
Managing Endometriosis: What You Need to Know
Table of contents
Endometriosis is a common condition that occurs when tissue similar to the interior layer of the uterus grows outside the uterus. These pathologic tissues respond to hormones, nutrition, lifestyle, and stress level. Endometriosis can cause pain, fatigue, other symptoms, and infertility. Fortunately, there are several ways to manage endometriosis and reduce its effects on your life. Let’s look at what you need to know about managing endometriosis.
Can endometriosis be cured completely?
Hormonal Therapy for Endometriosis Management
Hormonal therapy is one of the most common treatments for endometriosis management. Hormones like progestins and birth control pills work by suppressing ovulation and reducing estrogen levels in the body, which helps reduce the growth of endometriosis tissue. While this treatment may not be suitable for everyone, it can effectively reduce pain and other symptoms associated with endometriosis. But it is not a cure or a permanent solution. You might feel better if you take hormonal therapy, and endometriosis symptoms most likely come back whenever you stop the medication.
Surgery for Endometriosis Management
Surgery may sometimes be the best choice to treat endometriosis and alleviate its symptoms. Endometriosis surgeons use laparoscopes or robots to remove most endometriosis and adhesions or cysts. After surgery, your doctor may also prescribe hormonal therapy to help keep the condition under control. Your endometriosis surgeon might also recommend physical therapy before or after surgery to help manage symptoms and regain your functions.
Physical Therapy for the Management of Endometriosis
Physical therapists can have a significant impact on your life with endometriosis. They can help you know your body better and understand your limitations. A physical therapist or occupational therapist might be a great resource if you have any pelvic area spasms or movement limitations because of endometriosis pain.
Physical Therapy Before Excision Surgery for Endometriosis
Physical Therapy after excision surgery
Questions to Ask Your Physical Therapist When you have endometriosis
Dietary Changes for Endometriosis Management
Making dietary changes can also help manage endometriosis symptoms and reduce inflammation in your body. Eating fruits and vegetables—especially those rich in antioxidants—can help reduce inflammation and improve overall health. Avoiding processed foods and refined sugars can also help lessen symptoms associated with this condition. You need a dietitian to help you with this dietary planning.
Lifestyle Changes for Endometriosis Management
More body fat can mean higher estrogen and higher inflammation levels. Therefore, some healthy changes in your lifestyle to optimize the fat storage in your body can positively impact endometriosis management and symptoms. These changes can mean more physical activity or less junk food, or else. You are the best person to decide what lifestyle you should pursue. Moreover, a healthy lifestyle can improve your mental health and quality of life.
People with endometriosis should talk to their doctor about treatment options that are right for them to manage their condition effectively. In many cases, combining hormonal therapy, surgery, lifestyle, physical therapy, and dietary changes can help reduce pain and other symptoms associated with this condition. The goal should be for you to live a fuller life free from endometriosis effects. With proper management strategies, people with endometriosis can live healthier lives despite their diagnosis!
Find the best endometriosis specialists around the world!

Endometriosis Excision Surgery: What You Need to Know About
Endometriosis is a gynecological condition that affects approximately 10% of women between 15-55. It can cause chronic pain, infertility, and other issues. It happens when a similar tissue to tissue that lines the uterus grows outside of the uterus. One way to manage endometriosis is through endometriosis excision surgery. Let’s take a deeper look into what this surgery involves.
Table of contents
The Procedure
Endometriosis excision surgery is a procedure in which a gynecologist uses specialized tools and techniques to remove endometriosis tissue from the pelvis, abdomen, and other regions. Excision means removing the tissue from organs near the uterus, such as the ovaries, fallopian tubes, bladder, rectum, or intestines. The doctor will remove any adhesions (scar tissue) causing pelvic pain or threatening fertility. The surgery requires an outpatient surgery center or a hospital operating room.
Benefits of Endometriosis Excision Surgery
Endometriosis excision surgery aims to reduce or eliminate the pain caused by endometriosis growths, improve fertility outcomes for those who want children, and prevent new growths from developing. In some cases, patients can experience improved symptoms after just one procedure; however, some patients may need multiple surgeries. This need for repeat surgeries depends on the surgeon’s experience, disease behavior and severity, and some unknown factors.
Precautions to Take Before Surgery
Before undergoing endometriosis excision surgery, you should speak with your doctor about any concerns about anesthesia or other risks associated with the procedure. Additionally, depending on the severity of your condition and your treatment goals (fertility vs. symptom relief), other treatments may need to be considered before considering surgical intervention.
Talk with your doctor first to ensure that endometriosis excision surgery is right for your needs. If you have questions about this procedure or any other treatments available for managing endometriosis symptoms, don’t hesitate to reach out to your healthcare provider today! They will help you determine if endo excision surgery is a good option.
Have you considered endometriosis excision surgery? What is your most burning question about endometriosis excision surgery?

Understanding Endometriosis Through Blood Tests
Endometriosis is a condition in which tissue similar to endometrial cells grows outside the uterus and can cause severe pain, discomfort, and infertility. While many women with endometriosis experience physical symptoms such as abdominal pain or cramping, it can be challenging to diagnose without a medical professional. A blood test is one-way doctors can help narrow down the diagnosis. Let’s explore how this works.
What Can Blood Tests Show?
Blood tests help measure levels of hormones in the body that could indicate endometriosis. The two most common hormones related to the condition are estradiol (an estrogen hormone) and progesterone (a progestin hormone). High estradiol levels can indicate an imbalance in female hormones, which may be associated with endometriosis. Low progesterone levels suggest an underlying issue with the reproductive system.
In addition, some blood tests specifically measure for markers like CA-125, a protein in high concentrations in some women with endometriosis. By measuring these markers alongside other hormonal levels, doctors can build a better picture of your overall health and determine whether or not you may have endometriosis.
It’s important to note that blood tests alone aren’t enough to make a definitive diagnosis. Your doctor will likely need to perform additional tests, such as an ultrasound, MRI, or laparoscopy before they can confirm if you have endometriosis.
While blood tests cannot definitively diagnose endometriosis, they can provide valuable information about your overall health that could help guide diagnosis and treatment decisions. If you think you may be suffering from this condition, you must speak with your doctor so they can determine the best approach for testing and treatment options based on your individual needs. Taking proactive care now will help ensure better long-term outcomes for managing your condition effectively and efficiently!

A Guide to Endometriosis Surgery and Its Success Rate
Endometriosis is a condition in which tissue similar to the uterine lining grows outside the uterus. Endometriosis can cause pain, heavy bleeding, and infertility. Women seeking relief from endometriosis symptoms and want to maintain their fertility consider surgery an option. This guide will discuss the types of endometriosis surgery available and their success rates.
Table of contents
Types of Endometriosis Surgery
Two types of endometriosis surgery are available: minimally invasive (laparoscopy and robotics) and open abdominal surgery. In a minimally invasive procedure, a thin tube with a camera and tiny surgical instruments are inserted into the abdomen through small incisions in the belly area. During the minimally invasive procedure, surgeons can remove or destroy endometriosis tissue with lasers or other tools. Open abdominal surgery involves making a wide incision in the abdomen to access any affected areas directly and remove them surgically. Most top surgeons with significant experience prefer minimally invasive surgeries with laparoscopy or robotics.
Success Rates
The success rate of endometriosis surgeries depends on factors such as the severity of symptoms, type of procedure performed, and experience of the surgeon performing the procedure, etc. Patients can achieve complete or partial relief in complaints in up to 93.2% of cases with surgery. And 65% of those wishing for pregnancy but were unsuccessful in the past, could conceive after surgery. Some experts believe success rate increases when additional treatments such as hormone therapy or medications are used following surgery to reduce recurrence risk. But hormonal therapy after surgery is not an option if you plan to conceive right after recovery. Minimally invasive surgery is superior to open surgeries because it results in lower risk of surgical complications, such as bleeding, infection and damage to other abdominal organs. Minimally invasive procedure also offers faster recovery compared to open surgery.
Endometriosis can cause significant physical discomfort and emotional distress for individuals living with it. However, fortunately, some treatments can relieve painful symptoms while still allowing to maintain fertility if desired. Surgery is one such treatment option and provides varying levels of success depending on factors such as experience level, the severity of the disease, and the type of procedure used. Studies have found that up to 93% of patients report partial or complete decreased pain after undergoing endometriosis surgery. And 65% of patients achieved pregnancy after surgery. Talk with your doctor if you think you are suffering from this condition. Discuss testing options and treatment plans, including surgical interventions, so that you can take control of your health today!
Featured specialists:

Can Endometriosis Be Cured Completely?
Endometriosis is a common condition that affects 1 in 10 women between 15 and 55 years old. It occurs when tissue similar to the lining of the uterus grows outside the uterus. Endometriosis can cause painful periods and sex, abdominal pain, and fertility issues. But what exactly is endometriosis, and can it be cured? Let’s take a closer look.
Table of contents
What Causes Endometriosis?
The exact cause of endometriosis is unknown, but several theories exist about how it develops. One theory suggests that during menstruation, some of the uterine linings flow back through the fallopian tubes and into the abdomen, where it implants and begins to grow. Another theory suggests that stem cells present in the body can transform into endometriosis tissue.
Can Endometriosis Be Cured Completely?
Unfortunately, no—endometriosis cannot be cured entirely at this time. However, there are treatments available to alleviate symptoms. These treatments include hormonal medications or surgery, depending on your condition’s severity and preferences. Hormonal medications such as birth control pills or hormone-releasing IUDs may help reduce pain and stop endometriosis growth from progressing further by stopping ovulation and changing hormone levels in your body. Surgery may also be a choice, especially if you have severe symptoms that are not responding to routine treatments. Surgery is also more desirable with deeply infiltrated lesions or cysts on your organs, such as your ovaries or intestines.
Endometriosis affects millions of women worldwide. Although not curable, you can manage this disease with proper surgery, medical care, and lifestyle plans. Lifestyle steps such as maintaining a healthy diet, exercising regularly, reducing stress levels, and avoiding certain foods known to worsen your symptoms can be helpful. Although there is currently no cure for endometriosis, many treatment options exist that can help minimize symptoms. These treatment options can help you lead a near-normal life and improve pain or fertility issues. If you suspect you have endometriosis, talk to your doctor about available treatments for managing your condition today!

Laparoscopy: A Common Treatment for Endometriosis
Endometriosis is a common condition that mainly affects women of reproductive age. It occurs when tissue similar to the uterine lining grows outside the uterus, typically on other organs in the pelvic area. One of the most common treatments for endometriosis is laparoscopy, a minimally invasive surgical procedure used to diagnose and treat the disorder. Let’s take a closer look at what this procedure entails.
Table of contents
How Laparoscopy Works
During a laparoscopy, your doctor will insert a thin, lighted tube called a laparoscope through small incisions in your belly. The laparoscope allows your doctor to see inside your abdomen and pelvis and identify areas of endometriosis tissue growth. In some cases, they may also use laparoscopic tools to remove any abnormal tissue growth they find during this process.
This procedure can be performed in several ways. Your doctor may perform it under general anesthesia, where you are completely asleep during the operation. Depending on what your doctor finds during the laparoscopy, they may perform additional procedures, such as removing cysts or scarring caused by endometriosis.
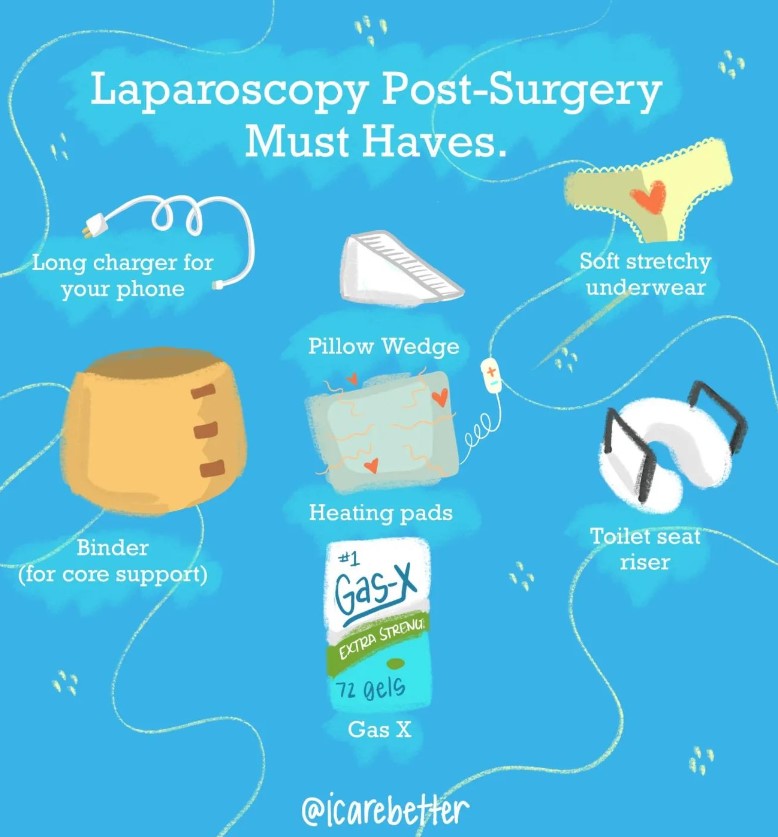
Recovery from Laparoscopy
The recovery time after a laparoscopic surgery depends on several factors, including how extensive the procedure was and how long it took to complete. Most people return home within 24 hours after having this done and can expect to recover fully within two to six weeks with minimal pain or discomfort afterward. You should follow all your doctor’s post-operative instructions, including taking medications as prescribed and avoiding strenuous activities like heavy lifting until your healthcare provider clears you to resume normal activities.
Laparoscopies can be an effective way to diagnose and treat endometriosis in women of reproductive age. This minimally invasive surgical procedure involves inserting thin, lighted tubes into incisions on your belly to identify areas of endometrial tissue growth that could be causing pain and other symptoms. While recovery time varies depending on the procedure’s extent, most people can return home within 24 hours and resume their normal activities within two weeks or so with minimal pain or discomfort afterward. If you think you may have endometriosis, talk to your healthcare provider about whether laparoscopy works for you!

The Different Tests Used to Diagnose Endometriosis
Table of contents
Endometriosis is a chronic condition characterized by the growth of endometrial-like tissue, which is found throughout the body, primarily in the abdominopelvic cavity, and affects an estimated 176 million women globally. While its exact causes remain elusive, this disorder can inflict debilitating pelvic pain, dysmenorrhea, dyspareunia, and even infertility on those afflicted. However, the path to an accurate diagnosis can be arduous, often spanning years due to the condition’s elusive nature and the lack of a definitive, non-invasive test. In this comprehensive guide, we’ll unravel the complexities of diagnosing endometriosis, exploring the various tests and imaging techniques employed by healthcare professionals to identify this enigmatic condition.
Understanding the Diagnostic Challenges
Endometriosis presents a diagnostic conundrum, as its symptoms can mimic those of other conditions, such as irritable bowel syndrome, interstitial cystitis, or fibromyalgia. Moreover, the severity of symptoms often bears little correlation with the extent of the disease, further compounding the diagnostic challenge. Some women with minimal endometriosis may experience excruciating pain, while others with advanced stages may remain asymptomatic. This unpredictable nature underscores the importance of a multi-faceted diagnostic approach, combining clinical evaluation, imaging techniques, and, in some cases, surgical intervention.
The Importance of Early Diagnosis
Prompt diagnosis is crucial for effective management of endometriosis, as the condition can progress over time, potentially exacerbating symptoms and increasing the risk of infertility. Early intervention can help mitigate long-term impacts, improve quality of life, and enhance fertility outcomes. However, the diagnostic journey can be prolonged, with an average delay of 7 to 10 years from the onset of symptoms, owing to factors such as lack of awareness, normalization of menstrual pain, and the absence of a definitive non-invasive test.
The Role of Clinical Evaluation
The diagnostic process typically commences with a comprehensive clinical evaluation, encompassing a detailed medical history and physical examination. Healthcare providers will inquire about the nature, timing, and severity of symptoms, such as pelvic pain, dysmenorrhea, dyspareunia, and abnormal bleeding patterns. A pelvic exam may reveal signs of endometriosis, such as pelvic masses, nodules, or scarring, although the absence of these findings does not necessarily rule out the condition. They may also order blood work to check hormone levels and screen for other conditions with similar symptoms.
Imaging Techniques for Endometriosis Diagnosis
While there have been significant improvements in imaging modalities in recent years, most imaging techniques implemented currently cannot definitively diagnose endometriosis. However, they do currently play a crucial role in identifying specific manifestations of the disease and guiding treatment strategies.
Transvaginal Ultrasound
Transvaginal ultrasound (TVUS) is a widely accessible and non-invasive imaging technique that can detect ovarian endometriomas (chocolate cysts) and deep infiltrating endometriotic (DIE) nodules or adhesions. Most people will receive a basic ultrasound, While a basic ultrasound may be able to detect endometriomas and DIE, it lacks efficacy in identifying superficial peritoneal implants. Research focusing on the use of advanced ultrasound shows promise in better detection and earlier diagnosis of endometriosis. Until more providers are trained and routinely use advanced ultrasound, the accuracy of TVUS in diagnosing endometriosis remains limited and highly dependent on the operator’s expertise and experience.
Magnetic Resonance Imaging (MRI)
MRI is particularly valuable in assessing the extent and location of deep infiltrating endometriosis, as well as identifying endometriotic lesions in atypical locations, such as the bladder, ureters, or rectosigmoid region. While more expensive and less readily available than ultrasound, MRI can provide detailed information to aid surgical planning and ensure the involvement of appropriate specialists, if necessary. Similar to TVUS, the ability of the MRI to identify endometriosis also relies on the experience and expertise of the technician taking the images, and the radiologist reading them.
The Gold Standard: Laparoscopic Surgery
Despite advancements in imaging techniques, laparoscopic surgery remains the gold standard for definitive diagnosis of endometriosis. During this minimally invasive procedure, a surgeon inserts a laparoscope (a thin, lighted instrument) through a small incision in the abdomen, allowing direct visualization of the pelvic organs and potential endometriotic lesions. Tissue samples can be obtained for histological confirmation, providing a definitive diagnosis. Laparoscopies are performed under general anesthesia, so you will not feel anything during the procedure. Laparoscopy not only serves a diagnostic purpose but also offers the opportunity for simultaneous surgical treatment, with excision being the preferred method to remove endometriosis lesions.
Endometriosis can be hard to diagnose because its symptoms are often very similar to other conditions, such as period discomfort, ovarian cysts, or pelvic inflammatory disease. If you think you have endometriosis, you must talk to your doctor as soon as possible so they can determine what type of testing is right for you and how best to treat it. Working with the right healthcare provider ensures you receive the best care possible for managing your condition and improving your overall quality of life.
Comprehensive Management: Beyond Diagnosis
Endometriosis management often requires a multidisciplinary approach, combining medical and surgical interventions tailored to individual circumstances. While surgery is currently the only treatment to address the lesions, several options are recommended for addressing other pain generators and for symptom management, including:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) and hormonal contraceptives for pain management
- Gonadotropin-releasing hormone (GnRH) agonists or antagonists to suppress ovarian function
- Progestin therapy to inhibit lesion growth
- Pelvic floor physical therapy to address the myofascial components of pelvic pain and the secondary impact of the endometriosis lesions
- Complementary and alternative medicine such as acupuncture and functional or integrative medicine
- Dietary and lifestyle changes
- Psychological support and mental health support
Effective management of endometriosis and the impact of living with endometriosis involves addressing all of the pain generators and associated conditions. A comprehensive approach, incorporating a multidisciplinary approach can significantly improve the overall quality of life for those affected by this challenging condition.
Emerging Diagnostic Approaches
Researchers are actively exploring novel, non-invasive diagnostic methods for endometriosis to reduce the reliance on surgery and improve early detection. One promising area of investigation involves the analysis of endometrial nerve fibers, as studies have shown an increased density of nerve fibers in the endometrium of women with endometriosis compared to those without the condition.
Additionally, researchers are evaluating the potential of serum biomarkers or panels of biomarkers to aid in the diagnosis of endometriosis. While no single biomarker has proven sufficiently accurate thus far, ongoing research aims to identify combinations of markers that can reliably detect the presence and severity of the disease. Other research has focused on better understanding the nature of the disease and factors involved in the mediation of it, including genetics and the influence of the microbiome.
References:
https://www.mayoclinic.org/diseases-conditions/endometriosis/diagnosis-treatment/drc-20354661
https://www.nichd.nih.gov/health/topics/endometri/conditioninfo/diagnose
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2880548
https://www.advancedgynaecologymelbourne.com.au/endometriosis/diagnosis
https://www.webmd.com/women/endometriosis/do-i-have-endometriosis
Updated: September 5, 2024

Endometriosis Surgery Risks
Endometriosis is a condition that affects millions of women around the world. Endometriosis occurs when tissue similar to the tissue found in the uterus grows outside the uterus. This can create intense pain and other health complications, such as infertility. While surgery may be an option for some, it is essential to understand the risks associated with endometriosis surgery before making a decision.
Table of contents
Types of Surgery for Endometriosis
Several types of surgeries exist to treat endometriosis, including minimally invasive (laparoscopy or robotics) and open surgery (laparotomy.) Minimally invasive surgery typically involves making small incisions in the abdomen so that a camera can be inserted into the body to view abnormal endometriosis growths or lesions. Laparotomy involves a larger incision and allows for more extensive examination and treatment. Almost all top endometriosis surgeons worldwide prefer minimally invasive surgery vs. open surgery.
Risks Associated With Endometriosis Surgery
As with any surgery, there are risks associated with endometriosis surgery. These include bleeding, infection, and nerve damage due to surgery or anesthesia during the procedure. During surgical procedures, there is also a risk of harm to surrounding organs such as the bladder or bowels. Additionally, there is a risk that a surgeon will not remove all of the endometriosis tissue during surgery. This incomplete removal could lead to recurrent symptoms or disease if not appropriately addressed by your doctor post-surgery.
Other Treatment Options for Endometriosis
Suppose you are concerned about undergoing surgery for your endometriosis. In that case, other treatment options are available such as hormone therapy or medications used to reduce pain and inflammation caused by endometrial growths or lesions. Additionally, lifestyle changes such as exercise and diet might help reduce endometriosis’s associated symptoms without requiring surgery. Speak with your doctor about other options that may work best for you before deciding on any procedure related to your endometriosis diagnosis.
Find the best endometriosis specialists around the world:
Endometriosis Surgery Costs: Everything You Need to Know
Endometriosis is a chronic gynecological disorder that affects many women. One of the treatments for endometriosis is surgery, which can be expensive. This post will discuss what endometriosis surgery costs and how you can manage these costs.
Table of contents
Endometriosis Surgery
Endometriosis surgery needs minimally invasive tools such as laparoscopy and robotics. The endometriosis surgery usually includes a general anesthetic to reduce pain and discomfort during the procedure. Surgery removes endometrial tissue, scar tissue, and other growths from around the uterus and other organs in the pelvic region. This type of surgery can cost anywhere from $2,500 to $7,500. The cost depends on where you perform the surgery, how severe your endometriosis is, and how long it takes to complete the procedure.
How You Can Manage Endometriosis Surgery Cost?
Other options are available if you don’t have insurance coverage or if your insurance does not cover the cost of endometriosis surgery. Some hospitals offer payment plans or discounts if you pay all or part of your bill upfront. You may also qualify for financial aid programs or grants provided by local organizations or charities that help cover medical expenses for those with limited incomes. Additionally, some states assist with Medicaid programs that can help cover some or all of your medical costs related to endometriosis treatment.
It would be best if you spoke with your doctor about your options before deciding which route to take in terms of paying for endometriosis surgery. Your doctor can recommend a hospital that offers discounted rates or a payment plan that makes it easier for you to manage costs associated with treatment. Many healthcare providers also offer free consultations so you can discuss possible treatment options without any additional cost upfront.
Taking care of your body should never come at a heavy price tag — but unfortunately, endometriosis surgery can be costly. That doesn’t mean there aren’t ways to manage those costs, though! From payment plans to financial aid programs and even grants from local organizations, plenty of resources are available if you need help paying for endometriosis-related medical expenses. Talk with your doctor about your options before making any decisions. With the right resources, getting the care you need shouldn’t feel out of reach!
What is your experience about dealing with surgery costs and finding resources?
Featured Specialists

5 Podcasts About Endometriosis to Listen to Right Now
Do you like listening to podcasts and want to learn more about endometriosis? We got you. There are several teams out there trying to make some sense of endometriosis and bring real-world stories as well as education and news to you. Here we are introducing some podcasts that we found interesting. Please keep reading to learn more about these podcasts.
Table of contents
1- In Sixteen Years of Endometriosis
“Laugh, cry, and shout with us as we talk all things endometriosis. We’re 2 witty best friends that pride ourselves on sharing accurate, well-researched information. We delve into all those embarrassing did-that-really-just-happen?! endo stories, talk vulnerably about our personal growth, and share disease facts with a side of humor. We hope our podcast will support and empower you. —Important note on inclusive language: We hadn’t yet been educated about inclusive language when we began our podcast; but after learning, we used this language midway through the show and going forward.”
2- The Cycle
“The Cycle is a podcast about endometriosis stories from patients as well as helpful information about the disease and ways to cope with it. Our goal is to share endo stories from people all over the world to empower you.
Medical disclaimer: THIS PODCAST IS NOT INTENDED FOR THE PURPOSE OF PROVIDING MEDICAL ADVICE. All information, content, and material of this podcast is for informational purposes only and is not intended to serve as a substitute for the consultation, diagnosis, and/or medical treatment of a qualified physician or healthcare provider.”
3- Not Defined by Endo
“Not Defined by Endo Podcast, hosted by Endometriosis Warrior Teniola Ogunro, is created for and dedicated to women who have been diagnosed with endometriosis or who suffer from symptoms that they suspect to be caused by endometriosis. Every week, Teniola shares her own experiences, interviews health professionals and endo specialists who provide their much-needed insight and speaks to fellow endometriosis warriors who know what it feels like to live with and fight an incurable disease.”
4- Endometriosis | Journey to Butterfly
“This podcast is about my journey with endometriosis over the last 15 plus years including my present day. I will talk all things endometriosis-symptoms, surgery, medical appointments, medications, natural methods, products, eating habits and more. Support this podcast: https://anchor.fm/journeytobutterfly/support.”
5- Peace With Endo
“Peace With Endo encompasses the journey to naturally managing endometriosis through diet, lifestyle and mindful thinking. Endometriosis impacts your body, mind and spirit. (I know this all too well). All three factors need to be addressed if you’re going to heal. I invite you to join the journey.”
Source : Apple podcast

4 Endometriosis Book You Must Read
Disclaimer: This post is not a paid promotion. iCareBetter does not do affiliate marketing and does not get paid if you decide to purchase any of these books. This post is purely informational, and we do not give any medical advice.
Table of contents
1- Beating Endo
How to Reclaim Your Life from Endometriosis
By Iris Kerin Orbuch MD (Author), Amy Stein DPT (Author)
“Approximately one out of every 10 women has endometriosis, an inflammatory disease that causes chronic pain, limits life’s activities, and may lead to infertility. Despite the disease’s prevalence, the average woman may suffer for a decade or more before receiving an accurate diagnosis. Once she does, she’s often given little more than a prescription for pain killers and a referral for the wrong kind of surgery. Beating Endo arms women with what has long been missing—even within the medical community—namely, cutting-edge knowledge of how the disease works and what the endo sufferer can do to take charge of her fight against it.”
2- The Endometriosis Health and Diet Program
Get Your Life Back
by Dr. Andrew S. Cook MD FACOG (Author), Danielle Cook MS RD CDE (Author)
“This timely book will dispel the myths surrounding endometriosis and provide scientifically based recommendations that are easy to understand and follow. It offers recommendations on treating root causes rather than just symptoms — it’s a comprehensive, integrative program for treating endometriosis and serves as a starting point for building an individualized program”
3- Know Your Endo
An Empowering Guide to Health and Hope With Endometriosis
by Jessica Murnane (Author)
“Learn how to navigate your life with endometriosis in this essential and hopeful guide–including tools and strategies to gain a deeper understanding of your body and manage chronic pain through diet, movement, stress management, and more.”
4- The Endo Patient’s Survival Guide
A Patient’s Guide to Endometriosis & Chronic Pelvic Pain
by Andrew S. Cook MD FACOG (Author), Libby Hopton MS (Author), Danielle Cook MS RD CDE (Author)
“The Endo Survival Guide is the patient’s essential companion to living with and overcoming endometriosis and pelvic pain: from seeking help and getting an initial diagnosis, to navigating treatment options, and achieving optimal relief and wellness.”
Source: Amazon

6 Movies & Documentaries About Endometriosis You Need to Watch
Some popular movies and documentaries about endometriosis.
Disclaimer: we don’t necessarily approve of all the content in these shows. But still the impact of these efforts on raising endometriosis awareness is important. We live in a world where most people haven’t even heard the word “endometriosis.” This leads to gaslighting and dismissal of a lot of patients. Therefore, any efforts like these documentaries and movies can change the life of many.
1- All about NINA – Drama, 97 min
“Nina Geld, a brilliant stand-up comedian onstage but an emotional mess offstage, is forced to face her troubled past when she meets Rafe”
2- Endo what? – Documentary
“Women who are suffering from endometriosis and experts discuss treatments for the disease.”
3- The painful truth – Documentary
“a film about endometriosis and adenomyosis”
4- A thousand needles – Short, 29 min
“A Thousand Needles Film is a documentary about the effects of women’s sexual and reproductive health issues like endometriosis on a woman’s life”
5- End-o – Short, 15 min
“Jaq is a typical young woman, navigating the foibles of life, love and endometriosis.”
6- The resilience of woman in pain – short, 27 min
“Rose has been suffering in silence from endometriosis and chronic illness for years. But it’s beginning to wear her down. An unexpected act of kindness from a stranger shows her the power of human connection during hardship.”
source: IMDB & Google Library

