoscopy, target biopsy, and virtual colonoscopy are being explored and studied for their potential to improve the accuracy of bowel endometriosis diagnosis. These advancements, coupled with a deeper understanding of the condition, may pave the way for more accurate and less invasive diagnostic options in the future.
Bowel endometriosis is a complex condition that can significantly impact the quality of life of those affected. While colonoscopy can play a role in its diagnosis, its effectiveness and accuracy are subject to continuous research and improvement. Exploring new diagnostic methods and refining existing ones are crucial steps toward enhancing the detection and treatment of this condition. As we continue to learn more about bowel endometriosis and its nuances, we can hope for more efficient and accurate diagnostic tools in the future.
Related Reading:
- Endo-Fighting Microbiome Optimization: Research-based Tips
- Endometriosis and the Microbiome: Insights and Emerging Research
References:
- Walter SA, Kjellström L, Nyhlin H, Talley NJ, Agréus L. Assessment of normal bowel habits in the general adult population: the Popcol study. Scand J Gastroenterol. 2010;45(5):556-566. doi:10.3109/00365520903551332
- Habib, N., Centini, G., Lazzeri, L., Amoruso, N., El Khoury, L., Zupi, E., & Afors, K. (2020). Bowel Endometriosis: Current Perspectives on Diagnosis and Treatment. Int J Womens Health, 12, 35-47. https://doi.org/10.2147/IJWH.S190326
- Milone, M., Mollo, A., Musella, M., Maietta, P., Sosa Fernandez, L. M., Shatalova, O., Conforti, A., Barone, G., De Placido, G., & Milone, F. (2015). Role of colonoscopy in the diagnostic work-up of bowel endometriosis. World J Gastroenterol, 21(16), 4997-5001. https://doi.org/10.3748/wjg.v21.i16.4997
- Tomiguchi, J., Miyamoto, H., Ozono, K., Gushima, R., Shono, T., Naoe, H., Tanaka, M., Baba, H., Katabuchi, H., & Sasaki, Y. (2017). Preoperative Diagnosis of Intestinal Endometriosis by Magnifying Colonoscopy and Target Biopsy. Case Rep Gastroenterol, 11(2), 494-499. https://doi.org/10.1159/000475751

Understanding Bowel Endometriosis
Bowel Endometriosis is a debilitating chronic health condition that affects a significant number of women worldwide. This disease is characterized by the growth of endometrial-like tissue outside the uterus, specifically on or inside the bowel walls. The condition often presents with varying gastrointestinal symptoms like painful bowel movements, constipation, and diarrhea, making it difficult to diagnose.
Table of contents
What is Bowel Endometriosis?
Bowel Endometriosis is a specific form of endometriosis that involves the intestines. In this condition, cells similar to those that line the uterus start growing on the bowel or even penetrate into the bowel wall. This growth can lead to painful and uncomfortable symptoms, particularly during a woman’s menstrual cycle.
Prevalence and Affected Areas
Bowel Endometriosis is a subset of a larger condition, endometriosis, affecting 1 in 5 endo patients. The most common sites for bowel involvement are the rectum, appendix, sigmoid, cecum, and distal ileum. It’s also worth noting that bowel endometriosis frequently co-exists with endometriosis in other areas, making it a multifaceted disease that requires comprehensive treatment.
Symptoms of Bowel Endometriosis
Understanding the symptoms of bowel endometriosis can help in early diagnosis and treatment. It’s essential to note that these symptoms often overlap with other gastrointestinal conditions, making it a challenging disorder to diagnose.
Common Symptoms of Endometriosis
- Painful bowel movements: This is one of the most common symptoms of bowel endometriosis. The pain is often described as sharp or cramping and may worsen during menstruation.
- Constipation and Diarrhea: Changes in bowel habits are another common symptom. Some women may experience constipation, while others may have diarrhea. These symptoms may also worsen during menstruation.
- Rectal Bleeding: While not as common, some women may experience rectal bleeding, particularly during their menstrual period. A healthcare professional should always evaluate this symptom as it can also be a sign of other serious conditions.
- Abdominal Pain: Abdominal pain, often worsening during the menstrual cycle, is another common symptom. The pain can range from mild to severe and may be constant or intermittent.
- Dyspareunia: Dyspareunia, or painful sex, is another symptom that may indicate the presence of bowel endometriosis. This pain often stems from endometriosis lesions in the posterior pelvic compartment peritoneum, an area around the rectum that includes the surface peritoneum, commonly called the pouch of Douglas.
Diagnosing Bowel Endometriosis
Diagnosing bowel endometriosis can be challenging due to the overlap of symptoms with other gastrointestinal disorders. However, several diagnostic tools can aid in the identification of this condition.
Physical Examination and Patient History
A detailed patient history and a thorough physical examination are crucial first steps in diagnosing bowel endometriosis. The doctor will ask about the symptoms, their severity, and if they worsen during menstruation. A pelvic exam may also be performed to check for any abnormalities.
Imaging Tests
Imaging tests, such as transvaginal sonography (TVS) and magnetic resonance imaging (MRI), are commonly used to identify and characterize endometriosis lesions.
TVS is a first-line imaging technique providing detailed dynamic images of the pelvis with minimal patient discomfort. It helps identify all of the bowel’s layers and any potential endometriosis nodules.
MRI, on the other hand, is typically used as a second-line diagnostic tool. It excels in evaluating the extent of the disease and identifying any specific organ involvement and depth of infiltration.
Endoscopy and Biopsy
An endoscopy may also be performed to examine the bowel for any abnormalities. A biopsy can be taken during this procedure to check for the presence of endometriosis cells. However, this method has its limitations as it only provides a superficial sample, and endometriosis usually involves deeper layers of the bowel wall.
Laparoscopy
Laparoscopy is the gold standard for diagnosing endometriosis. This surgical procedure allows for visual inspection of the peritoneal cavity and can provide a definitive diagnosis. The surgeon can also assess the extent of the disease and its impact on other organs.
Misdiagnosis of Bowel Endometriosis
Bowel endometriosis is often misdiagnosed due to its similar symptoms to other gastrointestinal disorders. This condition is frequently mistaken for irritable bowel syndrome (IBS), Crohn’s disease, and even colon cancer.
It’s crucial for healthcare providers to consider a possible diagnosis of bowel endometriosis in women presenting with gastrointestinal symptoms, especially if these symptoms worsen around the menstrual cycle.
Treatment of Bowel Endometriosis
Treating bowel endometriosis is typically multidisciplinary, involving a team of specialists. It generally involves a combination of medical and surgical therapies.
Medical Therapy
Medical treatments aim to control the symptoms of bowel endometriosis and may include pain relievers, hormonal therapies like oral contraceptives or progestins, and gonadotropin-releasing hormone analogs. These treatments work by reducing inflammation and suppressing the growth of endometrial tissue.
Surgical Therapy
In more severe cases, or when medical therapy is ineffective, surgery may be necessary. The type of surgery will depend on the extent and location of the endometriosis. In some cases, a conservative approach may be used, where the surgeon attempts to remove the endometriosis while preserving as much of the bowel as possible. In other cases, a segment of the bowel may need to be removed.
Laparoscopic Surgery
Laparoscopic surgery is often the preferred method for treating bowel endometriosis. This minimally invasive procedure allows for precise removal of the endometriosis with less damage to surrounding tissue and quicker recovery times. However, it requires a skilled surgeon and may only be an option in some cases.
Read More: Why It’s Important Your OB-GYN Specializes in Endometriosis?
Bowel Endometriosis and Fertility
Research indicates that bowel endometriosis may have an impact on a woman’s fertility. This could be due to the inflammation and scarring caused by the disease, which can interfere with the normal function of the reproductive organs.
In cases where infertility is an issue, assisted reproductive technologies may be considered. However, surgery to remove the endometriosis is often recommended first to increase the chances of a successful pregnancy.
Read More: Does Endometriosis Cause Infertility?
Conclusion
Bowel endometriosis is a complex condition that can significantly impact a woman’s quality of life and fertility. Early diagnosis and effective treatment are crucial to managing this condition and minimizing its effects. Suppose you’re experiencing symptoms of bowel endometriosis. In that case, it’s important to consult with a healthcare provider who is knowledgeable about this condition and can guide you through the diagnosis and treatment process.
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6996110/

