Endometriosis after a hysterectomy or menopause
what are the symptoms of endometriosis after menopause?
Endometriosis does not “die off” or go away with a hysterectomy or menopause. Some people do find some relief from their symptoms, but endometriosis can still persist. Endometriosis often has several related or comorbid conditions (such as adenomyosis or fibroids) that share similar symptoms (pain with menstruation, chronic pelvic pain, etc.) that a hysterectomy might help – but it may not stop your symptoms from endometriosis. Endometriosis exists outside of the uterus and can still respond to hormonal influences (Bulun et al., 2002). Even if your ovaries are removed, endometriosis lesions can produce their own estrogen (Huhtinen et al., 2012). This is important to note because estrogen causes endometriosis lesions to grow and persist (Bulun et al., 2012). So even with the removal of the ovaries or with menopause, endometriosis can sustain itself.
There is high recurrence of symptoms with the removal of just the uterus; but, even with the removal of the ovaries, any endometriosis lesions left behind can continue to grow, progress, and cause symptoms (Clayton et al., 1999; Inceboz, 2015; Khan et al., 2013; Rizk et al., 2014). So, if you have your uterus and ovaries removed for other conditions, it is best that all endometriosis lesions be removed as well. The skill of the surgeon at removing all endometriosis is important. Rizk et al. (2014) report that “the recurrence of endometriosis symptoms and pelvic pain are directly correlated to the surgical precision and removal of peritoneal and deeply infiltrated disease.”
Endometriosis has been found in about 2.2% of postmenopausal women (Zanello et al., 2019). Inceboz (2015) states that “endometriotic lesions remained biologically active, with proliferative activity and preserved hormonal responsiveness, even in the lower estrogenic environment in the postmenopause.” Postmenopausal endometriosis should be managed surgically according to Streuli et al. (2017) and Zanello et al. (2019).
What about hormone replacement if you are in menopause or have had your uterus and ovaries removed? Hormone replacement therapy (HRT) is important as “the hypo-estrogenic state was demonstrated to be a risk factor for cardiovascular and bone disease” (Zanello et al., 2019). While HRT has not been concluded useful for preventing heart disease, it can be useful for those at a higher risk of osteoporosis (Zanello et al., 2019). There isn’t much data available to help guide the decision, but Zanello et al. (2019) report that “in young menopausal women with premature or surgically-induced menopause the benefits of HRT probably overcome the risks” and “in women with residual endometriosis after surgery, the use of HRT should be discussed and the risk of recurrence should be carefully considered before starting an estrogen-based replacement therapy”. Rizk et al. (2014) also states that “the general consensus is that the benefits outweigh the risks” and that starting HRT soon after menopause does not seem to have a faster rate of recurrence. Zanello et al. (2019) concludes that “based on low-grade evidence in the literature, we recommend prescribing combined HRT instead of unopposed estrogen.” It also depends on if your endometriosis was removed.
Does Endometriosis Go Away After Menopause?
endometriosis symptoms after menopause
References
Bulun, S. E., Gurates, B., Fang, Z., Tamura, M., Sebastian, S., Zhou, J., … & Yang, S. (2002). Mechanisms of excessive estrogen formation in endometriosis. Journal of reproductive immunology, 55(1-2), 21-33. Retrieved from https://doi.org/10.1016/S0165-0378(01)00132-2
Bulun, S. E., Monsavais, D., Pavone, M. E., Dyson, M., Xue, Q., Attar, E., … & Su, E. J. (2012, January). Role of estrogen receptor-β in endometriosis. In Seminars in reproductive medicine (Vol. 30, No. 01, pp. 39-45). Thieme Medical Publishers. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4034571/…
Clayton, R. D., Hawe, J. A., Love, J. C., Wilkinson, N., & Garry, R. (1999). Recurrent pain after hysterectomy and bilateral salpingo‐oophorectomy for endometriosis: evaluation of laparoscopic excision of residual endometriosis. BJOG: An International Journal of Obstetrics & Gynaecology, 106(7), 740-744. Retrieved from https://obgyn.onlinelibrary.wiley.com/doi/full/10.1111/j.1471-0528.1999.tb08377.x?fbclid=IwAR04aFoLsukqsYutNPNXtJNZpKLNEJbgOOon334NW8D7wvwzZMWaS2YaZts
Huhtinen, K., Ståhle, M., Perheentupa, A., & Poutanen, M. (2012). Estrogen biosynthesis and signaling in endometriosis. Molecular and cellular endocrinology, 358(2), 146-154. Retrieved from https://www.sciencedirect.com/science/article/abs/pii/S0303720711005041
Inceboz, U. (2015). Endometriosis after menopause. Women’s Health, 11(5), 711-715. Retreived from https://journals.sagepub.com/doi/full/10.2217/whe.15.59
Khan, K. N., Kitajima, M., Fujishita, A., Nakashima, M., & Masuzaki, H. (2013). Toll‐like receptor system and endometriosis. Journal of Obstetrics and Gynaecology Research, 39(8), 1281-1292. Retrieved from https://obgyn.onlinelibrary.wiley.com/doi/full/10.1111/jog.12117
Rizk, B., Fischer, A. S., Lotfy, H. A., Turki, R., Zahed, H. A., Malik, R., … & Herrera, D. (2014). Recurrence of endometriosis after hysterectomy. Facts, views & vision in ObGyn, 6(4), 219. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4286861/
Zanello, M., Borghese, G., Manzara, F., Degli Esposti, E., Moro, E., Raimondo, D., … & Seracchioli, R. (2019). Hormonal replacement therapy in menopausal women with history of endometriosis: a review of literature. Medicina, 55(8), 477. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6723930/

Endometriosis and Pregnancy
Endometriosis is often associated with infertility. Infertility does not mean you cannot get pregnant, but rather there is a delay in achieving pregnancy. It is technically defined as not achieving a “clinical pregnancy after 12 months or more of regular unprotected sexual intercourse” (World Health Organization, n.d.). An estimated 30–50% of women with endometriosis are reported to have difficulty with infertility (Macer & Taylor, 2012). In addition, endometriosis does not have to be an “advanced stage” for it to affect fertility (Bloski & Pierson, 2008).
“Current evidence indicates that suppressive medical treatment of endometriosis does not benefit fertility and should not be used for this indication alone. Surgery is probably efficacious for all stages of the disease.”
(Ozkan, Murk, & Arici, 2008)
With infertility being related to endometriosis, it is unbelievable that pregnancy might still be recommended as a treatment for endometriosis. While some may have a temporary relief of symptoms, others can experience an increase. In fact, some “imaging and histopathology studies of endometriotic lesions during pregnancy show that they may grow rapidly during pregnancy” (Leeners & Farquhar, 2019). Pregnancy will not treat or cure endometriosis. Research has stated that “women aiming for pregnancy on the background of endometriosis should not be told that pregnancy may be a strategy for managing symptoms and reducing progression of the disease” (Leeners et al., 2018). This is echoed again by Leeners and Farquhar (2019) who point out that “the decision to have children should not be influenced by any perceived benefit of improving endometriosis but should be made solely on the wish for parenthood.”
While the overall risk is still low, endometriosis has been associated with some difficulties during pregnancy. Zullo et al. (2017) looked at 24 studies involving almost 2 million women with endometriosis to consider the possible effects of endometriosis during pregnancy . They found that “women with endometriosis have a statistically significantly higher risk of preterm birth, miscarriage, placenta previa, small for gestational age infants, and cesarean delivery” compared to healthy controls (Zullo et al., 2017). Zullo et al. (2017) did not find any significant association with gestational hypertension and preeclampsia with endometriosis; however, adenomyosis has been found to have some correlation with pregnancy-induced hypertension and preeclampsia (Porpora et al., 2020). Adenomyosis has been found to result in a higher likelihood of preterm birth, small for gestational age, and pre-eclampsia (Razavi et al., 2019). Adenomyosis and endometriosis frequently coexist, so it can be hard to determine how much is one or the other causing these effects (Choi et al., 2017).
On a positive note, Porpora et al. (2020) noted that “no difference in fetal outcome was found” and concluded that “endometriosis does not seem to influence fetal well-being”. This was also found by Uccella et al. (2019), stating that “neonatal outcomes are unaffected by the presence of the disease”. Again, a normal pregnancy is still highly possible. For more information on this topic, see Pregnancy and Endometriosis.
References
Bloski, T., & Pierson, R. (2008). Endometriosis and chronic pelvic pain: unraveling the mystery behind this complex condition. Nursing for women’s health, 12(5), 382-395. doi: 10.1111/j.1751-486X.2008.00362.x
Choi, E. J., Cho, S. B., Lee, S. R., Lim, Y. M., Jeong, K., Moon, H. S., & Chung, H. (2017). Comorbidity of gynecological and non-gynecological diseases with adenomyosis and endometriosis. Obstetrics & gynecology science, 60(6), 579. Retrieved from https://synapse.koreamed.org/upload/SynapseData/PDFData/3021ogs/ogs-60-579.pdf
Leeners, B., Damaso, F., Ochsenbein-Kölble, N., & Farquhar, C. (2018). The effect of pregnancy on endometriosis—facts or fiction?. Human reproduction update, 24(3), 290-299. Retrieved from https://doi.org/10.1093/humupd/dmy004
Leeners, B., & Farquhar, C. M. (2019). Benefits of pregnancy on endometriosis: can we dispel the myths?. Fertility and sterility, 112(2), 226-227. Retrieved from https://doi.org/10.1016/j.fertnstert.2019.06.002
Macer, M. L., & Taylor, H. S. (2012). Endometriosis and infertility: a review of the pathogenesis and treatment of endometriosis-associated infertility. Obstetrics and Gynecology Clinics, 39(4), 535-549. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3538128/pdf/nihms422379.pdf
Ozkan, S., Murk, W., & Arici, A. (2008). Endometriosis and infertility: epidemiology and evidence‐based treatments. Annals of the New York Academy of Sciences, 1127(1), 92-100. DOI: 10.1196/annals.1434.007
Porpora, M. G., Tomao, F., Ticino, A., Piacenti, I., Scaramuzzino, S., Simonetti, S., … & Benedetti Panici, P. (2020). Endometriosis and pregnancy: a single institution experience. International journal of environmental research and public health, 17(2), 401. Retrieved from https://www.mdpi.com/1660-4601/17/2/401
Razavi, M., Maleki‐Hajiagha, A., Sepidarkish, M., Rouholamin, S., Almasi‐Hashiani, A., & Rezaeinejad, M. (2019). Systematic review and meta‐analysis of adverse pregnancy outcomes after uterine adenomyosis. International Journal of Gynecology & Obstetrics, 145(2), 149-157. Retrieved from https://www.endometriozisdernegi.org/konu/dosyalar/pdf/makale_ozetleri/Mayis2019/makale17.pdf
Uccella, S., Manzoni, P., Cromi, A., Marconi, N., Gisone, B., Miraglia, A., … & Ghezzi, F. (2019). Pregnancy after endometriosis: maternal and neonatal outcomes according to the location of the disease. American journal of perinatology, 36(S 02), S91-S98. DOI: 10.1055/s-0039-1692130
World Health Organization. (n.d.).Infertility definitions and terminology. Retrieved from https://www.who.int/teams/sexual-and-reproductive-health-and-research/areas-of-work/fertility-care/infertility-definitions-and-terminology
Zullo, F., Spagnolo, E., Saccone, G., Acunzo, M., Xodo, S., Ceccaroni, M., & Berghella, V. (2017). Endometriosis and obstetrics complications: a systematic review and meta-analysis. Fertility and sterility, 108(4), 667-672. Retrieved from https://doi.org/10.1016/j.fertnstert.2017.07.019

How to Study a Research Study
We post a lot of links and references to research studies, but it can be difficult to interpret them. Even harder is determining how relevant those studies are. Here are a few things to consider as you look at research on endometriosis.
When you look at research studies, you first want to assess how strong of evidence it is presenting. One quick way to tell is by the type of study. The University of Alabama at Birmingham (2021) has a good list of the types of studies, going from strongest evidence to weakest. In short:
“The most scientific, rigorous study designs are randomized controlled trials, systematic reviews, and meta-analysis. These types of studies are thought to provide stronger levels of evidence because they reduce, but do not eliminate, potential biases and confounders.”
(University of Alabama at Birmingham, 2021)
Bias is any errors in design that might throw off the conclusions. Bias, whether intentional or unintentional, can occur in “data collection, data analysis, interpretation and publication which can cause false conclusions” (Simundic, 2013). Find out more about that here. Confounding factors are any variables not factored into the study that can muddle with the interpretation of the results- “they can suggest there is correlation when in fact there isn’t” (Statistics How To, n.d.). This is important when looking at the conclusions drawn. For instance, in last week’s newsletter about endometriomas, we noted that recurrence rates are hard to tell from studies because their definition of “recurrence” varies widely from study to study (was it pathology from surgery or recurrence of symptoms that might actually be from a related condition?). You also want to look how large the study was, did it include several different variables, was it limited to a specific group, how was the study funded and what ethical considerations are given, etc. One tool for helping to analyze such factors can be found here.
Most studies have a short summary at the beginning that can be helpful. For instance, let’s look at this study from Shigesi et al. (2019) found here. The title itself tells us it is a systematic review and meta-analysis: “The association between endometriosis and autoimmune diseases: a systematic review and meta-analysis”. So, we’re starting off good.
The study then starts with the summary called an abstract- which tells us the background of the problem they want to study, how they performed the study, the outcomes they found, and a discussion on what those outcomes mean. In the background, they state that “an association between endometriosis and autoimmune diseases has been proposed”, so that is what they are studying. Then they detail how they are going to study it- what databases they are using to look for information, what they are going to include or exclude from their study, and the statistical analysis they will utilize. They next present the outcomes: “the studies quantified an association between endometriosis and several autoimmune diseases, including systemic lupus erythematosus (SLE), Sjögren’s syndrome (SS), rheumatoid arthritis (RA), autoimmune thyroid disorder, coeliac disease (CLD), multiple sclerosis (MS), inflammatory bowel disease (IBD), and Addison’s disease”. But wait! There is a caveat they note- “the quality of the evidence was generally poor due to the high risk of bias in the majority of the chosen study designs and statistical analyses” and that “only 5 of the 26 studies could provide high-quality evidence”. Then they present their conclusions of how this information might be useful- “the observed associations between endometriosis and autoimmune diseases suggest that clinicians need to be aware of the potential coexistence of endometriosis and autoimmune diseases when either is diagnosed”. They end by giving suggestions for future research that might strengthen the body of evidence for this. In short, after looking deeper into the association, the evidence available is overall poor so more research is warranted.
This is by no means a comprehensive review of looking at research study but rather a brief intro. There are many available resources on the internet for looking more in depth about how to assess research and draw conclusions from it.
References
Shigesi, N., Kvaskoff, M., Kirtley, S., Feng, Q., Fang, H., Knight, J. C., … & Becker, C. M. (2019). The association between endometriosis and autoimmune diseases: a systematic review and meta-analysis. Human reproduction update, 25(4), 486-503. Retrieved from https://academic.oup.com/humupd/article/25/4/486/5518352?login=true
Simundic, A. M. (2013). Bias in research. Biochemia medica, 23(1), 12-15. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3900086/
Statistics How To. (n.d.). Confounding Variable: Simple Definition and Example. Retrieved from https://www.statisticshowto.com/experimental-design/confounding-variable/
University of Alabama at Birmingham. (2021). Study Types- Definitions. Retrieved from https://guides.library.uab.edu/ebd/evidencestrength
The Aggravating Endometrioma
What are endometriomas anyway? Endometriosis is classified into three main types: superficial peritoneal endometriosis, deep infiltrating endometriosis, and endometriomas (see more about that here). Endometriomas are ovarian cysts lined by endometriotic tissue and can be filled with blood (why they are at times called “chocolate cysts”). Like the other types of endometriosis, no one knows for sure how they form. It has been theorized that endometriosis tissue on the surface of the ovary invades and forms a cyst like formation or they start as a functional ovarian cyst with gradual infiltration of endometriotic tissue. Endometriomas have been found in up to 44% of those with endometriosis and are associated with deep infiltrating endometriosis (Cranney, Condous, & Reid, 2017).
Endometriomas can be suspected with ultrasound or MRI, but as with other types of endometriosis, surgery is gold standard for diagnosis (Gałczyński et al., 2019). Endometrioma treatment can often be focused on the effect on fertility, so it is important to consider your goals when looking at treatment options. While medications are used to manage endometriomas, “endometriomas do not respond to medical therapy alone, thus usually surgical treatment is necessary” (Gałczyński et al., 2019). Many may be hesitant to perform surgery for fear of loss of healthy ovarian function and may put off surgery until the endometrioma reaches a certain size. However, Gałczyński et al. (2019) reports that treating “early-stage endometrioma provides less damage to the ovary by a less invasive surgical procedure which decreases the risk of iatrogenic premature ovarian failure” and that “long-term ovarian endometriosis leads to persistent inflammation” that can lead to loss of ovarian function. Skill of the surgeon is important in this aspect.
Gałczyński et al. (2019) reports that “the level of expertise in endometriotic surgery is inversely correlated with inadvertent removal of healthy ovarian tissue along with the endometrioma capsule”. There are multiple surgical techniques that can be used to treat endometriomas and there is no consensus on the best method, although ovarian cystectomy (removal of the ovarian cyst) is the preferred method based on studies (Pais et al., 2021). One recently published study cites “excisional surgery allows for pain resolution, a high rate of spontaneous pregnancies and a lower recurrence rate of ovarian cysts when compared to drainage and ablation techniques” (Angioni et al., 2021).
The aggravating thing about endometriomas is the likelihood of recurrence. It can hard to tell true recurrence rates from studies because “recurrence is variously defined in the literature as the relapse of pain, clinical or instrumental detection of an endometriotic lesion, repeat rise in CA 125 levels, or evidence of recurrence found during repeat surgery,” which results in the wide range of reported recurrence in studies (Ceccaroni et al., 2019). In addition, the method of surgical treatment has a bearing on recurrence rate (excision versus draining etc.). One study reported recurrence rates to be “24.2% for patients aged 20–30 years, 17.7% for 31–40 years, and 7.9% for 41–45 years” (Li et al., 2019). Other studies have echoed that younger age was linked to increased recurrence (Gałczyński et al., 2019). While younger age seems to have a direct correlation with recurrence, other factors not as much. For instance, Gałczyński et al. (2019) reports that the “diameter of the tumor, stage of endometriosis, coexistence of deep-infiltrating endometriosis, or uni- or bi-lateral involvement of ovaries were all not associated with the risk of recurrence” and that the “median time to recurrence was 53 months”.
There is also controversy about the use of hormonal suppression to prevent recurrence. Some studies and a meta-analysis report that there is not enough evidence for the use of medications to help prevent recurrence, while others indicate that it may delay but will not prevent recurrence (Gałczyński et al., 2019; Li et al., 2019; Wattanayingcharoenchai et al., 2021). Confusing? Others agree that it is- with one commentary stating that “so what are we to believe and what should we advise women affected by endometriosis to do?” (Saridogan, 2020). In the end, we each have to do our research, look at our individual goals, and decide what is best for our unique situation.
Endometriosis after a hysterectomy or menopause
References
Angioni, S., Scicchitano, F., Sigilli, M., Succu, A. G., Saponara, S., & D’Alterio, M. N. (2021). Impact of Endometrioma Surgery on Ovarian Reserve. In Endometriosis Pathogenesis, Clinical Impact and Management (pp. 73-81). Springer, Cham. Retrieved from https://link.springer.com/chapter/10.1007/978-3-030-57866-4_8
Ceccaroni, M., Bounous, V. E., Clarizia, R., Mautone, D., & Mabrouk, M. (2019). Recurrent endometriosis: a battle against an unknown enemy. The European Journal of Contraception & Reproductive Health Care, 24(6), 464-474. Retrieved from https://www.tandfonline.com/doi/abs/10.1080/13625187.2019.1662391
Cranney, R., Condous, G., & Reid, S. (2017). An update on the diagnosis, surgical management, and fertility outcomes for women with endometrioma. Acta obstetricia et gynecologica Scandinavica, 96(6), 633-643. Retrieved from https://obgyn.onlinelibrary.wiley.com/doi/full/10.1111/aogs.13114
Gałczyński, K., Jóźwik, M., Lewkowicz, D., Semczuk-Sikora, A., & Semczuk, A. (2019). Ovarian endometrioma–a possible finding in adolescent girls and young women: a mini-review. Journal of ovarian research, 12(1), 1-8. Retrieved from https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-019-0582-5
Li, X. Y., Chao, X. P., Leng, J. H., Zhang, W., Zhang, J. J., Dai, Y., … & Wu, Y. S. (2019). Risk factors for postoperative recurrence of ovarian endometriosis: long-term follow-up of 358 women. Journal of ovarian research, 12(1), 1-10. Retrieved from https://link.springer.com/article/10.1186/s13048-019-0552-y
Pais, A. S., Flagothier, C., Tebache, L., Almeida Santos, T., & Nisolle, M. (2021). Impact of Surgical Management of Endometrioma on AMH Levels and Pregnancy Rates: A Review of Recent Literature. Journal of Clinical Medicine, 10(3), 414. Retrieved from https://www.mdpi.com/2077-0383/10/3/414
Saridogan, E. (2020). Postoperative medical therapies for the prevention of endometrioma recurrence–do we now have the final answer?(Mini-commentary on BJOG-19-1705. R2). Authorea Preprints. Retrieved from https://d197for5662m48.cloudfront.net/documents/publicationstatus/41937/preprint_pdf/d4903f81caf3e8838e672d7631e6b8bd.pdf
Wattanayingcharoenchai, R., Rattanasiri, S., Charakorn, C., Attia, J., & Thakkinstian, A. (2021). Postoperative hormonal treatment for prevention of endometrioma recurrence after ovarian cystectomy: a systematic review and network meta‐analysis. BJOG: An International Journal of Obstetrics & Gynaecology, 128(1), 25-35. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32558987/

Celiac Disease and Endometriosis
Much like thyroid disease and endometriosis, there are not many studies looking at an association between celiac disease and endometriosis. One study found the “risk of endometriosis in patients with [celiac disease] was 112/100 000 person” (Stephansson et el., 2011). Another noted that celiac disease “is common in this population group [women with endometriosis and infertility] (2.5%) and may be clinically relevant” (Aguiar et al., 2009). Another study noted a slightly increased risk of celiac disease in those with endometriosis (“Celiac disease was diagnosed in 5 of 223 women with endometriosis and in 2 of 246 controls (2.2% versus 0.8%)”) (Seracchiolo et al., 2014). Some have had positive results on endometriosis symptoms from following a gluten free diet (Marziali et al., 2012).
On the flip side, celiac disease can present with symptoms similar to endometriosis. “Celiac disease has also been associated with chronic pelvic pain, including dysmenorrhea and deep dyspareunia” and “patients with atypical pelvic pain, particularly with GI components, may also benefit from screening” (Ory & Christie, 2013). This points out the importance of looking beyond the diagnosis of endometriosis with recurring symptoms in order to rule out other health issues that can mimic endometriosis symptoms.
References
Aguiar, F. M., Melo, S. B., Galvao, L. C., Rosa-e-Silva, J. C., dos Reis, R. M., & Ferriani, R. A. (2009). Serological testing for celiac disease in women with endometriosis. A pilot study. Clinical and experimental obstetrics & gynecology, 36(1), 23-25. Retrieved from https://pubmed.ncbi.nlm.nih.gov/19400413/
Marziali, M., Venza, M., Lazzaro, S., Lazzaro, A., Micossi, C., & Stolfi, V. M. (2012). Gluten-free diet: a new strategy for management of painful endometriosis related symptoms. Minerva Chir, 67(6), 499-504. Retrieved from https://www.minervamedica.it/en/journals/minerva-surgery/article.php?cod=R06Y2012N06A0499
Ory, S. J., & Christie, D. R. (2013). Reproductive effects of celiac disease. Contemporary OB/GYN, 58(4), 34. Retrieved from https://www.contemporaryobgyn.net/view/reproductive-effects-celiac-disease
Seracchioli, R., Montanari, G., Mabrouk, M., & Nassif, J. (2014). Endometriosis: novel models, diagnosis, and treatment. Retrieved from https://doi.org/10.1155/2014/236821
Stephansson, O., Falconer, H., & Ludvigsson, J. F. (2011). Risk of endometriosis in 11 000 women with celiac disease. Human reproduction, 26(10), 2896-2901. Retrieved from https://doi.org/10.1093/humrep/der263

Keep Endometriosis Awareness Going
As we come to the end of endometriosis awareness month, those of us with endometriosis knows it doesn’t end in March. Raising awareness and fighting against misinformation is a constant effort. Please feel free to share links from the webpage. The more we share, the more awareness and up-to-date information is out there for others. It can be discouraging to see so much of the same old misinformation perpetuated that can cause others to suffer as we have. Let’s spread hope!
We have collected all the infographs shared on Nancy’s Nook Facebook page and have sprinkled them throughout the website so that you can share the infograph and the link to more information. All the infographs are also collected here.
Endometriosis Quick Facts to Share is also another good resource to share. One of my favorites to reference to is the Myths and Misinformation page. Keep the awareness going, because endometriosis doesn’t stop in March.






The Personal Burden of Endometriosis
Last week we looked at the direct financial burden of endometriosis, including the loss of education, loss of productivity at work and home, and loss of income. Today we look at the personal burden of endometriosis- the altered relationships with family and friends, the pain and suffering, the ill effects on mental health, and the loss of who we feel we are as a person because of it.
Pain and fatigue can limit our ability to function and the quality of our life experience (Missmer et al., 2021). Our ability to maintain relationships can be difficult, especially when others do not understand the impact that endometriosis has on us. Much research has shown the effect on intimate partner relationships due to the interference with sexual health (Missmer et al., 2021). Not as many studies have been done on the effects of parenting with endometriosis; however, in our Facebook group Nancy’s Nook, many of you have shared the significant effect endometriosis has had on the ability to function as a parent. These limitations imposed from our illness can affect our mental health as well.
In studies, people with endometriosis express “feelings of worthlessness, guilt, and frustration connected with disease-related limitations on participation in daily activities, social functioning, independence, and interpersonal relationships” as well as frustration “from a woman’s inability to manage or predict her pain and the feeling that endometriosis/endometriosis-associated pain controls her life” (Missmer et al., 2021). Add to this the burden of the “perception that others (even healthcare professionals) consider what they are experiencing to be ‘all in their heads’” (Missmer et al., 2021). The struggle is real. And it is no wonder that many feel a loss of who they are as a person because of it.
On a positive note, a systematic review and meta-analysis, as well as other studies, reveal that surgery for endometriosis does improve quality of life (Arcoverde et al., 2019; Parra et al., 2021). Another study reports that “laparoscopic surgery is associated with improved quality of life and emotional well-being compared to medical therapies” and cautions that “although the GnRH agonists are effective in reducing endometriosis symptoms, they are often associated with anxiety and depression during treatment” (Laganà et al., 2017). To help manage symptoms, one study that surveyed people with endometriosis found that “heat (70%), rest (68%), and meditation or breathing exercises (47%)” helped and to a lesser degree “yoga/Pilates, stretching, and exercise” (Armour et al., 2019). Changes in diet, individualized to your specific needs, can help with symptom management for some (Karlsson, Patel, & Premberg, 2020). Other things such as acupuncture have been helpful to some as well. Mental healthcare is important to our well-being and should not be neglected either.
The impact endometriosis has on our lives is significant. Know that you are not alone.

References
Arcoverde, F. V. L., de Paula Andres, M., Borrelli, G. M., de Almeida Barbosa, P., Abrão, M. S., & Kho, R. M. (2019). Surgery for endometriosis improves major domains of quality of life: a systematic review and meta-analysis. Journal of minimally invasive gynecology, 26(2), 266-278. Retrieved from https://doi.org/10.1016/j.jmig.2018.09.774
Armour, M., Sinclair, J., Chalmers, K. J., & Smith, C. A. (2019). Self-management strategies amongst Australian women with endometriosis: a national online survey. BMC complementary and alternative medicine, 19(1), 1-8. Retrieved from https://link.springer.com/article/10.1186/s12906-019-2431-x
Karlsson, J. V., Patel, H., & Premberg, A. (2020). Experiences of health after dietary changes in endometriosis: a qualitative interview study. BMJ open, 10(2), e032321. Retrieved from https://bmjopen.bmj.com/content/10/2/e032321.abstract
Laganà, A. S., La Rosa, V. L., Rapisarda, A. M. C., Valenti, G., Sapia, F., Chiofalo, B., … & Vitale, S. G. (2017). Anxiety and depression in patients with endometriosis: impact and management challenges. International journal of women’s health, 9, 323. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5440042/
Missmer, S. A., Tu, F. F., Agarwal, S. K., Chapron, C., Soliman, A. M., Chiuve, S., … & As-Sanie, S. (2021). Impact of Endometriosis on Life-Course Potential: A Narrative Review. International Journal of General Medicine, 14, 9. doi: 10.2147/IJGM.S261139
Parra, R. S., Feitosa, M. R., Camargo, H. P. D., Valério, F. P., Zanardi, J. V. C., Rocha, J. J. R. D., & Féres, O. (2021). The impact of laparoscopic surgery on the symptoms and wellbeing of patients with deep infiltrating endometriosis and bowel involvement. Journal of Psychosomatic Obstetrics & Gynecology, 42(1), 75-80. Retrieved from https://doi.org/10.1080/0167482X.2020.1773785

The Costly Burden of Endometriosis
Endometriosis has a powerful cost in terms of quality of life. However, there are financial costs as well. Financial loss can come from direct healthcare costs as well as loss of productivity. The estimated annual cost between those two in 2009 was $69.4 billion (Della Corte et al., 2020).
Della Corte et al. (2020) notes that “in employed women with endometriosis, as a consequence of productivity loss of 6.3 h per week, the total loss per person is approximately $10,177.54 per year.” Chronic pain is a significant factor in the loss of productivity and Armour et al. (2019) concludes that “priority should be given to improving pain control in women with pelvic pain.” Similarly, Facchin et al. (2019) notes that those with greater severity of symptoms were less likely to be employed and state that “endometriosis symptoms may significantly affect women’s professional life, with important socioeconomic, legal, and political implications.” The loss of productivity doesn’t only affect the workplace. Soliman et al. (2017) found that there was loss of household productivity as well.
The loss of productivity can start with symptom onset, starting in adolescence. Missmer et al. (2021) state that “endometriosis (and its associated symptoms) has been shown to hamper educational attainment, hinder work productivity, alter career choices and success, impair social life and activities, affect family choices, induce strain in personal relationships, negatively influence mental and emotional health, and adversely affect [quality of life]. These multiple and pervasive effects are anticipated to materially alter the life-course trajectory of women with endometriosis.”
So how can we help this? Earlier diagnosis and successful treatment are key. Surrey et al. (2020) notes that “patients with endometriosis who had longer diagnostic delays had more pre-diagnosis endometriosis-related symptoms and higher pre-diagnosis healthcare utilization and costs compared with patients who were diagnosed earlier after symptom onset, providing evidence in support of earlier diagnosis.” On the same note, Missmer et al. (2021) state that “unfortunately, current practice models too often result in a prolonged delay between symptom onset, diagnosis, and treatment of endometriosis, thereby increasing the impact on the life course.” This is why we advocate and share evidence-based information- so that the next person doesn’t have their life so significantly altered by endometriosis.
References
Armour, M., Lawson, K., Wood, A., Smith, C. A., & Abbott, J. (2019). The cost of illness and economic burden of endometriosis and chronic pelvic pain in Australia: A national online survey. PloS one, 14(10), e0223316. Retrieved from https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0223316
Della Corte, L., Di Filippo, C., Gabrielli, O., Reppuccia, S., La Rosa, V. L., Ragusa, R., … & Giampaolino, P. (2020). The burden of endometriosis on women’s lifespan: a narrative overview on quality of life and psychosocial wellbeing. International Journal of Environmental Research and Public Health, 17(13), 4683. Retrieved from https://www.mdpi.com/1660-4601/17/13/4683/htm
Facchin, F., Buggio, L., Ottolini, F., Barbara, G., Saita, E., & Vercellini, P. (2019). Preliminary insights on the relation between endometriosis, pelvic pain, and employment. Gynecologic and obstetric investigation, 84(2), 190-195. Retrieved from https://doi.org/10.1159/000494254
Missmer, S. A., Tu, F. F., Agarwal, S. K., Chapron, C., Soliman, A. M., Chiuve, S., … & As-Sanie, S. (2021). Impact of Endometriosis on Life-Course Potential: A Narrative Review. International Journal of General Medicine, 14, 9. doi: 10.2147/IJGM.S261139
Soliman, A. M., Coyne, K. S., Gries, K. S., Castelli-Haley, J., Snabes, M. C., & Surrey, E. S. (2017). The effect of endometriosis symptoms on absenteeism and presenteeism in the workplace and at home. Journal of managed care & specialty pharmacy, 23(7), 745-754. Retrieved from https://doi.org/10.18553/jmcp.2017.23.7.745
Surrey, E., Soliman, A. M., Trenz, H., Blauer-Peterson, C., & Sluis, A. (2020). Impact of endometriosis diagnostic delays on healthcare resource utilization and costs. Advances in therapy, 37(3), 1087-1099. Retrieved from https://link.springer.com/article/10.1007/s12325-019-01215-x
Endometriosis Quick Facts to Share
What is endometriosis?
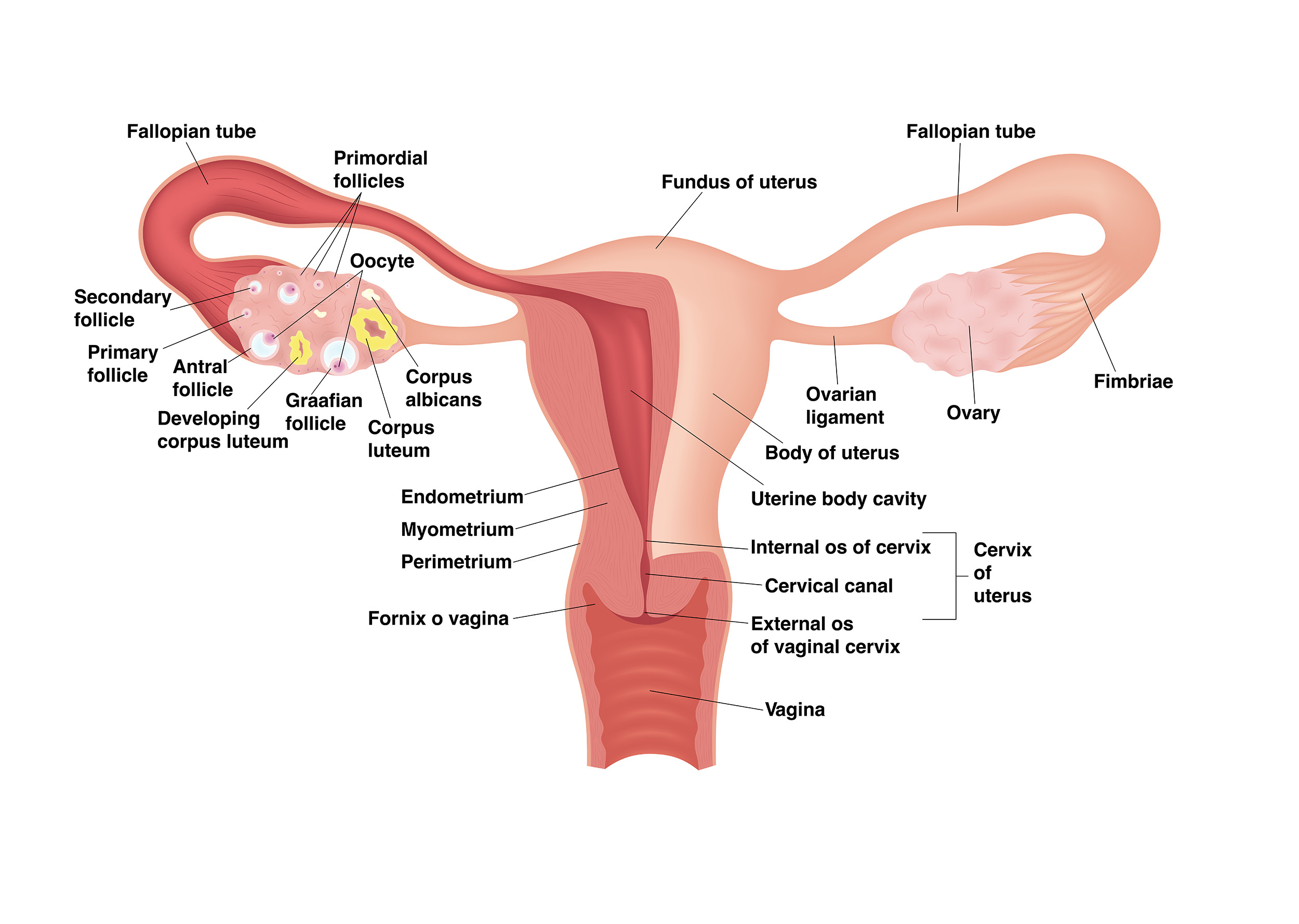
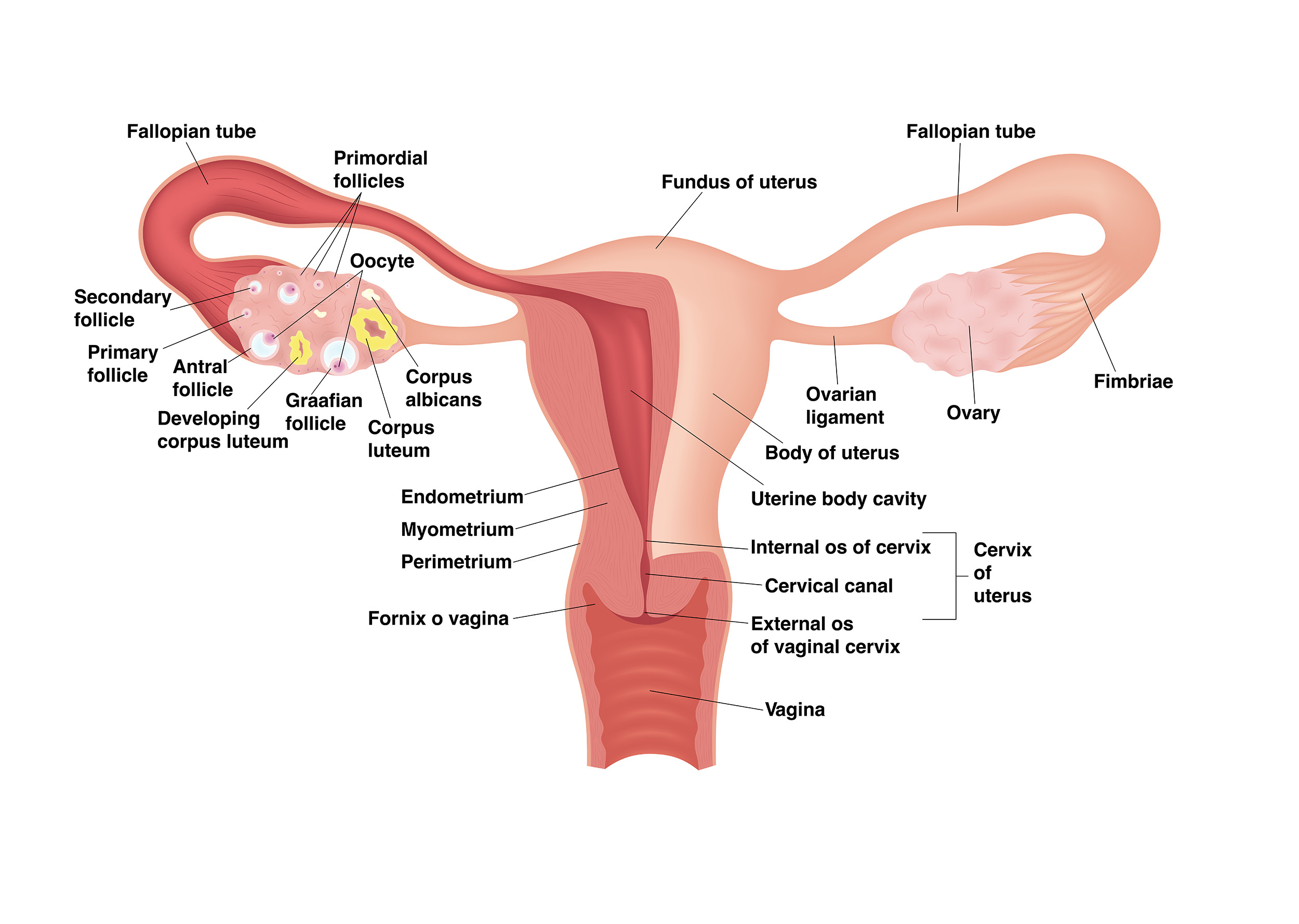
Endometriosis is an inflammatory disorder where lesions similar to the lining of the uterus are located outside of the uterus. Endometriosis lesions have distinct differences from the lining of the uterus in both their form and function. The lesions release proinflammatory chemicals, can produce estrogen, can grow their own nerves and blood vessels, and can cause adhesions. It is usually located in the pelvis but has been found in other areas throughout the body. An estimated 11% of people assigned female at birth (including teenagers)have endometriosis- although it has been found in men on rare occasion.
What causes it?
No one knows. There is a genetic component, with higher rates seen in those with close relatives having endometriosis. It has been found in fetuses, suggesting it is present before birth.
What are its symptoms?
Endometriosis has many symptoms- from chronic pelvic pain to fatigue to infertility. Symptom severity does not necessarily correlate with the extent of lesions.
- Pain: chronic pelvic pain, pain with menses, pain in between menses, pain with exercise, pain with sex, pain with bowel movements, pain with urination, low back pain
- Fatigue
- Bowel symptoms similar to irritable bowel syndrome such as constipation, diarrhea, and bloating
- Infertility
- And many others
How is diagnosed?
Endometriosis is diagnosed with surgery, preferably with pathology from tissue samples. Some imaging, such as MRI’s and ultrasounds, can rule in endometriosis, but they cannot rule it out. The accuracy of diagnosis depends on the knowledge and skill of the provider.
How is it treated?
While there is no definitive cure for endometriosis, excision surgery where all lesions are removed is recommended. The skill and knowledge of the surgeon is paramount in the ability to recognize and remove all lesions. Hormonal medication might help temporarily with symptom management, but it cannot be used to diagnosis, cure (“clean up”), or prevent the progression of endometriosis. Endometriosis can persist after a hysterectomy or menopause. Endometriosis is often present with other painful conditions such as adenomyosis and interstitial cystitis.
For more information see: nancysnookendo.com
Reaching Out To Teach Another: nancysnookendo.com/support-us/


Chronic Pelvic Pain: More Than Endometriosis Alone
If you have chronic pelvic pain, endometriosis is likely- endometriosis is diagnosed in up to 80% of patients with chronic pelvic pain (Butrick, 2007). Endometriosis is bad enough, but it is frequently accompanied by other conditions that can cause chronic pelvic pain and other symptoms similar to endometriosis. For instance:
- Adenomyosis: Adenomyosis and endometriosis have been found together anywhere from 21.8% to 79% of the time (Antero et al., 2017; Di Donato et al., 2014; Kunz et al., 2005).
- Interstitial cystitis (IC): The so-called “evil twin” of endometriosis occurs in anywhere between 33-65% of people with endometriosis (Butrick, 2007; Chung et al., 2005). One article stated that “if [endometriosis] symptoms recur within the first 12 months after surgical therapy, IC should be considered as a possible cause” or “when therapy for the symptoms of endometriosis is unsuccessful, increasing evidence suggests that IC may be an underlying cause” (Butrick, 2007).
- Endometrial/uterine polyps: Uterine polyps have been found in 48% of people with endometriosis (Zhang et al., 2018; Zheng et al., 2015). And if you have uterine polyps, you are also more likely to have adenomyosis as well (Indraccolo & Barbieri, 2011).
- Fibroids (Leiomyomas): Both endometriosis and fibroids have been found together in 12-26% of patients, although one small study found both in 86% of the patients studied (Huang et al., 2010; Nezhat et al., 2016; Uimara et al., 2011).
These can also lead to other problems such as pelvic floor dysfunction. Other conditions not necessarily associated with endometriosis can also cause chronic pelvic pain. These might include pelvic congestion syndrome, pudendal neuralgia, or occult hernias. This is why it is so important to identify other pain/symptom generators and treat those as well. If it all gets blamed on endometriosis, you may miss a key to finding relief.
References
Antero, M. F., O’Sullivan, D., Mandavilli, S., & Mullins, J. (2017). High prevalence of endometriosis in patients with histologically proven adenomyosis. Fertility and Sterility, 107(3), e46. Retrieved from https://doi.org/10.1016/j.fertnstert.2017.02.088
Butrick, C. W. (2007). Patients with chronic pelvic pain: endometriosis or interstitial cystitis/painful bladder syndrome?. JSLS: Journal of the Society of Laparoendoscopic Surgeons, 11(2), 182. Retrieved from https://europepmc.org/article/med/17761077
Chung, M. K., Chung, R. P., & Gordon, D. (2005). Interstitial cystitis and endometriosis in patients with chronic pelvic pain: the “evil twins” syndrome. JSLS: Journal of the Society of Laparoendoscopic Surgeons, 9(1), 25. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3015562/
Di Donato, N., Montanari, G., Benfenati, A., Leonardi, D., Bertoldo, V., Monti, G., … & Seracchioli, R. (2014). Prevalence of adenomyosis in women undergoing surgery for endometriosis. European Journal of Obstetrics & Gynecology and Reproductive Biology, 181, 289-293. Retrieved from https://doi.org/10.1016/j.ejogrb.2014.08.016
Huang, J. Q., Lathi, R. B., Lemyre, M., Rodriguez, H. E., Nezhat, C. H., & Nezhat, C. (2010). Coexistence of endometriosis in women with symptomatic leiomyomas. Fertility and sterility, 94(2), 720-723. Retrieved from https://www.fertstert.org/article/S0015-0282(09)00620-7/pdf
Indraccolo, U., & Barbieri, F. (2011). Relationship between adenomyosis and uterine polyps. European Journal of Obstetrics & Gynecology and Reproductive Biology, 157(2), 185-189. Retrieved from https://pubmed.ncbi.nlm.nih.gov/21470766/
Kunz, G., Beil, D., Huppert, P., Noe, M., Kissler, S., & Leyendecker, G. (2005). Adenomyosis in endometriosis—prevalence and impact on fertility. Evidence from magnetic resonance imaging. Human reproduction, 20(8), 2309-2316. Retrieved from https://doi.org/10.1093/humrep/dei021
Nezhat, C., Li, A., Abed, S., Balassiano, E., Soliemannjad, R., Nezhat, A., … & Nezhat, F. (2016). Strong association between endometriosis and symptomatic leiomyomas. JSLS: Journal of the Society of Laparoendoscopic Surgeons, 20(3). doi: 10.4293/JSLS.2016.00053
Uimari, O., Järvelä, I., & Ryynänen, M. (2011). Do symptomatic endometriosis and uterine fibroids appear together?. Journal of human reproductive sciences, 4(1), 34. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3136067/
Zhang, Y. N., Zhang, Y. S., Yu, Q., Guo, Z. Z., Ma, J. L., & Yan, L. (2018). Higher prevalence of endometrial polyps in infertile patients with endometriosis. Gynecologic and obstetric investigation, 83(6), 558-563. DOI:10.1159/000487946
Zheng, Q. M., Mao, H. L., Zhao, Y. J., Zhao, J., Wei, X., & Liu, P. S. (2015). Risk of endometrial polyps in women with endometriosis: a meta-analysis. Reproductive Biology and Endocrinology, 13(1), 1-9. Retrieved from https://doi.org/10.1186/s12958-015-0092-2

Thyroid disease and endometriosis
There are not many studies looking into the association of endometriosis and thyroid diseases. One study found that Graves disease (hyperthyroidism) was associated with endometriosis, but hypothyroidism was not (Yuk et al., 2016). Another study did not show any increase in prevalence in thyroid disorders among people with endometriosis (it was, in fact, less than the control group) (Petta et al., 2007). However, in another study that was looking into infertility, the researchers found that there was a higher prevalence of positive thyroid antibodies in those with endometriosis (Poppe et al., 2002). There are not enough high-quality studies to give strong evidence to a direct correlation between thyroid disorders and endometriosis. The incidence of endometriosis is estimated to be about 1 in 10 women, while the incidence of thyroid disorder is about 1 in 8 women (American Thyroid Association, n.d.). Thus, there may be significant overlap of the two.
However, endometriosis lesions may respond differently to circulating thyroid hormones. Just as endometriosis lesions have altered estrogen and progesterone receptors (see Role of Estrogen and Progesterone Resistance), endometriosis lesions may have altered thyroid metabolism (Petneau et al., 2019). This altered metabolism can lead to resistance to triiodothyronine (T3) action and local accumulation of thyroxine (T4), which could lead to proliferation of the endometriosis tissue (Peyeau et al., 2019). The study also mentions that “in humans, thyroid disorders are associated with more severe forms of endometriosis” as well as “increased chronic pelvic pain and disease score” (Peyneau et al., 2019). This study further demonstrates that endometriosis tissue has its own unique form and functionality.
References
American Thyroid Association. (n.d.). General Information/Press Room. Retrieved from https://www.thyroid.org/media-main/press-room/
Petta, C. A., Arruda, M. S., Zantut-Wittmann, D. E., & Benetti-Pinto, C. L. (2007). Thyroid autoimmunity and thyroid dysfunction in women with endometriosis. Human reproduction, 22(10), 2693-2697. Retrieved from https://doi.org/10.1093/humrep/dem267
Peyneau, M., Kavian, N., Chouzenoux, S., Nicco, C., Jeljeli, M., Toullec, L., … & Batteux, F. (2019). Role of thyroid dysimmunity and thyroid hormones in endometriosis. Proceedings of the National Academy of Sciences, 116(24), 11894-11899. Retrieved from https://www.pnas.org/content/116/24/11894.short
Poppe, K., Glinoer, D., Van Steirteghem, A., Tournaye, H., Devroey, P., Schiettecatte, J., & Velkeniers, B. (2002). Thyroid dysfunction and autoimmunity in infertile women. Thyroid, 12(11), 997-1001. Retrieved from https://doi.org/10.1089/105072502320908330
Shigesi, N., Kvaskoff, M., Kirtley, S., Feng, Q., Fang, H., Knight, J. C., … & Becker, C. M. (2019). The association between endometriosis and autoimmune diseases: a systematic review and meta-analysis. Human reproduction update, 25(4), 486-503. Retrieved from https://doi.org/10.1093/humupd/dmz014
Yuk, J. S., Park, E. J., Seo, Y. S., Kim, H. J., Kwon, S. Y., & Park, W. I. (2016). Graves disease is associated with endometriosis: a 3-year population-based cross-sectional study. Medicine, 95(10). Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4998884/

Is there an endometriosis Diet?
There is no one specific diet for endometriosis. No food, diet, or supplement will “cure” endometriosis, but it can help manage symptoms and is great for overall health and well-being. Your diet needs to be individualized to your specific needs, and it can take quite a bit of experimentation to find what works for you.
Some studies have found that a few things seem to help manage symptoms of endometriosis. Most of the strategies help to eliminate any food intolerances and influence inflammation and estrogen (Thomas & Natarajan, 2013). Some of the dietary strategies might include:
- Gluten free diet (Marziali et al., 2012)
- Low FODMAP diet (Moore et al., 2017)
- Anti-inflammatory diet (Leonardi et al., 2020)
- Fruits, vegetables (“preferably organic”), and whole grains (Ghonemy & El Sharkawy, 2017; Harris et al., 2018)
- Antioxidants, such as vitamins A, C, D, and E as well as B vitamins (Darling et al., 2013; Ghonemy & El Sharkawy, 2017; Huijs & Nap, 2020; Thomas & Natarajan, 2013) [Caveat- one study stated that vitamins from vitamin rich food and not supplements were noted with the difference (Darling et al., 2013)]
- Anti-inflammatories such as green tea, resveratrol, fish oil, healthy fatty acids (omega-3), N-acetylcysteine, quercitin, curcumin, parthenium, nicotinamide, 5‐methyltetrahydrofolate (Ghonemy & El Sharkawy, 2017; Huijs & Nap, 2020; Leonardi et al., 2020; Signorile, Viceconte, & Baldi, 2018)
- High fiber diet (Thomas & Natarajan, 2013)
- Rule out food intolerances and individualize your diet (Karlsson, Patel, & Premberg, 2020; Kronemyer, 2019; Leonardi et al., 2020)
- “Balanced diet with adequate vitamins and minerals, reduction of alcohol, sugar, and caffeine intake, exclusion of fructose or lactose intolerance” (Halis, Mechsner, & Ebert, 2010)
- The consumption of soy is controversial in endometriosis; however, Huijs & Nap (2020) note that “the amount of phytoestrogens present in soy is relatively low, making the effect of avoiding soy on suppressing endometriosis-related symptoms questionable”. They conclude that “there is insufficient evidence to advise women with endometriosis to avoid soy” (Huijs & Nap, 2020).
Karlsson, Patel, and Premberg (2020) summed it up best by stating that “participants experienced decreased symptoms and increased well-being after adopting an individually-adapted diet”; therefore, it may take some experimenting to find what works best for you as an individual.
*Interstitial cystitis is often called the “evil twin” of endometriosis and its symptoms can be greatly influenced by diet (see Interstitial Cystitis).
more topics:
Curcumin’s effect on endometriosis
Endometriosis Diet and Nutrition
Social gatherings and food choices
Links:
- “Endo Diet” from the Nutritionista
- Podcast on “Outsmart Endometriosis: The Elimination ‘Undiet’ for Endometriosis with Dr Jessica Drummond”
References
Darling, A. M., Chavarro, J. E., Malspeis, S., Harris, H. R., & Missmer, S. A. (2013). A prospective cohort study of Vitamins B, C, E, and multivitamin intake and endometriosis. Journal of Endometriosis and Pelvic Pain Disorders, 5(1), 17-26. Retrieved from https://journals.sagepub.com/doi/abs/10.5301/je.5000151
Ghonemy, G. E., & El Sharkawy, N. B. (2017). Impact of changing lifestyle on endometriosis related pain. IOSR Journal of Nursing and Health Science, 6(2), 120-129. DOI: 10.9790/1959-060205120129
Halis, G., Mechsner, S., & Ebert, A. D. (2010). The diagnosis and treatment of deep infiltrating endometriosis. Deutsches Ärzteblatt International, 107(25), 446. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2905889/
Harris, H. R., Eke, A. C., Chavarro, J. E., & Missmer, S. A. (2018). Fruit and vegetable consumption and risk of endometriosis. Human Reproduction, 33(4), 715-727. Retrieved from https://doi.org/10.1093/humrep/dey014
Huijs, E., & Nap, A. W. (2020). The effects of nutrients on symptoms in women with endometriosis: a systematic review. Reproductive BioMedicine Online. Retrieved from https://www.sciencedirect.com/science/article/abs/pii/S147264832030225X
Leonardi, M., Horne, A. W., Vincent, K., Sinclair, J., Sherman, K. A., Ciccia, D., … & Armour, M. (2020). Self-management strategies to consider to combat endometriosis symptoms during the COVID-19 pandemic. Human Reproduction Open, 2020(2), hoaa028. Retrieved from https://academic.oup.com/hropen/article/2020/2/hoaa028/5849477?login=true
Karlsson, J. V., Patel, H., & Premberg, A. (2020). Experiences of health after dietary changes in endometriosis: a qualitative interview study. BMJ open, 10(2), e032321. https://bmjopen.bmj.com/content/10/2/e032321.abstract
Kronemyer, B. (2019). Nutrient intake and gastrointestinal comorbidities with endometriosis. Contemporary OB/GYN, 64(10), 26-26. Retrieved from https://search.proquest.com/openview/1b532d099eb09103200be8ee1bae4f3c/1?pq-origsite=gscholar&cbl=48920
Marziali, M., Venza, M., Lazzaro, S., Lazzaro, A., Micossi, C., & Stolfi, V. M. (2012). Gluten-free diet: a new strategy for management of painful endometriosis related symptoms?. Minerva chirurgica, 67(6), 499-504. Retrieved from https://europepmc.org/article/med/23334113
Moore, J. S., Gibson, P. R., Perry, R. E., & Burgell, R. E. (2017). Endometriosis in patients with irritable bowel syndrome: specific symptomatic and demographic profile, and response to the low FODMAP diet. Australian and New Zealand Journal of Obstetrics and Gynaecology, 57(2), 201-205. Retrieved from https://obgyn.onlinelibrary.wiley.com/doi/abs/10.1111/ajo.12594
Signorile, P. G., Viceconte, R., & Baldi, A. (2018). Novel dietary supplement association reduces symptoms in endometriosis patients. Journal of cellular physiology, 233(8), 5920-5925. Retrieved from https://onlinelibrary.wiley.com/doi/abs/10.1002/jcp.26401
Thomas, D. S., & Natarajan, J. R. (2013). Diet–A New Approach To Treating Endometriosis–What Is The Evidence?. IOSR Journal of Nursing and Health Science, 1(5), 4-11. Retrieved from https://www.researchgate.net/publication/282006175_Diet-A_new_approach_to_treating_endometriosis-_What_is_the_evidence

