
Finding an endometriosis specialist
Endometriosis often requires specialized care. Just as there are specialists such as endocrinologists, oncologists, rheumatologists, cardiovascular surgeons, orthopedic surgeons, and so on, there are specialists for endometriosis. Even within those specialties, there are subspecialties for even more specific disease processes. However, finding those elusive providers can be difficult.
When looking for an endometriosis specialist, it is important for you to understand about the disease yourself- which is why this website is in existence. Start at the beginning and work your way through the site. It is equally important to educate yourself on common diseases that occur with endometriosis and can cause similar symptoms. Treating one disease process (endometriosis) and not treating another (such as interstitial cystitis) can leave you with symptoms and questions as to why.
When looking at a surgeon for endometriosis, we have some resources to help you. Start with this article about Choosing Your Surgeon. Join our Facebook group to find other resources on endometriosis. Take a look at vetted surgeons who have chosen to refine their skills on endometriosis and have subspecialties in endometriosis surgery (bowel, thoracic, etc.) (https://icarebetter.com/).
Endometriosis can cause a lot of problems with our health and healing takes time and effort. It can take addressing multiple pain generators and mental health care. Finding the right specialist/surgeon is an important first step on that journey towards better health.

7 Ways to Prepare For First Endometriosis Specialist Appointment
Table of contents
Diagnosis. Treatment. Surgery. Many Topics May Be Discussed At Your Visit
An endometriosis specialist appointment is not something you do every day (although sometimes it might feel like all day while you’re waiting there). However, the time you get to talk with the doctor may be pretty short. During that moment of consultation with the endometriosis (endo) specialist, you might feel brain fogged or bombarded. Whether it’s the diagnosis, treatment, surgery, pain management, or an endometriosis symptom you want to bring up, it’s easy to forget an essential topic while you’re there.
To make the most out of your initial endometriosis specialist appointment with an endometriosis specialist, we’ve made a list of seven ways you can prepare for the visit. First, we will give a short description of what endometriosis is.
What’s Endometriosis?
Endometriosis is a female medical disorder in which tissue similar to the endometrium (tissue that lines the walls of the uterus) grows outside the uterus. This endometriosis tissue can grow on the surface of the uterus, ovaries, intestines, fallopian tubes, bladder, or other organs in the body.
During menstruation, this tissue releases blood, and it sloughs off. However, this blood and tissue often remain trapped with no way to escape the body. This increased pressure can result in moderate to severe pain, among other symptoms. If you want to learn more about endometriosis and get a general background on the condition, read our article, “Endometriosis 101: Covering the Basics.”
Why You Are Here
People of various ages and demographics are subject to this often debilitating inflammatory pelvic disorder. Whether you have confirmed the diagnosis of endometriosis or if you need surgery to verify its presence and remove lesions – these suggestions can help you prepare for the endometriosis specialist appointment. There are many stages of endometriosis. Whether you’ve got into a specialist early on your journey or later, the important thing is that you are here now – exploring treatment options.
7 Ways to Prepare for Endometriosis Specialist Appointment
Once you have found an experienced endometriosis specialist, it’s essential to prepare yourself for the doctor’s appointment ahead of time. There is no concrete test to diagnose endometriosis (outside of surgery). Therefore, it’s imperative to have a solid understanding of the signs and symptoms of endo and detailed accounts of your own experience ready. Simple things such as medical records or journals that list all your endometriosis symptoms are a vital arsenal that will help you and your doctor determine your treatment plan.
1. Gather Your Records.
Unfortunately, most people with endometriosis have had many doctor appointments before seeing an endometriosis specialist. Therefore, you should have some medical records for them to review during your first appointment with an endo specialist. Gather everything from your regular medical history from your general practitioner to your OB/GYN records, testing, imaging, blood work, etc. Even if you think the particular doctor appointment or medical history is insignificant, you might be surprised by the various conditions linked to endometriosis. Bring it all. This information could play a vital role in your endometriosis treatment.
2. Keep a Journal of Endometriosis Symptoms/Pain.
Write down all the possible endo signs and symptoms you’ve had leading up to the doctor’s appointment. If you get a visit scheduled, and it’s a couple of weeks out, start the journal at that time, but also include the signs and symptoms you’ve experienced leading up to that point. Then, from that date until your appointment, write down all the different types of symptoms you experience. Include everything, even if you don’t think it’s relevant, like colds, headaches, stomach issues, shortness of breath, chest pain, etc. Also, be sure to include your emotions and feelings because endometriosis can significantly impact mental health and can lead to conditions such as depression and anxiety. Emotions and mental health are essential as you might want to include a counselor as part of your holistic endometriosis treatment team.
3. Bring This Printable Guide.
At endometriosis.org, they’ve created a convenient guide that can help you describe your symptoms and know what to ask your endometriosis specialist. Click here for the PDF. Please print it out and answer all the questions. Bring this with you to your doctor’s appointment to help specifically describe your endometriosis pain and other symptoms.
4. Take All Your Medications With You.
The importance of this cannot be understated. Even if you have a medication reconciliation (also known as a “med rec” for short) from your doctor, it’s important to realize those are not always up-to-date with everything you take. This inconsistency is especially true if you are on medications from multiple specialists or take supplements as well. The best way for your endo specialist to have a complete picture of all the medicines you are currently taking is by bringing them with you to the doctor’s appointment. You should include any supplements or over-the-counter medications. Bring in the physical bottles along with any medication history records.
5. Prepare Yourself Mentally.
Go into the appointment with the bold mindset that you will ask every single question you have to gain clarity on your endometriosis diagnosis and treatment options. Endometriosis is an aggressive inflammatory disorder that can have a devastating impact on your quality of life. It would help if you carried an even more aggressive attitude toward trying to stop it dead in its tracks.
6. Bring a List of Questions.
What’s been bothering you the most? Pain? Bowel symptoms? Bring a list of all the important questions that you want answers to. Writing them down will help you not forget during the appointment. Furthermore, when the doctor sees you have a list of questions you want answers to, it makes it harder for them to get up and walk out of the room like the appointment is over. If something like that has ever happened to you, we are sorry you’ve experienced this. That’s why it’s crucial to find a vetted endometriosis expert.
7. Take a Support Person With You.
Finding a good endo expert is no easy task (unless you use iCareBetter to connect you to one). If you are the type of person who is a bit shy or feels intimidated, you should bring your best support person to the appointment with you. Even if you are not nervous about your first endometriosis specialist appointment, having someone you trust by your side can help you process the information and encourage you along your journey. If no one you would like to accompany you, consider bringing a recorder and taping the visit. Because this can help you go back later and make sure you’ve understood all the information. Most doctors will have no qualms about recording your visit.
Endometriosis Care Process with iCareBetter
1- Find an expert based on keyword/ specialty or state
2- choose your doctor from the list
3- Get the contact info
4- First call and consultation.
5- Get info regarding costs and care process
6- Receive care
We Want to Hear From You
Have you been to an endometriosis specialist (OB-GYN experienced in endo)? If so, is there anything you wished you would have done differently? If you’ve not been to an endo specialist yet, what is your biggest concern about the first doctor visit?

Endometriosis Myths & Facts: Dispelling the Misconceptions
Table of contents
- Debunking the Myths About Endometriosis & Exploring the Facts
- Overview of Endometriosis
- Why is it Difficult to Diagnose Endometriosis?
- Myth #1: Severe Period Pain is Normal
- Myth #2: A Hysterectomy Cures Endometriosis
- Myth #3: Endometriosis Only Affects the Pelvic Area
- Myth #4: Endometriosis Symptoms are Simply a “Heavy Period”
- Myth #5: Douching Causes Endometriosis
- Myth #6: Having an Abortion Can Cause Endometriosis
- Myth #7: You’re Too Young to Have Endometriosis
- Myth #8: Endometriosis Can Be Prevented
- Myth #9: Endometriosis is Always Painful
- Myth #10: Pregnancy is a Cure for Endometriosis
- Myth #11: Menopause Cures Endometriosis
- Myth #12: Hormonal Therapy Cures Endometriosis
- Myth #13: Endometriosis is Cancer
- Myth #14: Tubal Endometriosis Always Causes Infertility
- Myth #15: Endometriosis Symptoms Are the Results of Emotional Distress (It Is All in Your Head)
- We Want Your Input
Debunking the Myths About Endometriosis & Exploring the Facts
One in ten women worldwide is affected by endometriosis, also known as “endo,” for short. While this number is an estimate, the actual figures may be higher. Not only is the person with this inflammatory disorder affected, so are the family members and people around her due to the often debilitating effects of this disease. Endometriosis facts are important because it is complex and often misunderstood even though it’s a common disorder. Because of this, there are many myths and misconceptions regarding endometriosis prognosis, treatment, causes, symptoms, diagnosis, complications, etc.
Focusing on the disease itself often ignores the vicious cycles of stress, fatigue, pain, doctor visits, flare-ups, and loss of productivity experienced by the patient. These factors can lead to a decreased quality of life. Worse is that endometriosis facts come behind outdated treatment options, myths, and misconceptions about this disorder. It takes an average of eight to ten years for a patient to be diagnosed with endometriosis. One of the biggest problems with the misconceptions about endo is that they can prevent women from seeking treatment. Keep reading as we review endometriosis facts and debunk the myths.
Overview of Endometriosis
Endometriosis is a pelvic disorder characterized by endometriosis tissue similar but not the same as the tissue inside the uterus, growing elsewhere. Typically, the growth occurs outside the uterus, ovaries, fallopian tubes, cervix, the surface of the bladder, bowel, and distant organs.
Endometriosis growths can cause pain, scarring, and sometimes infertility. Pain from endometriosis is usually the result of menstrual bleeding from the tissues. Unlike the endometrium inside your uterus, blood that comes from endo tissue outside this organ has no means of escaping the body. This blood causes increased pressure and inflammation, which can result in pain that’s often debilitating. If you would like to learn more information about endometriosis, please read our introduction article, “Endometriosis 101: Covering the Basics.”
Why is it Difficult to Diagnose Endometriosis?
Studies show that it can take an average of seven years or more for a woman to get an endometriosis diagnosis. Why is this? Endometriosis signs and symptoms are often similar to other conditions, such as irritable bowel syndrome or pelvic inflammatory disease (PID). Therefore, it’s often mistaken for another illness. Furthermore, the myths and misconceptions we discuss below also prevent a lot of women from seeking help. For this reason, it’s crucial to get the endometriosis facts clear. Keep reading as we debunk the myths and state the facts.
Myth #1: Severe Period Pain is Normal
Nineteenth-century doctors were often perplexed by “women’s problems.” As a result, women were often discounted as being unstable mentally. While the attitudes and thoughts have improved since, some of those old beliefs persist, including those regarding period pain.
Many patients with endometriosis hear that their severe period pain is “normal.” Pain and cramping are normal during menstruation. However, the pain should not be so intense that it interferes with functioning or impacts the quality of life. If your period pain is so severe that you cannot carry out daily activities, you should seek an endometriosis expert.
Myth #2: A Hysterectomy Cures Endometriosis
Endometriosis growths are tissues “similar” to those inside of the uterus. It is not the same tissue. Simply removing the uterus and/or ovaries without excising any endometriotic implants growing outside the uterus will not cure it.
Myth #3: Endometriosis Only Affects the Pelvic Area
Locations within the pelvis, such as the surface of the uterus, bladder, or fallopian tubes, are the most common locations where endometriosis growths occur. However, endo can occur elsewhere in the body. In some cases, endometriosis growths have been present in distant organs, such as the lungs.
Myth #4: Endometriosis Symptoms are Simply a “Heavy Period”
Bleeding during menstruation can be heavy at times. However, it should not exceed the saturation of a pad or tampon in one hour. If you experience that degree of bleeding, you should bring this up with your healthcare provider. The fact is that many women with endometriosis experience abnormally heavy flow due to the excess tissue.
Myth #5: Douching Causes Endometriosis
No scientific evidence links douching with the development of endometriosis.
Myth #6: Having an Abortion Can Cause Endometriosis
No scientific evidence demonstrates that having an abortion causes endometriosis. Those who claim otherwise might be confusing endometritis and endometriosis.
Myth #7: You’re Too Young to Have Endometriosis
A common misconception is that endometriosis is rare or doesn’t occur in young women and teenagers. As a result, many doctors do not consider an endometriosis diagnosis in young women with typical symptoms. Endometriosis facts demonstrate that teenagers and women in their early 20s can have the disorder. Most people with endometriosis state they experienced endo symptoms during adolescence.
Myth #8: Endometriosis Can Be Prevented
It’s not clearly understood what causes endometriosis. Therefore, there are no proven ways to prevent this inflammatory condition. Anything else is purely speculation at this point.
Myth #9: Endometriosis is Always Painful
Not all women with endometriosis experience pain. Studies show that some women with advanced stages of endometriosis do not experience pain as a symptom.
Myth #10: Pregnancy is a Cure for Endometriosis
This misconception about endometriosis is slowly beginning to fade. However, not quickly enough! Pregnancy fluctuates hormones in the female body, which can temporarily suppress some symptoms of endometriosis. However, these symptoms usually recur for most patients following the pregnancy. Therefore, it’s not a cure.
Myth #11: Menopause Cures Endometriosis
Endometriosis symptoms often occur during menstruation, but many women experience them long after periods stop. Following menopause, the body still produces small amounts of hormones, and the endometriosis tissue still responds to them, thus causing pain. For many women, the symptoms of endometriosis may improve after menopause, but that does not mean it’s a cure. Depending on the case, it might be necessary to remove endometriosis implants or adhesions even after menopause.
Myth #12: Hormonal Therapy Cures Endometriosis
Doctors have been treating endometriosis for years using hormonal therapy drugs. However, these medications do not have long-term effects on the disease itself. Hormones can help relieve the symptoms temporarily and even shrink the growths, but they do not cure endometriosis.
Myth #13: Endometriosis is Cancer
Endometriosis growths are not cancerous. To date, there is little evidence that shows endometriosis directly causes cancer. However, some types of cancers are more common in women who have endometriosis. Endometrial cancer is also known as uterine cancer. Many studies have examined the relationship between the two, and one showed that merely 0.7 percent of patients with endometriosis had endometrial cancer at the 10-year follow-up. Therefore, endometriosis does not equal cancer, but it may increase the risk of cancer.
Myth #14: Tubal Endometriosis Always Causes Infertility
Tubal endometriosis is not very common, and it does not always cause infertility. Does endometriosis cause infertility? It can be in many cases, but the mechanisms of infertility in endometriosis remain multifactorial. Can you get pregnant with endometriosis? It is possible, and many women do – especially with proper treatment early on.
Myth #15: Endometriosis Symptoms Are the Results of Emotional Distress (It Is All in Your Head)
Yes. People have heard many times that emotional distress could be the cause of their endometriosis and pain. This statement is false. The fact is, endometriosis is a highly complex disorder with many underpinnings. Those with endometriosis often experience emotional distress as an impact of the symptoms such as pain and infertility. But emotional distress it’s not the cause of endometriosis symptoms.
Endometriosis quick facts:
1- There is no blood test available for the diagnosis of endometriosis.
Mehedintu C, J Med Life, 2014
2- The diagnosis of endometriosis starts by taking a good history from patients, and performing a detailed physical exam including pelvic exam. In some cases, a doctor might ask for MRI and Ultrasound to have a more thorough picture. But the ultimate diagnosis is only possible with laparoscopic /robotic surgery and taking a biopsy for histopathology. There is no blood test that can tell if you have endometriosis.
3- Studies show that those with endometriosis have an increased risk of developing depression and anxiety disorders.
Chen LC, et al, J Affect Disord, 2016
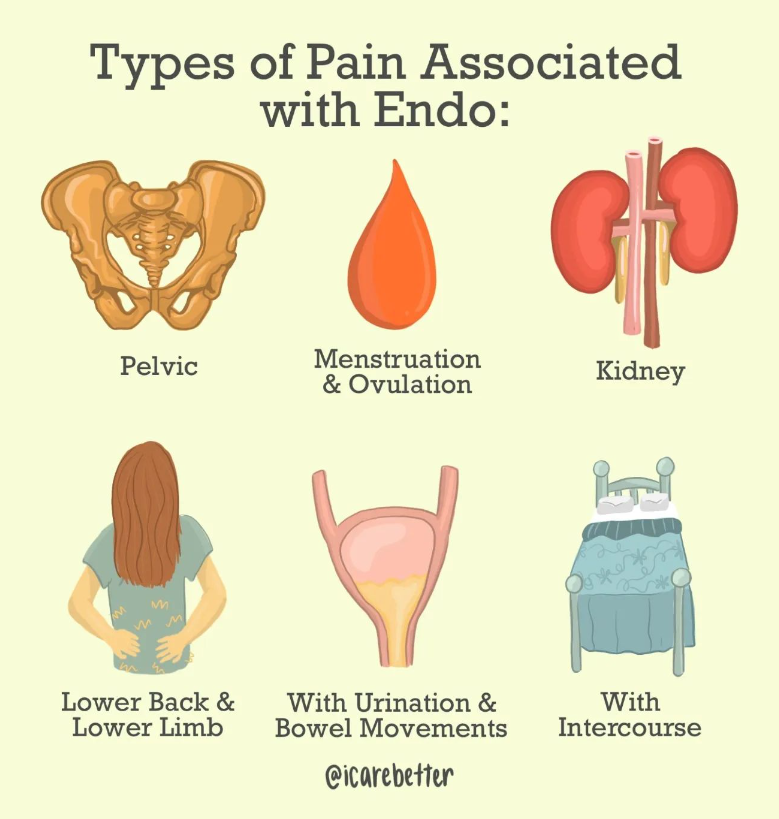
4- Pelvic pain due to endo occurs a day part of an inflammatory cycle which can affect the pelvic organs and functions such as sitting, sex, bowel movements and even urination. Pelvic floor physical therapy can help with restoring balance to the pelvic floor muscles.
Dr. Juan Michelle Martin, Endometriosis Physical Therapist.
5- “The most common clinical signs of endometriosis are menstrual irregularities, chronic pelvic pain, dysmenorrhea (painful periods), dyspareunia (painful sex), and infertility.”
Lagana AS, et al, Int J Womens Health. 2017
We Want Your Input
Are there any endometriosis myths or misconceptions we did not list here? Let us know in the comments below!

Pelvic Congestion Syndrome- another cause of chronic pelvic pain
When talking about endometriosis and chronic pelvic pain, it is important to remember that often endometriosis is not the only pelvic pain generator. Another possible contributor to chronic pelvic pain is pelvic congestion syndrome (PCS). PCS is like having varicose veins in the pelvis. Blood pulls in the veins and can cause symptoms such as heaviness, pain with penetration, noncyclical pain, positional lower back pain, pelvic and upper thigh pain, prolonged postcoital discomfort, symptoms that worsen throughout the day and are exacerbated by activity or prolonged standing, and non-specific lower abdominal and pelvic pain (Durham & Machan, 2013; Mistry & le Roux, 2017). LIANG and Brown (2021) report that:
“Typical pelvic congestion syndrome pain is:
– Heaviness and dull aching in nature
– Located deep in the pelvis and on the left
– Exacerbated by upright position (standing or sitting) and exercise (walking, running, weightlifting)
– Worse towards the end of the day
– Worse after sexual intercourse
– Worse when bladder is full
– Chronic and insidious onset
Atypical pelvic congestion syndrome pain is:
– Constant pain not related to time of day, upright posture or physical activities
– Pain worse premenstrually and during menstrual periods
– More on the right than the left
– Acute and sudden onset
– Sharp or colicky in nature”
While the gold standard for diagnosis is contrast venogram, this procedure is usually done as part of the treatment (embolization procedure) (LIANG & Brown, 2021). LIANG and Brown (2021) report that “all non-invasive imaging like ultrasound, CT and MRI can detect pelvic varicosities” but that the key is “to alert the imaging technicians and specialist to look out for pelvic varicosities and to report them” (LIANG & Brown, 2021). A CT scan can also help diagnose other syndromes such as Nutcracker Syndrome (left renal vein compression) and May-Thurner Syndrome (left iliac vein compression) (LIANG & Brown, 2021). If you’ve had surgeries before for endometriosis and wonder why it wasn’t seen during surgery, it is because surgery “is performed with the patient in supine or Trendelenburg position, and with the use of CO2 for abdominal distention” thus meaning that the “veins are often collapsed, and pelvic varicosities can be missed”- it would take the surgeon who suspects pelvic varicosities to put the patient in “reverse Trendelenburg position and easing off CO2 distention” that “might allow the dilated veins to fill” and possibly be seen (LIANG & Brown, 2021).
Unfortunately, PCS doesn’t just go away or improve with time, therefore, treatment is usually needed for those who are symptomatic (LIANG & Brown, 2021). Because there is pooling and back flow of blood in the veins, the treatment suggested is transcatheter embolization (LIANG & Brown, 2021). Medication, hysterectomy, and other treatments have not proved as effective (LIANG & Brown, 2021). The transcatheter embolization “is performed with conscious sedation under local anaesthetic, as a day procedure” and “is one of the safest embolisation procedures” (LIANG & Brown, 2021). LIANG and Brown (2021) report that “some feel the relief of pelvic congestion syndrome symptoms soon after embolisation, while others might have to wait for the thrombophlebitis to settle before appreciating the result”- reporting that it is best to wait 4-6 weeks to better judge the effectiveness. Mistry & le Roux (2017) report that after looking at 20 studies that “the overall technical success rate was as high as 99%” and that “with a mean follow up of 15 months, 80% of the patients reported benefit from the procedure while 13% experienced little or no relief of the symptoms”.
PCS may be another piece in the puzzle of ongoing chronic pelvic pain.
References
Durham, J. D., & Machan, L. (2013, December). Pelvic congestion syndrome. In Seminars in interventional radiology (Vol. 30, No. 04, pp. 372-380). Thieme Medical Publishers. Retrieved from https://www.thieme-connect.com/products/ejournals/html/10.1055/s-0033-1359731
LIANG, D. E., & Brown, B. (2021). Pelvic congestion syndrome: Are we missing the diagnosis?. The Medical Republic. Retrieved from https://www.sydneyfibroidclinic.com.au/app/uploads/2021/06/PCS-Medical-Republic.pdf
Mistry, P. P., & le Roux, D. A. (2017). Pelvic congestion syndrome (PCS). Practice Perspectives for Venous Disorders, 46. Retrieved from http://www.vascularsociety.co.za/wp-content/uploads/2019/02/VASSA-venous-guidelines-Practice-perspectives-for-venous-disorders-2017.pdf#page=46

A Multidisciplinary Team for Endometriosis is Key to Positive Outcomes
Table of contents
- Why Your Endometriosis Treatment Plan Should be Multidisciplinary
- What is Endometriosis?
- What is a Multidisciplinary Team Approach in Medicine?
- Benefits of a Multidisciplinary Treatment (MDT) Team for Endometriosis
- Who comprises an Endometriosis Multidisciplinary Team?
- Psychiatrist/Psychologist:
- Building Your Multidisciplinary Team for Endometriosis
Why Your Endometriosis Treatment Plan Should be Multidisciplinary
Endometriosis (endo) is a chronic and progressive disorder characterized by the growth of endometriosis tissue outside the uterus. This disorder often affects various organs in the body and results in pain and other issues. In addition to the intense physical and often debilitating symptoms of the disease, it can also take a toll on mental and spiritual health. Therefore, a multidisciplinary team (MDT) approach to endometriosis pain, surgery, and disease management leads to the best outcomes for patients. Keep reading to learn how.
What is Endometriosis?
Pronounced (en-doe-me-tree-O-sis), endometriosis is a chronic inflammatory disorder in which a type of tissue that is similar to the endometrial tissue that normally grows inside the uterus, grows outside this organ. Sometimes, the endometriosis tissue appears on the outer side of the uterus. These lesions can also grow on the ovaries, fallopian tubes, bladder wall, and on the outside of other organs within the pelvic cavity and other regions of the body.
Endometriosis is often a very painful and debilitating disease. During menstruation, these endometriosis growths shed blood into the body which is not able to be released. This causes an increase in pressure throughout the pelvic and sometimes abdominal region. Endo often involves other organs such as the bowels, ovaries, fallopian tubes, vagina, and cervix. In rare cases, it may affect other organs, such as the bladder, lungs, diaphragm, or kidneys. If you would like to learn more information about endometriosis, read our article, “Endometriosis 101: Covering the Basics”.
What is a Multidisciplinary Team Approach in Medicine?
Multidisciplinary care is when multiple members of the healthcare team come together to collaborate to provide optimal care for a patient. When it comes to endometriosis treatment, it’s important to involve various disciplines across the healthcare spectrum to achieve the best possible outcomes for patients.
Benefits of a Multidisciplinary Treatment (MDT) Team for Endometriosis
Draw in endo experts across different care areas to enhance the patient’s prospects and outcomes. Physicians benefit from this approach as they are able to provide a better framework for decision-making on a collaborative level and implementation. These aspects are particularly important when dealing with complex endometriosis cases. When several endo experts work together in unison, the benefits include cross-discipline learning, research, and review.
There is a type of disease, called deep infiltrating endometriosis (DIE). Alarmingly, about 20 percent of endo patients have this type. With DIE, the lesions can penetrate 5 mm deep into the organs affected by the disorder. A multidisciplinary treatment plan is the best approach for better outcomes and improved quality of life for the patient. The resection of DIE lesions requires a surgeon with expertise in endometriosis and a multidisciplinary approach coordinated by the endo specialist.
In fact, in 2019, the Society for Women’s Health Research assembled a team of clinicians, researchers, and patients to deliberate on the barriers in the commonly accepted forms of endometriosis treatment and management. The team underscored the importance of comprehensive and interdisciplinary approaches to disease and pain management for proper treatment and diagnosis.
Who comprises an Endometriosis Multidisciplinary Team?
The following are some of the endometriosis experts that come together and help treat patients holistically:
Endometriosis Surgeon (Gynecologist):
If you have endometriosis, a regular obstetrics-gynecological surgeon is not going to suffice. It’s important to have an endometriosis specialist, who is an OB surgeon with experience in the treatment of this pelvic disease. An endometriosis laparoscopy is often needed to diagnose and treat the disease. It’s important to choose a surgeon familiar with endo to ensure all lesions are removed. Learn more about endometriosis specialists and how to find a vetted physician in our article here.
Colorectal Surgeon (Bowel Surgeon):
If the endometriosis affects the bowel, surgical excision may be necessary to remove the lesions. Surgical treatment, such as full-thickness disc excision or a bowel resection should only be performed by an experienced colorectal surgeon. This physician will participate in the care from the diagnostic workup to surgical treatment and follow-up care.
Urologist (Genitourinary Tract Doctor):
A urologist treats disorders of the urethra, kidneys, urinary bladder, and adrenal glands. Having an experienced urologist as part of your multidisciplinary team can help aid in the treatment of ureter and bladder lesions as well as minimize kidney or bladder complications.
Radiologist Experienced in Endometriosis:
Endometriosis may have several presentations, which can make diagnostic testing challenging. Because endometriosis lesions can present in other areas of the body away from the reproductive organs, it’s important that the radiologist on your team is familiar with the pelvic nerve anatomy and how to detect signs of neural endometriosis.
Physical Therapist/Pelvic Floor Therapist:
Physical therapy can be very important in the treatment of endometriosis. While some patients may require physical therapy to help them adapt to pain and stay mobile, others may need highly specific pelvic floor therapy. A pelvic floor physical therapist can work with the patient to help reduce adhesions and scar tissue which can limit pelvic floor extensibility. These exercises are important to help reduce pain sometimes associated with intercourse or the insertion of a tampon.
Pain Management Doctor:
Endometriosis pain is often the primary complaint and most debilitating symptom of this disease. In fact, it’s not uncommon for the pain associated with endo to become so intense that a person is no longer able to function in daily life. For this reason, a pain management doctor should be a part of the team to improve functioning and overall quality of life.
Psychiatrist/Psychologist:
Anxiety and depression are two of the biggest mental health disorders that often accompany endometriosis. Furthermore, the pain and sometimes infertility that come with this disorder can further aggravate these negative emotions. Therefore, a holistic MDT for endometriosis will include a psychiatrist or psychologist, possibly one who specializes in pain management.
Nutritionist:
Nutrition plays a key role in the processes and regulation of your digestive and immune systems. A proper endometriosis diet can help to reduce the chronic inflammation that keeps the endometriosis lesions growing and spreading. A nutritionist with experience in treating endo patients is key for successful outcomes.
Pathologist:
There are different stages and types of endometriosis. Endometriosis with architectural atypia is one type that may be a precursor of ovarian cancer. Therefore, it’s important that a pathologist carefully examines the lesions to discover if they could be indicative of endometriosis-associated ovarian cancer.
Building Your Multidisciplinary Team for Endometriosis
Who’s got your back? If you have or suspect you might have endometriosis, this is a very important question to ask yourself. iCareBetter is a digital platform that connects endo patients to vetted endometriosis experts across a variety of disciplines. If you have endo, we want to hear from you. Do you already have an MDT for endo? If so, who are the members of your personal team?

How Do I Know If I Have Endometriosis? Endometriosis Signs
Table of contents
Learn Endometriosis Signs & Symptoms & What to Tell Your Doctor
Pelvic pain is common for most women during their period. However, for some – this time of the month comes with excruciating pain due to the medical condition – endometriosis (also known as endo for short). Believe it or not, endometriosis signs extend beyond just the debilitating pain, although, that’s the hallmark symptom of this inflammatory disorder.
If you think you might have endometriosis, it’s important to have a solid foundation of information before you see your doctor for a possible endo diagnosis. Keep reading to learn what endometriosis is and what are the most common signs and symptoms of this condition.
What Is Endometriosis?
Pronounced (en-doe-me-tree-O-sis), endometriosis is a chronic inflammatory disorder of the pelvis where tissue similar to that normally grows inside your uterus, grows elsewhere instead, usually on the outside of it. The endometriosis tissue can block fallopian tubes, cover your ovaries, and even line the organs of your pelvis.
Endometriosis can cause intense pain and fatigue, which makes it a disabling inflammatory condition for many women. Pain from endometriosis can be so intense that sometimes even medication cannot touch it. Other organs commonly involved include the fallopian tubes, bowels, cervix, ovaries, vagina, and pelvic tissue. Rarely, endo may also affect distant organs. Learn more about the disorder in our previous article, “Endometriosis 101: Covering the Basics”.
What Are Endometriosis Signs and Symptoms?
Sadly, endometriosis is an inflammatory disorder that often goes undiagnosed for years because the hallmark symptoms are things that some women take for granted as “normal”: heavy bleeding and pain during periods. If you think you might have endometriosis, it’s important that you know what to look for and when you should notify a doctor. The following are seven common signs of endometriosis:
Dysmenorrhea (Painful Periods):
Intense pelvic or abdominal pain is one of the most common symptoms of endometriosis. Endometriosis pain is often described as a sharp or stabbing sensation. During menstruation, women with endo may experience very painful periods because the endometrial tissue swells and bleeds every month, just like the uterine lining would. However, because this process is occurring outside the uterus, blood is not easily shed, and this pressure can cause extreme cramping that is much more intense than typical period cramps. Period pain should not disrupt your daily life, so if it does, you need to let your doctor know or find a qualified endo specialist.
Menorrhagia (Heavy Menstrual Bleeding):
While many women bleed heavily during their period, endometriosis can cause significant blood loss. How do you know if your amount of bleeding is excessive? Watch for these signs:
- Passing large clots
- Period goes on longer than a week
- Bleeding through a pad or tampon in an hour
- Too fatigued to carry out daily activities
If you have these symptoms, you may have menorrhagia and should contact a gynecologist. Menorrhagia is sometimes caused by endometriosis, and it can cause anemia and severe fatigue.
Dyspareunia (Pain During or After Intercourse):
When endometriosis is the cause of painful intercourse, the woman may not experience the pain upon entry, only upon deep penetration. There can be physical and psychological causes of this condition, and endometriosis may be the culprit, as tissue builds up on the other side of the lower uterus or vagina – and sexual intercourse can stretch the tissue. You should talk to an experienced physician if you have pain during or after intercourse.
Chronic Pelvic Pain:
While the inflammatory condition usually involves pain during menstruation, endometriosis pain can occur at any time of the month. Endometriosis causes an increase in pressure due to the excessive tissue in the pelvic cavity. This can cause a chronic pain condition that might be felt exclusively in the pelvis or manifest as abdominal or back pain.
Ovarian Cysts:
There is a type of endometriosis that causes endometriomas (also known as chocolate cysts) to grow on your ovaries. These cysts are non-cancerous but may become large and painful. Also, women who have these may also have other endometrial growths in the abdominal or pelvic areas.
Infertility:
Up to about half of women who have problems with fertility also have endometriosis. Furthermore, up to 50 percent of women who have endometriosis are unable to get or stay pregnant. The relationship between these conditions isn’t always clear as many factors can impact fertility. However, in the event that the endometriosis tissue blocks the reproductive organs, there is a clear connection. Treating the condition can increase your odds of having a baby. If these fertility issues are affecting you, contact an endometriosis specialist.
Bowel/Bladder Problems:
Bathroom visits may be problematic if you have endometriosis lesions growing near your bladder or bowels. And if you are experiencing difficulty with urination or bowel movements or bleeding in the bowel – these may be signs of endometriosis. Also, if you have painful urination, blood in your stool, nausea, or hyper urgency to urinate – you should tell your medical provider immediately.
When to Call Your Healthcare Provider
Share with your healthcare provider any of the following endometriosis signs and symptoms:
- Pain. Pain is the most common sign of endometriosis, and it can be present:
- During or after sex
- With bowel movements
- When urinating during your period
- As chronic abdominal, lower back, or intestinal pain
- Similar to menstrual cramps that get worse gradually
- Bleeding or spotting between periods
- Difficulty getting pregnant or infertility
- Digestive issues or stomach problems such as diarrhea, constipation, bloating, or nausea—especially during your periods

Genes associated with endometriosis
It’s an exciting title: “Genetic cause of endometriosis discovered, pointing to new drug therapy” (Haridy, 2021). But it is misleading. When you look further, it reveals it is referencing a study (Tapmeier et al., 2020) that identified “a novel genetic variant that is associated with severe cases of endometriosis” (Haridy, 2021). The article further states that “NPSR1 mutations have never before been linked with endometriosis” but “they have, however, been associated with inflammatory diseases including arthritis, inflammatory bowel disease and asthma” (Haridy, 2021). This gene was noted in endometriosis patients in a 2016 study that identified several genes associated with endometriosis (Houshdaran et al., 2016). The article also notes “not every woman with endometriosis was found to have this particular NPSR1 variant, affirming the heterogenous nature of the condition” and that the gene has a “potential role in endometriosis” that “points to the development of anti-inflammatory therapeutics targeting this mechanism” (Haridy, 2021).
We know there is a genetic component to endometriosis; however, a single gene has not been identified as the cause. This study notes that this particular gene is associated with stage III/IV endometriosis and with other inflammatory conditions. The research is identifying new potential drug targets to help with symptoms.
Genetics account for about 50% of the risk for endometriosis with the other 50% “likely owing to environmental factors” (Montgomery et al., 2020). “As with other complex diseases, genetic variants in the DNA sequence increasing endometriosis risk all have small effects, unlike most single-gene disorders” and “it is the combinations of these variants adding together that contribute to higher risks for individual women” (Montgomery et al., 2020). The science of epigenetics should also be considered.
Epigenetics is “the study of biological mechanisms that will switch genes on and off” (What Is Epigenetics, 2019). Epigenetics can be influenced by almost everything: “what you eat, where you live, who you interact with, when you sleep, how you exercise, even aging – all of these can eventually cause chemical modifications around the genes that will turn those genes on or off over time” (What Is Epigenetics, 2019). Epigenetics involved with endometriosis might include “DNA methylation and histone modification, and, other non-classic mechanisms: miRNAs and lncRNA” (Chen et al., 2020). “Increased estrogen activity and progesterone resistance are the main hormonal substrate of this disease and are associated with inflammatory response and debilitating symptoms, including pain and infertility….The regulation of receptor expression by epigenetics maybe a critical factor for endometriosis” (Chen et al., 2020).
In short, endometriosis is pretty complicated and we still have much to learn.
References
Chen, H., Malentacchi, F., Fambrini, M., Harrath, A. H., Huang, H., & Petraglia, F. (2020). Epigenetics of estrogen and progesterone receptors in endometriosis. Reproductive Sciences, 1-8. Retrieved from https://link.springer.com/article/10.1007/s43032-020-00226-2
Haridy, R. (2021). Genetic cause of endometriosis discovered, pointing to new drug therapy. Retrieved from https://newatlas.com/science/genetic-cause-endometriosis-inflammation-new-drug-therapy/
Houshdaran, S., Nezhat, C. R., Vo, K. C., Zelenko, Z., Irwin, J. C., & Giudice, L. C. (2016). Aberrant endometrial DNA methylome and associated gene expression in women with endometriosis. Biology of reproduction, 95(5), 93-1. Retrieved from https://doi.org/10.1095/biolreprod.116.140434
Montgomery, G. W., Mortlock, S., & Giudice, L. C. (2020). Should genetics now be considered the pre-eminent etiologic factor in endometriosis?. Journal of minimally invasive gynecology, 27(2), 280-286. Retrieved from https://doi.org/10.1016/j.jmig.2019.10.020
Tapmeier, T. T., Rahmioglu, N., Lin, J., Obendorf, M., de Leo, B., Montgomery, G., … & Zondervan, K. T. (2020). Neuropeptide S Receptor 1 is a Novel Non-Hormonal Treatment Target in Endometriosis. Reproductive Sciences, 27(SUPPL 1), 130A-130A. Retrieved from https://stm.sciencemag.org/content/13/608/eabd6469
What Is Epigenetics. (2019). A Super Brief and Basic Explanation of Epigenetics for Total Beginners. Retrieved from https://www.whatisepigenetics.com/what-is-epigenetics/

Endometriosis Doctor For Diagnosis, Treatment, & Surgery

What a Pain! Vaginismus, Vulvodynia, and More
Endometriosis can have a cascade effect on the muscles, fascia, and nerves of the pelvis. Myofascial pain is involved in up to 94% of chronic pelvic pain and can occur “independently or in conjunction with disorders such as vaginismus, dysmenorrhea, and endometriosis and is frequently a causative factor in sexual pain or dyspareunia” (Ross et al., 2021). Vaginismus, vulvodynia, and pudendal neuralgia are a few of things that can contribute to chronic pelvic pain.
Vaginismus is the “recurrent involuntary tightening of muscles around the vagina” (spasms) whenever penetration is attempted- such as “the use of tampons, penetrative intercourse, cervical examinations, and other activities” (Haire, 2021). Phenomena such as endometriosis, recurrent bladder infections (or painful bladder syndrome), yeast infections, hormonal changes (such as decreased lubrication with menopause) are a few of the things that might trigger it (HealthDirect, 2019). Therapies might include pelvic floor physiotherapy, local anesthetics (such as lidocaine), muscle relaxants (such as medications/creams or even botulinum toxin injections), and/or anxiolytic medication (Lahaie et al., 2010).
Vulvodynia is “chronic discomfort in the vulvar region” (Reed, 2006). The pain has been “described as ‘burning,’ but it may be irritating, sharp, prickly, or, occasionally, pruritic, and it can be mild to severe” (Reed, 2006) (pruritic meaning itching). Reed (2006) also reports that “the pain can begin suddenly when provoked, and it tends to dissipate gradually; women with vulvodynia often report hours to days of discomfort after intercourse or a pelvic examination.” The pain with vulvodynia can be exacerbated by prolonged sitting, tight clothes, riding a bike, use of tampons, or intercourse (Reed, 2006). Vulvodynia might be contributed to by “injury to, or irritation of, the nerves that transmit pain from the vulva to the spinal cord, an increase in the number and sensitivity of pain-sensing nerve fibers in the vulva, elevated levels of inflammatory substances in the vulva, an abnormal response of different types of vulvar cells to environmental factors such as infection or trauma, genetic susceptibility to chronic vestibular inflammation, chronic widespread pain and/or inability to combat infection, or pelvic floor muscle weakness, spasm or instability” (National Vulvodynia Association, n.d.). The National Vulvodynia Association has good information on treatment options here: https://www.nva.org/what-is-vulvodynia/treatment/.
Another entity associated with pain in the pelvic region is pudendal neuralgia. This is “a painful condition caused by inflammation, compression or entrapment of the pudendal nerve; it may be related to or be secondary to childbirth, pelvic surgery, intense cycling, sacroiliac skeletal abnormalities or age-related changes” (Perez-Lopez & Hita-Contreras, 2014). Symptoms usually present with “pelvic pain with sitting which increases throughout the day and decreases with standing or lying down, sexual dysfunction and difficulty with urination and/or defecation” (Perez-Lopez & Hita-Contreras, 2014). Treatment options might include “physiotherapy, analgesics and nerve block, surgical pudendal nerve decompression, radiofrequency and spinal cord stimulation” (Perez-Lopez & Hita-Contreras, 2014).
The pelvic floor is a busy highway of muscles, nerves, ligaments, blood vessels (see Pelvic Congestion Syndrome), and more. There is a lot that can contribute to chronic pelvic pain, and it is important to address all the factors that might be contributing to it. You can find more information here:
- https://icarebetter.com/pudendal-neuralgia-vulvodynia/
- https://icarebetter.com/pelvic-floor-dysfunction
References
Haire, G. (2021). When the Body Says No: The Experience of Vaginismus and the Validity of Female Pain. Brief Encounters. Retrieved from https://kar.kent.ac.uk/89429/1/document.pdf
HealthDirect. (2019). Vaginismus. Retrieved from https://www.healthdirect.gov.au/vaginismus
Lahaie, M. A., Boyer, S. C., Amsel, R., Khalifé, S., & Binik, Y. M. (2010). Vaginismus: a review of the literature on the classification/diagnosis, etiology and treatment. Women’s Health, 6(5), 705-719. Retrieved from https://journals.sagepub.com/doi/full/10.2217/WHE.10.46
Perez-Lopez, F. R., & Hita-Contreras, F. (2014). Management of pudendal neuralgia. Climacteric, 17(6), 654-656. Retrieved from https://doi.org/10.3109/13697137.2014.912263
National Vulvodynia Association. (n.d.). Retrieved from https://www.nva.org/
Reed, B. D. (2006). Vulvodynia: diagnosis and management. American family physician, 73(7), 1231-1238. Retrieved from https://www.aafp.org/afp/2006/0401/p1231.html
Ross, V., Detterman, C., & Hallisey, A. (2021). Myofascial Pelvic Pain: An Overlooked and Treatable Cause of Chronic Pelvic Pain. Journal of Midwifery & Women’s Health, 66(2), 148-160. Retrieved from https://doi.org/10.1111/jmwh.13224

What are the First Signs and Symptoms of Endometriosis: Everything You Need to Know
Table of contents
- What is the Endometrium?
- What is Endometriosis Pain?
- Mechanisms of Signs and Symptoms of Endometriosis :
- Painful Periods (dysmenorrhea)
- Diarrhea During Menstrual Periods
- Pain During Intercourse (Dyspareunia)
- Abdominal or Pelvic Pain After Vaginal Sex
- Painful Urination During or Between Menstrual Periods (Dysuria)
- Painful Bowel Movements During or Between Menstrual Periods (Dyschezia)
- Gastrointestinal Problems, Including Bloating, Diarrhea, Constipation, and Nausea
- Causes of Endometriosis
- Complications of Endometriosis
- Diagnosis of Endometriosis
- Treatment for Endometriosis
- Surgical Treatment Options for Endometriosis:
- Multidisciplinary Care
Sharp. Stabbing. Burning. Throbbing. Aching. All these adjectives have been used to describe endometriosis pain. Endometriosis is a condition that, for some women, can cause excruciating uterus pain. Some describe it as feeling like their insides are being pulled out of their bodies. Even worse – endometriosis pain medication doesn’t cut through or provide relief for many patients with this condition. Therefore, an endometriosis diagnosis can be very serious and life-changing news.
Our commitment to our patients runs deep, and our mission is to help patients with endometriosis pain and other complications find the skilled doctors they need.
As our first introduction to the disorder, we will give you a brief overview of the signs and symptoms of endometriosis, its causes, complications, and treatment options (or, as we like to call it – hope). First, we will give you general information on the disease and cover what endometriosis is.
What is the Endometrium?
The endometrium, also known as the endometrial lining, is the tissue that comprises the “wallpaper”, or lining of the uterus. The uterus is the pear-shaped organ that houses a growing baby. During pregnancy and menstruation, the endometrium plays vital functions.
What is Endometriosis Pain?
Endometriosis is pronounced (en-doe-me-tree-O-sis). Endometriosis is a medical condition in which tissue similar to what normally lines the inner walls of the uterus, also known as the endometrium, grows outside the uterus. It is often a very painful, even debilitating disorder. It may involve the ovaries, fallopian tubes, bowels, vagina, cervix, and the tissues that line the pelvis. In rare cases, it can also affect other organs, such as the bladder, kidneys, or lungs.
Signs and Symptoms of Endometriosis Pain

Not all women will experience the same symptoms of endometriosis or degree of intensity/severity. Some women may not experience any symptoms at all.
It is also important to keep in mind that the severity of symptoms is not a solid indicator of the progress of the disease. There are women with advanced stages of endometriosis who experience no symptoms at all and others with mild cases who endure many. Common endometriosis pain symptoms include:
- Painful periods, or dysmenorrhea
- Infertility
- Diarrhea during period
- Pain during intercourse
- Heavy or abnormal menstrual flow
- Abdominal or pelvic pain after vaginal sex
- Painful urination during or between menstrual periods
- Painful bowel movements during or between menstrual periods
- Gastrointestinal problems, including bloating, diarrhea, constipation, and/or nausea
Mechanisms of Signs and Symptoms of Endometriosis:
Painful Periods (dysmenorrhea)
Cyclic release of multiple inflammatory factors activates nerve fiber growth, leads to cell damage and fibrosis, and exacerbates pain during periods.
Infertility
The overall mechanisms can include tubal blockage, local inflammation, uterine muscle dysfunction, local hormonal alterations, and much more.
Diarrhea During Menstrual Periods
Diarrhea may result from endometriosis growing directly on the rectal muscle or endometriosis inflammatory substances. Local production of inflammatory molecules can lead to hyper-motility of the sigmoid and rectum muscles, which can manifest as cramping and diarrhea.
Pain During Intercourse (Dyspareunia)
Endometriosis implants have more nerve endings than usual (hyperinnervated) and can produce pain with pressure. The act of intercourse can apply this pressure on the upper vaginal area and uterosacral ligaments, which are common locations of endo implants. Once this pain occurs and local inflammation further causes tension in the pelvic floor, the muscles surrounding the vagina can contract, which worsens the problem.
Heavy or abnormal menstrual flow
Endometriosis can impact your bleeding by increasing stress from pain or damage to the ovaries, which can change local hormonal function.
Abdominal or Pelvic Pain After Vaginal Sex
Uterine and pelvic floor spasms are part of regular orgasms. When these areas are hypersensitive due to endometriosis, spasms lead to continued contractions and pain that lasts for a while. In addition, rectal fusion to the posterior vaginal wall will also cause more direct pain and inflammation by the vaginal area pulling on the rectal wall. Also, as you probably recognize, any event that stirs up the pelvis and causes some trauma leads to increased molecular signaling, further amplifying the problem.
Painful Urination During or Between Menstrual Periods (Dysuria)
Painful and frequent urination is a prevalent symptom of endometriosis. Endo cells and responding inflammatory cells produce inflammatory molecular signals that aggregate in the area of injury. These molecular signals affect all pelvic organs, including the bladder, leading to bladder wall spasms. Moreover, interstitial cystitis is common in endometriosis patients and can also be a factor. In the worst-case scenario, endo lesions implant inside the bladder, which can also cause cyclic bleeding from the bladder (hematuria).
Painful Bowel Movements During or Between Menstrual Periods (Dyschezia)
Endometriosis causes inflammation and fibrosis or scarring as your body attempts to heal. This inflammation and fibrosis can severely alter the anatomy in the pelvis and distort the rectal course, gluing it to the uterus, cervix, and posterior vaginal wall. This angulation can cause constipation and trouble evacuating stool, while the inflammatory signals cause the rectal muscles to hyper-contract. These mechanisms lead to painful bowel movements, which worsen during the cyclic increases in inflammatory molecules. In the worst-case scenario, the endo will grow through the rectum wall over time, causing cyclic rectal bleeding.
Gastrointestinal Problems, Including Bloating, Diarrhea, Constipation, and Nausea
Generally, intestinal symptoms of endometriosis can be direct or indirect or related to conditions like small intestinal bacterial overgrowth (SIBO). Even if there are no direct implants on the bowel, the endo inside the abdomen and pelvis can cause enough inflammation to irritate the intestine and cause symptoms. In addition, endometriosis implants directly on the bowel can worsen the symptoms.
Causes of Endometriosis
One cause of endometriosis is the direct transplantation of endometrial cells into the abdominal wall during a medical procedure, such as a cesarean section. Besides this known cause of endometriosis, other theories exist as to how it develops:
1. One theory is that during the menstrual cycle, a reverse process takes place where the tissue backs up through the fallopian tubes and into the abdominal cavity, where it attaches and grows.
2. Another theory is a genetic link. This is based on studies that show if someone has a family member with endometriosis, they are more likely to have it as well.
3. Some also suggest that the endometrial tissues travel and implant in other body parts via blood or lymphatic channels, like cancer cells spread.
4. A fourth theory suggests that all cells throughout the body have the ability to transform into endometrial cells.
Complications of Endometriosis
The following are complications of endometriosis if left untreated or in advanced stages of the disorder:
- Infertility/subfertility
- Chronic pelvic pain that can result in disability
- Anatomic disruption of involved organ systems (i.e., adhesions, ruptured cysts, renal failure)
Diagnosis of Endometriosis
The diagnosis starts with assessing signs and symptoms and then performing imaging studies such as MRI and ultrasonography. But the confirmation or exclusion of the endometriosis diagnosis is only possible with surgical biopsy and histopathology. Laparoscopy is the gold-standard surgical modality for diagnosis in all cases.
Treatment for Endometriosis
Endometriosis needs a multidisciplinary team approach for effective and holistic treatment. This team should include the following medical professionals:
- Nutritionist
- Physical therapist
- Endometriosis surgeon
- Mental health therapist
- Pain management specialist
Pain is often the biggest complaint from patients with endometriosis. Therefore, many treatment options are aimed at pain control. So first, here are some options for women to help temporarily ease the pain of endometriosis:
- Exercise
- Meditation
- Breath work
- Heating pads
- Rest and relaxation
- Prevention of constipation
These therapies may be used in combination with medical and/or surgical options to lessen the pelvic pain associated with this disorder. Furthermore, alternative therapies exist that may be used in conjunction with other interventions, and those include but are not limited to:
- Homeopathy
- Immune therapy
- Allergy management
- Nutritional approached
- Traditional Chinese medicine
*Be sure to discuss any of these treatment options with a physician before implementing them.
The Right Medical Treatment For You:
Options for medical and/or surgical treatments for endometriosis are going to depend on several factors, including:
- Desire for pregnancy
- The extent of the disease
- Type and severity of symptoms
- Patient opinions and preferences
- Overall health and medical history
- Expectations of the course of the disease
- Patients’ tolerance level for medications, therapies, and/or procedures
In some cases, management of pain might be the only treatment. In others, medical options may be considered. The following are typical non-surgical, medical treatments for endometriosis:
- “Watch and Wait” approach, where the course of the disease is monitored and treated accordingly
- Pain medication (anything from non-steroidal anti-inflammatory drugs [NSAIDs] to other over-the-counter and/or prescription analgesics)
- Hormonal therapy, such as:
- Progestins
- Oral contraceptives with both estrogen and progestin to reduce menstrual flow and block ovulation
- Danazol (a synthetic derivative of the male hormone testosterone)
- Gonadotropin-releasing hormone antagonist, which stops ovarian hormone production
Surgical Treatment Options for Endometriosis:
Despite their effectiveness in symptom control, pain medications can have significant side effects. Moreover, these medications do not stop the progression of the disease, and symptoms might return once stopped. But on the other side, surgery can lead to long-term relief and can prevent further damage to tissues. Your treatment plan should be a shared decision based on your desires, goals, and abilities.
Almost all endometriosis surgical procedures are laparoscopic or robotic. These are minimally invasive surgeries in which small tubes with lights and cameras are inserted into the abdominal wall. It allows the doctor to see the internal organs and remove endometriosis.
Excision of Endometriosis
In this technique, a surgeon cuts out much or all of the endometriosis lesions from the body. Therefore, surgeons avoid leaving any endometriosis lesions behind while preserving normal tissues. This technique is widely adopted by highly skilled endometriosis surgeons who are world leaders.
Ablation of Endometriosis
In this technique, a surgeon burns the surface of the endometriosis lesions and leaves them in the body. Most top experts highly criticize this ablation method. Ablation is most popular with surgeons who have not received enough training to do excision. As a result, these surgeons are not comfortable performing excision, and they do the ablation.
Hysterectomy
this is a surgery in which surgeons remove the uterus and sometimes ovaries. But, many surgeons consider hysterectomy an outdated and ineffective treatment for endometriosis. Almost all top endometriosis surgeons reject doing it unless there is a clear indication for hysterectomy such as adenomyosis.
Laparotomy
this surgical procedure cuts and opens the abdomen and does not use thin tubes. Therefore it is more extensive than a laparoscopy. Very few surgeons still do laparotomy because of its complications. Almost none of the top endometriosis surgeons do laparotomy for endometriosis.
Multidisciplinary Care
Along with effective surgical treatment, the patient should start working with endometriosis experts in physical therapy, mental health, nutrition, and pain management to achieve the best possible outcome.
Get in touch with Dr. Steve Vasilev

Pain with sex
A little spoken of symptom of endometriosis is pain with sex. In medical terms, it is called dyspareunia- meaning pelvic pain that occurs before, during, or after intercourse (although similar pain can also be felt with an exam or insertion of a tampon). Deep dyspareunia is “a cardinal symptom of endometriosis” (Wahl et al., 2020) with more than half of women with endometriosis experiencing it (Yong, 2017). This can play a significant role in the quality of life and relationships (Denny & Mann, 2007). The pain has been described cramping, stabbing, or stinging- among other things.
Yong (2017) proposes a classification of four types of deep dyspareunia in people with endometriosis: “type I that is directly due to endometriosis; type II that is related to a comorbid condition; type III in which genito-pelvic pain penetration disorder is primary; and type IV that is secondary to a combination of types I to III.” Fritzer and Hudelist (2017) found that “surgical excision of endometriosis is a feasible and good treatment option for pain relief and improvement of quality of sex life in symptomatic women with endometriosis.” Excision surgery for endometriosis overall shows improvement in pain with sex; however, other factors such as adenomyosis or painful bladder syndrome (interstitial cystitis) can continue to cause symptoms and should be addressed (Crispi et al., 2021). “Myofascial or nervous system mechanisms may be important for deep dyspareunia in women with endometriosis, even in those with moderate-to-severe disease (Stage III/IV)” (Orr et al., 2018). While it may feel embarrassing to bring up, it is an important aspect of your health to discuss with your provider. They might suggest pelvic floor therapy, medication, or other options to help. But it is important to address any underlying conditions.
In the meantime, some things to try:
- Have open communication with your partner about what you are feeling and your needs
- Experiment with different times of your cycle that may be less painful (such as the week after ovulation or the first couple of weeks after your period)
- Use of a lubricant
- Try different positions to find which is best for you
- Utilizing forms of intimacy that does not involve penetration
Find more here: https://icarebetter.com/pain-with-penetration/
References
Crispi Jr, C. P., Crispi, C. P., de Oliveira, B. R. S., de Nadai Filho, N., Peixoto-Filho, F. M., & Fonseca, M. D. F. (2021). Six-month follow-up of minimally invasive nerve-sparing complete excision of endometriosis: What about dyspareunia?. Plos one, 16(4), e0250046. Retrieved from https://doi.org/10.1371/journal.pone.0250046
Denny, E., & Mann, C. H. (2007). Endometriosis-associated dyspareunia: the impact on women’s lives. BMJ Sexual & Reproductive Health, 33(3), 189-193. Retrieved from https://srh.bmj.com/content/familyplanning/33/3/189.full.pdf
Fritzer, N., & Hudelist, G. (2017). Love is a pain? Quality of sex life after surgical resection of endometriosis: a review. European Journal of Obstetrics & Gynecology and Reproductive Biology, 209, 72-76. Retrieved from https://doi.org/10.1016/j.ejogrb.2016.04.036
Orr, N. L., Noga, H., Williams, C., Allaire, C., Bedaiwy, M. A., Lisonkova, S., … & Yong, P. J. (2018). Deep dyspareunia in endometriosis: role of the bladder and pelvic floor. The journal of sexual medicine, 15(8), 1158-1166. DOI: 10.1016/j.jsxm.2018.06.007
Wahl, K. J., Orr, N. L., Lisonek, M., Noga, H., Bedaiwy, M. A., Williams, C., … & Yong, P. J. (2020). Deep dyspareunia, superficial dyspareunia, and infertility concerns among women with endometriosis: a cross-sectional study. Sexual medicine, 8(2), 274-281. Retrieved from https://doi.org/10.1016/j.esxm.2020.01.002
Yong, P. J. (2017). Deep dyspareunia in endometriosis: a proposed framework based on pain mechanisms and genito-pelvic pain penetration disorder. Sexual medicine reviews, 5(4), 495-507. Retrieved from https://doi.org/10.1016/j.sxmr.2017.06.005
Physical Therapy Before Excision Surgery for Endometriosis
Table of contents
- Physical Therapists can Optimize Care by Helping a Patient Get to a Specialist while Providing Physical Therapy Treatment.
- Endo Specialists’ Wait Times Vary Greatly Depending on Where You are Located.
- Most Studies Research the Effectiveness of Physical Therapy Following Excision Surgery. What About Physical Therapy Before Excision Surgery?
- A Few Factors to Keep in Mind if You are Seeking Pelvic Physical Therapy Before Excision Surgery
Endometriosis can cause multiple issues for patients. And it can create the need for a multidisciplinary care team to address chronic pelvic pain. Physical therapy is one example of part of a multidisciplinary treatment plan for endometriosis symptoms. Guest writer Rebecca Patton, PT, DPT, discusses considerations for using physical therapy while awaiting excision surgery:
Pelvic physical therapy has gained more following and prompted much-needed discussions in recent years. However, pelvic physical therapy looks quite different for someone with chronic pelvic pain and endometriosis.
The reality is that pelvic physical therapists may be the first line of defense to refer a patient to a specialist. First, because we have direct access, meaning a patient can see us for an evaluation before seeing a physician. Second, because symptoms of endometriosis are often missed or dismissed by referring providers. In the latter case, someone may be referred to physical therapy before excision surgery or even before seeing an endo specialist.
Physical Therapists can Optimize Care by Helping a Patient Get to a Specialist while Providing Physical Therapy Treatment.
If we are seeking to provide the best care available for the treatment of endo, getting a faster diagnosis and referring a patient to an excision specialist is the primary goal. With a thorough medical history including bowel and bladder habits, menstrual symptoms, pelvic pain symptoms, previous treatment, and understanding the patient’s experience, a pelvic physical therapist can create a differential diagnosis list that may include endometriosis. If endometriosis is suspected, a referral to an excision specialist should be given to the patient and explained.
Endo Specialists’ Wait Times Vary Greatly Depending on Where You are Located.
In my personal experience in Phoenix, AZ, a large metropolitan area with several specialists, it takes anywhere from 3-12 months. More time if we are in the middle of a global pandemic. Decreased access in rural areas may also increase waiting times. One positive change is the inclusion of virtual appointments which may improve access for those in rural areas.
During the waiting period, the goal is to manage pain and maintain some regularity with bowel and bladder habits until excision surgery. Internal pelvic floor retraining may or may not be appropriate during this time.
As mentioned before, physical therapy before excision surgery is going to look different from treatments for other conditions. As a patient, you want to ensure the physical therapist you are seeing treats patients with endo regularly. You may want to consult with them prior about how often they treat patients with endo and what treatments they use specifically. Additional coursework for visceral and abdominal manual therapy techniques, nerve mobilization, and myofascial therapy techniques will be helpful.
Most Studies Research the Effectiveness of Physical Therapy Following Excision Surgery. What About Physical Therapy Before Excision Surgery?
Zhao et al. (1) found that 12 weeks of PMR (progressive muscle relaxation) training is effective in improving anxiety, depression, and quality of life of endometriosis patients under GnRH agonist therapy. These participants had not received excision surgery.
Awad et al. (2) found improvements in posture and pain with an 8-week regular exercise program in those diagnosed with mild to moderate endometriosis. This exercise program included posture awareness, diaphragm breathing, muscle relaxation techniques, lower back and hip stretches, and walking. Of note, this exercise program was not vigorous exercise. These participants were also receiving hormonal treatment but not receiving pain medication.
Both studies did not say that physical exercise or PMR plays a role in the prevention of the occurrence or progression of endometriosis. Both studies were short-term (8-12 weeks) and did not explore pain management directly before excision or outcomes after excision.
In the time that a patient is waiting for excision surgery, I believe physical therapy treatment can be effective at minimizing overall pain levels and improving quality of life.
A Few Factors to Keep in Mind if You are Seeking Pelvic Physical Therapy Before Excision Surgery
1. Your symptoms after physical therapy should not last more than 1-2 days and should feel manageable. Being bedridden for a week after physical therapy is not a helpful treatment. If you experience this, be sure to communicate it with your physical therapist to adjust the plan. Not all pelvic PTs are experienced with this type of treatment and they may create an exercise plan that is too vigorous.
2. Internal pelvic floor treatment is not always the most helpful in this situation and may exacerbate symptoms. An individualized plan is important to discuss with your provider.
3. You are in charge of your body. If you don’t feel like treatment is working then communicate that to your team and discuss other options. It is always okay to voice your concerns to change the treatment to fit you best.
4. Treatment before surgery requires a multidisciplinary team. This may include other pain management options including medication.
iCareBetter is doing the groundwork to vet pelvic physical therapists.
Rebecca Patton PT, DPT (If you are seeking a pelvic PT, I accept consultations through my website for in person and telehealth appointments: https://www.pattonpelvichealth.com/)
For more resources on physical therapy for endometriosis see: https://nancysnookendo.com/learning-library/treatment/lessons/physical-therapy-resources/
References
Zhao L, Wu H, Zhou X, et al.: Effects of progressive muscular relaxation training on anxiety, depression and quality of life of endometriosis patients under gonadotrophin-releasing hormone agonist therapy. Eur J Obstet Gynecol Reprod Biol, 2012, 162: 211–215. [PubMed] [Google Scholar]
Awad E, Ahmed HAH, Yousef A, Abbas R. Efficacy of exercise on pelvic pain and posture associated with endometriosis: within subject design. J Phys Ther Sci. 2017;29(12):2112-2115. doi:10.1589/jpts.29.2112 [NCBI]

