
Top Endometriosis Specialist Florida: Your Path to Pain-Free Living
Endometriosis affects approximately 10% of women in Florida, impacting their daily lives and overall well-being. This chronic condition, characterized by the growth of uterine-like tissue outside the uterus, can cause debilitating pain, fertility issues, and a range of other symptoms. For those living in the Sunshine State, an endometriosis specialist is crucial to managing this complex disorder effectively. The persistent pelvic pain, heavy menstrual bleeding, and fatigue associated with the condition can significantly hinder one’s ability to enjoy the state’s beautiful beaches, outdoor activities, and vibrant social scene. Patients can benefit from personalized care plans tailored to their unique needs and lifestyles by choosing an endometriosis specialist in Florida.
As we delve deeper into the world of endometriosis care in Florida, we’ll explore the importance of specialized treatment, highlight top experts in the field, and discuss the various options available to those seeking relief from this challenging condition. Whether you’re newly diagnosed or have been struggling with endometriosis for years, this comprehensive guide will empower you to take control of your health and find your path to pain-free living in the Sunshine State.
Understanding Endometriosis: More Than Just a Sunshine State Struggle
Endometriosis is a complex gynecological condition that affects women worldwide, including those living in Florida. To fully appreciate the importance of seeking specialized care, it’s crucial to understand the intricacies of this disorder and how it impacts the lives of patients.
Decoding the Complexities of Endometriosis
Endometriosis occurs when tissue similar to the lining of the uterus grows outside the uterine cavity. This misplaced tissue can be found on various organs, including the ovaries, fallopian tubes, bladder, and even the intestines. Despite being outside the uterus, this tissue continues to respond to hormonal changes throughout the menstrual cycle, leading to inflammation, pain, and the formation of scar tissue.
The exact cause of endometriosis remains unknown, but several factors may contribute to its development, including:
- Retrograde menstruation
- Genetic predisposition
- Immune system dysfunction
- Environmental factors
Understanding these potential causes is essential for developing effective treatment strategies and managing the condition long-term.
How Endometriosis Affects Floridians’ Active Lifestyles
Florida’s warm climate and abundance of outdoor activities make it an ideal place for an active lifestyle. However, for women with endometriosis, the state’s unique environment can present additional challenges:
- Heat sensitivity: Florida’s hot and humid weather can exacerbate pelvic pain and inflammation associated with endometriosis.
- Beach activities: Swimming and sunbathing, popular pastimes in Florida, may be uncomfortable or even painful for those with severe pelvic pain or bloating.
- Outdoor sports: Engaging in high-impact activities like running or tennis can be challenging due to pelvic discomfort and fatigue.
- Social events: Florida’s vibrant social scene may be difficult to enjoy fully when dealing with unpredictable pain and fatigue.
- Work-life balance: The state’s tourism and service industries often require long hours and physical stamina, which can be taxing for those managing endometriosis symptoms.
Recognizing the Signs of Endometriosis: A Comprehensive Symptom Checklist
Recognizing endometriosis can be difficult due to its wide range of symptoms. To help, here’s a comprehensive checklist of common endometriosis symptoms to watch for:
- Severe menstrual cramps
- Chronic pelvic pain
- Pain during or after sexual intercourse
- Heavy or irregular menstrual bleeding
- Painful bowel movements or urination, especially during menstruation
- Lower back pain
- Abdominal bloating
- Fatigue
- Nausea or vomiting
- Infertility or difficulty conceiving
- Diarrhea or constipation
- Mood swings or depression
- Leg pain
- Painful ovulation
- Chest pain or shortness of breath (in rare cases of thoracic endometriosis)
- Painful urination
It’s important to note that experiencing one or more of these symptoms doesn’t necessarily mean you have endometriosis. However, if you’re concerned about your symptoms, consulting with an endometriosis specialist in Florida can help you receive an accurate diagnosis and appropriate treatment plan.
The Florida Advantage: Cutting-Edge Endo Care Close to Home
Florida offers its residents and visitors a unique advantage regarding endometriosis care. The Sunshine State has become a hub for advanced medical treatments and research, providing women with access to top-tier care without requiring extensive travel. This section explores the benefits of seeking endometriosis treatment in Florida and highlights the state’s commitment to medical excellence in this field.
Access to Top-Tier Treatments and Research
Florida’s medical landscape is characterized by its commitment to innovation and cutting-edge treatments. For women with endometriosis, this translates to:
- Advanced Diagnostic Techniques: Florida’s leading medical centers utilize state-of-the-art imaging technologies, such as high-resolution ultrasounds and MRI scans, to accurately diagnose and stage endometriosis.
- Minimally Invasive Surgical Options: Some Florida specialists are trained in advanced laparoscopic and robotic surgical techniques, offering patients less invasive treatment options with shorter recovery times.
- Participation in Clinical Trials: Several Florida medical institutions actively participate in endometriosis research, allowing patients to access experimental treatments and contribute to scientific advancements.
- Multidisciplinary Approach: Some of Florida’s experts employ a team-based approach, bringing together gynecologists, general surgeons, urologists, pain specialists, fertility experts, and other relevant professionals to provide comprehensive care.
- Fertility Preservation Options: For women concerned about their future fertility, Florida offers advanced reproductive technologies and fertility preservation techniques alongside endometriosis treatment.
Top Endometriosis Specialists in Florida: Experts You Can Trust
Florida is home to some highly skilled and best endometriosis specialists dedicated to providing exceptional care for women struggling with this complex condition. These experts combine their extensive knowledge with cutting-edge techniques to offer personalized treatment plans that address each patient’s unique needs. In this section, we’ll highlight some of the leading endometriosis specialists in Florida and explore their areas of expertise.
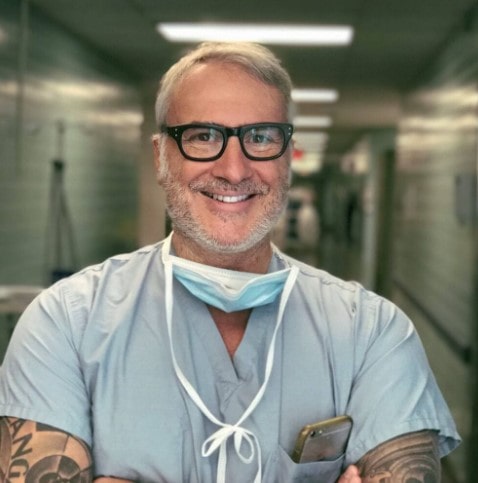
Dr. Andrea Vidali is a renowned endometriosis specialist in Miami, Florida, and New York. With over two decades of experience in reproductive endocrinology and infertility, Dr. Vidali has gained international recognition for his expertise in minimally invasive surgical techniques for endometriosis treatment.
Key areas of expertise:
- Advanced excision surgery
- Fertility preservation in endometriosis patients
- Immunological aspects of endometriosis
- Robotic-assisted endometriosis surgery
Dr. Vidali’s approach focuses on thorough diagnosis and comprehensive treatment plans that address both pain management and fertility concerns. His patients benefit from his extensive experience in complex cases and his commitment to staying at the forefront of endometriosis research and treatment innovations.
Dr. Gaby Moawad is a highly respected gynecologist and endometriosis specialist in Orlando, Florida. Known for his patient-centered approach, he combines surgical expertise with a deep understanding of the holistic needs of women with endometriosis.

Areas of specialization:
- Laparoscopic and robotic excision of endometriosis
- Management of chronic pelvic pain
- Fertility-sparing endometriosis treatments
- Multidisciplinary approach to endometriosis care
Dr. Moawad’s practice emphasizes comprehensive care, addressing not only the physical symptoms of endometriosis but also the emotional and psychological aspects of living with a chronic condition. His patients appreciate his compassionate approach and dedication to improving their quality of life.
Finding the right endometriosis specialist in Florida takes time and research. Consultations offer a chance to discuss your case and assess the fit. Choosing the best specialist is key to managing your condition and improving your quality of life, as these experts understand the unique challenges women with endometriosis face in Florida.
Treatment Options: As Diverse as Florida’s Landscape
Just as Florida boasts a diverse landscape of beaches, swamps, and citrus groves, the treatment options for endometriosis in the state are equally varied and comprehensive. Florida’s endometriosis specialists offer a wide range of advanced surgical techniques, non-invasive therapies, and holistic approaches to address the complex needs of patients with this challenging condition. This section explores the diverse treatment landscape available to women seeking endometriosis care in Florida.
Advanced Surgical Techniques Available in Florida
Surgical intervention remains a cornerstone of endometriosis treatment, especially for severe cases or when conservative measures have failed. Florida’s top endometriosis specialists are skilled in various advanced surgical techniques:
- Laparoscopic Excision Surgery:
- A minimally invasive approach using small incisions
- Allows for thorough removal of endometrial implants
- Reduced scarring and faster recovery compared to open surgery
- Often considered the gold standard for endometriosis treatment
- Robotic-Assisted Surgery:
- Utilizes advanced robotic technology for enhanced precision
- Offers 3D visualization and improved dexterity for complex procedures
- Particularly useful for deep-infiltrating endometriosis
- Fertility-Preserving Surgery:
- Focuses on removing endometriosis while preserving reproductive organs
- Often combined with fertility treatments for women trying to conceive
- Presacral Neurectomy:
- Targets nerve pathways to alleviate chronic pelvic pain
- It can be performed alongside excision surgery for comprehensive treatment
- Hysterectomy with Bilateral Salpingo-Oophorectomy:
- Reserved for severe cases or when other treatments have failed
- Involves the removal of the uterus, fallopian tubes, and ovaries
- Considered a last resort due to its impact on fertility and hormonal balance
Non-Invasive Therapies and Holistic Approaches
Florida’s endometriosis specialists recognize the importance of non-surgical interventions and holistic care in managing the condition. Some common non-invasive therapies include:
- Hormonal Treatments:
- Birth control pills
- Progestin-only medications
- GnRH agonists and antagonists
- Aromatase inhibitors
- Pain Management Techniques:
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Nerve blocks
- Transcutaneous electrical nerve stimulation (TENS)
- Physical Therapy:
- Pelvic floor therapy
- Manual therapy techniques
- Exercise programs tailored for endometriosis patients
- Nutritional Counseling:
- Anti-inflammatory diets
- Elimination diets to identify food sensitivities
- Supplementation strategies
- Complementary Therapies:
- Acupuncture
- Yoga and mindfulness practices
- Herbal medicine under professional guidance
- Psychological Support:
- Cognitive-behavioral therapy
- Support groups
- Stress management techniques
Choosing the Right Treatment Plan
When considering endometriosis treatment options in Florida, working closely with your specialist to develop a personalized plan is essential. Factors to consider include:
- Severity and location of endometriosis lesions
- Primary symptoms and their impact on quality of life
- Fertility goals and reproductive health concerns
- Overall health and any coexisting conditions
- Personal preferences and lifestyle considerations
Florida endometriosis specialists offer comprehensive care through a multimodal approach. They combine surgery with noninvasive therapies to address physical and emotional symptoms. With diverse treatment options—from advanced surgery to holistic therapies—patients can access personalized care for effective management and improved quality of life.
Living with Endometriosis in Florida: Beyond Medical Care
Managing endometriosis extends far beyond the doctor’s office or operating room. For those living with this condition in Florida, finding ways to cope with symptoms and maintain a high quality of life is crucial. The Sunshine State’s unique environment and lifestyle offer challenges and opportunities for those navigating life with endometriosis. This section explores strategies for managing symptoms in Florida’s climate and lifestyle and the supportive therapies and resources available to endometriosis patients in the state.
Adapting to Florida’s Climate and Lifestyle
Florida’s warm, humid climate and active lifestyle can present unique challenges for women with endometriosis. Here are some strategies to help manage symptoms while enjoying all that the state has to offer:
- Heat Management:
- Use cooling products like portable fans or cooling towels when outdoors
- Plan outdoor activities for cooler parts of the day
- Stay hydrated to help regulate body temperature
- Beach-Friendly Strategies:
- Invest in comfortable, supportive swimwear
- Use beach umbrellas or tents for shade and privacy
- Bring a supportive cushion or beach chair for comfort
- Exercise Adaptations:
- Opt for low-impact activities like swimming or yoga
- Try water aerobics or beach walks for gentle exercise
- Listen to your body and pace yourself during physical activities
- Workplace Accommodations:
- Use ergonomic furniture to reduce pelvic strain
- Take regular breaks to stretch and move
- Communicate with employers about flexible work arrangements if needed
- Social Life Adjustments:
- Plan activities with built-in rest periods
- Choose venues with comfortable seating options
- Be open with friends about your needs and limitations
Supportive Therapies for Endometriosis Management
Florida offers many supportive therapies that can complement medical treatments and help manage endometriosis symptoms.
- Acupuncture:
- It may help reduce pain and inflammation
- It can be particularly beneficial for menstrual cramps and chronic pelvic pain
- Massage Therapy:
- It helps relax tense muscles and reduce overall body pain
- It may improve circulation and reduce stress
- Yoga and Pilates:
- Gentle stretching can help alleviate pelvic pain
- Mindfulness aspects can aid in stress reduction
- Nutritional Counseling:
- Guidance on anti-inflammatory diets
- Help in identifying and managing food sensitivities
- Pelvic Floor Physical Therapy:
- Addresses muscle tension and dysfunction in the pelvic area
- Can improve pain during intercourse and bladder/bowel symptoms
- Mindfulness and Meditation:
- Techniques for managing pain and reducing stress
- Can improve overall emotional well-being
Community Resources and Support Groups
Florida offers numerous resources and support groups for women living with endometriosis:
- Endometriosis Association of Florida:
- Provides education and support for patients and families
- Organizes regular meetups and events across the state
- Online Support Communities:
- Florida-specific Facebook groups and forums
- Virtual support meetings for those unable to attend in-person events
- Fertility Support Networks:
- Resources for women dealing with endometriosis-related infertility
- Connections to fertility specialists and treatment options in Florida
- Workplace Advocacy Groups:
- Organizations that help women navigate workplace challenges related to chronic illness
- Resources for understanding employment rights and accommodations
Lifestyle Modifications for Symptom Management
In addition to medical treatments and supportive therapies, certain lifestyle modifications can help manage endometriosis symptoms:
- Stress Reduction Techniques:
- Regular meditation or deep breathing exercises
- Engaging in hobbies or activities that promote relaxation
- Sleep Hygiene:
- Establishing a consistent sleep schedule
- Creating a comfortable sleep environment
- Dietary Adjustments:
- Keeping a food diary to identify trigger foods
- Incorporating anti-inflammatory foods into the diet
- Exercise Routine:
- Finding a balance between rest and gentle activity
- Incorporating low-impact exercises like swimming or cycling
- Emotional Well-being:
- Seeking counseling or therapy to address the emotional impact of living with a chronic condition
- Practicing self-compassion and setting realistic expectations
By using Florida’s resources and strategies, women with endometriosis can manage symptoms and maintain a fulfilling lifestyle. Remember, it’s a journey—be patient and celebrate small victories.
Conclusion: Empowering Your Endo Journey in the Sunshine State
As we conclude our exploration of endometriosis care in Florida, it’s clear that the Sunshine State offers a wealth of resources, expertise, and support for women navigating this challenging condition. From world-class specialists to cutting-edge treatments and supportive communities, Florida provides a comprehensive ecosystem for endometriosis management. We encourage you to take the next step in your endometriosis care journey. Whether that means scheduling a consultation with a specialist, exploring new treatment options, or connecting with a local support group, every action you take is a step towards better health and well-being.
Remember, your health journey is unique, and finding the right care may take time. Be patient with yourself, advocate for your needs, and don’t hesitate to seek second opinions or explore different treatment options. With perseverance and the right support, you can navigate the challenges of endometriosis and embrace all that life in Florida has to offer.
Here’s to your health, well-being, and a brighter, pain-free future in the Sunshine State!
REFERENCES:
https://ufhealth.org/conditions-and-treatments/endometriosis
https://www.medicalnewstoday.com/provider-near-me/condition-or-procedure/endometriosis/fl-florida
https://www.acibademhealthpoint.com/endometriosis-specialist-in-miami-expert-care
https://health.usf.edu/care/obgyn/services-specialties/endometriosis

Endometriosis in College: How to Take Care of Yourself When Life Doesn’t Pause
College is challenging enough when you’re healthy – throw endometriosis into the mix, and it can feel downright impossible some days. Classes, exams, and the whirlwind of social life don’t slow down just because you’re curled up in pain or fighting the crushing fatigue that comes with a flare-up.
But here’s the thing: you don’t have to do this alone, and you don’t have to choose between your health and your education. With the right strategies (and a little grace for yourself), you can navigate college life and even thrive. Let’s talk about how.
What Is Endometriosis? It’s More Than “Just Period Pain.”
Endometriosis isn’t something you “push through.” It’s a medical condition where tissue similar to the uterine lining grows where it doesn’t belong – on your ovaries, fallopian tubes, or other parts of your pelvis. This rogue tissue causes pain, inflammation, and sometimes fatigue so heavy it feels like you’re dragging a truck behind you.
For college students, the symptoms can make everything harder – from getting out of bed for a morning class to finding energy to finish assignments. The key to surviving (and thriving) is recognizing your limits and being intentional about how you take care of yourself.
How to Balance Endometriosis and College Life
- Be Your Own Biggest Advocate
No one knows your body better than you do. If you need extra time on assignments or flexibility with attendance, don’t hesitate to speak up. Colleges have disability services for a reason – use them. You’re not asking for favors; you’re getting what you need to succeed. - Plan Around Your Energy, Not Against It
You don’t have to be a superhero. If mornings leave you drained, schedule your classes for later in the day. Block off downtime in your calendar like you would a class. Rest is just as important as studying – maybe even more so. - Build a Self-Care Toolkit
Think of self-care as your secret weapon. Maybe it’s a heating pad for bad cramps, a playlist of calming music, or a few yoga stretches that actually feel good. The point isn’t to “fix” everything but to give yourself moments of comfort when you need them. - Don’t Let Food Be an Afterthought
When you’re busy (or exhausted), it’s tempting to grab whatever’s easiest. But fueling your body with anti-inflammatory foods – like leafy greens, salmon, or nuts – can make a difference in how you feel. And yes, chocolate is allowed. - Learn to Say No
Not every party or event is worth draining your already limited energy. Saying no doesn’t make you boring or antisocial – it makes you smart. Save your energy for the things (and people) that truly matter to you.
What Happens When It’s All Too Much?
Let’s be honest: some days, it’s all just too much. The pain, the deadlines, the constant juggling act – it can feel like you’re drowning.
Here’s the truth: you don’t have to do everything. When the weight of schoolwork gets overwhelming, it’s okay to hand off some of that burden. Services like pay someone to do your homework exist for a reason – to give you time to breathe, heal, and focus on what matters most.
Imagine handing over that impossible assignment and taking the evening to rest or catch up on lecture notes without the stress of yet another deadline. That’s not cheating; it’s surviving smart.
Why Self-Care Is More Than Bubble Baths
Self-care gets a bad rap as something indulgent, but let’s set the record straight: self-care is survival. It’s doing what you need to feel human again, whether that’s asking for an extension, eating ice cream for dinner, or saying no to plans because you need a night in bed with Netflix.
You’re not lazy for resting. You’re not weak for asking for help. You’re taking care of the most important tool you have: your body.
Give Yourself Permission to Ask for Help
Endometriosis is hard. College is hard. Doing both at once? It’s a lot. But you’re not alone, and you’re not failing if you need a little help along the way.
When life feels overwhelming, take a step back. Prioritize your health. Delegate when you need to. And remember: balance your college life and health effortlessly – pay for homework help today!
You’ve got this, even if it doesn’t feel like it every day. Keep going. You’re stronger than you think.

Pablo Picasso’s Advice For Video Vetting Of Endometriosis Surgeons
Table of contents
- Understanding Endometriosis Patients: Challenges and Behaviors
- Building Trust Through Video Vetting in Endometriosis Care
- What is the Video Vetting Process for Endometriosis Surgeon Verification?
- Why Video Vetting is Important for Endometriosis Surgeons
- Steps to Go Through Video Vetting Process as an Endometriosis Surgeon
- Challenges and Solutions in Video Vetting for Surgeons
- Video Vetting as a Vital Tool for Building Patient Relationships
No one can argue that a surgeon’s skills significantly impact a patient’s surgical outcome. However, the challenge has always been finding a method to assess a surgeon’s skills. To answer this question, we combined evidence and common sense. It is common sense that when you plan to evaluate a performance, you watch it. Think of the Olympic gymnastics competition. The athlete performs, and a group of experts scores her on a scale of one to ten.
How can we apply a similar method to endometriosis surgery to assess surgeons’ skills? To answer this study, a group of researchers published an article in the New England Journal of Medicine with an interesting solution. They showed that if a group of experts anonymously rates surgeons’ skills based on their surgical videos, the scores significantly correlate with fewer long-term complications. So the vetting idea was out there, and someone needed to be a great artist and follow Pablo Picasso’s advice: “Good artists copy; great artists steal.”
Understanding Endometriosis Patients: Challenges and Behaviors
The list of shortcomings in endometriosis care is prolonged. The long delays in diagnosis and treatments, failed treatments and surgeries, traumas, gaslighting, and many other issues exist. However, if there is one thing that has minimized the challenges, it is working with the right endometriosis expert early in the treatment journey. In today’s digital age, innovative methods are being introduced to enhance patients’ knowledge and access to high-quality care. However, it is not easy for a patient to know the surgical skills of a surgeon when they plan to do surgeries. They typically use proxy methods such as reviewing Instagram channels and Google reviews, talking to other patients, and looking at advocacy groups. They use these proxies to validate a surgeon’s skills, and we all know how easy it is to game the system and manipulate the outcomes of these proxies. For example, hundreds of tools and companies exist to help surgeons look good on Google Reviews, regardless of their true outcome and skills. Advocacy groups recommend doctors primarily based on their personal relationships, and they do not vet surgeons. So, patients can not confidently trust these resources and are looking for new resources.
Building Trust Through Video Vetting in Endometriosis Care
In endometriosis care, where patient trust is key, video vetting is a helpful way to build confidence and openness. This innovative approach not only showcases a surgeon’s expertise but also helps patients make more informed decisions about their care. The video vetting process offers a transparent and comprehensive means of assessing a doctor’s skills and expertise. By the end of this article, you’ll understand what video vetting is, why it’s significant for specialized fields like endometriosis surgery, and how it’s changing patients’ behaviors in finding their surgeons.
What is the Video Vetting Process for Endometriosis Surgeon Verification?
The video vetting process for endometriosis surgeon verification is a comprehensive and specialized approach designed to assess and validate surgeons’ skills. This process goes beyond traditional credentialing methods, offering a more nuanced and accurate evaluation of a surgeon’s capabilities.
Submission of Surgical Videos
The process begins with surgeons submitting videos of their endometriosis surgeries. These videos typically showcase procedures demonstrating the surgeon’s ability to handle stage II or higher endometriosis cases. Key areas of focus often include:

- Management of deep endometriosis
- Pelvic wall dissection techniques
- Endometrioma removal procedures
- Specialized areas such as diaphragm, bowel, or ureter for higher designation
Accompanying Documentation
Surgeons are required to submit corresponding operative and pathology reports along with the surgical videos. These documents provide crucial context to the procedures shown in the videos, offering insights into the surgeons’ decision-making process and the outcomes of their interventions.
Expert Review Process
Once submitted, the videos and accompanying documents undergo a rigorous review by a panel of expert endometriosis surgeons. This review is conducted anonymously to ensure objectivity. The experts assess various aspects of the surgeon’s performance, including:
- Surgical technique and precision
- Decision-making during complex situations
- Adherence to best practices in endometriosis surgery
- Management of potential complications
Here is an example of what the reviewers see: https://icarebetter.net/video-id-32×3/
Specialized Verifications
The video vetting process can also lead to specialized verifications. For instance, a surgeon might receive specific designations for their expertise in areas like:
- Diaphragm endometriosis
- Bowel endometriosis management
- Urinary tract endometriosis treatment
- Advanced endometrioma excision techniques
These specialized verifications provide a more granular view of a surgeon’s expertise, allowing patients to find specialists who closely match their specific needs.
Why Video Vetting is Important for Endometriosis Surgeons
The importance of video vetting for endometriosis surgeons cannot be overstated. This approach to surgeon verification addresses several critical needs in endometriosis care, benefiting both patients and doctors.
Elevating Standards of Care
Video vetting raises the bar for endometriosis surgery by setting a new standard for skill verification. It encourages surgeons to continually refine their techniques so they can successfully pass the vetting. This drive for excellence ultimately translates to better patient outcomes and a higher overall standard of care in endometriosis treatment.
Addressing the Complexity of Endometriosis
Endometriosis is a complex condition that can present in various forms and severity. Video vetting allows surgeons to demonstrate their ability to handle this complexity in each specific disease region, such as bowel, diaphragm, ovaries, ureters, bladder, and other organs. By showcasing their skills in managing different types of endometriosis lesions and associated complications, surgeons can prove their readiness to tackle even the most challenging cases.
Enhancing Professional Development
The process of preparing for and undergoing video vetting can be a valuable learning experience for surgeons. It encourages self-reflection and critical analysis of one’s surgical techniques. This introspective approach can lead to continuous improvement and professional growth, benefiting the surgeon and their future patients.
Building a Network of Excellence
Video vetting creates a community of verified endometriosis specialists. This network can facilitate knowledge sharing, collaboration on complex cases, and the advancement of endometriosis treatment techniques. Such a community of excellence can drive innovation and improve the overall quality of endometriosis care globally.
Facilitating Patient-Surgeon Matching
For patients, finding the right surgeon for their specific endometriosis case is crucial. Video vetting facilitates this matching process by providing detailed insights into a surgeon’s areas of expertise. Patients can more easily identify surgeons who have demonstrated proficiency in endometriosis. This will lead to more targeted search and effective treatment plans.
Steps to Go Through Video Vetting Process as an Endometriosis Surgeon
For endometriosis surgeons looking to undergo the video vetting process, there are several key steps to follow. This structured approach ensures a comprehensive and fair evaluation of surgical skills and expertise.
Selecting the Right Platform – iCareBetter
The first step is choosing an appropriate platform for video vetting. Currently, iCareBetter stands out as the primary platform offering transparent double-blind video-vetting verification for endometriosis surgeons. When selecting a platform, consider factors such as:
- Reputation and credibility in the medical community
- Transparency of the vetting process
- Quality and expertise of the reviewing panel
- Potential impact on your practice and patient trust
Preparing Surgical Videos
The core of the video vetting process lies in the surgical videos surgeons submit. Here are key considerations for preparing these videos:
- Focus on Representative Cases: Choose surgeries that best showcase your skills in managing stage II or higher endometriosis.
- Highlight Key Techniques: Ensure your videos demonstrate crucial skills such as:
– Deep endometriosis excision
– Pelvic wall dissection
– Endometrioma management - Include Specialized Procedures: If aiming for specific designations, include videos of specialized techniques like:
– Diaphragm endometriosis treatment
– Bowel resection for endometriosis
– Ureter re-implantation
– Bladder excision procedures - Ensure Video Quality: Make sure the video quality is sufficient for clear evaluation.
Submitting Your Materials
Once your videos and documents are prepared:
- Use a secure cloud storage system like Dropbox to share your content.
- Organize all materials in a clear, easily navigable format. Create one folder for each patient and put all the videos and documents there.
- Ensure all patient-identifying information is properly redacted to maintain privacy.
Undergoing the Review Process
After submission, your materials will undergo a rigorous double-blind review process:
- Three expert reviewers will anonymously evaluate your surgical videos and documents.
- The review focuses on surgical technique, decision-making, and adherence to best practices.
- You may receive requests for additional information during this process.
Receiving and Implementing Feedback
Upon completion of the review:
- You’ll receive detailed feedback on your submitted materials.
- Use this feedback as an opportunity for professional growth and improvement.
- Consider implementing suggested changes in your surgical practice.
Promoting Your Video Vetting Designation
Once successfully vetted:
- Update your professional profiles and website to reflect your new designation.
- Inform your patients about the significance of this verification.
- Consider sharing your experience with colleagues to encourage wider adoption of video vetting in the endometriosis surgery community.
Challenges and Solutions in Video Vetting for Surgeons
While video vetting offers numerous benefits, it also presents certain challenges for endometriosis surgeons. Understanding these video vetting challenges and their potential solutions is crucial for the successful implementation and widespread adoption of this innovative verification process.
Addressing Patient Privacy and HIPAA Compliance
One of the primary concerns in video vetting is maintaining patient privacy and adhering to HIPAA regulations. Surgeons must ensure that all patient-identifying information is removed from their submitted materials.
Solutions:
- Implement robust de-identification processes for all video and document submissions.
- Use secure platforms for storing and sharing videos and documents.
Managing Technical and Time Constraints
Preparing high-quality surgical videos and compiling comprehensive documentation can be time-consuming and technically challenging for busy surgeons. Plan ahead to record the appropriate cases and seek help from your team to collect documents.
Video Vetting as a Vital Tool for Building Patient Relationships
Video vetting has emerged as an invaluable approach for endometriosis surgeons to build rapport and provide crucial information to patients early in their decision-making journey. This innovative process not only confirms a surgeon’s expertise but also elevates trust and engagement. This trust lays the foundation for strong patient relationships.
Enhancing Transparency and Trust
By participating in video vetting, surgeons demonstrate a commitment to transparency and excellence. This openness can significantly boost patient trust, as it provides tangible evidence of a surgeon’s skills and expertise.
- Patients gain confidence in their surgeon’s abilities before the first consultation.
- The transparency of the vetting process helps alleviate anxiety and uncertainty about surgical procedures.
Facilitating Informed Decision-Making
Video vetting empowers patients with detailed information about a surgeon’s capabilities. This information enables them to make a more informed decision about their care.
- Patients can better understand and trust the skills of surgeons.
- This knowledge allows for more meaningful discussions during consultations, as patients come prepared with relevant questions and concerns.
Creating a Personal Connection
Although patients don’t directly view the surgical videos, the knowledge that their surgeon has undergone this rigorous process can create a sense of personal connection and trust.
- Patients feel more comfortable knowing their surgeon’s skills have been independently verified.
- This initial trust can lead to more open and productive doctor-patient communications.
Demonstrating Commitment to Quality Care
Surgeons who undergo video vetting showcase their dedication to providing the highest standard of care, which resonates strongly with patients.
- It signals a surgeon’s willingness to be evaluated and continuously improve their skills.
- This commitment to excellence can be a key differentiator in a patient’s choice of their surgeon.
Addressing Specific Patient Concerns
Video vetting allows surgeons to demonstrate proficiency in specific areas of endometriosis surgery, directly addressing common patient concerns.
- Patients with complex cases can find surgeons verified in handling their specific type of endometriosis.
- This targeted matching can lead to better outcomes and higher patient satisfaction.
Encourage Patient Engagement
The existence of a video vetting process can encourage patients to be more engaged in their healthcare decisions.
- It prompts patients to ask more informed questions about surgical techniques and outcomes.
- This increased engagement can lead to better preparation for surgery and more realistic expectations.
Facilitating Referrals and Second Opinions
Video-vetted surgeons can more confidently claim endometriosis expertise and offer second opinions, knowing their skills have been objectively verified.
- This can lead to a more collaborative approach to patient care.
- Patients benefit from a network of verified experts working together for their best interests.
In conclusion, video vetting is a vital tool in building strong, trust-based relationships between endometriosis surgeons and their patients. By undergoing this process, surgeons not only validate their skills but also demonstrate a commitment to patient-centered excellence in care. This approach aligns perfectly with the evolving healthcare landscape, where informed patients seek transparency and excellence in their medical care. As the field of endometriosis surgery continues to advance, video vetting will likely play an increasingly crucial role in ensuring high-quality care and facilitating positive patient outcomes.
References:
https://www.benefitspro.com/2021/01/07/4-steps-to-vetting-a-virtual-care-solution-for-your-employees
https://www.gov.uk/government/publications/demystifying-vetting

Top Endometriosis Specialist in New York—Find Expert Care Near You Today!
Table of Contents
- New York’s Endometriosis Experts: Hope in the City That Never Sleeps
- Endometriosis Symptoms Checklist
- Advanced Endometriosis Treatment in New York City
- Best Endometriosis Surgeons in New York City
- Endometriosis Treatment Options New York: As Diverse as New York Itself
- Fertility Preservation and Treatment
- Living with Endometriosis in New York: Endometriosis Support
- Empowering Your Endo Journey in the City of Dreams
New York’s Endometriosis Experts: Hope in the City That Never Sleeps
Endometriosis affects millions of women worldwide, causing debilitating pain and potential fertility issues. For those living in or near New York City, finding a top endometriosis specialist is crucial for proper diagnosis and treatment. This comprehensive guide will help you navigate the process of locating expert care, understanding treatment options, and taking control of your health.
Living with endometriosis can be challenging, but with the right medical team by your side, relief is possible. New York City is home to some of the world’s leading endometriosis experts, offering hope and healing to those struggling with this complex condition. Moreover, New York’s specialists combine the latest endometriosis research, treatment, and community resources. Whether you’re experiencing symptoms for the first time or seeking more effective management of long-standing issues, this article will equip you with the knowledge to find the best care available. Finding expert care is a big step toward reclaiming your quality of life!
Endometriosis Symptoms Checklist
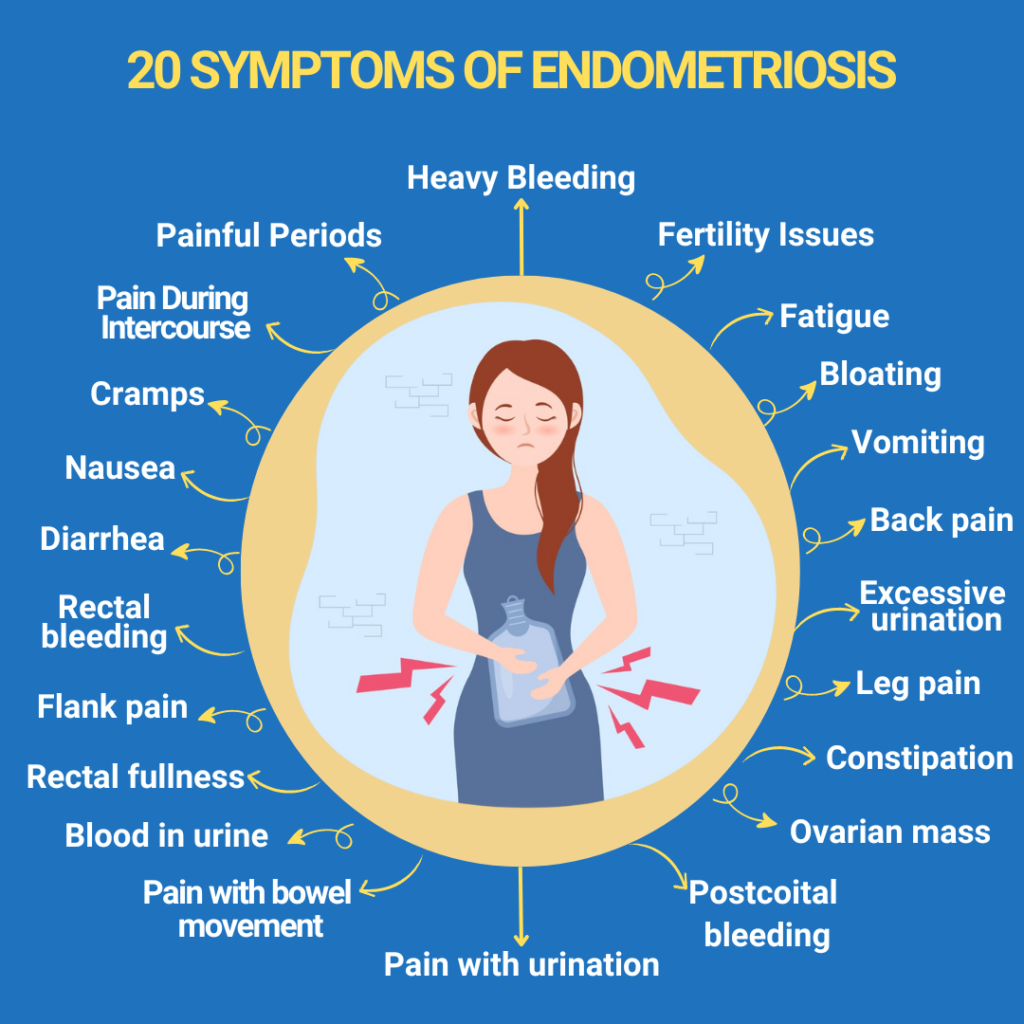
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus, often affecting the ovaries, fallopian tubes, and pelvic lining. This misplaced tissue responds to hormonal changes, leading to inflammation, pain, and potential scarring. The condition can have far-reaching effects on a woman’s quality of life, impacting everything from daily activities to intimate relationships and fertility.
Endometriosis Symptoms Checklist for Your Guidance:
- Heavy bleeding
- Fertility Issues
- Fatigue
- Bloating
- Vomiting
- Back pain
- Excessive urination
- Leg pain
- Constipation
- Ovarian mass
- Postcoital bleeding
- Pain with urination
- Pain with bowel movements
- Blood in urine
- Rectal fullness
- Flank pain
- Rectal bleeding
- Diarrhea
- Nausea
- Cramps
- Pain during intercourse
- Painful periods
It’s important to note that symptoms can vary widely between individuals, and some women may have few or no apparent symptoms despite having the condition. This variability makes accurate diagnosis crucial, highlighting the need for experienced specialists to recognize the subtle signs of endometriosis.
Advanced Endometriosis Treatment in New York City
New York City is recognized worldwide for its exceptional healthcare system, offering patients access to cutting-edge treatments and advanced research. This reputation for medical excellence is precious for those with complex conditions like endometriosis, who benefit from having a range of specialized care options nearby. In New York, renowned experts consistently push the boundaries of what’s possible in endometriosis treatment, often setting new standards for care. Patients here can access minimally invasive surgical options, advanced diagnostic imaging, and innovative pain management techniques that may not be widely available elsewhere.
Moreover, New York is home to many leading researchers actively working on understanding and treating endometriosis. For those impacted by endometriosis, this means better symptom management, faster recoveries, and potentially reduced recurrence rates. In addition, the collaborative environment among New York’s medical institutions allows for a holistic approach to patient care. Specialists, surgeons, pain management experts, and reproductive endocrinologists often work together to design individualized treatment plans.
Best Endometriosis Surgeons in New York City
New York City is home to numerous world-class specialists, making it an ideal location for those seeking expert endometriosis care. These surgeons often have extensive training in minimally invasive techniques, such as laparoscopic and robotic-assisted excision surgery, which can provide more effective symptom relief and lower recurrence rates than other methods. Leading surgeons also frequently collaborate with other specialists to offer comprehensive, individualized treatment plans tailored to each patient’s needs.
Among the best endometriosis surgeons in NYC are Dr. Andrea Vidali, Dr. Lora Liu, and Dr. Amanda Chu. They are known for their expertise and dedication to advancing care for patients with this complex condition. You can find more information about them and search for additional doctors in New York at iCareBetter. On this platform, you can find vetted top-notch doctors specializing in treating endometriosis and women’s pelvic pain worldwide.
Dr. Andrea Vidali

Dr. Andrea Vidali, a renowned endometriosis and reproductive immunology specialist, is celebrated for his minimally invasive excision surgery skills and personalized approach to fertility preservation. Through his comprehensive treatment plans, he has helped many women achieve successful pregnancies.
Dr. Lora Liu

Dr. Lora Liu is recognized for her precision in laparoscopic and robotic-assisted surgeries, providing endometriosis patients with effective and minimally invasive options to manage endometriosis. Her commitment to innovative techniques and compassionate approach to patient care make her a trusted figure in New York’s medical community. She is known for her collaborative, patient-centered methods, empowering individuals with endometriosis to reclaim their quality of life.
Dr. Amanda Chu, MD

Dr. Amanda Chu, MD, is a Board-Certified Gynecologic Surgeon specializing in minimally invasive techniques, particularly endometriosis excision surgery and treatment for pelvic endometriosis and fertility-related issues. Her expertise extends to multi-organ endometriosis and its impact on pain, fertility, and overall quality of life. Dr. Chu is dedicated to enhancing patient and provider education on endometriosis. Her focus areas include advanced robotic surgery, chronic pelvic pain management, and advanced hysteroscopy.
Endometriosis Treatment Options New York: As Diverse as New York Itself
Dr. Vidali is a Video-Vetted excision surgeon for endometriosis. His approach to endometriosis is holistic, addressing the disease and any potentially associated conditions. Currently, since we lack medical options for curing endometriosis, the primary treatment step is excision surgery. Additionally, Dr. Vidali utilizes hormonal contraception, preferably progestins—either orally or via IUDs—to manage bleeding or any adenomyosis-related factors, if present. He does not favor GnRH agonists or antagonists, as, in his experience, their risk and efficacy profiles are not superior to those of progestins, making them less desirable.
Dr. Liu, a Video-Vetted excision surgeon for endometriosis, believes that the etiology of endometriosis is complex and multifactorial, and she supports the Mullerianosis theory. However, other contributing factors also exist, including oxidative stress, inflammation, impaired immune response, genetics, and both endogenous and exogenous hormones, all of which play a role in the pathogenesis and proliferation of endometriosis.
Dr. Amanda Chu, a Video-Vetted excision surgeon for endometriosis, believes that the approach to endometriosis care is rooted in the understanding that no single theory thoroughly explains all cases of endometriosis. She believes that specific theories may apply more significantly to individual patients. While older concepts like retrograde menstruation and coelomic metaplasia remain valuable, Dr. Chu emphasizes the importance of ongoing research. She believes emerging insights into epigenetics and immune dysregulation will play a growing role in understanding and treating endometriosis.
Advanced Diagnostic Techniques
Accurate diagnosis is crucial for effective endometriosis treatment. Top specialists in New York utilize a range of advanced diagnostic techniques to identify and assess the extent of endometriosis, including:
- High-Resolution Imaging
Advanced imaging technologies, such as transvaginal ultrasound and MRI, can help visualize endometriotic lesions and assess the extent of the disease. These noninvasive methods are often used as initial screening tools.
- Laparoscopy
L laparoscopy is considered the gold standard for endometriosis diagnosis. It allows doctors to inspect the pelvic cavity for endometriosis tissue and samples visually. This minimally invasive surgical procedure can also remove lesions and adhesions.
- Biomarker Testing
Emerging research explores the use of blood and tissue biomarkers to aid endometriosis diagnosis. While yet to be widely available, some specialized centers may offer these cutting-edge tests as part of their diagnostic toolkit.
Innovative Treatment Approaches in New York
New York’s top endometriosis specialists offer a range of treatment options, from conservative management to advanced surgical techniques. Some of the innovative approaches available include:
- Minimally Invasive Excision Surgery
Laparoscopic and robotic surgeries are considered the gold standard for treating endometriosis. This technique involves carefully removing endometriotic lesions while preserving healthy tissue and organs. Skilled surgeons can often perform complex procedures using minimally invasive techniques, leading to faster recovery and less scarring.
- Robotic-Assisted Surgery
Some specialists use robotic-assisted surgical systems to enhance precision and control during endometriosis excision. This technology can be particularly beneficial for complex cases or when operating in difficult-to-reach areas.
- Hormone Therapy
Advanced hormone therapies, including newer progestin-only options, can help manage symptoms in some cases. Specialists can tailor hormone treatments to patients’ unique needs and medical history.
- Integrative Approaches
Many top endometriosis centers in New York offer integrative care options, combining traditional medical treatments with complementary therapies like acupuncture, pelvic floor physical therapy, and nutritional counseling to address the multifaceted nature of endometriosis.
Fertility Preservation and Treatment
For women with endometriosis who hope to conceive, fertility preservation and treatment are crucial considerations. New York’s leading endometriosis specialists often work closely with reproductive endocrinologists to offer:
- Fertility assessments and counseling
- Egg freezing and fertility preservation options
- Assisted reproductive technologies like IVF
- Surgical interventions to improve fertility outcomes
By addressing both endometriosis and fertility concerns simultaneously, these integrated approaches can help maximize a woman’s chances of achieving a successful pregnancy.
Living with Endometriosis in New York: Endometriosis Support
Living with endometriosis can be isolating, but connecting with others who understand your experience can be incredibly empowering. New York offers several support groups and advocacy organizations for endometriosis patients, including:
- Endometriosis Foundation of America
- NYC Endometriosis Support Group
Additionally, you can find valuable information and resources on the iCareBetter website. Our blog, forum, and published articles offer significant insights about endometriosis and its specialists.
To adapt to city life with Endo, try flexible commuting options, consider an anti-inflammatory diet (easy with NYC’s healthy food options), and focus on gentle exercise like yoga or walks in Central Park. These lifestyle adjustments and community resources can make managing endometriosis in the city more accessible.
Empowering Your Endo Journey in the City of Dreams
Finding a top endometriosis specialist in New York is crucial to reclaiming your health and quality of life. With access to world-class medical care, innovative treatments, and supportive communities, women with endometriosis have more options than ever before. By arming yourself with knowledge, seeking expert care, and advocating for your needs, you can take control of your endometriosis journey and work towards a future free from debilitating pain and limitations.
If you are struggling with endometriosis and seeking proper care, don’t navigate this journey alone! Visit iCareBetter to connect with top endometriosis specialists in New York who can provide personalized treatment options and support. Empower yourself with the knowledge and resources you need for better health—take the first step toward a brighter future today!
Remember, every woman’s experience with endometriosis is unique, and finding the right specialist may take time. Don’t be discouraged if your first appointment doesn’t provide all the answers—perseverance and self-advocacy are keys to finding the care you deserve. With the right team by your side, relief and healing are possible, opening the door to a brighter, pain-free future.
References:
https://www.dukehealth.org/treatments/obstetrics-and-gynecology/endometriosis-and-pelvic-pain

Unraveling the Links Between Endometriosis and Mental Health
Endometriosis is a medical condition often associated with severe pelvic pain and fertility issues. This disease might have significant psychological implications. This article reviews the relationship between endometriosis and mental health, highlighting how the physical symptoms of this disorder can translate into emotional distress.
Understanding Endometriosis
Endometriosis is a prevalent systemic and gynecological condition characterized by the abnormal growth of uterine lining cells, known as endometrium, outside the uterus. These abnormal cell growths can affect various organs, including the ovaries, fallopian tubes, and sometimes even the bladder, intestines, and rectum.
The symptoms of endometriosis include chronic pelvic pain, heavy menstrual periods, pain during sexual intercourse, and infertility. It’s estimated that about one in 10 women of reproductive age experience endometriosis, with the condition mainly impacting women in their 30s and 40s. An estimated 40% of women with infertility have endometriosis.
1- The Pain-Depression Connection in Endometriosis
The chronic pain associated with endometriosis can significantly disrupt a woman’s daily life, causing distress and leading to mental health conditions like depression and anxiety. The persistent pain can trigger feelings of hopelessness and helplessness. The debilitating effects of endometriosis pain can impact work, social interactions, and intimate relationships, contributing to feelings of isolation and lowered self-esteem.
2- Psychological Toll of Challenges of Endometriosis Diagnosis
One of the significant mental health challenges associated with endometriosis comes from the often lengthy and distressing diagnostic process. It’s not uncommon for women to experience symptoms for several years before receiving a diagnosis. Such delays in diagnosis, often due to the normalization of symptoms by healthcare professionals, can exacerbate the psychological distress associated with the condition.
Moreover, women with endometriosis often report feeling dismissed or misunderstood by healthcare professionals, which can further impact their mental health. A lack of understanding and acknowledgment of the chronic pain experienced by these women can lead to feelings of invalidation and frustration.
3- The Impact of Endometriosis on Relationships
The physical symptoms of endometriosis can significantly influence a woman’s relationships. Painful intercourse, one of the common symptoms of the condition, can cause strain in intimate relationships, leading to feelings of guilt, resentment, and anxiety. On top of that, infertility challenges can also be a complex issue in relationships. Furthermore, individuals with endometriosis might have constant chronic pain and reduced energy for participation in events. This lack of energy and presence can majorly impact a person’s relationships. These factors’s deteriorating effects on relationships can further exacerbate mental health conditions like depression and anxiety.
4- Endometriosis and Work-Life
The impact of endometriosis extends to a woman’s professional life. The heavy menstrual bleeding and severe pain associated with the condition can make maintaining a regular work schedule challenging. This work-life issue can lead to feelings of guilt and stress, further contributing to the development of mental health conditions.
5- Racial and Ethnic Differences in Endometriosis and Mental Health Impact
There’s limited research on racial and ethnic differences in endometriosis and its mental health impacts. However, a review study found that compared with white women, black and Hispanic women were less likely to be diagnosed with endometriosis. This lack of diagnosis will make the whole treatment and diagnosis process longer, which will result in more adverse mental health impacts.
6- Treatment Options and Their Psychological Implications
While there’s no definitive cure for endometriosis, various treatment options can help manage the symptoms. These include over-the-counter pain medications, hormone therapies, and, in severe cases, surgical treatments. However, the effectiveness of these treatments can vary, and the prospect of long-term management can lead to feelings of anxiety and depression.
Furthermore, some treatments, particularly surgical ones, can have physical side effects that can impact a woman’s body image, leading to further psychological distress.
7- The Role of Support and Therapy
Support groups, counseling, and cognitive-behavioral therapies can play a significant role in managing the emotional distress associated with endometriosis. These strategies can provide patients with some help tools to cope with their physical symptoms, as well as the emotional toll of living with endometriosis.
Concluding Remarks
The links between endometriosis and mental health are complex and deeply personal. Recognizing the psychological implications of endometriosis is a critical step in providing comprehensive care to individuals affected by this condition. By acknowledging the psychological stress associated with this condition, healthcare providers can positively impact the mental health outcomes of women living with endometriosis. Patients with endometriosis should seek help not only for their physical symptoms but also for any emotional distress they may be experiencing. Doing so might improve their quality of life and overall well-being.
References:
https://www.psychiatry.org/news-room/apa-blogs/how-endometriosis-can-impact-mental-health
https://www.drdanielkushner.com/blog/how-does-endometriosis-impact-mental-health
https://www.medicalnewstoday.com/articles/endometriosis-and-depression
https://www.womenspelvicsurgery.com/blog/how-endometriosis-affects-emotional-wellbeing
https://share.upmc.com/2023/07/endometriosis-and-depression

How to Treat Deep Infiltrating Endometriosis
Endometriosis, bad enough when endometrial-like cells grow outside the uterus and on the surface of other organs, has an even more troubling variant called Deep-Infiltrating Endometriosis (DIE). This is a severe form of endometriosis defined by these abnormal cells burrowing or invading deeper into tissues and affected organs, like the bowel and bladder. Generally, the depth cutoff to fit this category is more than 5mm below the tissue surface. This guide will shed some light on how we treat and potentially cure deep infiltrating endometriosis in the future. At this time, a long-standing cure is still a stretch, even for superficial endometriosis.
Table of contents
- Understanding Deep Infiltrating Endometriosis
- Identifying Symptoms of Deep Infiltrating Endometriosis
- Causes and Risk Factors of Deep Infiltrating Endometriosis
- Diagnosing Deep Infiltrating Endometriosis
- Treatment Options for Deep Infiltrating Endometriosis
- Considerations in Surgical Management
- Conclusion
Understanding Deep Infiltrating Endometriosis
The good news is that this condition is relatively rare, affecting only about 1% of women of reproductive age and only 20% of those with endometriosis. The bad news is that molecular data suggests it may be a premalignant disease, along with endometrioma type. However, this is still undergoing research, and the malignancy potential remains low. However, when genetic mutations are shared with an aggressive disease like cancer, this may help explain why endometrioma and DIE types of endo are more likely to cause more local anatomic distortion and harm with pain and subfertility impact, as well as increased metastatic potential (i.e., spread to other parts of the body even if there is no associated cancer).
Anatomic Comparison of Endometriosis Types
Based on the anatomical location of endometriosis within the pelvic and abdominal cavities, there are three major types of endo:
- Superficial endometriosis (Peritoneal endometriosis or PEM): Lesions appear on the surface of organs outside the endometrium. Generally, but not always, they cause the least amount of tissue damage and distortion.
- Ovarian endometriomas (OE): Dark cysts due to old collected blood, also called chocolate cysts, develop in or on the ovaries due to endometriosis.
- Deep infiltrating endometriosis: The most severe form, where the endometrial-like tissue invades deeper into the pelvic organs, wreaking more havoc.
Anatomic locations and clinical degree of disease form the basis for most of the staging systems that are currently used. This is extremely “old school,” and we are about to step into a new age where molecular insights will help with diagnostics and treatment options because abnormal molecular pathways can be targeted with precision therapies.
Molecular Comparison of Endometriosis Types
This is an evolving hot topic of research in endometriosis, which goes well beyond comparisons based on hormonal factors like receptor activity, up and down-regulation, and relative progesterone resistance. It is too early to classify different types of endo by this gene mutation molecular pathway metric, but what is known so far might already help with recurrence and cancer risk mitigation.
What we know is as follows:
- Endometriosis overall (PEM, OE, and DIE types) is a disease of genetic and molecular heterogeneity, meaning multiple genes are affected. Some of these are mutations exactly like those found in cancer, even if no cancer is present or even destined to develop. This means endo may not be one disease entity between different individuals but rather different ones with varying degrees of aggressiveness. On the other hand, in any given individual, there is research data to support “clonal” molecular signature similarities between all three types of endo, meaning one type (e.g., PEM) advances or progresses to the other (OE or DIE).
- Mutations of interest include ARID1A, PIK3CA, KRAS, and PPP2R1A, among others
- Endometrioma type carries the highest risk of malignant degeneration, and ARID1A is considered to be one of the most important driver mutations to clear cell cancer.
- DIE type has a wider range of mutations and is at a lower risk of malignant degeneration, but these mutations may contribute to its more aggressive behavior.
- OE-type risk for malignant degeneration may be higher than that for DIE because the molecular micro-environment differs between these two, with the ovaries possibly being more “permissive” to malignant changes. This does not negate the aggressive, invasive, and potentially metastatic nature of DIE in the absence of cancer.
- Gene mutation expression varies based on epigenetic influences, including diet, lifestyle, toxin exposure, concurrent disease states, mind-body influence, etc.
What does this all mean in summary? Multiple genes are mutated in endometriosis, some of which may or may not lead to a low risk of cancer development but can dictate how aggressive endo types, especially DIE and OE, can be in an individual. These gene mutations can be suppressed or aggravated by epigenetic influences that you have some control over. Evolving research is helping uncover diagnostic and prescription molecular treatment options based on all of this.
Identifying Symptoms of Deep Infiltrating Endometriosis
The symptoms of DIE are similar to general endometriosis but usually more severe. They may include:
- Severe pelvic pain
- Painful urination (dysuria) of bleeding in the urine (hematuria)
- Painful menstruation (dysmenorrhea)
- Genital pain before, during, or after sex (dyspareunia)
- Digestive discomfort and rectal bleeding
- Distant symptoms like pain with breathing, related to possible diaphragm involvement
Causes and Risk Factors of Deep Infiltrating Endometriosis
Notwithstanding recent research advances, the exact cause of endometriosis, including DIE, is unknown. A family history of endo and/or cancer are important to consider. It is not likely that a single cause will be uncovered because of the probable multifactorial nature of endo. However, molecular research is taking this to a different level.
Diagnosing Deep Infiltrating Endometriosis
Since deep infiltrating endometriosis is an advanced form of endometriosis, its diagnosis can be challenging. Usually, multiple diagnostics are used, including medical history, physical examination, histological examination after surgery or upon biopsy (e.g., C-section scar endo), minimally invasive surgery, ultrasound, and MRI. A 3-Tesla (“3T” for short) MRI is probably the most accurate modality, but it still has many shortcomings. In other words, it can be helpful in planning for surgery but should not be used to determine definitively if DIE is present or not. It is as good as it gets but is imperfect, missing up to 20% of DIE.
In many, if not most, cases, the diagnosis will only be apparent and confirmed at the time of surgery. Since it is impossible to accurately predict the full extent of endo before surgery, this is the main reason that it is very prudent to pick the most skilled and experienced surgeon you can find. The more symptomatic you are, the more this is critical to your success. A botched surgery does not make it easier the second time around, and it exposes you to an increased risk of major complications.
Treatment Options for Deep Infiltrating Endometriosis
Medical Treatments
Medical treatments for DIE are extremely limited and basically non-existent. This is because the deep invasive infiltration of disease leads to scarring or fibrosis as your body tries to “wall off” or isolate this disease and heal. Any known medication cannot eliminate fibrosis. What we are left with are pain relievers and hormonal options that are used in all forms of endo, for symptomatic relief and possibly some suppressive effect.
Integrative options are also an option for symptomatic relief, just as they are for any type of endo. This includes mind-body-based biofeedback, nutrition, botanicals, essential oils, acupuncture and acupressure, electrical stimulation (TENS), etc. It is best to formulate an integrative strategy with a relevant practitioner.
Pelvic floor physical therapy (PFPT) is, of course, central to a treatment plan as well. However, depending on lesion location, this should be undertaken with some caution due to possible disruption of deep lesions with internal therapies, making surgery potentially less effective. A teamwork approach should be conducted to evaluate the best strategy.
Surgical Treatments
Surgical excision of DIE lesions and associated fibrosis is by far the best path forward in most cases where DIE is anticipated and/or already diagnosed from prior surgery. The usual admonitions of excision superiority over ablation are even more critical here because ablation or fulguration is totally useless for lesions of uncertain depth. Also, with ablation, there is an elevated risk of damaging tissues like the rectum, bladder, and ureters.
A master surgeon is best equipped for DIE, and, in the author’s opinion, these types of cases should be performed robotically because of the far superior optics and wristed robotic instruments. Further, the surgeon should either be able to handle bowel, bladder, and ureters, including reimplantation where required, or have a well-integrated team ready to participate in a planned fashion. The problem is that it is hard to tell what will be required before surgery. Still, the best efforts through imaging-based mapping and attention to symptoms should be made to adequately prepare for resection/excision of anything found.
DIE most definitely does not mean an automatic hysterectomy recommendation. However, if childbearing is complete, this may need to be discussed for risk vs. benefit to remove all diseased tissue. Similarly, the closer to menopause, the more disease and the higher the risk of malignancy due to family history or genetic testing, the more it is prudent to talk about the risk vs. benefit of ovarian conservation. This should be highly individualized and thoroughly discussed for the best outcome.
Considerations in Surgical Management
Indocyanine Green (ICG) Fluorescence
Indocyanine green (ICG) fluorescence imaging allows surgeons to visualize the details of the ureters and safely remove the maximum amount of infiltrating endometrial tissue without damaging the urinary tract. It is also helpful to determine if a bowel segment that has been operated upon retains good blood supply and viability. This helps avoid complications.
Stenting During Partial Cystectomy or Ureteral Reimplantation
During bladder surgery for urinary endometriosis, surgeons can place stents (tiny plastic catheters) to help protect the ureters (the delicate tubes through which urine travels from the kidneys to the bladder) from further damage or to enhance healing after reimplantation.
Pathology Evaluation
Other than standard pathology evaluation, research evidence suggests several newer assessments might be considered in DIE and OE. Specifically, the more the disease looks clinically aggressive, the more the pathologist should ensure that there is no clear cell cancer component. Beyond that, even with no evidence of cancer, the tissue specimens removed can be assessed for “mitotic index,” meaning whether the pathologist sees many dividing cells. This is more often seen in aggressive disease, even in the absence of cancer. This, in turn, may lead to consideration of some degree of well-tolerated hormone suppression (e.g., micronized progesterone) to potentially reduce recurrence risk. Finally, there are immunohistochemical (IHC) stains for some molecular abnormalities that gene mutations can spawn (e.g., ARID1A). This is not readily available but can be considered, especially in a situation where cancer risk is elevated. In the future, as discussed above, these aberrant molecular pathways will be targeted with precision therapies.
Endometriosis and Fertility
Endometriosis, including DIE, can impact fertility. Consequently, surgeons should employ as many atraumatic surgical techniques as possible to avoid injuring delicate structures in the reproductive system and improve the chances of pregnancy. This is optimized with the robotics platform.
Conclusion
Deep infiltrating endometriosis adds a layer of complexity to the management of endo. Surgery is the optimal therapy, followed by supportive care and strategies to mitigate recurrence if possible. Malignant degeneration is uncommon but possible, which means that, especially with a family history of cancer, genetics testing should be considered. The more complex, the more the need for an endometriosis expert master surgeon in your corner. If the cancer risk is elevated for any of the reasons noted in this article, a gynecologic oncologist should be considered at least as a consultant.
References:
The Diagnosis and Treatment of Deep Infiltrating Endometriosis

Rediscovering Life After Endometriosis Surgery: Tips and Strategies for a Full Recovery
Endometriosis surgery, typically excision of endo implants and related fibrosis, using minimally invasive laparoscopy or robotic surgery, significantly impacts women’s health and recovery journey. Here’s an enhanced guide to life post-surgery, incorporating tips to improve physical and mental healing towards lasting thrivorship.
Table of contents
Understanding Endometriosis and Its Surgical Treatment

Endometriosis involves the growth of tissue similar to the uterine lining outside the uterus, creating pain and sub-fertility. Thankfully, minimally invasive surgery requires only small incisions through which a camera and instruments can be placed. This is the gold standard for diagnosing and treating endometriosis and has revolutionized the healing process and length of time to full recovery. (Ferrero et al., 2018).
The Recovery Period
Recovery from laparoscopic or robotic minimally invasive surgery varies based on the extent of endometriosis and overall health. Typically, full recovery involves several weeks to a few months. Patients might experience tiredness initially and are advised to consume soft foods, stay hydrated, and take fiber supplements to avoid constipation, especially when using narcotic pain relief. It’s crucial to initially avoid strenuous activities but engage in light walks to promote healing. This reduces the risk of venous clots in the legs but avoids complications like hernias through the incisions.
How long you should take off work depends on the extent of the surgery, physical job demands, and any known medical co-existing conditions that might slow the healing process, such as diabetes. Discuss this with your surgeon before the procedure to set realistic expectations.
Enhanced Recovery Tips
- Balanced Nutrition: Within limits of allergies and food intolerance which may be specific to you, the following is a generic prudent healing plan:
- Protein: Lean meats, fish, eggs, tofu, and legumes help repair tissues.
- Fruits and Vegetables: Rich in vitamins, minerals, and antioxidants to reduce inflammation.
- Whole Grains: Brown rice, quinoa, and whole wheat bread for energy and fiber.
- Healthy Fats: Avocados, nuts, seeds, and olive oil for inflammation control.
- Hydration: Plenty of water, green and herbal teas.
- Bromelain Supplements: Bromelain, an enzyme found in pineapples, can reduce inflammation and promote healing by minimizing post-surgical scarring (Walker et al., 2018).
- Arnica: Homeopathic arnica can help reduce bruising and swelling, and may reduce pain as well.
- Vitamin C and Zinc: Essential for tissue repair and immune function.
- Probiotics: Support gut health, which can be disrupted by surgery, antibiotics used around the time of surgery, and pain medications.
- Red Light Therapy: Otherwise known as photobiomodulation, this modality can exert and anti-inflammatory effect, reducing prolonged inflammation and thereby can promote healing. Keep in mind, acute inflammation is part of normal healthy healing, so it may be prudent to avoid this for at least a month postop. (Hamblin MR)
Physical Health Post-Surgery
Post-surgery, physical health generally improves, with reduced bodily pain and better physical functioning. However, side effects like hot flashes can occur, particularly if the ovaries are removed or compromised and/or hormonal treatments are part of the post-surgery plan. Regular follow-ups are essential to monitor recovery and address any complications promptly. This is a highly individualized situation, so work with an expert before and after surgery.
Pain Management
- Heat Therapy: Use heating pads to alleviate abdominal pain. Be careful not to burn skin by not using something like a towel between the heat source and the skin.
- TENS Units: Transcutaneous Electrical Nerve Stimulation can help manage pain by sending small electrical pulses to the affected areas.
- Acupuncture: Can relieve pain and promote healing.
Mental Health Post-Surgery
Mental health is a crucial aspect of recovery. Enduring a chronic condition like endometriosis can lead to anxiety and depression. Therefore, incorporating mental health support into post-surgery care can be vital. Many women report improved emotional well-being post-surgery, but not all. So ongoing support may be necessary to manage any lingering psychological effects (Stratton et al., 2020).
Mental Health Tips
- Therapy and Counseling: Cognitive-behavioral therapy (CBT) can be effective.
- Mindfulness and Meditation: Practices like yoga and meditation can help manage stress and improve mental clarity.
- Support Groups: Joining endometriosis support groups can provide emotional support and practical advice.
Fertility and Family Planning
Fertility and family planning are significant concerns for many women with endometriosis. Studies show that surgery could double the spontaneous pregnancy rate in people with mild endometriosis. Those with moderate to severe endometriosis also have improved spontaneous birth rates after the laparoscopic removal of endometrial-like lesions.
However, even after successful surgery, some women may struggle with fertility issues. It is essential to have a candid discussion about fertility and family planning with your healthcare provider before surgery.
Financial Considerations
Endometriosis surgery can be financially burdensome. Many specialists are out-of-network, leading to high out-of-pocket costs in many, but not all, cases. It’s best to discuss potential expenses with your insurance provider and surgeon’s office beforehand. Additionally, explore options like payment plans or grants for financial support.
Managing Recurrence
Despite effective surgery, endometriosis can recur. Studies indicate a 51% recurrence rate within ten years. However, it can be in the 5-10% range if complete excision of visible implants is possible. This may require additional interventions that are often hormonally based but can also be integrative and holistic to some degree. Risk factors for recurrence include age, ovarian endometriosis, incomplete removal of lesions, and the initial surgeon’s expertise. Regular monitoring and follow-up surgeries may be required to manage recurrences effectively. It is very prudent to find the most experienced and highly trained surgeon possible. Here is a review of what you should be looking for in selecting a surgeon.
Prevention Strategies
- Hormonal Treatments: Birth control pills, gonadotropin-releasing hormone (GnRH) agonists, and other hormonal therapies can help prevent recurrence but may also carry significant and prolonged side effects. In general, the least potentially harmful option should be considered first and this should be highly individualized with your endo expert and/or reproductive endocrinologist.
- Lifestyle Modifications: Maintaining a healthy diet, avoiding toxins and regular exercise can support overall health and reduce the risk of recurrence by modulating and more efficiently eliminate excess estrogen in your system.
- Anti-inflammatory Diet: Incorporate foods rich in omega-3 fatty acids and antioxidants to reduce inflammation. It is best to craft a personalized plan with a nutrition expert.
Holistic Approaches
- Herbal Supplements: Consider supplements like turmeric, which has anti-inflammatory properties.
- Aromatherapy: Essential oils like lavender and peppermint can aid in relaxation and pain relief.
Conclusion
Quality of life after endometriosis surgery involves a multifaceted approach to physical and mental health, fertility, and financial planning. By understanding the recovery process and incorporating comprehensive care strategies, women can optimally navigate their post-surgery journey. Work with an endometriosis expert.
References
- Ferrero S, Evangelisti G, Barra F. Current and Emerging Treatment Options for Endometriosis. Expert Opin Pharmacother. 2018;19(11):1109-1125. doi:10.1080/14656566.2018.1507067. https://pubmed.ncbi.nlm.nih.gov/30096049/
- Vercellini P, Buggio L, Frattaruolo MP, Borghi A, Dridi D, Somigliana E. Medical treatment of endometriosis-related pain. Best Pract Res Clin Obstet Gynaecol. 2018;51:68-91. doi:10.1016/j.bpobgyn.2018.06.001. https://pubmed.ncbi.nlm.nih.gov/30126775/
- Zondervan KT, Becker CM, Missmer SA. Endometriosis. N Engl J Med. 2020;382(13):1244-1256. doi:10.1056/NEJMra1810764. https://pubmed.ncbi.nlm.nih.gov/32212520/
Updated Post: July 09, 2024
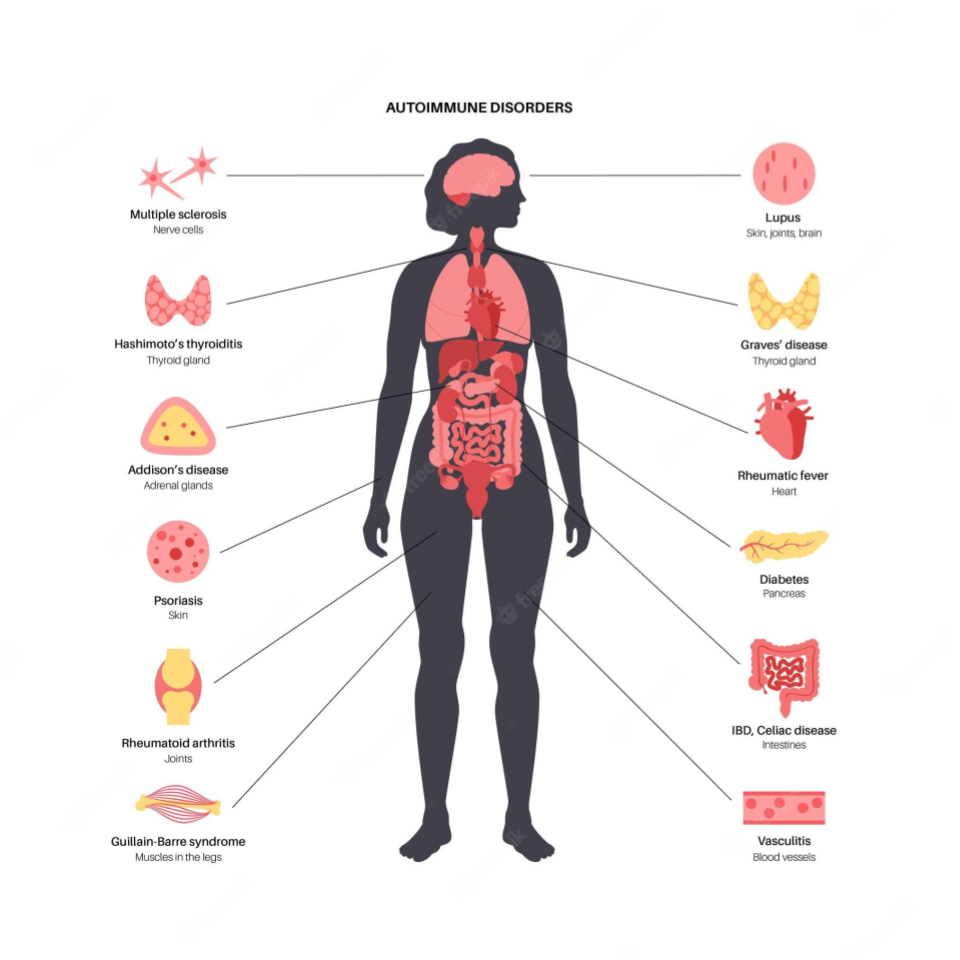
Unraveling the Connection Between Endometriosis and Autoimmune Diseases
Endometriosis causes pain, multiple bowel symptoms and infertility, among many other debilitating symptoms, in about 10% of women, mostly in the reproductive age range. Developing research has shown that there is a link to various autoimmune conditions.
Table of contents
- Understanding Endometriosis
- The Immune System’s Role
- Is Endometriosis an Autoimmune Disease?
- Systemic Lupus Erythematosus (SLE) and Endometriosis
- Sjögren’s Syndrome (SS) and Endometriosis
- Rheumatoid Arthritis (RA) and Endometriosis
- Autoimmune Thyroid Disorders (ATD) and Endometriosis
- Coeliac Disease (CLD) and Endometriosis
- Multiple Sclerosis (MS) and Endometriosis
- Inflammatory Bowel Disease (IBD) and Endometriosis
- The Bigger Picture
- The Path Ahead
Understanding Endometriosis
Endometriosis is a chronic gynecological disorder characterized by the presence of endometrial-like tissue growing outside the uterus. This means the cells look like those which line the inner part of the uterus but differ markedly in multiple ways at the molecular level. The more we find out the less it is clear what the origins are. However, they are likely partly genetic and partly based on other multiple influences of the environment on your body and genes.
The Immune System’s Role
Research suggests that abnormalities in the immune system may play a key role in the development of endometriosis. These abnormalities could prevent the immune system from effectively clearing ectopic endometrial cells, regardless of how they get there, allowing them to implant and grow outside the uterus. This hypothesis suggests that endometriosis might be, at least in part, an immunity-associated disorder.
Furthermore, endometriosis is often associated with a chronic inflammatory response, triggered by the presence of ectopic endometrial-like cells. This inflammation, coupled with the immune system’s inability to effectively remove ectopic cells, could partly explain the chronic pain often associated with endometriosis.
Is Endometriosis an Autoimmune Disease?
Autoimmune diseases occur when the immune system mistakenly attacks the body’s own cells, viewing them as foreign invaders. The link between endometriosis and autoimmune diseases is still being explored, but multiple studies suggest that women with endometriosis may have a higher risk for certain autoimmune diseases. It is not clear if endo carries a risk of developing autoimmune diseases or if the reverse is true or if they simply share common molecular mechanisms which results in both potentially occurring in any given individual. At this point it is important to stress that an “association” does not mean “cause”.
This review aims to delve into the current state of research on the association if endometriosis is an autoimmune disease. It presents key findings from population-based studies, discusses the potential implications, and highlights areas for future research.
Systemic Lupus Erythematosus (SLE) and Endometriosis
Systemic Lupus Erythematosus (SLE) is an autoimmune disease characterized by inflammation and damage to various body tissues, including the skin, joints, kidneys, and heart. Some studies have suggested a positive association between endometriosis and SLE.
One study suggested a seven-fold increase in the odds of having SLE among women with endometriosis. However, the study relied on self-reported diagnoses, which may introduce bias. A more recent cohort study found a more modest but still significant elevation in SLE risk among women with endometriosis.
Sjögren’s Syndrome (SS) and Endometriosis
Sjögren’s Syndrome (SS) is an autoimmune disorder characterized by dry eyes and mouth, often accompanied by other systemic symptoms. Several studies have investigated the potential link between SS and endometriosis.
A meta-analysis of three case-control studies found a 76% higher odds of SS in women with endometriosis. However, these studies had small sample sizes and wide confidence intervals, indicating a need for further research. Confidence intervals describe the range of results around a measurement which indicate how accurate the conclusion might be. The tighter it is among measurements the better.
Rheumatoid Arthritis (RA) and Endometriosis
Rheumatoid Arthritis (RA) is a chronic inflammatory disorder affecting many joints, including those in the hands and feet. Some studies have suggested a link between endometriosis and an increased risk of developing RA.
One meta-analysis, for example, found a 50% increased risk of RA among women with endometriosis. Again, the studies included in the analysis had limitations, including small sample sizes and wide confidence intervals.
Autoimmune Thyroid Disorders (ATD) and Endometriosis
Autoimmune thyroid disorders (ATDs), including Graves’ disease and Hashimoto’s thyroiditis, occur when the immune system attacks the thyroid gland, leading to either overactivity (hyperthyroidism) or underactivity (hypothyroidism) of the gland.
A meta-analysis of three case-control studies suggested a non-significant increase in the odds of ATD in women with endometriosis. However, the studies had high heterogeneity and low-quality scores, suggesting that further research is needed.
Coeliac Disease (CLD) and Endometriosis
Coeliac disease (CLD) is an autoimmune disorder where ingestion of gluten leads to damage in the small intestine. Some studies have suggested a possible link between endometriosis and CLD.
A meta-analysis of two case-control studies found a four-fold increase in the odds of CLD among women with endometriosis. Again, these studies had small sample sizes and wide confidence intervals, indicating a need for further research.
Multiple Sclerosis (MS) and Endometriosis
Multiple Sclerosis (MS) is a chronic disease that attacks the central nervous system. Current research on the association between MS and endometriosis is limited and inconclusive, with some studies suggesting a possible link while others finding no significant association.
Inflammatory Bowel Disease (IBD) and Endometriosis
Inflammatory bowel disease (IBD), including Crohn’s disease and ulcerative colitis, is characterized by chronic inflammation of the gastrointestinal tract. Some studies indicate a possible association between IBD and endometriosis.
One study found a 50% increase in the risk of IBD among women with endometriosis. However, the study had a small sample size and the confidence interval was wide, indicating a need for further research.
The Bigger Picture
While the evidence for an association between endometriosis and certain autoimmune diseases is compelling, it’s important to emphasize that correlation or association does not imply causation. Further research is needed to determine whether endometriosis actually increases the risk of developing autoimmune diseases or vice versa, or whether the two share common risk factors or underlying mechanisms.
The potential link between endometriosis and autoimmune diseases highlights the importance of a comprehensive approach to women’s health. For women with endometriosis, being aware of the potential increased risk of autoimmune diseases can inform their healthcare decisions and monitoring.
The Path Ahead
The intersection of endometriosis and autoimmune diseases is a complex and evolving field of research. Better understanding the relationship between these conditions could help improve diagnosis, treatment, and ultimately, the quality of life for patients with endometriosis.
By continuing to explore this connection, we are gaining new insights into the pathophysiology of endometriosis and autoimmune diseases, potentially leading to novel treatments and preventive strategies.
Reference:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6601386/

Pelvic floor dysfunction
Another condition that can have overlapping symptoms with endometriosis is pelvic floor dysfunction (PFD). PFD involves abnormal functioning of the pelvic floor muscles (Grimes & Stratton, 2020). The muscles can be too tight (hypertonia), too lax (hypotonia), or just not coordinate appropriately (Grimes & Stratton, 2020). Fraga et al. (2021) reports that those with deep infiltrating endometriosis (DIE) had higher pelvic floor hypertonia, weaker muscle contraction, and inability to completely relax the pelvic floor muscles. They also noted shortening of the anterior thigh, piriformis, and iliotibial band muscles (Fraga et al., 2021). PFD can be seen frequently in those with endometriosis “even after surgical excision of the endometriosis lesions” (Hunt, 2019).
Shrikhande (2020) reports:
“The presence of endometriosis in the pelvis can cause a secondary chronic guarding of pelvic floor musculature. This chronic guarding state leads to nonrelaxing pelvic floor dysfunction and myofascial trigger points (MTrPs)…. The pelvic floor muscles in nonrelaxing pelvic floor dysfunction are short, spastic, weaker and poorly coordinated…. Myofascial trigger points (MTrPs) are short contracted taut bands of skeletal muscle that often co-exist with nonrelaxing pelvic floor dysfunction… Once formed, MTrPs can become a self-sustaining source of pain even after the endometriosis has been excised. Active MTrPs serve as a source of ongoing nociception; they can decrease pain thresholds, upregulate visceral and referred pain patterns, and sensitize the nervous system contributing to both peripheral and central sensitization. Therefore, it is important to treat a hypertonic nonrelaxing pelvic floor and associated MTrPs in endometriosis patients.”
For more information see: https://icarebetter.com/pelvic-floor-dysfunction
References
Fraga, M. V., Oliveira Brito, L. G., Yela, D. A., de Mira, T. A., & Benetti‐Pinto, C. L. (2021). Pelvic floor muscle dysfunctions in women with deep infiltrative endometriosis: An underestimated association. International Journal of Clinical Practice, 75(8), e14350. DOI: 10.1111/ijcp.14350
Grimes, W. R., & Stratton, M. (2020). Pelvic floor dysfunction. https://www.ncbi.nlm.nih.gov/books/NBK559246/
Hunt, J. B. (2019). Pelvic Physical Therapy for Chronic Pain and Dysfunction Following Laparoscopic Excision of Endometriosis: Case Report. Internet Journal of Allied Health Sciences and Practice, 17(3), 10. Retrieved from https://nsuworks.nova.edu/cgi/viewcontent.cgi?article=1684&context=ijahsp
Shrikhande, A. A. (2020). The consideration of endometriosis in women with persistent gastrointestinal symptoms and a novel neuromusculoskeletal treatment approach. Archives of Gastroenterology Research, 1(3). https://www.scientificarchives.com/article/the-consideration-of-endometriosis-in-women-with-persistent-gastrointestinal-symptoms-and-a-novel-neuromusculoskeletal-treatment-approach

Pelvic Congestion Syndrome- another cause of chronic pelvic pain
When talking about endometriosis and chronic pelvic pain, it is important to remember that often endometriosis is not the only pelvic pain generator. Another possible contributor to chronic pelvic pain is pelvic congestion syndrome (PCS). “Pelvic congestion syndrome (PCS) accounts for up to 30% of patients presenting with chronic pelvic pain” (Reardon & Dillavou, 2021). There isn’t a significant amount of data about endometriosis and PCS, but one study found “the prevalence of ovarian varices in patients with endometriosis was 80%, whereas the control group was only 26.1%” (Pacheco & de Oliveira, 2016).
PCS is like having varicose veins in the pelvis. Blood pulls in the veins and can cause symptoms such as heaviness, pain with penetration, noncyclical pain, positional lower back pain, pelvic and upper thigh pain, prolonged postcoital discomfort, symptoms that worsen throughout the day and are exacerbated by activity or prolonged standing, and non-specific lower abdominal and pelvic pain (Durham & Machan, 2013; Mistry & le Roux, 2017). The cause of PCS is not clear, but it is associated with obstructions such as iliac vein compression (i.e., MTS) or left renal vein compression (i.e., Nutcracker syndrome) (Reardon & Dillavou, 2021).
For more information see: https://icarebetter.com/pelvic-congestion-syndrome/
References
Durham, J. D., & Machan, L. (2013, December). Pelvic congestion syndrome. In Seminars in interventional radiology (Vol. 30, No. 04, pp. 372-380). Thieme Medical Publishers. Retrieved from https://www.thieme-connect.com/products/ejournals/html/10.1055/s-0033-1359731
LIANG, D. E., & Brown, B. (2021). Pelvic congestion syndrome: Are we missing the diagnosis?. The Medical Republic. Retrieved from https://www.sydneyfibroidclinic.com.au/app/uploads/2021/06/PCS-Medical-Republic.pdf
Mistry, P. P., & le Roux, D. A. (2017). Pelvic congestion syndrome (PCS). Practice Perspectives for Venous Disorders, 46. Retrieved from http://www.vascularsociety.co.za/wp-content/uploads/2019/02/VASSA-venous-guidelines-Practice-perspectives-for-venous-disorders-2017.pdf#page=46
Pacheco, K. G., & de Oliveira, M. R. F. (2016). The prevalence of ovarian varices in patients with endometriosis. Annals of Vascular Surgery, 34, 135-143. https://www.annalsofvascularsurgery.com/article/S0890-5096(16)30232-1/fulltext
Reardon, E. S., & Dillavou, E. D. (2021). Venous disease—What we still do not know. In Vascular Disease in Women (pp. 157-163). Academic Press. https://www.sciencedirect.com/science/article/pii/B9780128229590000031
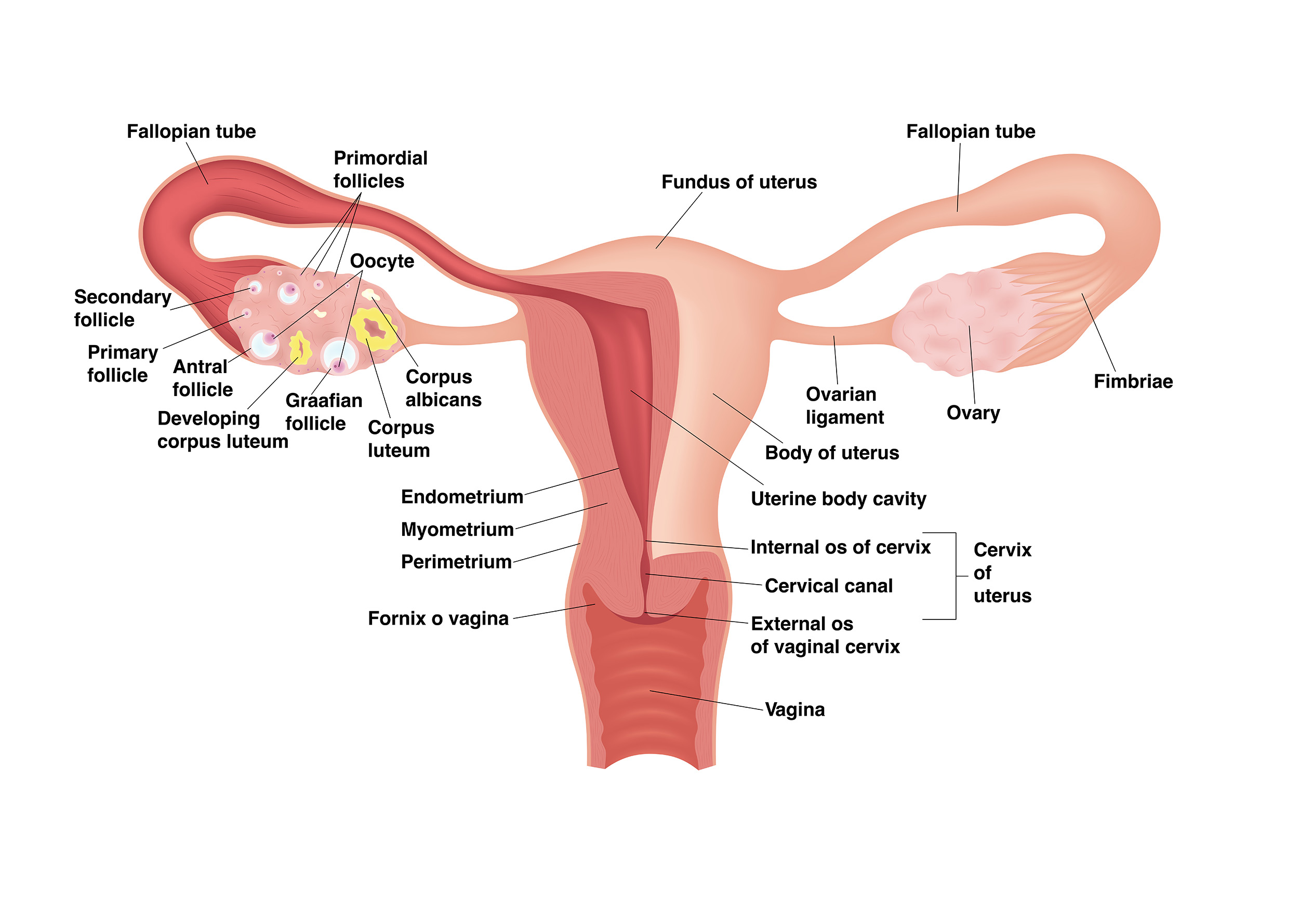
Fibroids
We have been looking at some of the related conditions that can cause overlapping symptoms with endometriosis. This is important because, if you only treat one condition and not the others, this can lead to continued symptoms and a great deal of discouragement. Another condition with overlapping symptoms with endometriosis is uterine fibroids (leiomyomas).
Fibroids are benign tumors of the smooth muscle cells of the uterus with symptoms that can range from being asymptomatic to having “abnormal uterine bleeding, specifically in terms of heavy and prolonged bleeding” as well as pain with penetration and non-cyclic pelvic pain (Zimmermann et al., 2012). They can also affect fertility and cause urinary dysfunction (Fortin, Flyckt, & Falcone, 2018).
There has not been much research on the correlation between endometriosis and fibroids. One study reports “an incidence of concomitant fibroids and endometriosis ranging between 12 and 20%, based on 2 previously published studies” (Nezhat et al., 2016). A small study that looked at patients with abnormal uterine bleeding found that “of the 208 patients with the presenting chief concern of symptomatic leiomyoma and who underwent surgical therapy, 181 had concomitant diagnoses of leiomyoma and endometriosis” (Nezhat et al., 2016). Another study looking at those with infertility found (by using ultrasound findings) the “diagnosis of fibroids was made in 3.1% of cases, adenomyosis was found in 21.2%, and the co-existence of both uterine disorders with endometriosis was reported in 14.6% of patients” (Capezzuoli et al., 2020). Nezhat et al. (2016) states that “because of the significant overlap of symptoms, it is often difficult to discern which pathology is responsible for the patient’s complaints” and recommends “a high level of suspicion for endometriosis before and during surgery in these women, with the goal of treating both pathologies in a single surgery.”
For more information see: https://icarebetter.com/fibroids/
References
Capezzuoli, T., Vannuccini, S., Fantappiè, G., Orlandi, G., Rizzello, F., Coccia, M. E., & Petraglia, F. (2020). Ultrasound findings in infertile women with endometriosis: evidence of concomitant uterine disorders. Gynecological Endocrinology, 36(9), 808-812. https://doi.org/10.1080/09513590.2020.1736027
Fortin, C., Flyckt, R., & Falcone, T. (2018). Alternatives to hysterectomy: the burden of fibroids and the quality of life. Best Practice & Research Clinical Obstetrics & Gynaecology, 46, 31-42. https://www.sciencedirect.com/science/article/abs/pii/S1521693417301487
Nezhat, C., Li, A., Abed, S., Balassiano, E., Soliemannjad, R., Nezhat, A., … & Nezhat, F. (2016). Strong association between endometriosis and symptomatic leiomyomas. JSLS: Journal of the Society of Laparoendoscopic Surgeons, 20(3). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5019190/
Zimmermann, A., Bernuit, D., Gerlinger, C., Schaefers, M., & Geppert, K. (2012). Prevalence, symptoms and management of uterine fibroids: an international internet-based survey of 21,746 women. BMC women’s health, 12(1), 1-11. https://link.springer.com/article/10.1186/1472-6874-12-6

Endometrial Polyps
The last couple of weeks, we have seen that adenomyosis and interstitial cystitis are found frequently in those with endometriosis and can cause similar symptoms. Another finding noted in those with endometriosis is endometrial (uterine) polyps. One meta-analysis found a significantly higher risk of endometrial polyps (EP) in those with endometriosis (Zheng et al., 2015). These polyps are overgrowths of endometrial glands and stroma (Zheng et al., 2015). While they may not cause any symptoms, they can cause abnormal menstrual bleeding, bleeding between menstrual periods, vaginal bleeding after menopause, and might affect fertility.
Zheng et al. (2015) notes that, like in endometriosis, the expression of estrogen receptors and aromatase (an enzyme that converts androgens to estrogens) is altered in endometrial polyps and can increase the local concentration of estrogen. The authors suggest that “it is important to determine whether patients with endometriosis also have EP and then remove any coexisting EP via hysteroscopy, especially for infertile patients” (Zheng et al., 2015).
For more information on endometrial polyps, see: https://icarebetter.com/endometrial_uterine-polyps/
Reference
Zheng, Q. M., Mao, H. L., Zhao, Y. J., Zhao, J., Wei, X., & Liu, P. S. (2015). Risk of endometrial polyps in women with endometriosis: a meta-analysis. Reproductive biology and endocrinology, 13(1), 1-9. https://link.springer.com/article/10.1186/s12958-015-0092-2

