Understanding How Endometriosis Can Cause Bowel Problems
Endometriosis, a common health concern among women, can manifest itself in various ways, one of them being bowel problems. But how exactly can endometriosis cause bowel problems? This article will take you through the intricate connection between endometriosis and bowel problems, the symptoms to look out for, diagnostic procedures, and potential treatments.
Table of contents
What is Endometriosis?
Endometriosis is a health condition where the tissue similar to the type that lines the uterus, known as the endometrium, grows outside the uterus. This condition predominantly affects the reproductive organs such as the ovaries, fallopian tubes, and the external part of the uterus. However, it can also extend to other parts of the body including the bowels, rectum, and other pelvic organs.
Understanding Bowel Endometriosis
Bowel endometriosis is a form of endometriosis that affects the gastrointestinal tract, specifically the bowels. It can appear in two forms: superficial (on the surface of the bowel) and deep (penetrating the bowel wall).
Read More: Understanding Bowel Endometriosis
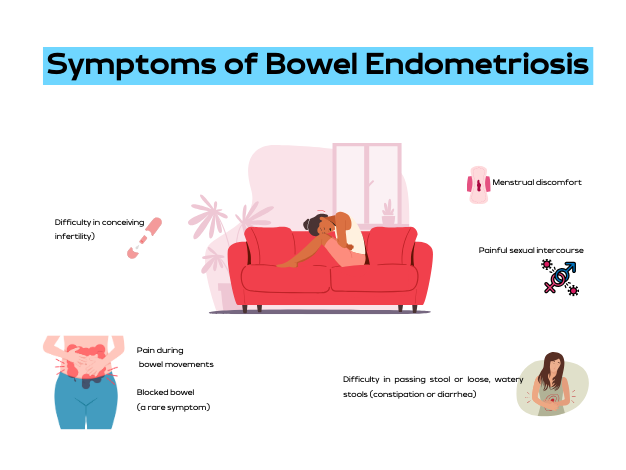
Symptoms of Bowel Endometriosis
The symptoms of bowel endometriosis can vary widely depending on the location of the lesion, its size, and how deep it is in the bowel wall. Some women may experience no symptoms. However, common symptoms include:
- Difficulty in passing stool or loose, watery stools (constipation or diarrhea)
- Pain during bowel movements
- Menstrual discomfort
- Painful sexual intercourse
- Difficulty in conceiving (infertility)
- Blocked bowel (a rare symptom)
It is noteworthy that these symptoms can often mimic other conditions like irritable bowel syndrome (IBS), but the two conditions are distinct. One distinguishing factor is that with bowel endometriosis, symptoms often worsen before and during the menstrual period.
Read More: Endometriosis and Painful Intercourse: Is it Really Just Endometriosis?
Causes of Bowel Endometriosis
The exact cause of bowel endometriosis is still under study. However, several factors have been linked to its occurrence. These include genetic predisposition, inflammation, and levels of estrogen, a female sex hormone.
The Prevalence of Endometriosis
Endometriosis affects approximately 10%-12% of women of childbearing age. The condition is often diagnosed in women who are in their 30s, although it can occur at any age.
Diagnosing Bowel Endometriosis
The diagnosis of bowel endometriosis starts with the doctor asking about your symptoms and medical history, followed by a physical examination of your pelvic area. The doctor may also recommend imaging tests to get more information on the location and size of any cysts or tissue damage related to endometriosis. These tests include:
- Transvaginal or transrectal ultrasound: This procedure involves the insertion of a wand-like device into your vagina or rectum. This device releases sound waves that create images of your organs.
- Magnetic resonance imaging (MRI): An MRI test provides detailed images of your organs and tissues using a magnetic field and radio waves.
- Laparoscopy: This surgical procedure involves making a small incision near your belly button and inserting a thin viewing tool called a laparoscope.
- Barium enema: This type of X-ray is used to see changes or defects in your large intestine (colon).
- Colonoscopy: They pass a tube with a camera on its tip through the anus into the colon to directly visualize the wall and take samples from inside the colon.
Read More: Colon Chronicles: Delving into Bowel Endometriosis
Treating Bowel Endometriosis
The treatment plan for bowel endometriosis will be personalized, taking into account your symptoms, medical history, age, and reproductive plans. Treatments can include:
- Surgery: The aim of surgery is to remove as many lesions as possible while preserving your organs and overall health.
- Hormone treatments: These medications control estrogen levels which can worsen the symptoms of bowel endometriosis.
- Counseling: Given the ongoing nature of bowel endometriosis and its impact on both physical and mental health, counseling may be recommended to provide emotional support.
The Prognosis for Bowel Endometriosis
There is currently no cure for endometriosis. However, treatments like surgery and hormone therapy can help manage the symptoms. It is also important to note that symptoms could return if treatment is halted, or they could recur on their own, especially in cases with deep lesions.
Endometriosis is a complex condition that can cause bowel problems and other health issues. If you suspect you have endometriosis and are experiencing bowel problems, it’s important to consult with a healthcare provider. Early diagnosis and treatment can help manage symptoms and improve your quality of life.
References:
https://www.webmd.com/women/endometriosis/bowel-endometriosis
https://www.endometriosis-uk.org/endometriosis-and-bowel
https://www.endofound.org/gastrointestinal-distress
ENDOMETRIOSIS AND CONSTIPATION

Anti-Mullerian Hormone & Endometriosis – What’s The Connection?
Endometriosis has been associated with a marker called Antimullerian hormone (AMH), which is a pivotal marker of ovarian reserve, and is commonly measured in women with endometriosis specifically in relation to fertility. There is debate among the community that your AMH level is what it is and it cannot change. I would challenge this notion though as I have seen people with endometriosis have significant increases after proper excision surgery, which is a point of debate. Recently, I had another patient send me lab work that demonstrated what some may call a low AMH, has confirmed endometriosis, but likely a surgery that was incomplete and is continuing to suffer ongoing symptoms. Though I have seen this change in my patients, I recognize this is only a small fraction of the people suffering, so it was time to review what the research says. This article aims to provide a review of the various studies conducted on this critical subject, exploring how endometriosis and AMH interact, the effect of surgical intervention on AMH levels, and the subsequent impact on fertility.
Table of contents
The Antimullerian Hormone (AMH): A Brief Overview
AMH, a hormone playing diverse roles during embryonic development and puberty, is produced by ovarian follicles smaller than 8 mm, hence linking ovarian reserve to AMH levels in the blood. The normal range for AMH hovers between 1 and 4 ng/mL. However, women’s AMH levels greatly vary based on factors like age, ethnic background, lifestyle, and genetics. Additionally, someone at the low end of range may still suffer problems despite them being “in range.”
AMH Testing in Reproductive Health
AMH testing is a crucial tool for evaluating female fertility. It can assist in:
- Assisting with understanding the prognosis of a woman’s response to assisted reproduction techniques (ART) such as in vitro fertilization (IVF)
- Confirming other markers of menopause
- Providing a more comprehensive evaluation when certain conditions are confirmed or suspected such as polycystic ovarian syndrome (PCOS), premature ovarian failure, and endometriosis
Endometriosis and AMH Levels
Endometriosis is a common culprit behind infertility, affecting nearly half of the women suffering from this ailment. This infertility arises from various factors, including inflammation in the reproductive tract, scar tissue-induced decreased blood supply to the ovaries, and pelvic anatomical distortions. Research reveals a significant correlation between endometriosis and lower than average AMH levels.
Some argue that surgical intervention of endometriosis often leads to a reduction in AMH levels, though many of us in the community may argue that this is a more nuanced topic and this highly depends on the skill of the surgeon, something that is often overlooked in endometriosis research. Various studies have attempted to decipher the impact of endometriosis surgery on AMH levels and fertility outcomes. A retrospective study conducted in 2016 found that preoperative AMH levels did not influence pregnancy rates after surgery. This is consistent with the literature we have on surgical impact, and thus the need for better research in the future. In my experience, this is the opposite of what I have seen, as many of us have seen when people get to the right surgeon.
Laparoscopic Cystectomy on AMH Levels
Laparoscopic ovarian cystectomy, a common surgical procedure to treat endometriomas, has been associated with decreased ovarian reserve. A study in 2019 demonstrated significantly lower AMH levels in women who underwent laparoscopic endometrioma cystectomy, especially in cases with bilateral cysts larger than 7 cm and stage 4 endometriosis.
Considerations: I want to highlight that we do not know the skill of the surgeon, but we do know that the skill of the surgeon matters. That being said, large endometriomas can often overtake ovarian tissue which is what happened to Christina. Hear her story here. This is why it is extremely important to find a knowledgeable surgeon that you feel comfortable with. If you need help finding a surgeon, you can start here.
Laparoscopic Endometriosis Surgery on AMH Levels
A literature review and meta-analysis of 19 studies conducted between 2010 and 2019 on the impact of laparoscopic endometriosis surgery on AMH levels post-surgery revealed a decline in AMH levels, extending beyond six months post-surgery. This decline was more pronounced in cases where surgery was performed on both sides of the body, compared to a single side.
Again, I would argue that we consider the quality of the research and the skill of the surgeon. Remember, ablation is different from excision and this may be another factor that is skewing results. I repeat this because, like many of us in the community, this is not our experience, thus I often read research with these things in mind. If many others in the community are also seeing this, there must be more to consider than what is presented. The bottom line is that we need better research.
AMH Levels Post-Surgery for Endometrioma
Several studies have observed that laparoscopic ovarian cystectomy results in a significant and progressive decrease in AMH levels post-surgery. However, other studies have noted that this decrease may only be temporary, with levels potentially returning to normal within a year. Another factor to consider is when the AMH was measured post-surgery and what other factors may have impacted the levels!
Certain studies have observed a temporary decrease in AMH levels following endometrioma ablation. However, this decrease did not persist beyond six months in most cases, suggesting a potential recovery of ovarian reserves.
Several studies have compared the decrease in AMH levels following ovarian cystectomy and endometrioma vaporization. The general consensus suggests a higher postoperative decline in AMH levels following cystectomy compared to vaporization, particularly in bilateral endometrioma cases.
This caught my attention and highlights my thoughts on how the surgery (excision) is being performed as to not compromise ovarian tissue. Using ablation, which is what the CO2 laser is referring to, may not compromise the ovarian tissue, but it also may not treat the disease. Paul Tyan, MD discusses this complex topic in our interview which you can find here.
The combined technique, involving partial cystectomy and ablation, has been shown to have less detrimental effects on the ovary, resulting in a lesser decline in AMH levels post-surgery.
The role of endometriosis surgery in improving pregnancy rates remains a topic of debate. Some studies suggest that surgery might improve the success rates of fertility treatment, while others highlight the risk of ovarian damage due to surgical intervention.
In conclusion, the Antimullerian hormone is a vital marker for assessing the impact of endometriosis and its surgical intervention on ovarian reserve and fertility. Understanding the complex relationship between AMH levels, endometriosis, and surgical intervention along with identifying gaps in the research can help medical professionals devise more effective treatment strategies, improve the quality of research studies which ultimately improves patient outcomes.
IRelated Reading:
- Does Endometriosis Cause Infertility? Covering the Basics
- Endometriosis and Pregnancy: Natural, Medical, & Surgical Options
References:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6603105/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7865255/
- https://drseckin.com/endometriosis-surgery-and-amh-levels/
Endometriosis and Inflammatory Bowel Disease: Distinguishing the Differences
Exploring the complex world of health and medical conditions can sometimes feel like navigating through a labyrinth. The similarities between certain conditions often blur the lines, making it challenging for individuals and even healthcare professionals to differentiate between them. This is notably true in the case of endometriosis and inflammatory bowel disease (IBD), two disorders that share several overlapping symptoms and characteristics. We’ve recently been discussing endometriosis and the bowel, this article aims to shed light on these conditions, highlighting the differences, similarities, and the challenges faced in their diagnosis.
Table of contents
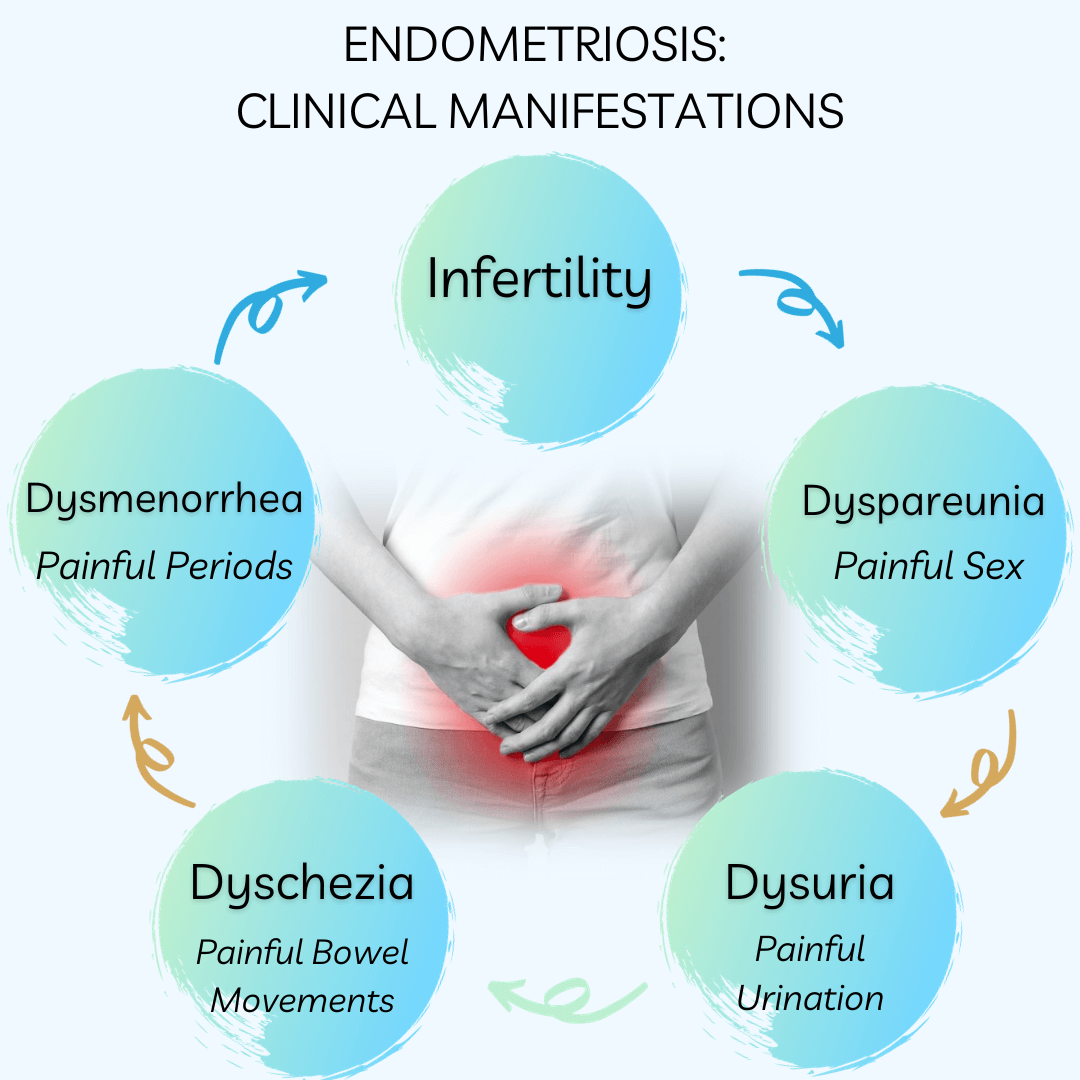
Symptoms of Endometriosis
The signs and symptoms of endometriosis can vary greatly, making it a complex disease to diagnose. Some of the most common symptoms include dysmenorrhea (painful periods), dyspareunia (painful intercourse), chronic pelvic pain, and gastrointestinal symptoms like diarrhea, constipation, and abdominal pain. Because endometriosis symptoms often overlap with GI symptoms, getting a diagnosis in general can be tricky, but especially if it may be impacting the bowels which is estimated in about 5-12% of cases, whereas approximately 90% of those with endometriosis suffer from gastrointestinal symptoms. In many cases, these symptoms can be mistaken for other conditions, leading to delays in diagnosis.
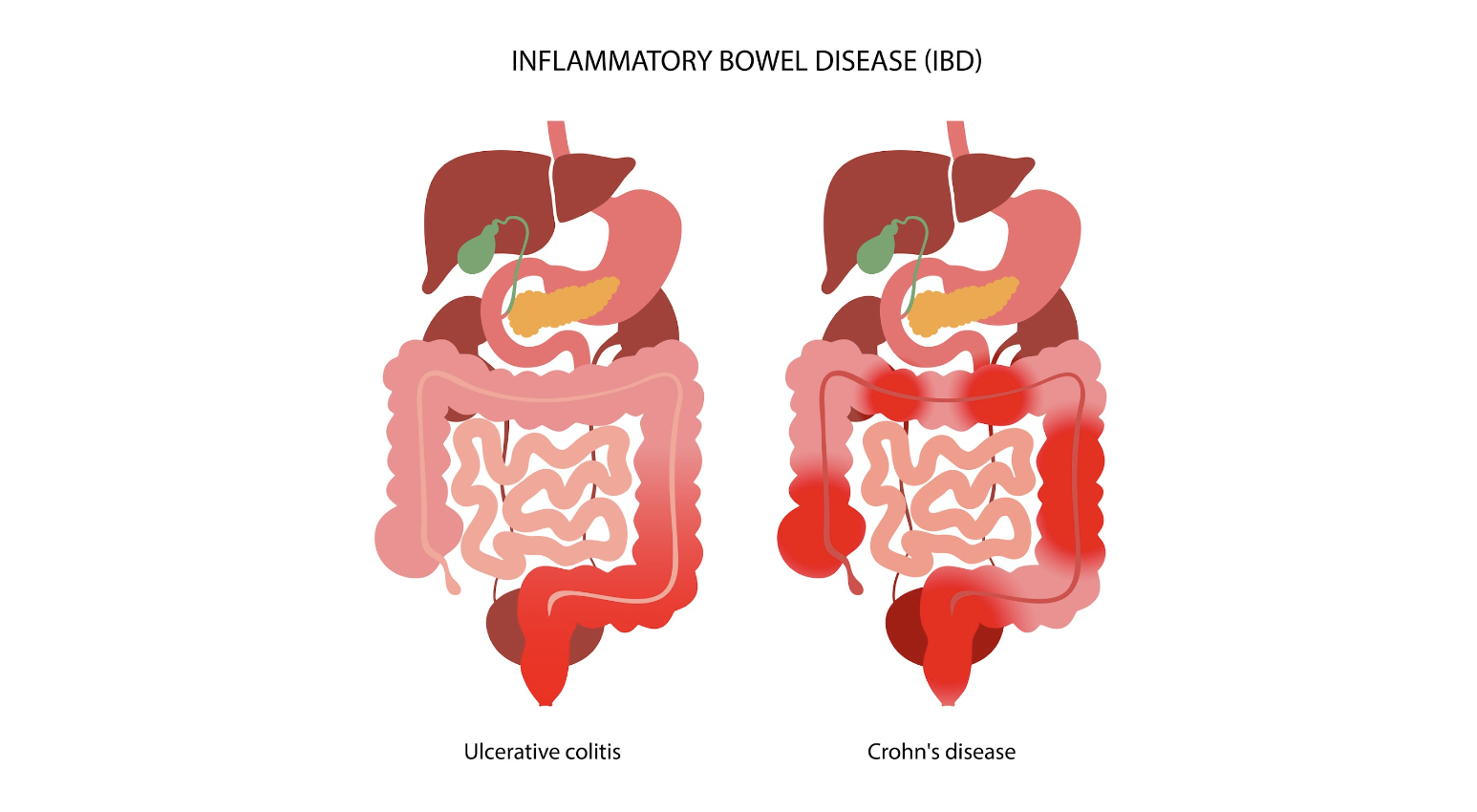
Inflammatory Bowel Disease: An Overview
Inflammatory bowel disease (IBD) is an umbrella term that encompasses two chronic autoimmune disorders: ulcerative colitis (UC) and Crohn’s disease (CD). These conditions are characterized by the chronic inflammation of the gastrointestinal tract, which can lead to a wide range of symptoms, including abdominal pain, diarrhea, weight loss, and fatigue.
The prevalence of IBD is highest in Europe, with reported cases reaching up to 505 per 100,000 for UC in Norway and 322 per 100,000 for CD in Italy. Like endometriosis, IBD can significantly impact an individual’s quality of life, necessitating long-term management strategies to control symptoms and prevent complications.
The Overlap: Endometriosis and IBD
Interestingly, endometriosis and IBD share several common traits, including immune dysregulation and overlapping clinical manifestations like abdominal pain and bowel-related symptoms. This overlap often poses a significant diagnostic challenge, as endometriosis can mimic IBD or vice versa, leading to delays or indeterminate diagnosis.
In fact, endometriosis has often been termed as having “IBD-like” features due to the similarities in symptoms and underlying pathophysiology. This has led to substantial interest in the potential link between these conditions, with several studies investigating the co-occurrence of endometriosis and IBD.
Investigating the Link: Endometriosis and IBD
To understand the potential link between endometriosis and IBD, numerous studies have been conducted, ranging from case reports and clinical series to epidemiological research. These studies have reported varying results, further highlighting the complexity of these conditions and the challenges associated with their diagnosis and management.
Case Reports and Clinical Series
Many case reports have been published that highlight the diagnostic challenges associated with endometriosis and IBD. For instance, several cases have been reported where an initial diagnosis of CD was later revised to intestinal endometriosis upon histopathological examination. Similarly, other case reports have documented instances where an initial diagnosis of UC was later confirmed to be appendiceal endometriosis.
Conversely, there have also been cases where an initial diagnosis of endometriosis was later revised to be CD upon histopathological examination. Additionally, several case reports have documented instances where both CD and endometriosis were diagnosed in the same patient.
Epidemiological Studies
In addition to case reports and clinical series, several epidemiological studies have investigated the co-occurrence of endometriosis and IBD. One such study, a nationwide Danish cohort study, reported a 50% increase in the risk of IBD in women with endometriosis compared to the general population. This increased risk persisted even more than 20 years after a diagnosis of endometriosis, suggesting a genuine association between the two conditions..
Another study, a retrospective cross-sectional study conducted in Israel, found that 2.5% of patients with endometriosis also had a diagnosis of IBD, compared to 1% in the general population. A recent Italian case-control study found that among 148 women with endometriosis, five had IBD, although this did not reach statistical significance.
The Challenge of Temporality
One of the critical aspects of evaluating the association between endometriosis and IBD is the issue of temporality, or the order in which the conditions are diagnosed. Many studies do not provide information on the temporal sequence of endometriosis and IBD, which poses a significant challenge in determining a cause-effect relationship between the two conditions.
Furthermore, the diagnosis of endometriosis often faces delays, with an average delay of seven years estimated between the onset of symptoms and definitive diagnosis. This delay further complicates the evaluation of the temporal relationship between endometriosis and IBD.
Distinguishing Between Endometriosis and IBD
Given the overlapping symptoms and shared characteristics of endometriosis and IBD, distinguishing between these conditions can be challenging. Both conditions can result in similar symptoms, such as abdominal pain and bowel-related symptoms, which can lead to misdiagnosis or delayed diagnosis.
In cases where endometriosis and IBD coexist, the symptoms can be atypical and cyclic, and fibrosis caused by chronic inflammation can lead to obstruction of the intestinal lumen. Therefore, it’s essential for healthcare professionals to consider both conditions when evaluating patients with such symptoms.
In cases of intestinal endometriosis, endoscopic biopsies may reveal IBD-like lesions. However, these lesions may represent an epiphenomenon of endometriosis rather than a true IBD. Hence, patients with concurrent IBD and endometriosis should be adequately followed up for the reassessment of IBD diagnosis over time.
The Role of Treatment in the Risk of IBD
The treatment of endometriosis could potentially influence the risk of developing IBD. For instance, oral contraceptives are a common treatment for endometriosis, and a meta-analysis of 14 studies suggested an increased risk of IBD among users of oral contraceptives. Additionally, non-steroidal anti-inflammatory drugs (NSAIDs), often used for pain relief in endometriosis, have been reported to increase the risk of IBD.
The Need for Further Research
Though existing research has shed some light on the association between endometriosis and IBD, there is still much to uncover. Further research is needed to better understand the temporal relationship between endometriosis and IBD in cases of co-occurrence and identify predictors that could be useful for evaluation and management of these patients.
Understanding these conditions and their potential links can not only improve diagnostic accuracy but also inform treatment strategies and improve the quality of life for those affected.
Distinguishing between endometriosis and inflammatory bowel disease can be a challenging task due to the overlapping symptoms and shared characteristics of these conditions. However, understanding the nuances of these conditions and the potential links between them can lead to improved diagnostic accuracy and more effective treatment strategies. As research progresses in this area, we hope to gain a better understanding of these complex conditions and continue to improve the lives of those affected.
Related Reading:
- Finding an Endometriosis Specialist: Your Guide to Effective Treatment
- Unraveling the Connection Between Endometriosis and Autoimmune Diseases
References:
- Parazzini F, Luchini L, Vezzoli F, Mezzanotte C, Vercellini P. Gruppo italiano perlo studio dell’endometriosi. Prevalence and anatomical distribution of endometriosisin women with selected gynaecological conditions: results from amulticentric Italian study. Hum Reprod 1994;9:1158–62.
- Bulun SE. Endometriosis. N Engl J Med 2009;360:268–79.
- Weed JC, Ray JE. Endometriosis of the bowel. Obstet Gynecol 1987;69:727–30.
- Molodecky NA, Soon IS, Rabi DM, Ghali WA, Ferris M, Chernoff G. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology 2012;142:46–54.
- Nielsen NM, Jorgensen KT, Pedersen BV, Rostgaard K, Frisch M. The co-occurrence of endometriosis with multiple sclerosis, systemic lupus erythematosus and Sjogren syndrome. Hum Reprod 2011;26:1555–9.

Rediscovering Life After Endometriosis Surgery: Tips and Strategies for a Full Recovery
Endometriosis surgery, typically excision of endo implants and related fibrosis, using minimally invasive laparoscopy or robotic surgery, significantly impacts women’s health and recovery journey. Here’s an enhanced guide to life post-surgery, incorporating tips to improve physical and mental healing towards lasting thrivorship.
Table of contents
Understanding Endometriosis and Its Surgical Treatment

Endometriosis involves the growth of tissue similar to the uterine lining outside the uterus, creating pain and sub-fertility. Thankfully, minimally invasive surgery requires only small incisions through which a camera and instruments can be placed. This is the gold standard for diagnosing and treating endometriosis and has revolutionized the healing process and length of time to full recovery. (Ferrero et al., 2018).
The Recovery Period
Recovery from laparoscopic or robotic minimally invasive surgery varies based on the extent of endometriosis and overall health. Typically, full recovery involves several weeks to a few months. Patients might experience tiredness initially and are advised to consume soft foods, stay hydrated, and take fiber supplements to avoid constipation, especially when using narcotic pain relief. It’s crucial to initially avoid strenuous activities but engage in light walks to promote healing. This reduces the risk of venous clots in the legs but avoids complications like hernias through the incisions.
How long you should take off work depends on the extent of the surgery, physical job demands, and any known medical co-existing conditions that might slow the healing process, such as diabetes. Discuss this with your surgeon before the procedure to set realistic expectations.
Enhanced Recovery Tips
- Balanced Nutrition: Within limits of allergies and food intolerance which may be specific to you, the following is a generic prudent healing plan:
- Protein: Lean meats, fish, eggs, tofu, and legumes help repair tissues.
- Fruits and Vegetables: Rich in vitamins, minerals, and antioxidants to reduce inflammation.
- Whole Grains: Brown rice, quinoa, and whole wheat bread for energy and fiber.
- Healthy Fats: Avocados, nuts, seeds, and olive oil for inflammation control.
- Hydration: Plenty of water, green and herbal teas.
- Bromelain Supplements: Bromelain, an enzyme found in pineapples, can reduce inflammation and promote healing by minimizing post-surgical scarring (Walker et al., 2018).
- Arnica: Homeopathic arnica can help reduce bruising and swelling, and may reduce pain as well.
- Vitamin C and Zinc: Essential for tissue repair and immune function.
- Probiotics: Support gut health, which can be disrupted by surgery, antibiotics used around the time of surgery, and pain medications.
- Red Light Therapy: Otherwise known as photobiomodulation, this modality can exert and anti-inflammatory effect, reducing prolonged inflammation and thereby can promote healing. Keep in mind, acute inflammation is part of normal healthy healing, so it may be prudent to avoid this for at least a month postop. (Hamblin MR)
Physical Health Post-Surgery
Post-surgery, physical health generally improves, with reduced bodily pain and better physical functioning. However, side effects like hot flashes can occur, particularly if the ovaries are removed or compromised and/or hormonal treatments are part of the post-surgery plan. Regular follow-ups are essential to monitor recovery and address any complications promptly. This is a highly individualized situation, so work with an expert before and after surgery.
Pain Management
- Heat Therapy: Use heating pads to alleviate abdominal pain. Be careful not to burn skin by not using something like a towel between the heat source and the skin.
- TENS Units: Transcutaneous Electrical Nerve Stimulation can help manage pain by sending small electrical pulses to the affected areas.
- Acupuncture: Can relieve pain and promote healing.
Mental Health Post-Surgery
Mental health is a crucial aspect of recovery. Enduring a chronic condition like endometriosis can lead to anxiety and depression. Therefore, incorporating mental health support into post-surgery care can be vital. Many women report improved emotional well-being post-surgery, but not all. So ongoing support may be necessary to manage any lingering psychological effects (Stratton et al., 2020).
Mental Health Tips
- Therapy and Counseling: Cognitive-behavioral therapy (CBT) can be effective.
- Mindfulness and Meditation: Practices like yoga and meditation can help manage stress and improve mental clarity.
- Support Groups: Joining endometriosis support groups can provide emotional support and practical advice.
Fertility and Family Planning
Fertility and family planning are significant concerns for many women with endometriosis. Studies show that surgery could double the spontaneous pregnancy rate in people with mild endometriosis. Those with moderate to severe endometriosis also have improved spontaneous birth rates after the laparoscopic removal of endometrial-like lesions.
However, even after successful surgery, some women may struggle with fertility issues. It is essential to have a candid discussion about fertility and family planning with your healthcare provider before surgery.
Financial Considerations
Endometriosis surgery can be financially burdensome. Many specialists are out-of-network, leading to high out-of-pocket costs in many, but not all, cases. It’s best to discuss potential expenses with your insurance provider and surgeon’s office beforehand. Additionally, explore options like payment plans or grants for financial support.
Managing Recurrence
Despite effective surgery, endometriosis can recur. Studies indicate a 51% recurrence rate within ten years. However, it can be in the 5-10% range if complete excision of visible implants is possible. This may require additional interventions that are often hormonally based but can also be integrative and holistic to some degree. Risk factors for recurrence include age, ovarian endometriosis, incomplete removal of lesions, and the initial surgeon’s expertise. Regular monitoring and follow-up surgeries may be required to manage recurrences effectively. It is very prudent to find the most experienced and highly trained surgeon possible. Here is a review of what you should be looking for in selecting a surgeon.
Prevention Strategies
- Hormonal Treatments: Birth control pills, gonadotropin-releasing hormone (GnRH) agonists, and other hormonal therapies can help prevent recurrence but may also carry significant and prolonged side effects. In general, the least potentially harmful option should be considered first and this should be highly individualized with your endo expert and/or reproductive endocrinologist.
- Lifestyle Modifications: Maintaining a healthy diet, avoiding toxins and regular exercise can support overall health and reduce the risk of recurrence by modulating and more efficiently eliminate excess estrogen in your system.
- Anti-inflammatory Diet: Incorporate foods rich in omega-3 fatty acids and antioxidants to reduce inflammation. It is best to craft a personalized plan with a nutrition expert.
Holistic Approaches
- Herbal Supplements: Consider supplements like turmeric, which has anti-inflammatory properties.
- Aromatherapy: Essential oils like lavender and peppermint can aid in relaxation and pain relief.
Conclusion
Quality of life after endometriosis surgery involves a multifaceted approach to physical and mental health, fertility, and financial planning. By understanding the recovery process and incorporating comprehensive care strategies, women can optimally navigate their post-surgery journey. Work with an endometriosis expert.
References
- Ferrero S, Evangelisti G, Barra F. Current and Emerging Treatment Options for Endometriosis. Expert Opin Pharmacother. 2018;19(11):1109-1125. doi:10.1080/14656566.2018.1507067. https://pubmed.ncbi.nlm.nih.gov/30096049/
- Vercellini P, Buggio L, Frattaruolo MP, Borghi A, Dridi D, Somigliana E. Medical treatment of endometriosis-related pain. Best Pract Res Clin Obstet Gynaecol. 2018;51:68-91. doi:10.1016/j.bpobgyn.2018.06.001. https://pubmed.ncbi.nlm.nih.gov/30126775/
- Zondervan KT, Becker CM, Missmer SA. Endometriosis. N Engl J Med. 2020;382(13):1244-1256. doi:10.1056/NEJMra1810764. https://pubmed.ncbi.nlm.nih.gov/32212520/
Updated Post: July 09, 2024

Understanding Bowel Endometriosis
Bowel Endometriosis is a debilitating chronic health condition that affects a significant number of women worldwide. This disease is characterized by the growth of endometrial-like tissue outside the uterus, specifically on or inside the bowel walls. The condition often presents with varying gastrointestinal symptoms like painful bowel movements, constipation, and diarrhea, making it difficult to diagnose.
Table of contents
What is Bowel Endometriosis?
Bowel Endometriosis is a specific form of endometriosis that involves the intestines. In this condition, cells similar to those that line the uterus start growing on the bowel or even penetrate into the bowel wall. This growth can lead to painful and uncomfortable symptoms, particularly during a woman’s menstrual cycle.
Prevalence and Affected Areas
Bowel Endometriosis is a subset of a larger condition, endometriosis, affecting 1 in 5 endo patients. The most common sites for bowel involvement are the rectum, appendix, sigmoid, cecum, and distal ileum. It’s also worth noting that bowel endometriosis frequently co-exists with endometriosis in other areas, making it a multifaceted disease that requires comprehensive treatment.
Symptoms of Bowel Endometriosis
Understanding the symptoms of bowel endometriosis can help in early diagnosis and treatment. It’s essential to note that these symptoms often overlap with other gastrointestinal conditions, making it a challenging disorder to diagnose.
Common Symptoms of Endometriosis
- Painful bowel movements: This is one of the most common symptoms of bowel endometriosis. The pain is often described as sharp or cramping and may worsen during menstruation.
- Constipation and Diarrhea: Changes in bowel habits are another common symptom. Some women may experience constipation, while others may have diarrhea. These symptoms may also worsen during menstruation.
- Rectal Bleeding: While not as common, some women may experience rectal bleeding, particularly during their menstrual period. A healthcare professional should always evaluate this symptom as it can also be a sign of other serious conditions.
- Abdominal Pain: Abdominal pain, often worsening during the menstrual cycle, is another common symptom. The pain can range from mild to severe and may be constant or intermittent.
- Dyspareunia: Dyspareunia, or painful sex, is another symptom that may indicate the presence of bowel endometriosis. This pain often stems from endometriosis lesions in the posterior pelvic compartment peritoneum, an area around the rectum that includes the surface peritoneum, commonly called the pouch of Douglas.
Diagnosing Bowel Endometriosis
Diagnosing bowel endometriosis can be challenging due to the overlap of symptoms with other gastrointestinal disorders. However, several diagnostic tools can aid in the identification of this condition.
Physical Examination and Patient History
A detailed patient history and a thorough physical examination are crucial first steps in diagnosing bowel endometriosis. The doctor will ask about the symptoms, their severity, and if they worsen during menstruation. A pelvic exam may also be performed to check for any abnormalities.
Imaging Tests
Imaging tests, such as transvaginal sonography (TVS) and magnetic resonance imaging (MRI), are commonly used to identify and characterize endometriosis lesions.
TVS is a first-line imaging technique providing detailed dynamic images of the pelvis with minimal patient discomfort. It helps identify all of the bowel’s layers and any potential endometriosis nodules.
MRI, on the other hand, is typically used as a second-line diagnostic tool. It excels in evaluating the extent of the disease and identifying any specific organ involvement and depth of infiltration.
Endoscopy and Biopsy
An endoscopy may also be performed to examine the bowel for any abnormalities. A biopsy can be taken during this procedure to check for the presence of endometriosis cells. However, this method has its limitations as it only provides a superficial sample, and endometriosis usually involves deeper layers of the bowel wall.
Laparoscopy
Laparoscopy is the gold standard for diagnosing endometriosis. This surgical procedure allows for visual inspection of the peritoneal cavity and can provide a definitive diagnosis. The surgeon can also assess the extent of the disease and its impact on other organs.
Misdiagnosis of Bowel Endometriosis
Bowel endometriosis is often misdiagnosed due to its similar symptoms to other gastrointestinal disorders. This condition is frequently mistaken for irritable bowel syndrome (IBS), Crohn’s disease, and even colon cancer.
It’s crucial for healthcare providers to consider a possible diagnosis of bowel endometriosis in women presenting with gastrointestinal symptoms, especially if these symptoms worsen around the menstrual cycle.
Treatment of Bowel Endometriosis
Treating bowel endometriosis is typically multidisciplinary, involving a team of specialists. It generally involves a combination of medical and surgical therapies.
Medical Therapy
Medical treatments aim to control the symptoms of bowel endometriosis and may include pain relievers, hormonal therapies like oral contraceptives or progestins, and gonadotropin-releasing hormone analogs. These treatments work by reducing inflammation and suppressing the growth of endometrial tissue.
Surgical Therapy
In more severe cases, or when medical therapy is ineffective, surgery may be necessary. The type of surgery will depend on the extent and location of the endometriosis. In some cases, a conservative approach may be used, where the surgeon attempts to remove the endometriosis while preserving as much of the bowel as possible. In other cases, a segment of the bowel may need to be removed.
Laparoscopic Surgery
Laparoscopic surgery is often the preferred method for treating bowel endometriosis. This minimally invasive procedure allows for precise removal of the endometriosis with less damage to surrounding tissue and quicker recovery times. However, it requires a skilled surgeon and may only be an option in some cases.
Read More: Why It’s Important Your OB-GYN Specializes in Endometriosis?
Bowel Endometriosis and Fertility
Research indicates that bowel endometriosis may have an impact on a woman’s fertility. This could be due to the inflammation and scarring caused by the disease, which can interfere with the normal function of the reproductive organs.
In cases where infertility is an issue, assisted reproductive technologies may be considered. However, surgery to remove the endometriosis is often recommended first to increase the chances of a successful pregnancy.
Read More: Does Endometriosis Cause Infertility?
Conclusion
Bowel endometriosis is a complex condition that can significantly impact a woman’s quality of life and fertility. Early diagnosis and effective treatment are crucial to managing this condition and minimizing its effects. Suppose you’re experiencing symptoms of bowel endometriosis. In that case, it’s important to consult with a healthcare provider who is knowledgeable about this condition and can guide you through the diagnosis and treatment process.
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6996110/
https://drseckin.com/bowel-endometriosis/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6397811/

Through the Looking Glass: Reflecting on 2023
Embarking on the journey of self-reflection is not just a personal endeavor; for us at iCareBetter, it’s a collective celebration of progress, community, and collaboration. As we bid farewell to 2023, a year marked by challenges and triumphs, it’s time to take a look into the past year and reflect on all that has been accomplished. Join us as we navigate through the areas of growth, community involvement, projects, and meaningful collaborations that shaped our year. In this special blog post, we’re excited to share the insights gained from our podcast endeavors and offer a sneak peek into the thrilling developments that await us in 2024. Let’s rewind, recap, and anticipate the exciting narrative that continues to unfold in the ever-evolving story of iCareBetter.
About iCareBetter
iCareBetter is an innovative platform dedicated to helping patients with endometriosis and chronic pelvic pain find compassionate and skilled experts. All experts on iCareBetter have shown knowledge and expertise in the treatment of endometriosis and chronic pelvic pain.
Vision
Our vision is to reduce the symptom-to-effective treatment of endometriosis to less than a year. Studies show that patients with endometriosis spend an average of 7.5 years to have an official diagnosis. Moreover, even after the diagnosis, patients will have to spend several years with multiple failed treatment attempts. After the long delays in diagnosis and treatment, they might be lucky enough to receive effective treatment from an expert.
Mission
Our mission is to improve access to high-quality specialized care for those with endometriosis. iCareBetter wants to combat the issue of patients living in confusion, pain, and isolation. To that end, we hope to connect as many patients to the right experts as early as possible. And we hope that this will ensure timely diagnosis and effective treatment.
To read more about why iCareBetter was built and the inspiration behind it, check out our blog here and listen to episode 1 of the podcast here, where Saeid and Jandra give you a behind the scenes look into what inspired them.
What happened in 2023?
In 2023, iCareBetter grew in many ways, including new avenues to provide education along with collaboration from the community. Here are some of the highlights!
- We started a podcast! iCareBetter: Endometriosis Unplugged is hosted by Jandra Mueller, DPT, MS a pelvic floor physical therapist and endometriosis patient. The podcast is available on Spotify, Apple Podcasts, and Youtube.
- We had 19 weekly episodes in season one
- Listeners joined from all over the world, reaching 22 countries
- We brought on a team to help with new content on social media creating a more visually appealing platform, community engagement, and followers.
- We now have 211 providers on our website available and ready to help those suffering from endometriosis and we are continuing to grow!
- Our blog content is now consistent with twice weekly posts bringing you updates on all things endometriosis.
What To Expect in 2024
While 2023 was a big year for iCareBetter, we hope to continue the growth and expand our providers across the globe. Our hope is to increase our collaboration with medical specialists, researchers, and advocates. There are some exciting things to come in 2024 including a new season of iCareBetter: Endometriosis Unplugged as well as some other projects that will be announced in 2024.
We hope you have found our resources helpful either for yourself or a loved one, and hope you continue to share the love and spread the word about Endometriosis. All of us here at iCareBetter wish you a safe and happy new year.

Cheers to 2024!
Do you or a loved one have Endometriosis? Here are some blogs that may help you get started on your journey.
- Endometriosis Signs and Symptoms: Everything You Need to Know
- Endometriosis Facts & Myths: Dispelling the Misconceptions

Women’s Health Research and the White House Initiative
Merry Christmas and Happy Holidays! It’s time for some good news when it comes to researching ‘women’s diseases.’
Women’s health has long been an area that has been overlooked and understudied in medical research. Despite making up more than half of the population, women have historically been underrepresented in clinical trials and medical studies, leading to significant gaps in knowledge and understanding of women’s health issues. However, recent developments, such as the establishment of the White House Initiative on Women’s Health Research, are changing the landscape and paving the way for a new era of research and innovation in women’s health.
Table of contents
The Historical Underrepresentation of Women in Research
For decades, women’s health needs were considered a low priority in the scientific and medical fields. During the 1970s, when the women’s health movement emerged as part of the larger women’s movement, it became apparent that women were significantly underrepresented in medical and scientific research. At that time, there were few women working in medicine and science, and the lack of representation had serious implications for the understanding and treatment of women’s health conditions.
One significant example of the cautious approach towards including women in research was the Food and Drug Administration’s policy in 1977, which recommended excluding women of childbearing potential from early-stage drug trials. This policy was a response to the tragic consequences of the drug thalidomide, which caused severe birth defects in thousands of babies born to women who had taken the drug during pregnancy. While the intention was to protect women from potential harm, it resulted in a lack of data on how drugs specifically affected women.
The Shift Towards Inclusion and Advocacy
As awareness grew about the exclusion of women from research studies, advocacy groups and activists began to protest for change. They argued that individual women should be allowed to make informed decisions about participating in research and that excluding women limited their access to potentially life-saving treatments. The Public Health Service Task Force on Women’s Health Issues, in their 1985 report, called for long-term research on how behavior, biology, and social factors affect women’s health, further highlighting the need for inclusion.
In response to these concerns, the National Institutes of Health (NIH) established a policy in 1986 that encouraged the inclusion of women in studies. This policy, published in the NIH Guide for Grants and Contracts in 1987, urged researchers to include women and minorities in their studies and provided guidelines for doing so. The policy was further reinforced in 1989 when NIH announced that research solicitations should prioritize the inclusion of women and minorities.
The Founding of the White House Initiative on Women’s Health Research
In 1990, the Congressional Caucus for Women’s Issues requested an investigation into NIH’s implementation of guidelines for the inclusion of women in research studies. The subsequent report by the General Accounting Office (now known as the Government Accountability Office) highlighted inconsistencies in applying the inclusion policy and the need for improved communication. As a result, the Office of Research on Women’s Health (ORWH) was established in 1991 to monitor and promote the inclusion of women in research.
Under the leadership of Dr. Bernadine Healy, the first female NIH Director, the Women’s Health Initiative was launched in 1991. This initiative consisted of clinical trials and an observational study involving over 150,000 postmenopausal women. The trials aimed to investigate the effects of hormone therapy but was stopped due to incorrect interpretation of the data resulting in the majority of women stopping their hormone therapy overnight, literally. We are still dealing with the consequences of this today.
Legislation and Policies to Ensure Inclusion
While the inclusion of women in research was initially an NIH policy, it became federal law in 1993 through the NIH Revitalization Act. This act included provisions requiring the inclusion of women and minorities in clinical research funded by NIH. The law mandated that NIH ensure the inclusion of women and minorities and that trials be designed to analyze whether variables affect women and minorities differently. It also emphasized that cost should not be a reason for exclusion and called for outreach efforts to recruit diverse populations for clinical studies.
Since the establishment of the ORWH, the office has monitored adherence to inclusion policies and guidelines. Researchers receiving NIH funding are required to report on the sex, race, and ethnicity of participants enrolled in clinical trials. These reports contribute to the ongoing efforts to promote inclusivity and address health disparities among different populations.
Improving Women’s Health Through Research
The White House Initiative on Women’s Health Research, announced by President Biden and led by First Lady Jill Biden, signifies a renewed commitment to advancing women’s health research. The initiative aims to galvanize the federal government, private sector, and philanthropic communities to close research gaps, address health disparities, and pioneer the next generation of discoveries in women’s health.
Under this initiative, concrete recommendations will be delivered to the Biden-Harris Administration within 45 days, outlining actions to improve research on women’s health and maximize investments in this field. Priority areas of focus will be identified to ensure transformative outcomes, ranging from heart attacks in women to menopause and beyond. The initiative also seeks to engage stakeholders from the scientific, private sector, and philanthropic communities to drive innovation and foster collaborative partnerships.
By prioritizing research on women’s health, we can gain a deeper understanding of conditions and diseases that predominantly affect women, such as endometriosis, cardiovascular disease, and Alzheimer’s disease. This knowledge will enable healthcare providers to better prevent, diagnose, and treat these conditions, ultimately improving the lives of millions of women.
The establishment of the White House Initiative on Women’s Health Research and the ongoing efforts to promote inclusion in medical research mark significant milestones in addressing the historical underrepresentation of women in studies. Through policies and legislation, initiatives like the Women’s Health Initiative, and the monitoring of adherence to inclusion guidelines, progress is being made to close research gaps and improve women’s health outcomes.
Research plays a crucial role in understanding the unique aspects of women’s health and developing effective treatments and interventions. By prioritizing and investing in research on women’s health, we can empower women, healthcare providers, and researchers to make informed decisions and advancements that will positively impact the health and well-being of women across the nation. The White House Initiative on Women’s Health Research is a vital step towards achieving this goal and creating a future where women’s health is fully understood, supported, and prioritized.
What you can do!
The Initiative is accepting written comments and input, we urge everyone to get involved.
You can send in either a word document or PDF file to WomensHealthResearch@who.eop.gov
Related reading:
- Endometriosis Signs and Symptoms: Everything You Need to Know
- Endometriosis Facts & Myths: Dispelling the Misconceptions
- Why was iCareBetter built?
References:
- https://www.whitehouse.gov/briefing-room/statements-releases/2023/11/13/fact-sheet-president-joe-biden-to-announce-first-ever-white-house-initiative-on-womens-health-research-an-effort-led-by-first-lady-jill-biden-and-the-white-house-gender-policy-council/
- https://www.whitehouse.gov/gpc/briefing-room/2023/11/17/launch-of-white-house-initiative-on-womens-health-research/
- https://www.whitehouse.gov/briefing-room/speeches-remarks/2023/11/13/remarks-by-president-biden-and-first-lady-jill-biden-establishing-the-first-ever-white-house-initiative-on-womens-health-research/
- https://orwh.od.nih.gov/toolkit/recruitment/history#:~:text=Inclusion%20Becomes%20Law&text=In%201993%2C%20Congress%20wrote%20the,as%20Subjects%20in%20Clinical%20Research.

Endometriosis: Is it a Disability?
Endometriosis, a debilitating condition affecting millions of women globally, often prompts questions about its influence on daily life and work ability. This article provides an in-depth analysis of endometriosis, how it affects women’s work ability, and the possibility of qualifying for disability benefits.
Endometriosis is a medical condition that primarily affects women during their reproductive years, and is very prevalent, with over 80 million women diagnosed worldwide, typically between the ages of 20 and 40. Treatments such as surgery and medical management as well as physical therapy can alleviate some symptoms, but there is currently no definitive cure for the disease.
Table of contents
Endometriosis and Disability: An Intricate Relationship
The symptoms of endometriosis vary greatly among individuals. The most common symptom is pelvic pain, particularly during menstruation, sexual intercourse, bowel movements, or urination. Other symptoms include abdominal bloating, nausea, as well as infertility, among other symptoms.
Endometriosis can significantly disrupt daily functioning due to associated symptoms such as pain, fatigue, and psychological distress especially during one’s menses (period) but is not always confined to that time of the month. Consequently, the disease might qualify as a disability under the Americans with Disabilities Act (ADA) in certain cases. However, it is important to know that the Social Security Administration (SSA) does not automatically classify endometriosis as a disability in endometriosis disability act.
Endometriosis and Social Security Disability Benefits
Qualifying for Social Security disability benefits due to endometriosis is not straightforward. The SSA considers two primary factors when determining if an individual qualifies for SSDI (Social Security disability insurance) or SSI (Supplemental Security Income) disability benefits:
1. Does the individual’s condition meet (or equal) the requirements of a listed impairment?
2. If not, do the symptoms of endometriosis significantly interfere with the individual’s ability to function, to the point where they cannot perform any type of job safely?
Since endometriosis is not listed as a qualifying condition, sufferers cannot automatically meet the first criterion. However, they might still qualify for Social Security disability if their symptoms significantly impede their ability to work, what the SSA calls “substantial gainful activity,” or SGA.
How to Qualify for Social Security Disability for Endometriosis
To qualify for Social Security disability due to endometriosis, it must be demonstrated that the symptoms of the disease prevent the afflicted individual from performing their job. The SSA will then assess if there is any type of job that the individual can safely perform. This evaluation considers medical records, age, work experience and job skills, education, and residual functional capacity (the minimum work that can be expected from an individual).
Applying for Social Security Disability for Endometriosis
Applications for Social Security disability benefits can be made online, through a phone call to the Social Security’s national office, or in person at a local Social Security field office. Winning a disability claim for endometriosis can be challenging, but applicants can seek assistance from an experienced disability attorney or non-attorney representative.
Endometriosis and Employment: A Complex Scenario
While endometriosis can significantly impact an individual’s ability to work, it does not automatically lead to unemployment or early retirement. In fact, many women suffering from endometriosis are able to maintain their employment status, albeit with certain adjustments to accommodate their symptoms.
Work Ability and Endometriosis
A woman’s ability to work can be severely compromised by endometriosis, with the disease often linked to poor work ability at age 46. This decreased work ability can lead to increased absence from work due to health issues. However, despite the increased absenteeism, women with endometriosis often maintain an employment rate comparable to women without the disease. It makes you question why?
Over the past few years, emphasis has been put on staying home if you are sick, as a safety measure for spreading disease, though many with endometriosis may not be able to afford days off of work either because financially they are unable, or there is worry about saying PTO for an unexpected turn of event such as a necessary surgery, or increased symptoms causing debilitating pain. So we suffer through expecting there to be worse days. Women in general, tend to minimize their own symptoms or question if they are “really that bad” as a result of societal influences.
Endometriosis Disability Act and Retirement
The emergence of disability retirement due to endometriosis is not common. Despite the debilitating symptoms of the disease, the risk of early retirement is not significantly higher for women with endometriosis compared to those without the condition. This finding is encouraging and demonstrates the resilience and determination of women battling this condition. Or, is it that those with endometriosis stay working longer because of the financial need and medical bills?
Conclusion
Endometriosis is a complex and debilitating condition that can significantly impact a woman’s ability to work. However, it does not inevitably lead to unemployment or early retirement per the literature, though that does not mean that those living with the condition are able to work feeling well or without worry about consequences of not working. With appropriate medical treatment and workplace accommodations, we hope that not only can those with endometriosis keep working, but with a higher quality of life while working.
References:
- The Americans with Disabilities Act www.ada.gov
- Rossi, H., Uimari, O., Arffman, R., Vaaramo, E., Kujanpää, L., Ala‐Mursula, L., Piltonen, T.T., 2021. The association of endometriosis with work ability and work life participation in late forties and lifelong disability retirement up till age 52: A Northern Finland Birth Cohort 1966 study. Acta Obstetricia et Gynecologica Scandinavica 100, 1822–1829.

Your Guide to Supporting a Loved One Through the Holidays: The Ultimate Endometriosis Resource List Updated and Revised
Table of contents
The holiday season can be a joyous time filled with festivities, but for individuals navigating the challenges of endometriosis, it can also present unique hurdles. Supporting a loved one with endometriosis during this time involves not only empathy but also understanding the complexities of the disease. To aid both those directly affected and their support systems, a plethora of resources are available, ranging from insightful blogs and informative books to engaging movies and podcasts. These tools not only offer a wealth of knowledge about endometriosis but also provide a platform for individuals seeking a better understanding of the condition or those desiring to support their loved ones effectively.
In this guide, we will explore a curated selection of resources, offering both emotional support, educational insights, and even some ideas for your holiday shopping list to help individuals navigate the holiday season with a heightened awareness of endometriosis and a supportive approach to those impacted by this often misunderstood condition.
Understanding Endometriosis
For those of you unfamiliar with our blog, endometriosis is a chronic disease that primarily affects women (XX) of reproductive age. It involves the growth of endometrial-like tissue (the tissue that lines the inside of the uterus) outside of the uterus, leading to inflammation and pain, particularly during menstruation, though many other symptoms may be present.
For more information on symptoms of endometriosis, read our blog 20 Signs and Symptoms of Endometriosis.
Despite being a common condition, endometriosis is often misdiagnosed or overlooked, leading to many women suffering in silence. However, with the right information, supportive community, and access to informed medical providers, it is possible to manage the condition and lead a fulfilling life.
Podcasts on Endometriosis
Podcasts are an excellent way of gaining insights and information about endometriosis in a convenient and accessible format. Here are some podcasts that delve into various aspects of the disease, from personal stories to expert opinions:
- “iCareBetter: Endometriosis Unplugged”: Hosted by yours truly, is a video podcast (Spotify & Youtube) that focuses on expert interviews and patient stories with a few bonus episodes of specialists who treat conditions that often coexist with those with endometriosis. We have completed season 1 and hope to have season 2 coming in 2024!
- “In Sixteen Years of Endometriosis”: Hosted by two witty best friends who share their personal journey with the disease, this podcast offers a blend of humor, vulnerability, and accurate information.
- “The Cycle”: This podcast features stories of people living with endometriosis from around the world, providing practical ways to cope with the disease.
For more podcasts about endo, check out our previous blog here.
Books about Endometriosis
Reading about endometriosis can provide a comprehensive understanding of the disease. Here are some books written by medical experts and those living with the condition:
- “Beating Endo: How to Reclaim Your Life from Endometriosis”: Written by Iris Kerin Orbuch, MD, and Amy Stein, DPT, this book provides actionable insights into understanding and managing the disease.
- “Heal Endo”: By Katie Edmonds, (F)NTP provides a book that is patient focused with a more indepth understanding of the science balanced by actionable items that range from surgery to dietary and lifestyle changes.
- “The Endometriosis Health and Diet Program”: Authored by Dr. Andrew S. Cook, MD, FACOG, and Danielle Cook, MS, RD, CDE, this book focuses on treating endometriosis holistically, offering a comprehensive program tailored to individual needs.
- “Know Your Endo: An Empowering Guide to Health and Hope With Endometriosis”: Authored by Jessica Murnane, this book provides tools and strategies to manage chronic pain associated with endometriosis.
- “The Endo Patient’s Survival Guide: A Patient’s Guide to Endometriosis & Chronic Pelvic Pain”: This book by Andrew S. Cook, MD, FACOG, Libby Hopton, MS, and Danielle Cook, MS, RD, CDE, is a companion guide for patients, offering insights into diagnosis, treatment options, and achieving optimal relief.
Videos and Documentaries about Endometriosis
Visual content can help in understanding complex information about endometriosis. Several documentaries and movies have been produced to increase awareness about the disease.
- “Below the Belt”: A documentary from Shannon Cohn who created “Endo What?” focuses on the journey of several women seeking an endometriosis diagnosis and the challenges they face. “Below the belt” is not only an empowering film for educating the masses, it has become a tool for legislative change. A must see for everyone.
- “All about NINA”: A drama highlighting the experience of a woman, Nina Geld, managing her life with endometriosis.
- “Endo what?”: A documentary featuring women living with endometriosis and experts discussing treatment options.
- “The painful truth”: This film focuses on endometriosis and adenomyosis, another related condition.
- “A thousand needles”: A short documentary about the impact of endometriosis on a woman’s life.
- “End-o”: A short film showcasing the life of a young woman, Jaq, living with endometriosis.
- “The resilience of women in pain”: This short film focuses on Rose, a woman suffering from endometriosis and chronic illness, and her journey towards resilience.
Your Endo Shopping List: Comfort Tools for Loved Ones
In case you need to do some last minute shopping and want to show your loved ones you understand, here are some essential items that have proven useful for many. While these tools may not be able to stop this awful disease, they may provide some degree of comfort and relief when things get bad. Whether you are prepping for surgery, or just need some handy tools, here are some of my favorite items.
- Wedge Pillow. This is a must for those preparing for surgery during recovery. I only found this at my 3rd (and hopefully last) surgery and it was a game changer. When your belly is full of air, tender, and you don’t feel like moving (or sitting up at the very least), this helps to provide relief for recovering in bed or on the couch and is great if you are a side or back sleeper.
- Heating pads. This is probably the number one item most endo warriors have – likely at home and work. They are always handy to have wherever you are, and for a more personalized gift, ETSY.COM has some amazing endo swag (including heating pads).
- My Obi Apollo. This is a TENS unit with heat and multiple programs to help with cramps and reduce pain. To learn more about how TENS may be helpful, check out our blog here.
- Squatty Potty. Everyone should have one. This is the gift that no one really wants, but secretly is so happy when they get one. It is essential for optimal toileting for everyone, but especially if you have endometriosis. Constipation and pelvic floor dysfunction are two issues the majority of those with endometriosis suffer from and this tool can make a world of a difference for toileting….
Until recently, endometriosis was not a term most people were familiar with, unless you are suffering. It is amazing how this is shifting and so many more people are familiar with the term, but may not understand how impactful this disease is to one’s life. Finding the right surgeon is key to address the lesions, but having tools to help in the meantime is crucial. More importantly, your loved one will most appreciate the effort you made to educate yourself about their disease, especially during the stress the holidays may bring. Give them the gift of understanding and empathy this year, and maybe something to help their pain in the meantime.
Please note: We do not have financial affiliations with any of these products listed above.
Related Reading:
- Find an Endometriosis Specialist for Diagnosis, Treatment, & Surgery
- Endometriosis Facts & Myths: Dispelling the Misconceptions
- What You Need to Know About Endometriosis Excision Surgery
- Managing Endometriosis: What You Need to Know.

Preparing for the Holidays: Tips for Managing Flares
Table of contents
As the holiday season approaches, individuals grappling with endometriosis or other chronic illnesses are contemplating how to sidestep discomfort and flare-ups. Despite our concerted efforts to prevent or mitigate the frequency and intensity of flares associated with endometriosis, the truth remains that flare-ups are inevitable.
The holiday season holds the promise of joy, connections, and quality time with loved ones for many, but for others, it may bring stress, indulgence, worry, temptation, or even apprehension. The prospect of navigating gatherings, grappling with uncomfortable inquiries, or being compelled to make challenging food choices after diligently avoiding certain items for an extended period can be disheartening. Although flares may be an inherent part of the journey at any given time, holidays are no exception. The good news is that there are strategies available to effectively manage or minimize flares during these festive times!
Managing endometriosis or any chronic illness during the holiday season can present unique challenges, but there are strategies to help minimize flares and make the most of the festive season. Here are some tips:
Plan and Pace Yourself
- Plan your activities and commitments wisely. Don’t overcommit to events or tasks.
- Prioritize what’s most important to you and conserve your energy for those activities.
Communicate Openly
- Communicate with friends and family about your condition. Let them know your limitations and needs.
- Be open about your health concerns, so they can better understand and support you during gatherings.
- Or have a script of what you may want to say to those you do not want to share this information with such as: “Thank you for asking, though I’d prefer not to share those details right now, thank you for understanding.”
For a list of resources for yourself or others, check these out:
Choose Your Events
- Select events that align with your energy levels and health status.
- It’s okay to decline invitations or leave early if you’re not feeling well.
Mindful Eating
- Food is more than just its ingredients and nutrients, food is a major part of many of our cultures, enjoy it!
- Remember, stressing about trigger foods may be just as triggering as enjoying some of your favorite dishes.
- Consider bringing a dish that aligns with your dietary restrictions to ensure there’s something you can comfortably eat.
- Eat prior to going to events to avoid overindulging in foods that may be a trigger for your symptoms.
Rest and Relaxation
- Schedule breaks for rest and relaxation. Give yourself permission to step away from activities and take time for self-care.
- Incorporate relaxation techniques such as deep breathing or meditation to manage stress.
Create a Comfortable Space:
- If attending gatherings, find a comfortable spot to rest if needed.
- Consider bringing a cushion, heating pad, or any other items that provide comfort during flare-ups.
Be Kind to Yourself
- Understand that flares may still happen despite your best efforts. Be kind to yourself and acknowledge that it’s okay to take a step back when needed.
Stay Connected
- Stay connected with supportive friends or online communities. Sharing experiences and tips with others who understand what you’re going through can be comforting.
Use your toolbox!
- For many, you have gathered your individual tools that have worked well for you in the past, don’t forget about these!
- Connect with your providers, if you haven’t seen your providers in a while, it may be helpful to touch base with your mental health therapist, nutritionist, or physical therapist.
- Maybe you opt for that less intense workout to give your body a break.
Remember, everyone’s experience with endometriosis is unique, so tailor these tips to your specific needs and preferences. It’s essential to prioritize your well-being and enjoy the holiday season in a way that works best for you.
For more on this topic, check out our blog Managing Endometriosis: What You Need to Know.
Understanding Endometriosis: Unveiling the Common Symptoms and Their Impact
Table of contents
A recent article from Australia on common symptoms and endometriosis was released recently that followed several thousand women that were both surgically and clinically diagnosed (evaluated separately) with endometriosis and their symptoms to look at associations. There are minimal longitudinal studies available, so this article can be very impactful in raising awareness of the variable, but common, symptoms those with endometriosis experience.
Endometriosis, a chronic gynecologic disorder, is characterized by the presence of endometrium-like tissue outside the uterus. This condition has a profound impact on women’s (XX) lives, often leading to increased hospitalizations, diminished work productivity, and a reduced quality of life. While menstrual symptoms are the most commonly associated with endometriosis, an array of other symptoms can significantly affect the physical and mental wellbeing of women diagnosed with this condition. This article aims to provide an in-depth understanding of the common symptoms associated with endometriosis and their impact on women’s health.
The Prevalence of Endometriosis
Endometriosis is a prevalent health condition affecting approximately 1 in 9 women (11.4%) in Australia by the age of 44 years and in the US the estimation is 1 in 10, though this may be inaccurate due to the significant delay or issues with misdiagnosis. The nonspecific nature and normalization of the symptoms often lead to a significant delay in the diagnosis of endometriosis, with several studies reporting an average delay of 7 to 11 years. This delay in diagnosis results in untreated endometriosis-related symptoms, increased hospitalizations, higher healthcare resource utilization, and potentially reduced success using assisted reproductive technologies. Additionally, some of the overlapping symptoms may be due to the “treatments” offered for symptom management such as hormonal supressive therapies.
Endometriosis and Menstrual Symptoms
Women diagnosed with endometriosis frequently report an array of menstrual symptoms. These may include severe period pain (dysmenorrhea), heavy menstrual bleeding, irregular periods, and premenstrual tension. The association between endometriosis and these symptoms is strong, with the odds ratio for severe period pain being as high as 3.61.
Endometriosis and Mental Health Problems
Apart from physical discomfort, endometriosis can significantly affect a woman’s mental health. Studies reveal a higher incidence of mental health problems, including depression, anxiety, and other mental health disorders, in women with endometriosis. The adjusted odds ratios for depression and anxiety are 1.67 and 1.59, respectively.
Endometriosis and Bowel Symptoms
Bowel symptoms are another common complaint among women with endometriosis. These may include constipation, hemorrhoids or piles, indigestion, or heartburn, bloating, diarrhea, or a combination of these. Additionally, one of the clinical manifestations is dyschezia, or discomfort/pain associated with bowel movements. The adjusted odds ratio for constipation is 1.67, indicating a significant association between endometriosis and bowel symptoms. Additional studies have demonstrated that approximately 90% of those with endometriosis have IBS-like symptoms.
Endometriosis and Urinary Symptoms
Urinary symptoms, such as burning with urination (dysuria) and vaginal discharge or irritation, are also more prevalent in women with endometriosis. The increased odds of urinary symptoms suggest a possible alteration in the pelvic innervation caused by endometriotic lesions.
Endometriosis and Pain Symptoms
Endometriosis is often associated with other forms of pain, including back pain, headaches or migraines, and stiff or painful joints. The adjusted odds ratios for these pain symptoms range from 1.50 to 1.76, further emphasizing the multifaceted impact of endometriosis on women’s health.
Endometriosis and Nonspecific Symptoms
In addition to the symptoms described above, endometriosis is also linked to various nonspecific symptoms. These may include severe tiredness, difficulty sleeping, palpitations, and allergies or hay fever or sinusitis. The association between endometriosis and these symptoms underlines the complex nature of this condition and its wide-ranging effects on women’s health.We need more understanding whether these symptoms are a direct result of the endometriosis, the side effects of treatments, or another related issue.
The Importance of Early Diagnosis
Given the wide array of symptoms associated with endometriosis and their significant impact on a woman’s quality of life, the importance of early diagnosis and treatment cannot be overstated. Early intervention can not only alleviate the physical discomfort associated with the disease but also significantly improve mental health outcomes. Furthermore, it can potentially prevent the development of chronic pain conditions and other long-term health complications.
Conclusion
Endometriosis is a complex condition that affects multiple aspects of a woman’s health. It is associated with a wide range of symptoms, extending beyond menstrual problems to include mental health issues, bowel and urinary symptoms, pain, and other nonspecific symptoms. Understanding these symptoms and their impact on women’s lives is crucial for providing comprehensive care to those diagnosed with this condition. While further research is needed to elucidate the specific mechanisms underlying these associations, the current evidence underscores the importance of early diagnosis and intervention in improving health outcomes for women with endometriosis.
Related reading:
- Understanding fatigue and endometriosis: A Practical No-Nonsense Guide
- Interstitial Cystitis and Endometriosis: Unraveling the “Evil Twins” Syndrome of Chronic Pelvic Pain
- Endometriosis Signs and Symptoms: Everything You Need to Know
References:
- Gete DG, Doust J, Mortlock S, et al. Associations between endometriosis and common symptoms: findings from the Australian Longitudinal Study on Women’s Health. Am J Obstet Gynecol 2023;229:536.e1-20.
Dr. David Redwine Obituary : A Modern Hero in Endometriosis Research and Excision Surgery
The recent death of David Redwine has undoubtedly left many with sadness and devastation. Our thoughts are with his friends, family, colleagues, and the endometriosis community as a whole. The world of gynecology has been significantly influenced and transformed by the groundbreaking work of Dr. David Redwine, a significant contributor to those suffering from this disease. A modern hero in this community in his contributions to endometriosis research, excision surgery, and fighting alongside patients and advocating for better answers and better care. His innovative approaches and relentless pursuit of knowledge have positioned him as a leading advocate for patients with endometriosis, a debilitating condition that affects millions of women worldwide.
Table of contents
Who is David Redwine?
A formidable figure in the medical community, Dr. David Redwine has devoted his career to understanding and treating endometriosis. His profound commitment to research and patient care has made him a renowned authority in the field.
Redwine’s Contribution to the Understanding of Endometriosis
Endometriosis is a complex and often misunderstood condition. Dr. Redwine’s research has been instrumental in challenging established theories and introducing new perspectives on the origins and treatment of the disease.
Challenging Sampson’s Theory
One of the most significant contributions of Dr. Redwine has been his challenge to the widely accepted Sampson’s Theory of endometriosis. The theory, proposed by Dr. John Sampson in the 1920s, suggests that endometriosis is caused by retrograde menstruation, where menstrual blood containing endometrial cells flows back through the fallopian tubes and into the pelvic cavity. Redwine questioned the validity of this theory, arguing that if retrograde menstruation were indeed the cause of endometriosis, there should be ample microscopic evidence of refluxed endometrial cells attaching to the pelvic lining and subsequently proliferating. Yet, such evidence is conspicuously lacking. While modern day understanding by experts support alternative theories and are moving toward more plausible explanations, Dr. Redwine is largely to thank for this movement.
Proposing an Embryonic Origin
In place of Sampson’s Theory, Redwine proposed that endometriosis originates from an embryonic source. He argued that endometriosis is derived from mesoderm, the middle layer of the three embryonic layers, and is a result of abnormal differentiation and migration of cells during embryonic formation of the female reproductive tract. This theory suggests that endometriosis is a congenital condition that can manifest later in life under the influence of hormones and other factors.
The Concept of Mulleriosis
To further elucidate the embryonic origin of endometriosis, Redwine introduced the concept of ‘Mulleriosis.’ This term embraces a wider perspective, encompassing all pathologies associated with abnormal development of the Mullerian ducts, the precursor structures to the female reproductive organs.
Redwine’s Innovations in Endometriosis Surgery
Dr. Redwine has not only helped reshape our understanding of endometriosis but also revolutionized its treatment. He is a staunch advocate for excision surgery, a procedure that aims to completely remove endometriosis lesions. While early surgeries also focused on excision surgery, though lacking the precision and advanced technology we have today, the introduction of ablation surgery in the 70’s has complicated research findings, surgical outcomes, and the overall role of surgery in the treatment of this disease resulting in a further push towards hormonal suppression and the fight against Big Pharma.
The Importance of Excision Surgery
Whereas traditional first-line therapies often rely on hormonal therapy or less thorough surgical methods, Redwine emphasizes the importance of excision surgery in effectively treating endometriosis. Through extensive research and practice, he has demonstrated that excision surgery can significantly alleviate symptoms and improve the quality of life for patients with endometriosis.
The Concept of Cure
Contrary to the prevalent belief that endometriosis is incurable, Redwine insists that the disease can be effectively treated through excision surgery. He defines ‘cure’ as the complete absence of the disease, as proven by follow-up laparoscopy. While this topic may be nuanced to a degree and there are cases of regrowth, those of who have undergone a true excision surgery, and those that perform skilled excision surgery understand the difference of persistent pain vs. incomplete technique.
Redwine’s Advocacy for Patients with Endometriosis
In addition to his clinical and research work, Dr. David Redwine is a passionate advocate for patients with endometriosis. He strongly believes in empowering patients with knowledge about their condition and available treatment options.
Redwine is committed to educating both the medical community and the public about endometriosis. He regularly delivers lectures and presentations, sharing his insights and the latest research findings. His dedication to education aims to foster a more informed and empathetic understanding of endometriosis.
As a fervent advocate for patient-centered care, Redwine emphasizes the need to listen to patients’ experiences and concerns. He argues that an effective treatment approach should consider not only the physical manifestations of the disease but also its impact on a patient’s mental and emotional well-being.
You Will Be Missed!
Dr. David Redwine’s pioneering work in endometriosis research, excision surgery, and patient advocacy has had a profound impact on the understanding and treatment of the disease. His unwavering dedication to advancing knowledge and improving patient care serves as an inspiration for both medical professionals and patients alike. Dr. Redwine’s contributions will undoubtedly continue to shape the future of endometriosis care and research, despite his recent passing. His name will always be known in this community for the significant contributions he has made and the patients whom he has helped whether directly, or indirectly.
Rest in peace Dr. Redwine, you will be missed.

