
Mast cells and endometriosis
Endometriosis is an inflammatory disorder, and this inflammation can lead to increased pain, fatigue, and general feelings of unwellness. Mast cells are immune system cells that can stimulate inflammation (Graziottin, Skaper, & Fusco, 2014). Mast cells hold proinflammatory substances (such as histamine, cytokines, prostaglandins, and more), and, when activated, release these proinflammatory substances (Weller, n.d.). When responding to a threat to the body and for healing, this is a good thing. But when mast cells are activated in endometriosis, not so much.
Activated mast cells (the ones that have released all those proinflammatory substances) have been found in higher quantities in endometriosis lesions versus normal tissue (Hart, 2015; Indraccolo & Barbieri, 2010; Sugamata et al., 2005). Estrogen seems to stimulate mast cells to support the inflammatory process (Zhu et al., 2018). In fact, estrogen receptors are found on mast cells and the high local levels of estrogen from endometriotic lesions may activate the mast cells and lead to pain (Hart, 2015; Zhu et al., 2018). While many therapies for endometriosis involve lowering estrogen production by the feedback loop between the brain and the ovaries, it should be remembered that endometriosis lesions demonstrate production of estrogen themselves (and also show resistance to progesterone) (Delvoux et al., 2009). In fact, the level of estrogen in endometriosis lesions were related to pain symptoms in patients with endometriosis while blood levels of estrogen were not (Zhu et al., 2018).
In addition, nerve fibers in endometriosis lesions have been shown to “release neural peptides such as nerve growth factor and substance P” that in turn activate mast cells to release those proinflammatory substances “which contributes to the development of pain and hyperalgesia in patients with endometriosis” (Zhu & Zhang, 2013). Those granules released by mast cells can contribute to new blood vessel growth, more inflammation, and nerve growth, which can lead to pain (Graziottin, 2009). This persistent inflammation from endometriosis lesions “intensifies neurogenic inflammation and tissue damage” leading to “progressive functional and anatomic damage associated with prominent tissue scarring, exemplified by the natural history of endometriosis” and “up-regulation of nerve pain” (Graziottin, 2009).
So, mast cells are recruited to endometriosis lesions, respond to the higher local estrogen and other inflammatory conditions, release their proinflammatory substances which can lead to pain and scarring. This effect of mast cells is associated in other pain syndromes as well, such as interstitial cystitis, IBS, vulvodynia, complex regional pain syndrome, migraines, and fibromyalgia (Aich et al., 2015).
References
Aich, A., Afrin, L. B., & Gupta, K. (2015). Mast cell-mediated mechanisms of nociception. International journal of molecular sciences, 16(12), 29069-29092. Retrieved from https://doi.org/10.3390/ijms161226151
Delvoux, B., Groothuis, P., D’Hooghe, T., Kyama, C., Dunselman, G., & Romano, A. (2009). Increased production of 17β-estradiol in endometriosis lesions is the result of impaired metabolism. The Journal of Clinical Endocrinology & Metabolism, 94(3), 876-883. Retrieved from https://academic.oup.com/jcem/article/94/3/876/2596530
Graziottin, A., Skaper, S. D., & Fusco, M. (2014). Mast cells in chronic inflammation, pelvic pain and depression in women. Gynecological Endocrinology, 30(7), 472-477. Retrieved from https://www.tandfonline.com/doi/abs/10.3109/09513590.2014.911280
Graziottin, A. (2009). Mast cells and their role in sexual pain disorders. Female Sexual Pain Disorders, 176. Retrieved from https://www.fondazionegraziottin.org/ew/ew_articolo/1820%20-%20mast%20cells%20and%20SPD.pdf
Hart, D. A. (2015). Curbing inflammation in multiple sclerosis and endometriosis: should mast cells be targeted?. International journal of inflammation, 2015. Retrieved from https://www.hindawi.com/journals/iji/2015/452095/
Indraccolo, U., & Barbieri, F. (2010). Effect of palmitoylethanolamide–polydatin combination on chronic pelvic pain associated with endometriosis: Preliminary observations. European Journal of Obstetrics & Gynecology and Reproductive Biology, 150(1), 76-79. Retrieved from https://www.sciencedirect.com/science/article/abs/pii/S0301211510000424
Sugamata, M., Ihara, T., & Uchiide, I. (2005). Increase of activated mast cells in human endometriosis. American journal of reproductive immunology, 53(3), 120-125. Retrieved from https://doi.org/10.1111/j.1600-0897.2005.00254.x
Weller, C. (n.d.). Mast cells. Retrieved from https://www.immunology.org/public-information/bitesized-immunology/cells/mast-cells
Zhu, T. H., Ding, S. J., Li, T. T., Zhu, L. B., Huang, X. F., & Zhang, X. M. (2018). Estrogen is an important mediator of mast cell activation in ovarian endometriomas. Reproduction, 155(1), 73-83. Retrieved from https://doi.org/10.1530/REP-17-0457
Zhu, L., & Zhang, X. (2013). Research advances on the role of mast cells in pelvic pain of endometriosis. Journal of Zhejiang University (Medical Science), 42(4), 461. DOI: 10.3785/j.issn.1008-9292.2013.04.015

FAQ’s, Podcasts, Resources About Endo, and More!
You can find a diverse gathering of information about endometriosis on our website. We have some information you may not have thought to look for or were unsure of where it might located. Here’s a glimpse at a few of the resources you can find:
In our Resources section, you will find material that includes a wide variety of topics and links to help you on your endometriosis journey.
- If you prefer to listen instead of read, we have several links to podcasts, videos, and webinars.
- If you are looking for info on advocacy and other helpful sources, then see here.
- Need information about navigating insurance? We have info on what to know to help be your own best advocate- as well as info for those on Tricare
- We have topics specific for teens, infertility, pregnancy, and LGBTQIA+
- Tips for topics such as keeping track of your personal medical history, things to pack for surgery/hospital, what to expect before and after surgery, and more.
- Resources for those in the UK and Australia
- and more!
In our Frequently Asked Questions section, you can find answers to questions such as:
- Is that really true? Info on Myths and Misinformation
- Is endometriosis an autoimmune disease?
- Does endometriosis increase my risk of cancer?
- Is There Microscopic or Occult Endometriosis
- Can endometriosis persist after hysterectomy/ovary removal/menopause?
- Is there a genetic component to endometriosis?
- Is there a link between heart disease and endometriosis?
- What effects can long term low estrogen cause?
Endometriosis has several related conditions that can cause similar symptoms. While treating endometriosis is important, it is equally important to treat these other conditions that might be present in order to find relief.
- Adenomyosis
- Endometrial/Uterine Polyps
- Interstitial Cystitis/Bladder Pain Syndrome
- Pelvic Floor Dysfunction
- Fibroids (Leiomyomas)
- Polycystic Ovarian Syndrome (PCOS)
- Pudendal Neuralgia and Vulvodynia
- Pelvic Congestion Syndrome
- Occult Hernia
- Migraines and Endometriosis
Information about endometriosis itself and its treatment can be found throughout the website.
- What makes endometriosis different from the lining of the uterus? Differences in how endometriosis looks and behaves (how it behaves in response to estrogen and progesterone, can make its own nerves and blood vessels, as well as other differences)
- Where can endometriosis be found in the body? (including some weird places)
- How does endometriosis start?
- What are the symptoms of endometriosis?
- How is it diagnosed? How useful are an ultrasound, MRI, or labwork with endometriosis?
- Why is excision surgery recommended? Why should I see a specialist?
- What treatment options are there?
You’ll find all these topics and more on the website. Start exploring!

Your Story Isn’t Over; Mental Health Awareness
May is mental health awareness month and a good time to shine a light on the affects that endometriosis has on our mental health. A significant number of people worldwide suffer from a mental health disorder. While mental health covers a wide spectrum of disorders, two of the most pervasive are anxiety and depression (NAMI, 2021). Both of these not only affect a large portion of the population in general, but also can be found in higher rates in those with chronic illnesses- especially those involving chronic pain (Li et al., 2018).
Endometriosis has been associated “a wide spectrum of different types of pain, ranging from severe dysmenorrhea to chronic pelvic and other comorbid pain conditions” and those with endometriosis have an “elevated likelihood of developing depression and anxiety disorders” (Li et al., 2018). Endometriosis greatly affects quality of life, relationships, stress, professional life, and many other factors that can play into depression and anxiety (Donatti et al., 2017; Lagana et al., 2017). While these factors can play into depression and anxiety, research has suggested that endometriosis leads to specific changes in the brain that are associated with pain, anxiety, and depression (Lima Filho et al., 2019). For example, in a study done on mice, researchers found that “endometriosis led to changes in expression of several genes in the brain regions associated with pain, anxiety, and depression” (Li et al., 2018). In addition, some studies have shown a shared genetic predisposition between depression and endometriosis (Adewuyi et al., 2021).
Our mental health is important. As chronic pelvic pain from endometriosis can affect our mental health, it is important to address the underlying cause (Van den Broeck et al., 2013). But we also need to seek care for our mental health in other ways as well. We can’t do it all alone and seeking help from a professional for our mental health is every bit as important as seeking help for a broken bone. Just as we do physical therapy to help our musculoskeletal system, counseling and cognitive behavioral therapy is like physical therapy for our mental well-being. Endometriosis impacts our relationships, our ability to work, our sense of self, and pretty much every aspect of our lives. Seeking help to cope is not a sign of weakness, but of strength. One of my favorite symbols for mental health is from The Semicolon Project. The semicolon is a sign that the sentence, the story, isn’t over yet. Know that you are not alone, and your story isn’t over yet.
National Suicide Prevention Hotline: 1-800-273-8255
References
Adewuyi, E. O., Mehta, D., Sapkota, Y., Auta, A., Yoshihara, K., Nyegaard, M., … & Nyholt, D. R. (2021). Genetic analysis of endometriosis and depression identifies shared loci and implicates causal links with gastric mucosa abnormality. Human Genetics, 140(3), 529-552. doi: 10.1007/s00439-020-02223-6
Donatti, L., Ramos, D. G., Andres, M. D. P., Passman, L. J., & Podgaec, S. (2017). Patients with endometriosis using positive coping strategies have less depression, stress and pelvic pain. Einstein (São Paulo), 15(1), 65-70. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5433310/
Laganà, A. S., La Rosa, V. L., Rapisarda, A. M. C., Valenti, G., Sapia, F., Chiofalo, B., … & Vitale, S. G. (2017). Anxiety and depression in patients with endometriosis: impact and management challenges. International journal of women’s health, 9, 323. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5440042/
Li, T., Mamillapalli, R., Ding, S., Chang, H., Liu, Z. W., Gao, X. B., & Taylor, H. S. (2018). Endometriosis alters brain electrophysiology, gene expression and increases pain sensitization, anxiety, and depression in female mice. Biology of reproduction, 99(2), 349-359. Retrieved from https://doi.org/10.1093/biolre/ioy035
Lima Filho, P. W. L., Chaves Filho, A. J. M., Vieira, C. F. X., de Queiroz Oliveira, T., Soares, M. V. R., Jucá, P. M., … & das Chagas Medeiros, F. (2019). Peritoneal endometriosis induces time-related depressive-and anxiety-like alterations in female rats: involvement of hippocampal pro-oxidative and BDNF alterations. Metabolic brain disease, 34(3), 909-925. Retrieved from https://doi.org/10.1007/s11011-019-00397-1
National Alliance on Mental Illness (NAMI). (2021). Mental health by the numbers. Retrieved from https://www.nami.org/mhstats
Van den Broeck, U., Meuleman, C., Tomassetti, C., D’Hoore, A., Wolthuis, A., Van Cleynenbreugel, B., … & D’Hooghe, T. (2013). Effect of laparoscopic surgery for moderate and severe endometriosis on depression, relationship satisfaction and sexual functioning: comparison of patients with and without bowel resection. Human Reproduction, 28(9), 2389-2397. Retrieved from https://doi.org/10.1093/humrep/det260
Endometriosis after a hysterectomy or menopause
what are the symptoms of endometriosis after menopause?
Endometriosis does not “die off” or go away with a hysterectomy or menopause. Some people do find some relief from their symptoms, but endometriosis can still persist. Endometriosis often has several related or comorbid conditions (such as adenomyosis or fibroids) that share similar symptoms (pain with menstruation, chronic pelvic pain, etc.) that a hysterectomy might help – but it may not stop your symptoms from endometriosis. Endometriosis exists outside of the uterus and can still respond to hormonal influences (Bulun et al., 2002). Even if your ovaries are removed, endometriosis lesions can produce their own estrogen (Huhtinen et al., 2012). This is important to note because estrogen causes endometriosis lesions to grow and persist (Bulun et al., 2012). So even with the removal of the ovaries or with menopause, endometriosis can sustain itself.
There is high recurrence of symptoms with the removal of just the uterus; but, even with the removal of the ovaries, any endometriosis lesions left behind can continue to grow, progress, and cause symptoms (Clayton et al., 1999; Inceboz, 2015; Khan et al., 2013; Rizk et al., 2014). So, if you have your uterus and ovaries removed for other conditions, it is best that all endometriosis lesions be removed as well. The skill of the surgeon at removing all endometriosis is important. Rizk et al. (2014) report that “the recurrence of endometriosis symptoms and pelvic pain are directly correlated to the surgical precision and removal of peritoneal and deeply infiltrated disease.”
Endometriosis has been found in about 2.2% of postmenopausal women (Zanello et al., 2019). Inceboz (2015) states that “endometriotic lesions remained biologically active, with proliferative activity and preserved hormonal responsiveness, even in the lower estrogenic environment in the postmenopause.” Postmenopausal endometriosis should be managed surgically according to Streuli et al. (2017) and Zanello et al. (2019).
What about hormone replacement if you are in menopause or have had your uterus and ovaries removed? Hormone replacement therapy (HRT) is important as “the hypo-estrogenic state was demonstrated to be a risk factor for cardiovascular and bone disease” (Zanello et al., 2019). While HRT has not been concluded useful for preventing heart disease, it can be useful for those at a higher risk of osteoporosis (Zanello et al., 2019). There isn’t much data available to help guide the decision, but Zanello et al. (2019) report that “in young menopausal women with premature or surgically-induced menopause the benefits of HRT probably overcome the risks” and “in women with residual endometriosis after surgery, the use of HRT should be discussed and the risk of recurrence should be carefully considered before starting an estrogen-based replacement therapy”. Rizk et al. (2014) also states that “the general consensus is that the benefits outweigh the risks” and that starting HRT soon after menopause does not seem to have a faster rate of recurrence. Zanello et al. (2019) concludes that “based on low-grade evidence in the literature, we recommend prescribing combined HRT instead of unopposed estrogen.” It also depends on if your endometriosis was removed.
Does Endometriosis Go Away After Menopause?
endometriosis symptoms after menopause
References
Bulun, S. E., Gurates, B., Fang, Z., Tamura, M., Sebastian, S., Zhou, J., … & Yang, S. (2002). Mechanisms of excessive estrogen formation in endometriosis. Journal of reproductive immunology, 55(1-2), 21-33. Retrieved from https://doi.org/10.1016/S0165-0378(01)00132-2
Bulun, S. E., Monsavais, D., Pavone, M. E., Dyson, M., Xue, Q., Attar, E., … & Su, E. J. (2012, January). Role of estrogen receptor-β in endometriosis. In Seminars in reproductive medicine (Vol. 30, No. 01, pp. 39-45). Thieme Medical Publishers. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4034571/…
Clayton, R. D., Hawe, J. A., Love, J. C., Wilkinson, N., & Garry, R. (1999). Recurrent pain after hysterectomy and bilateral salpingo‐oophorectomy for endometriosis: evaluation of laparoscopic excision of residual endometriosis. BJOG: An International Journal of Obstetrics & Gynaecology, 106(7), 740-744. Retrieved from https://obgyn.onlinelibrary.wiley.com/doi/full/10.1111/j.1471-0528.1999.tb08377.x?fbclid=IwAR04aFoLsukqsYutNPNXtJNZpKLNEJbgOOon334NW8D7wvwzZMWaS2YaZts
Huhtinen, K., Ståhle, M., Perheentupa, A., & Poutanen, M. (2012). Estrogen biosynthesis and signaling in endometriosis. Molecular and cellular endocrinology, 358(2), 146-154. Retrieved from https://www.sciencedirect.com/science/article/abs/pii/S0303720711005041
Inceboz, U. (2015). Endometriosis after menopause. Women’s Health, 11(5), 711-715. Retreived from https://journals.sagepub.com/doi/full/10.2217/whe.15.59
Khan, K. N., Kitajima, M., Fujishita, A., Nakashima, M., & Masuzaki, H. (2013). Toll‐like receptor system and endometriosis. Journal of Obstetrics and Gynaecology Research, 39(8), 1281-1292. Retrieved from https://obgyn.onlinelibrary.wiley.com/doi/full/10.1111/jog.12117
Rizk, B., Fischer, A. S., Lotfy, H. A., Turki, R., Zahed, H. A., Malik, R., … & Herrera, D. (2014). Recurrence of endometriosis after hysterectomy. Facts, views & vision in ObGyn, 6(4), 219. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4286861/
Zanello, M., Borghese, G., Manzara, F., Degli Esposti, E., Moro, E., Raimondo, D., … & Seracchioli, R. (2019). Hormonal replacement therapy in menopausal women with history of endometriosis: a review of literature. Medicina, 55(8), 477. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6723930/

Endometriosis and Pregnancy
Endometriosis is often associated with infertility. Infertility does not mean you cannot get pregnant, but rather there is a delay in achieving pregnancy. It is technically defined as not achieving a “clinical pregnancy after 12 months or more of regular unprotected sexual intercourse” (World Health Organization, n.d.). An estimated 30–50% of women with endometriosis are reported to have difficulty with infertility (Macer & Taylor, 2012). In addition, endometriosis does not have to be an “advanced stage” for it to affect fertility (Bloski & Pierson, 2008).
“Current evidence indicates that suppressive medical treatment of endometriosis does not benefit fertility and should not be used for this indication alone. Surgery is probably efficacious for all stages of the disease.”
(Ozkan, Murk, & Arici, 2008)
With infertility being related to endometriosis, it is unbelievable that pregnancy might still be recommended as a treatment for endometriosis. While some may have a temporary relief of symptoms, others can experience an increase. In fact, some “imaging and histopathology studies of endometriotic lesions during pregnancy show that they may grow rapidly during pregnancy” (Leeners & Farquhar, 2019). Pregnancy will not treat or cure endometriosis. Research has stated that “women aiming for pregnancy on the background of endometriosis should not be told that pregnancy may be a strategy for managing symptoms and reducing progression of the disease” (Leeners et al., 2018). This is echoed again by Leeners and Farquhar (2019) who point out that “the decision to have children should not be influenced by any perceived benefit of improving endometriosis but should be made solely on the wish for parenthood.”
While the overall risk is still low, endometriosis has been associated with some difficulties during pregnancy. Zullo et al. (2017) looked at 24 studies involving almost 2 million women with endometriosis to consider the possible effects of endometriosis during pregnancy . They found that “women with endometriosis have a statistically significantly higher risk of preterm birth, miscarriage, placenta previa, small for gestational age infants, and cesarean delivery” compared to healthy controls (Zullo et al., 2017). Zullo et al. (2017) did not find any significant association with gestational hypertension and preeclampsia with endometriosis; however, adenomyosis has been found to have some correlation with pregnancy-induced hypertension and preeclampsia (Porpora et al., 2020). Adenomyosis has been found to result in a higher likelihood of preterm birth, small for gestational age, and pre-eclampsia (Razavi et al., 2019). Adenomyosis and endometriosis frequently coexist, so it can be hard to determine how much is one or the other causing these effects (Choi et al., 2017).
On a positive note, Porpora et al. (2020) noted that “no difference in fetal outcome was found” and concluded that “endometriosis does not seem to influence fetal well-being”. This was also found by Uccella et al. (2019), stating that “neonatal outcomes are unaffected by the presence of the disease”. Again, a normal pregnancy is still highly possible. For more information on this topic, see Pregnancy and Endometriosis.
References
Bloski, T., & Pierson, R. (2008). Endometriosis and chronic pelvic pain: unraveling the mystery behind this complex condition. Nursing for women’s health, 12(5), 382-395. doi: 10.1111/j.1751-486X.2008.00362.x
Choi, E. J., Cho, S. B., Lee, S. R., Lim, Y. M., Jeong, K., Moon, H. S., & Chung, H. (2017). Comorbidity of gynecological and non-gynecological diseases with adenomyosis and endometriosis. Obstetrics & gynecology science, 60(6), 579. Retrieved from https://synapse.koreamed.org/upload/SynapseData/PDFData/3021ogs/ogs-60-579.pdf
Leeners, B., Damaso, F., Ochsenbein-Kölble, N., & Farquhar, C. (2018). The effect of pregnancy on endometriosis—facts or fiction?. Human reproduction update, 24(3), 290-299. Retrieved from https://doi.org/10.1093/humupd/dmy004
Leeners, B., & Farquhar, C. M. (2019). Benefits of pregnancy on endometriosis: can we dispel the myths?. Fertility and sterility, 112(2), 226-227. Retrieved from https://doi.org/10.1016/j.fertnstert.2019.06.002
Macer, M. L., & Taylor, H. S. (2012). Endometriosis and infertility: a review of the pathogenesis and treatment of endometriosis-associated infertility. Obstetrics and Gynecology Clinics, 39(4), 535-549. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3538128/pdf/nihms422379.pdf
Ozkan, S., Murk, W., & Arici, A. (2008). Endometriosis and infertility: epidemiology and evidence‐based treatments. Annals of the New York Academy of Sciences, 1127(1), 92-100. DOI: 10.1196/annals.1434.007
Porpora, M. G., Tomao, F., Ticino, A., Piacenti, I., Scaramuzzino, S., Simonetti, S., … & Benedetti Panici, P. (2020). Endometriosis and pregnancy: a single institution experience. International journal of environmental research and public health, 17(2), 401. Retrieved from https://www.mdpi.com/1660-4601/17/2/401
Razavi, M., Maleki‐Hajiagha, A., Sepidarkish, M., Rouholamin, S., Almasi‐Hashiani, A., & Rezaeinejad, M. (2019). Systematic review and meta‐analysis of adverse pregnancy outcomes after uterine adenomyosis. International Journal of Gynecology & Obstetrics, 145(2), 149-157. Retrieved from https://www.endometriozisdernegi.org/konu/dosyalar/pdf/makale_ozetleri/Mayis2019/makale17.pdf
Uccella, S., Manzoni, P., Cromi, A., Marconi, N., Gisone, B., Miraglia, A., … & Ghezzi, F. (2019). Pregnancy after endometriosis: maternal and neonatal outcomes according to the location of the disease. American journal of perinatology, 36(S 02), S91-S98. DOI: 10.1055/s-0039-1692130
World Health Organization. (n.d.).Infertility definitions and terminology. Retrieved from https://www.who.int/teams/sexual-and-reproductive-health-and-research/areas-of-work/fertility-care/infertility-definitions-and-terminology
Zullo, F., Spagnolo, E., Saccone, G., Acunzo, M., Xodo, S., Ceccaroni, M., & Berghella, V. (2017). Endometriosis and obstetrics complications: a systematic review and meta-analysis. Fertility and sterility, 108(4), 667-672. Retrieved from https://doi.org/10.1016/j.fertnstert.2017.07.019

How to Study a Research Study
We post a lot of links and references to research studies, but it can be difficult to interpret them. Even harder is determining how relevant those studies are. Here are a few things to consider as you look at research on endometriosis.
When you look at research studies, you first want to assess how strong of evidence it is presenting. One quick way to tell is by the type of study. The University of Alabama at Birmingham (2021) has a good list of the types of studies, going from strongest evidence to weakest. In short:
“The most scientific, rigorous study designs are randomized controlled trials, systematic reviews, and meta-analysis. These types of studies are thought to provide stronger levels of evidence because they reduce, but do not eliminate, potential biases and confounders.”
(University of Alabama at Birmingham, 2021)
Bias is any errors in design that might throw off the conclusions. Bias, whether intentional or unintentional, can occur in “data collection, data analysis, interpretation and publication which can cause false conclusions” (Simundic, 2013). Find out more about that here. Confounding factors are any variables not factored into the study that can muddle with the interpretation of the results- “they can suggest there is correlation when in fact there isn’t” (Statistics How To, n.d.). This is important when looking at the conclusions drawn. For instance, in last week’s newsletter about endometriomas, we noted that recurrence rates are hard to tell from studies because their definition of “recurrence” varies widely from study to study (was it pathology from surgery or recurrence of symptoms that might actually be from a related condition?). You also want to look how large the study was, did it include several different variables, was it limited to a specific group, how was the study funded and what ethical considerations are given, etc. One tool for helping to analyze such factors can be found here.
Most studies have a short summary at the beginning that can be helpful. For instance, let’s look at this study from Shigesi et al. (2019) found here. The title itself tells us it is a systematic review and meta-analysis: “The association between endometriosis and autoimmune diseases: a systematic review and meta-analysis”. So, we’re starting off good.
The study then starts with the summary called an abstract- which tells us the background of the problem they want to study, how they performed the study, the outcomes they found, and a discussion on what those outcomes mean. In the background, they state that “an association between endometriosis and autoimmune diseases has been proposed”, so that is what they are studying. Then they detail how they are going to study it- what databases they are using to look for information, what they are going to include or exclude from their study, and the statistical analysis they will utilize. They next present the outcomes: “the studies quantified an association between endometriosis and several autoimmune diseases, including systemic lupus erythematosus (SLE), Sjögren’s syndrome (SS), rheumatoid arthritis (RA), autoimmune thyroid disorder, coeliac disease (CLD), multiple sclerosis (MS), inflammatory bowel disease (IBD), and Addison’s disease”. But wait! There is a caveat they note- “the quality of the evidence was generally poor due to the high risk of bias in the majority of the chosen study designs and statistical analyses” and that “only 5 of the 26 studies could provide high-quality evidence”. Then they present their conclusions of how this information might be useful- “the observed associations between endometriosis and autoimmune diseases suggest that clinicians need to be aware of the potential coexistence of endometriosis and autoimmune diseases when either is diagnosed”. They end by giving suggestions for future research that might strengthen the body of evidence for this. In short, after looking deeper into the association, the evidence available is overall poor so more research is warranted.
This is by no means a comprehensive review of looking at research study but rather a brief intro. There are many available resources on the internet for looking more in depth about how to assess research and draw conclusions from it.
References
Shigesi, N., Kvaskoff, M., Kirtley, S., Feng, Q., Fang, H., Knight, J. C., … & Becker, C. M. (2019). The association between endometriosis and autoimmune diseases: a systematic review and meta-analysis. Human reproduction update, 25(4), 486-503. Retrieved from https://academic.oup.com/humupd/article/25/4/486/5518352?login=true
Simundic, A. M. (2013). Bias in research. Biochemia medica, 23(1), 12-15. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3900086/
Statistics How To. (n.d.). Confounding Variable: Simple Definition and Example. Retrieved from https://www.statisticshowto.com/experimental-design/confounding-variable/
University of Alabama at Birmingham. (2021). Study Types- Definitions. Retrieved from https://guides.library.uab.edu/ebd/evidencestrength
The Aggravating Endometrioma
What are endometriomas anyway? Endometriosis is classified into three main types: superficial peritoneal endometriosis, deep infiltrating endometriosis, and endometriomas (see more about that here). Endometriomas are ovarian cysts lined by endometriotic tissue and can be filled with blood (why they are at times called “chocolate cysts”). Like the other types of endometriosis, no one knows for sure how they form. It has been theorized that endometriosis tissue on the surface of the ovary invades and forms a cyst like formation or they start as a functional ovarian cyst with gradual infiltration of endometriotic tissue. Endometriomas have been found in up to 44% of those with endometriosis and are associated with deep infiltrating endometriosis (Cranney, Condous, & Reid, 2017).
Endometriomas can be suspected with ultrasound or MRI, but as with other types of endometriosis, surgery is gold standard for diagnosis (Gałczyński et al., 2019). Endometrioma treatment can often be focused on the effect on fertility, so it is important to consider your goals when looking at treatment options. While medications are used to manage endometriomas, “endometriomas do not respond to medical therapy alone, thus usually surgical treatment is necessary” (Gałczyński et al., 2019). Many may be hesitant to perform surgery for fear of loss of healthy ovarian function and may put off surgery until the endometrioma reaches a certain size. However, Gałczyński et al. (2019) reports that treating “early-stage endometrioma provides less damage to the ovary by a less invasive surgical procedure which decreases the risk of iatrogenic premature ovarian failure” and that “long-term ovarian endometriosis leads to persistent inflammation” that can lead to loss of ovarian function. Skill of the surgeon is important in this aspect.
Gałczyński et al. (2019) reports that “the level of expertise in endometriotic surgery is inversely correlated with inadvertent removal of healthy ovarian tissue along with the endometrioma capsule”. There are multiple surgical techniques that can be used to treat endometriomas and there is no consensus on the best method, although ovarian cystectomy (removal of the ovarian cyst) is the preferred method based on studies (Pais et al., 2021). One recently published study cites “excisional surgery allows for pain resolution, a high rate of spontaneous pregnancies and a lower recurrence rate of ovarian cysts when compared to drainage and ablation techniques” (Angioni et al., 2021).
The aggravating thing about endometriomas is the likelihood of recurrence. It can hard to tell true recurrence rates from studies because “recurrence is variously defined in the literature as the relapse of pain, clinical or instrumental detection of an endometriotic lesion, repeat rise in CA 125 levels, or evidence of recurrence found during repeat surgery,” which results in the wide range of reported recurrence in studies (Ceccaroni et al., 2019). In addition, the method of surgical treatment has a bearing on recurrence rate (excision versus draining etc.). One study reported recurrence rates to be “24.2% for patients aged 20–30 years, 17.7% for 31–40 years, and 7.9% for 41–45 years” (Li et al., 2019). Other studies have echoed that younger age was linked to increased recurrence (Gałczyński et al., 2019). While younger age seems to have a direct correlation with recurrence, other factors not as much. For instance, Gałczyński et al. (2019) reports that the “diameter of the tumor, stage of endometriosis, coexistence of deep-infiltrating endometriosis, or uni- or bi-lateral involvement of ovaries were all not associated with the risk of recurrence” and that the “median time to recurrence was 53 months”.
There is also controversy about the use of hormonal suppression to prevent recurrence. Some studies and a meta-analysis report that there is not enough evidence for the use of medications to help prevent recurrence, while others indicate that it may delay but will not prevent recurrence (Gałczyński et al., 2019; Li et al., 2019; Wattanayingcharoenchai et al., 2021). Confusing? Others agree that it is- with one commentary stating that “so what are we to believe and what should we advise women affected by endometriosis to do?” (Saridogan, 2020). In the end, we each have to do our research, look at our individual goals, and decide what is best for our unique situation.
Endometriosis after a hysterectomy or menopause
References
Angioni, S., Scicchitano, F., Sigilli, M., Succu, A. G., Saponara, S., & D’Alterio, M. N. (2021). Impact of Endometrioma Surgery on Ovarian Reserve. In Endometriosis Pathogenesis, Clinical Impact and Management (pp. 73-81). Springer, Cham. Retrieved from https://link.springer.com/chapter/10.1007/978-3-030-57866-4_8
Ceccaroni, M., Bounous, V. E., Clarizia, R., Mautone, D., & Mabrouk, M. (2019). Recurrent endometriosis: a battle against an unknown enemy. The European Journal of Contraception & Reproductive Health Care, 24(6), 464-474. Retrieved from https://www.tandfonline.com/doi/abs/10.1080/13625187.2019.1662391
Cranney, R., Condous, G., & Reid, S. (2017). An update on the diagnosis, surgical management, and fertility outcomes for women with endometrioma. Acta obstetricia et gynecologica Scandinavica, 96(6), 633-643. Retrieved from https://obgyn.onlinelibrary.wiley.com/doi/full/10.1111/aogs.13114
Gałczyński, K., Jóźwik, M., Lewkowicz, D., Semczuk-Sikora, A., & Semczuk, A. (2019). Ovarian endometrioma–a possible finding in adolescent girls and young women: a mini-review. Journal of ovarian research, 12(1), 1-8. Retrieved from https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-019-0582-5
Li, X. Y., Chao, X. P., Leng, J. H., Zhang, W., Zhang, J. J., Dai, Y., … & Wu, Y. S. (2019). Risk factors for postoperative recurrence of ovarian endometriosis: long-term follow-up of 358 women. Journal of ovarian research, 12(1), 1-10. Retrieved from https://link.springer.com/article/10.1186/s13048-019-0552-y
Pais, A. S., Flagothier, C., Tebache, L., Almeida Santos, T., & Nisolle, M. (2021). Impact of Surgical Management of Endometrioma on AMH Levels and Pregnancy Rates: A Review of Recent Literature. Journal of Clinical Medicine, 10(3), 414. Retrieved from https://www.mdpi.com/2077-0383/10/3/414
Saridogan, E. (2020). Postoperative medical therapies for the prevention of endometrioma recurrence–do we now have the final answer?(Mini-commentary on BJOG-19-1705. R2). Authorea Preprints. Retrieved from https://d197for5662m48.cloudfront.net/documents/publicationstatus/41937/preprint_pdf/d4903f81caf3e8838e672d7631e6b8bd.pdf
Wattanayingcharoenchai, R., Rattanasiri, S., Charakorn, C., Attia, J., & Thakkinstian, A. (2021). Postoperative hormonal treatment for prevention of endometrioma recurrence after ovarian cystectomy: a systematic review and network meta‐analysis. BJOG: An International Journal of Obstetrics & Gynaecology, 128(1), 25-35. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32558987/

Celiac Disease and Endometriosis
Much like thyroid disease and endometriosis, there are not many studies looking at an association between celiac disease and endometriosis. One study found the “risk of endometriosis in patients with [celiac disease] was 112/100 000 person” (Stephansson et el., 2011). Another noted that celiac disease “is common in this population group [women with endometriosis and infertility] (2.5%) and may be clinically relevant” (Aguiar et al., 2009). Another study noted a slightly increased risk of celiac disease in those with endometriosis (“Celiac disease was diagnosed in 5 of 223 women with endometriosis and in 2 of 246 controls (2.2% versus 0.8%)”) (Seracchiolo et al., 2014). Some have had positive results on endometriosis symptoms from following a gluten free diet (Marziali et al., 2012).
On the flip side, celiac disease can present with symptoms similar to endometriosis. “Celiac disease has also been associated with chronic pelvic pain, including dysmenorrhea and deep dyspareunia” and “patients with atypical pelvic pain, particularly with GI components, may also benefit from screening” (Ory & Christie, 2013). This points out the importance of looking beyond the diagnosis of endometriosis with recurring symptoms in order to rule out other health issues that can mimic endometriosis symptoms.
References
Aguiar, F. M., Melo, S. B., Galvao, L. C., Rosa-e-Silva, J. C., dos Reis, R. M., & Ferriani, R. A. (2009). Serological testing for celiac disease in women with endometriosis. A pilot study. Clinical and experimental obstetrics & gynecology, 36(1), 23-25. Retrieved from https://pubmed.ncbi.nlm.nih.gov/19400413/
Marziali, M., Venza, M., Lazzaro, S., Lazzaro, A., Micossi, C., & Stolfi, V. M. (2012). Gluten-free diet: a new strategy for management of painful endometriosis related symptoms. Minerva Chir, 67(6), 499-504. Retrieved from https://www.minervamedica.it/en/journals/minerva-surgery/article.php?cod=R06Y2012N06A0499
Ory, S. J., & Christie, D. R. (2013). Reproductive effects of celiac disease. Contemporary OB/GYN, 58(4), 34. Retrieved from https://www.contemporaryobgyn.net/view/reproductive-effects-celiac-disease
Seracchioli, R., Montanari, G., Mabrouk, M., & Nassif, J. (2014). Endometriosis: novel models, diagnosis, and treatment. Retrieved from https://doi.org/10.1155/2014/236821
Stephansson, O., Falconer, H., & Ludvigsson, J. F. (2011). Risk of endometriosis in 11 000 women with celiac disease. Human reproduction, 26(10), 2896-2901. Retrieved from https://doi.org/10.1093/humrep/der263

Keep Endometriosis Awareness Going
As we come to the end of endometriosis awareness month, those of us with endometriosis knows it doesn’t end in March. Raising awareness and fighting against misinformation is a constant effort. Please feel free to share links from the webpage. The more we share, the more awareness and up-to-date information is out there for others. It can be discouraging to see so much of the same old misinformation perpetuated that can cause others to suffer as we have. Let’s spread hope!
We have collected all the infographs shared on Nancy’s Nook Facebook page and have sprinkled them throughout the website so that you can share the infograph and the link to more information. All the infographs are also collected here.
Endometriosis Quick Facts to Share is also another good resource to share. One of my favorites to reference to is the Myths and Misinformation page. Keep the awareness going, because endometriosis doesn’t stop in March.






The Personal Burden of Endometriosis
Last week we looked at the direct financial burden of endometriosis, including the loss of education, loss of productivity at work and home, and loss of income. Today we look at the personal burden of endometriosis- the altered relationships with family and friends, the pain and suffering, the ill effects on mental health, and the loss of who we feel we are as a person because of it.
Pain and fatigue can limit our ability to function and the quality of our life experience (Missmer et al., 2021). Our ability to maintain relationships can be difficult, especially when others do not understand the impact that endometriosis has on us. Much research has shown the effect on intimate partner relationships due to the interference with sexual health (Missmer et al., 2021). Not as many studies have been done on the effects of parenting with endometriosis; however, in our Facebook group Nancy’s Nook, many of you have shared the significant effect endometriosis has had on the ability to function as a parent. These limitations imposed from our illness can affect our mental health as well.
In studies, people with endometriosis express “feelings of worthlessness, guilt, and frustration connected with disease-related limitations on participation in daily activities, social functioning, independence, and interpersonal relationships” as well as frustration “from a woman’s inability to manage or predict her pain and the feeling that endometriosis/endometriosis-associated pain controls her life” (Missmer et al., 2021). Add to this the burden of the “perception that others (even healthcare professionals) consider what they are experiencing to be ‘all in their heads’” (Missmer et al., 2021). The struggle is real. And it is no wonder that many feel a loss of who they are as a person because of it.
On a positive note, a systematic review and meta-analysis, as well as other studies, reveal that surgery for endometriosis does improve quality of life (Arcoverde et al., 2019; Parra et al., 2021). Another study reports that “laparoscopic surgery is associated with improved quality of life and emotional well-being compared to medical therapies” and cautions that “although the GnRH agonists are effective in reducing endometriosis symptoms, they are often associated with anxiety and depression during treatment” (Laganà et al., 2017). To help manage symptoms, one study that surveyed people with endometriosis found that “heat (70%), rest (68%), and meditation or breathing exercises (47%)” helped and to a lesser degree “yoga/Pilates, stretching, and exercise” (Armour et al., 2019). Changes in diet, individualized to your specific needs, can help with symptom management for some (Karlsson, Patel, & Premberg, 2020). Other things such as acupuncture have been helpful to some as well. Mental healthcare is important to our well-being and should not be neglected either.
The impact endometriosis has on our lives is significant. Know that you are not alone.

References
Arcoverde, F. V. L., de Paula Andres, M., Borrelli, G. M., de Almeida Barbosa, P., Abrão, M. S., & Kho, R. M. (2019). Surgery for endometriosis improves major domains of quality of life: a systematic review and meta-analysis. Journal of minimally invasive gynecology, 26(2), 266-278. Retrieved from https://doi.org/10.1016/j.jmig.2018.09.774
Armour, M., Sinclair, J., Chalmers, K. J., & Smith, C. A. (2019). Self-management strategies amongst Australian women with endometriosis: a national online survey. BMC complementary and alternative medicine, 19(1), 1-8. Retrieved from https://link.springer.com/article/10.1186/s12906-019-2431-x
Karlsson, J. V., Patel, H., & Premberg, A. (2020). Experiences of health after dietary changes in endometriosis: a qualitative interview study. BMJ open, 10(2), e032321. Retrieved from https://bmjopen.bmj.com/content/10/2/e032321.abstract
Laganà, A. S., La Rosa, V. L., Rapisarda, A. M. C., Valenti, G., Sapia, F., Chiofalo, B., … & Vitale, S. G. (2017). Anxiety and depression in patients with endometriosis: impact and management challenges. International journal of women’s health, 9, 323. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5440042/
Missmer, S. A., Tu, F. F., Agarwal, S. K., Chapron, C., Soliman, A. M., Chiuve, S., … & As-Sanie, S. (2021). Impact of Endometriosis on Life-Course Potential: A Narrative Review. International Journal of General Medicine, 14, 9. doi: 10.2147/IJGM.S261139
Parra, R. S., Feitosa, M. R., Camargo, H. P. D., Valério, F. P., Zanardi, J. V. C., Rocha, J. J. R. D., & Féres, O. (2021). The impact of laparoscopic surgery on the symptoms and wellbeing of patients with deep infiltrating endometriosis and bowel involvement. Journal of Psychosomatic Obstetrics & Gynecology, 42(1), 75-80. Retrieved from https://doi.org/10.1080/0167482X.2020.1773785

The Costly Burden of Endometriosis
Endometriosis has a powerful cost in terms of quality of life. However, there are financial costs as well. Financial loss can come from direct healthcare costs as well as loss of productivity. The estimated annual cost between those two in 2009 was $69.4 billion (Della Corte et al., 2020).
Della Corte et al. (2020) notes that “in employed women with endometriosis, as a consequence of productivity loss of 6.3 h per week, the total loss per person is approximately $10,177.54 per year.” Chronic pain is a significant factor in the loss of productivity and Armour et al. (2019) concludes that “priority should be given to improving pain control in women with pelvic pain.” Similarly, Facchin et al. (2019) notes that those with greater severity of symptoms were less likely to be employed and state that “endometriosis symptoms may significantly affect women’s professional life, with important socioeconomic, legal, and political implications.” The loss of productivity doesn’t only affect the workplace. Soliman et al. (2017) found that there was loss of household productivity as well.
The loss of productivity can start with symptom onset, starting in adolescence. Missmer et al. (2021) state that “endometriosis (and its associated symptoms) has been shown to hamper educational attainment, hinder work productivity, alter career choices and success, impair social life and activities, affect family choices, induce strain in personal relationships, negatively influence mental and emotional health, and adversely affect [quality of life]. These multiple and pervasive effects are anticipated to materially alter the life-course trajectory of women with endometriosis.”
So how can we help this? Earlier diagnosis and successful treatment are key. Surrey et al. (2020) notes that “patients with endometriosis who had longer diagnostic delays had more pre-diagnosis endometriosis-related symptoms and higher pre-diagnosis healthcare utilization and costs compared with patients who were diagnosed earlier after symptom onset, providing evidence in support of earlier diagnosis.” On the same note, Missmer et al. (2021) state that “unfortunately, current practice models too often result in a prolonged delay between symptom onset, diagnosis, and treatment of endometriosis, thereby increasing the impact on the life course.” This is why we advocate and share evidence-based information- so that the next person doesn’t have their life so significantly altered by endometriosis.
References
Armour, M., Lawson, K., Wood, A., Smith, C. A., & Abbott, J. (2019). The cost of illness and economic burden of endometriosis and chronic pelvic pain in Australia: A national online survey. PloS one, 14(10), e0223316. Retrieved from https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0223316
Della Corte, L., Di Filippo, C., Gabrielli, O., Reppuccia, S., La Rosa, V. L., Ragusa, R., … & Giampaolino, P. (2020). The burden of endometriosis on women’s lifespan: a narrative overview on quality of life and psychosocial wellbeing. International Journal of Environmental Research and Public Health, 17(13), 4683. Retrieved from https://www.mdpi.com/1660-4601/17/13/4683/htm
Facchin, F., Buggio, L., Ottolini, F., Barbara, G., Saita, E., & Vercellini, P. (2019). Preliminary insights on the relation between endometriosis, pelvic pain, and employment. Gynecologic and obstetric investigation, 84(2), 190-195. Retrieved from https://doi.org/10.1159/000494254
Missmer, S. A., Tu, F. F., Agarwal, S. K., Chapron, C., Soliman, A. M., Chiuve, S., … & As-Sanie, S. (2021). Impact of Endometriosis on Life-Course Potential: A Narrative Review. International Journal of General Medicine, 14, 9. doi: 10.2147/IJGM.S261139
Soliman, A. M., Coyne, K. S., Gries, K. S., Castelli-Haley, J., Snabes, M. C., & Surrey, E. S. (2017). The effect of endometriosis symptoms on absenteeism and presenteeism in the workplace and at home. Journal of managed care & specialty pharmacy, 23(7), 745-754. Retrieved from https://doi.org/10.18553/jmcp.2017.23.7.745
Surrey, E., Soliman, A. M., Trenz, H., Blauer-Peterson, C., & Sluis, A. (2020). Impact of endometriosis diagnostic delays on healthcare resource utilization and costs. Advances in therapy, 37(3), 1087-1099. Retrieved from https://link.springer.com/article/10.1007/s12325-019-01215-x
Endometriosis Quick Facts to Share
What is endometriosis?
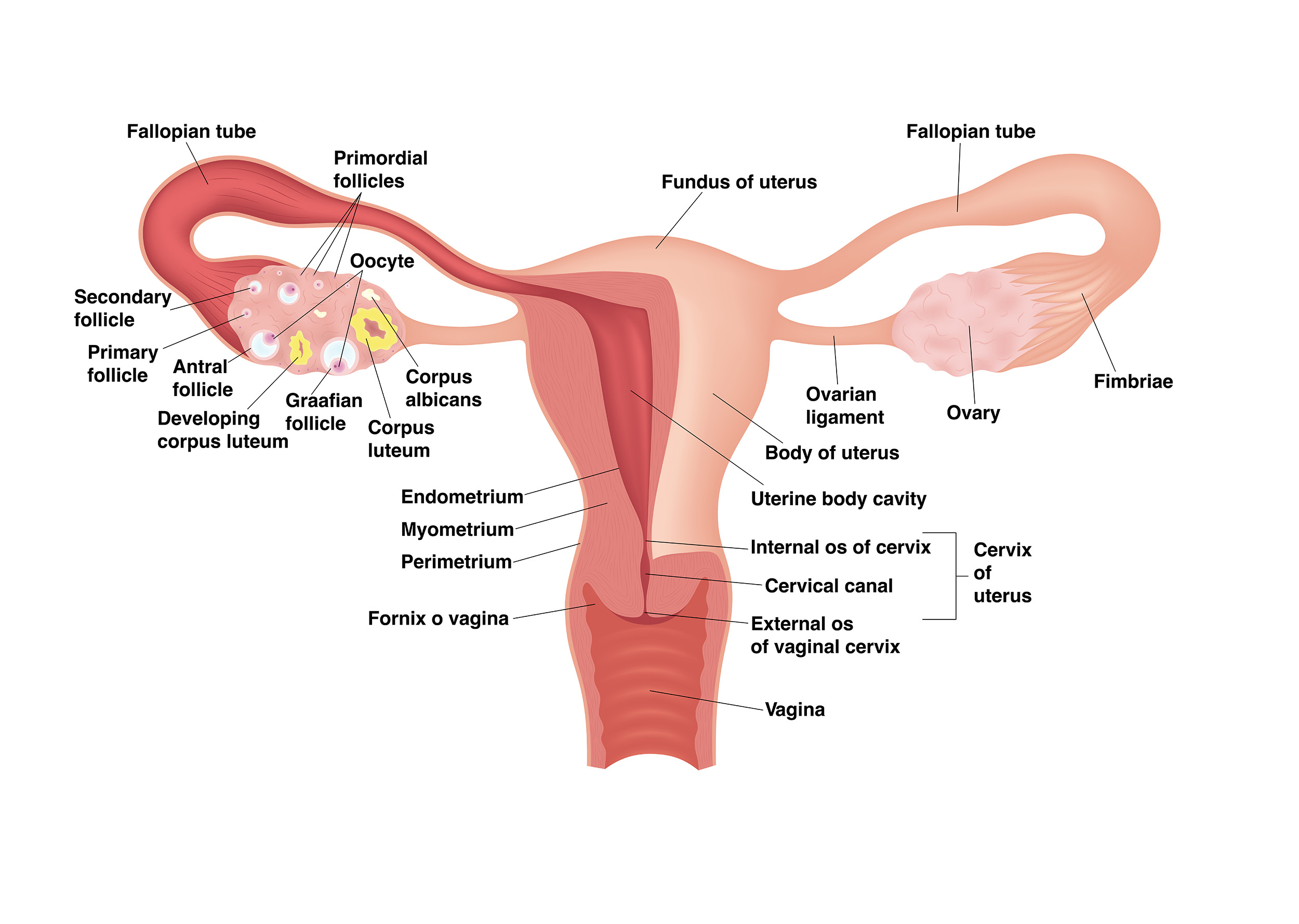
Endometriosis is an inflammatory disorder where lesions similar to the lining of the uterus are located outside of the uterus. Endometriosis lesions have distinct differences from the lining of the uterus in both their form and function. The lesions release proinflammatory chemicals, can produce estrogen, can grow their own nerves and blood vessels, and can cause adhesions. It is usually located in the pelvis but has been found in other areas throughout the body. An estimated 11% of people assigned female at birth (including teenagers)have endometriosis- although it has been found in men on rare occasion.
What causes it?
No one knows. There is a genetic component, with higher rates seen in those with close relatives having endometriosis. It has been found in fetuses, suggesting it is present before birth.
What are its symptoms?
Endometriosis has many symptoms- from chronic pelvic pain to fatigue to infertility. Symptom severity does not necessarily correlate with the extent of lesions.
- Pain: chronic pelvic pain, pain with menses, pain in between menses, pain with exercise, pain with sex, pain with bowel movements, pain with urination, low back pain
- Fatigue
- Bowel symptoms similar to irritable bowel syndrome such as constipation, diarrhea, and bloating
- Infertility
- And many others
How is diagnosed?
Endometriosis is diagnosed with surgery, preferably with pathology from tissue samples. Some imaging, such as MRI’s and ultrasounds, can rule in endometriosis, but they cannot rule it out. The accuracy of diagnosis depends on the knowledge and skill of the provider.
How is it treated?
While there is no definitive cure for endometriosis, excision surgery where all lesions are removed is recommended. The skill and knowledge of the surgeon is paramount in the ability to recognize and remove all lesions. Hormonal medication might help temporarily with symptom management, but it cannot be used to diagnosis, cure (“clean up”), or prevent the progression of endometriosis. Endometriosis can persist after a hysterectomy or menopause. Endometriosis is often present with other painful conditions such as adenomyosis and interstitial cystitis.
For more information see: nancysnookendo.com
Reaching Out To Teach Another: nancysnookendo.com/support-us/


