
Finding an Excision Specialist: What you Need to Know
Table of contents
Finding a true excision specialist is difficult for many reasons, including the paucity of skilled surgeons and the financial burden that may come with when you find one that is a good fit for you. So, the first step is to find the right surgeon and the second step is determining how to navigate the financial implications. It’s important not to do it the other way around because initial botched surgery and treatment can make it that much more difficult to find relief. Surgery is never easier the second or third time around.
There are a small handful of carefully monitored sites with very helpful information and a listing of qualified surgeons based mainly on patient outcomes feedback, none better than Nancy’s Nook. While there may be a few others that share patient experiences and some information, most are not well monitored or refereed, and thus, information and surgeon leads must be viewed with caution. Nancy Petersen has a vested personal interest in endometriosis and a deep understanding of the disease based on her work for many years with Dr. David Redwine, a pioneer in the field. Thus the information which is refereed by Nancy and her hand-picked editors forms a solid base. However, patient feedback, while important, is not the only way to determine who to pick as your surgeon.
The degree of a surgeon’s true technical skills is not easy to judge, especially if you are in the majority of not being medically trained yourself. Review of resumes and asking questions such as where did you go to school or train or how many cases do you do leaves a lot to be desired. It is simply not an accurate reflection, although knowing the surgeon’s background and pedigree can help. So, what else can be done to help find the right surgeon for you?
iCarebetter was created to help those in need find a specialist with a bit more objective information than patient recommendations alone. iCarebetter includes surgeons who are video-vetted by a peer review process. This means that acknowledged experts review surgical videos submitted by surgeons who wish to be vetted and are objectively either verified or not as possessing a high level of surgical capabilities. Of course, this does not reflect total patient management and bedside manner and more subjective skills. However, you want someone who can get the surgery properly done at the highest possible level for your needs. There is something to be said about a surgeon who is not afraid of showing other, perhaps better, surgeons what they’ve got, so to speak.
Additional related reading: Why was iCarebetter built?
Not too long ago, it used to be that when you showed up to your appointment and asked the surgeon what type of surgery they perform, you typically would hear ablation or excision. More recently, many more have adopted excision as the preferred method, or at least talk that way. But outcomes are variable among those receiving “excision surgery,” why? This article will help you better understand some of the key takeaways in finding the right surgeon for you. Some are simply not at a high enough skill level to help you, and others do not walk the talk.
Additional related reading: Laparoscopy: A Common Treatment for Endometriosis
Excision vs. Ablation
Excision is the removal of tissue diseased with endo, whereas ablation is the burning or fulguration of endo lesions and surrounding tissue and organs, usually using electrocautery. Research shows both may be effective for superficial endometriosis and not near delicate structures such as bowel and ureters; however, it is usually not possible to accurately determine which are superficial or deep infiltrating lesions based on looking at them.
While some patients do symptomatically improve with ablation surgery, clinically, it is recommended that excision is the preferred method because you really cannot know if a lesion invades deeper into the tissue, until you remove it. It is likely that those who have benefited from ablation surgery probably only had superficial lesions, and those who did not improve likely had more extensive endometriosis that was missed or not fully eradicated. While this is clinically accepted, we need more research to confirm this and show it truly is the preferred method. The problem with designing an accurate research study for this question is that the skill of surgeons participating in clinical trials is highly variable, so the results can be completely wrong because it almost entirely depends on surgical skill. More importantly, one size does not fit all, and everyone is different. Hence, a truly expert surgeon who can determine and act appropriately on findings and nuances is critical to your personal success.
Important Terms and Approaches
- Wide excision is a term you may hear which means that there is a wide margin of tissue that is removed to ensure that only healthy tissue remains. There is no consensus on this topic. Some surgeons will adopt wide excision, while others will remove the individual lesions, perhaps leaving micro-diseased tissue behind that is difficult to visualize during surgery. These areas may develop endometriosis in the future. In an expert’s hands, it is a judgment call as to how wide any given area of excision should be. There is a balance of too much and not enough, and this requires a high level of expertise to optimize benefits and minimize harm.
- Combination of excision and ablation. The other consideration when it comes to excision surgery is that some surgeons adopt a combination of excision and ablation. Some tissue will be excised for histological confirmation of the disease, but then many lesions may be ablated instead of excised. This generally does not make sense unless the surgeon simply does not believe that excision is better. The only exception is the ablation of tiny lesions on sensitive areas, such as the ovarian surface, where fertility preservation is a concern.
- Incomplete removal of lesions. Most general gynecologic surgeons will not be able to excise very many lesions and will handle them by fulguration or ablation. Some surgeons may be able to excise the majority of lesions but do not have extensive training to remove all lesions. Hopefully, your surgeon will advise you of their limitations prior to rather than after your incomplete surgery. However, in some cases, endometriosis is not suspected prior to surgery, and a general gynecologist, who is most often not trained in higher-level excision techniques, is caught by surprise. In that case it is better to biopsy, prove that endo exists, and refer to a specialist rather than poorly perform an incomplete surgery.
Complete excision, especially in a difficult case where there is a lot of disease or perhaps in case of distorted anatomy due to repeat surgery, will only occur with a surgeon who has been additionally trained not just in MIGS (minimally invasive gynecologic surgery) but in endo excision per se. The main surgeon has to be an expert because it is never possible to predict how much endo there is, even if imaging scans are negative. Beyond that, if the main surgeon is not trained to perform bowel or urologic surgery, then a well-coordinated team is mandatory. The problem is that this coordination is not too tightly organized in many centers. Ask questions about who can do what, if any required supporting surgeons are in surgery from the beginning or “on call” when needed. The latter does not often work out too well because of other commitments that might be conflicting.
What if I Cannot Afford to see an Excision Specialist?
It is true that many of the surgeons that specialize in excision surgery are out-of-network providers. However, in the past couple of years there have been more surgeons that do take insurance and hopefully, with legislative efforts and more education, this trend will continue to grow.
That being said, there is a good reason why many do not take insurance, and even if you have the option of an in-network provider, it may not be the right surgeon for you. Currently, there is no difference in the coding when undergoing laparoscopic or robotic surgery for endometriosis that discriminates between ablation versus excision. Ablating lesions takes far less skill, time and effort than excision does. Meaning, that an in-network surgeon who performs an ablation surgery that takes one hour will get paid the same as an in-network surgeon who does an excision surgery that takes four hours. Becoming a trained excision specialist costs money to the provider to undergo extra training to be able to perform these types of procedures, and even more training to become an expert in robotics.
Until our payment, insurance, and coding systems catch up to what is required, we will likely not see a dramatic shift in those who take insurance.
Aside from the financial difference, those who are in-network may not be able to spend the amount of time you may want during office visits to discuss the details of your surgery and your overall case as those who are out-of-network. Out-of-network doctors are usually able to provide longer visits to address your concerns in depth instead of the standard 15-20 minutes you typically get with your regular OBGYN. Some choose cost over this important treatment planning time, but there are many people who value a personalized approach which takes more time over the cost of the surgery. It is not just excision surgery that will get you to where you want to be, and this personalized treatment planning includes very important discussion about pre-operative and post-operative healing options.
Whatever you choose, you want to feel comfortable with your surgeon and find the right fit for you.
Other Considerations: Some Tips on Navigating the System
- Change your insurance provider. I know this is easier said than done, but for those with HMOs who are only allowed to stay within a small network, it may be worthwhile to talk to your employer, or partner (if applicable), or do some research on what other insurances are available to you. PPO plans include their list of in-network providers but also often provide some reimbursement for out-of-network providers, especially if their surgeons are not at the skill level that you need or are not within a reasonable geographic range. Open enrollment is typically once a year, or when you change jobs, or due to other qualifying life-changing events. So consider this as an option that may allow you to have more latitude and choice when planning for surgery.
- Work with your insurance company. This does not always work, and is time-consuming, but can have a big payoff at the end. There have been patients who have communicated and worked with their insurance companies when there is no available specialist around to cover your out-of-network provider services. While this has worked for some, be ready for a time commitment and likely many phone calls to get to the person who can help you.
- Ask the doctor you have selected. Some excision specialists have been helping patients with this insurance negotiation conundrum for many years. Because of that, some have teams that help you get an exception and lower your out of pocket costs tremendously.
- Adopt a new perspective. Lastly, this will not necessarily save you money, but looking at your surgery as an investment in your health may make it seem more doable. We often do not think twice about financing $30-$40k on a car or the thousands of dollars we spend on “stuff,” but we often hesitate when it comes to our health. Without health, nothing else matters. For many, excision surgery has been life-changing, and thinking of paying for your surgery as an investment in your health, may be the best thing for you. Again, while upfront costs may seem high, a concerted effort to find the right surgeon, advocate for yourself, and ideally find a surgeon’s office that can help you negotiate and advocate can lead to lower final out-of-pocket costs than you might think.
Whatever route you take, it needs to be the best route for you, with a full understanding of the pros and cons. Take your time when finding the right surgeon, and don’t rush into something you are not comfortable with.
Additional reading: 7 Ways to Prepare For First Endometriosis Specialist Appointment
Current Research in Endometriosis
Endometriosis affects roughly 190 million women and girls (assigned female at birth) worldwide. Despite its significant impact on the health of the individual due to both the disease and overlapping pain conditions, research funding for endometriosis lags behind other common diseases. However, we are starting to see small improvements. For example, in 2020, research funding by the NIH (National Institutes for Health) for endometriosis was 14 million dollars (US) and in 2022 nearly doubled at 27 million, and it is estimated for 2023 and 2024 to be approximately 29 million dollars.
The economic burden of endometriosis on the U.S. alone, in terms of medical care and lost productivity, is estimated to be around $78-120 billion annually. These figures underscore the urgent need for more research funding and better treatment options for endometriosis. Which is what we have been seeing more recently, research focused on other aspects of the disease and co-morbidities and not just drugs aimed at suppressing hormones.
Researchers have started to look more broadly and dive deeper into some areas that have only been superficially explored such as the impact of the microbiome and genetic studies. While the media has seemed overly excited about the findings and what this means now, this new research may be the stepping stones we need to better understand the variations of this disease and future treatments for managing endometriosis along with the overlapping symptoms.
This article aims at reviewing the new research in endometriosis.
Please note that this is a brief overview of some of the research, not opinions or endorsements from the iCareBetter team. More extensive research is needed in these areas before any conclusions can truly be drawn.
Here’s what researchers have been studying recently:
- Dichloroacetate. Researchers from the University of Edinburgh found that treatment with dichloroacetate reduced the size of endometriosis lesions and decreased lactate production, which has been associated with endometriosis manifestation in earlier studies.
- Cannabis. The Western Sydney University in Australia is investigating the potential benefits of medical cannabis for endometriosis treatment. The double-blind randomized controlled trial will evaluate whether medicinal cannabis can counter symptoms like pain caused by endometriosis against a placebo. This of course would not be focused on a treatment for endo, but as pain management.
- Immune system. It’s been recognized for many years that endometriosis and the immune system are intricately linked. Recent studies have found an overexpressed protein on endometriotic cells which may help drug development. Startup Fimmcyte is developing an antibody that labels endometriosis cells for clearance by the immune system, which could provide a much-needed non-hormonal therapy for women with endometriosis.
- Pelvic floor therapy. Studies have shown that pelvic floor therapy could be key to tackling endometriosis-induced pain, or identifying overlapping pain conditions. In addition to helping manage chronic pelvic pain, pelvic floor therapy has been effective in relieving pain through exercise, movements, and manual therapies that target the pelvic area. Read more about pelvic floor physical therapy from our recent blog here.
- Endometriosis and other inflammatory diseases. Recent research suggests that endometriosis may be linked to other inflammatory and pain-inducing diseases. A study by Celmatix and 23andMe, among others, found that endometriosis may be linked to 11 conditions, including migraine, back, and multisite chronic pain (MCP), and inflammatory conditions like asthma and osteoarthritis.
- Biotech and Endometriosis. Several ongoing studies aim to improve our understanding of endometriosis at the genetic level. The Research OutSmarts Endometriosis (ROSE) study is investigating the causes of endometriosis and aims to develop improved diagnostics and treatments for women with the condition.
Despite the challenges faced by researchers and patients alike, these recent developments in endometriosis research are a beacon of hope. As our understanding of this complex condition deepens, we edge closer to more effective treatments and perhaps, one day, a cure for endometriosis. One thing is certain though, endometriosis may be due to several factors which may need different targets. The expanding research into these topics may not seem relevant now, but may pave the way to better understanding of the variations of the disease, resulting in a wider array of therapies in addition to surgery for both treatment as well as symptom management.
Related Reading:
- Genetic Study On Patients With Confirmed or Suspected Endometriosis; Next Gen Jane
- Unraveling the Connection Between Endometriosis and Autoimmune Diseases
- The Hidden Connection Between Endometriosis and Systemic Lupus Erythematosus
- Genetics and Epigenetics of Endometriosis: Unraveling the Complex Web of Hereditary Implications
References:
- Endometriosis Clinical Trials – Mayo Clinic Research
- Giudice, L.C., Horne, A.W. & Missmer, S.A. Time for global health policy and research leaders to prioritize endometriosis. Nat Commun 14, 8028 (2023). https://doi.org/10.1038/s41467-023-43913-9

Your Guide to Supporting a Loved One Through the Holidays: The Ultimate Endometriosis Resource List Updated and Revised
Table of contents
The holiday season can be a joyous time filled with festivities, but for individuals navigating the challenges of endometriosis, it can also present unique hurdles. Supporting a loved one with endometriosis during this time involves not only empathy but also understanding the complexities of the disease. To aid both those directly affected and their support systems, a plethora of resources are available, ranging from insightful blogs and informative books to engaging movies and podcasts. These tools not only offer a wealth of knowledge about endometriosis but also provide a platform for individuals seeking a better understanding of the condition or those desiring to support their loved ones effectively.
In this guide, we will explore a curated selection of resources, offering both emotional support, educational insights, and even some ideas for your holiday shopping list to help individuals navigate the holiday season with a heightened awareness of endometriosis and a supportive approach to those impacted by this often misunderstood condition.
Understanding Endometriosis
For those of you unfamiliar with our blog, endometriosis is a chronic disease that primarily affects women (XX) of reproductive age. It involves the growth of endometrial-like tissue (the tissue that lines the inside of the uterus) outside of the uterus, leading to inflammation and pain, particularly during menstruation, though many other symptoms may be present.
For more information on symptoms of endometriosis, read our blog 20 Signs and Symptoms of Endometriosis.
Despite being a common condition, endometriosis is often misdiagnosed or overlooked, leading to many women suffering in silence. However, with the right information, supportive community, and access to informed medical providers, it is possible to manage the condition and lead a fulfilling life.
Podcasts on Endometriosis
Podcasts are an excellent way of gaining insights and information about endometriosis in a convenient and accessible format. Here are some podcasts that delve into various aspects of the disease, from personal stories to expert opinions:
- “iCareBetter: Endometriosis Unplugged”: Hosted by yours truly, is a video podcast (Spotify & Youtube) that focuses on expert interviews and patient stories with a few bonus episodes of specialists who treat conditions that often coexist with those with endometriosis. We have completed season 1 and hope to have season 2 coming in 2024!
- “In Sixteen Years of Endometriosis”: Hosted by two witty best friends who share their personal journey with the disease, this podcast offers a blend of humor, vulnerability, and accurate information.
- “The Cycle”: This podcast features stories of people living with endometriosis from around the world, providing practical ways to cope with the disease.
For more podcasts about endo, check out our previous blog here.
Books about Endometriosis
Reading about endometriosis can provide a comprehensive understanding of the disease. Here are some books written by medical experts and those living with the condition:
- “Beating Endo: How to Reclaim Your Life from Endometriosis”: Written by Iris Kerin Orbuch, MD, and Amy Stein, DPT, this book provides actionable insights into understanding and managing the disease.
- “Heal Endo”: By Katie Edmonds, (F)NTP provides a book that is patient focused with a more indepth understanding of the science balanced by actionable items that range from surgery to dietary and lifestyle changes.
- “The Endometriosis Health and Diet Program”: Authored by Dr. Andrew S. Cook, MD, FACOG, and Danielle Cook, MS, RD, CDE, this book focuses on treating endometriosis holistically, offering a comprehensive program tailored to individual needs.
- “Know Your Endo: An Empowering Guide to Health and Hope With Endometriosis”: Authored by Jessica Murnane, this book provides tools and strategies to manage chronic pain associated with endometriosis.
- “The Endo Patient’s Survival Guide: A Patient’s Guide to Endometriosis & Chronic Pelvic Pain”: This book by Andrew S. Cook, MD, FACOG, Libby Hopton, MS, and Danielle Cook, MS, RD, CDE, is a companion guide for patients, offering insights into diagnosis, treatment options, and achieving optimal relief.
Videos and Documentaries about Endometriosis
Visual content can help in understanding complex information about endometriosis. Several documentaries and movies have been produced to increase awareness about the disease.
- “Below the Belt”: A documentary from Shannon Cohn who created “Endo What?” focuses on the journey of several women seeking an endometriosis diagnosis and the challenges they face. “Below the belt” is not only an empowering film for educating the masses, it has become a tool for legislative change. A must see for everyone.
- “All about NINA”: A drama highlighting the experience of a woman, Nina Geld, managing her life with endometriosis.
- “Endo what?”: A documentary featuring women living with endometriosis and experts discussing treatment options.
- “The painful truth”: This film focuses on endometriosis and adenomyosis, another related condition.
- “A thousand needles”: A short documentary about the impact of endometriosis on a woman’s life.
- “End-o”: A short film showcasing the life of a young woman, Jaq, living with endometriosis.
- “The resilience of women in pain”: This short film focuses on Rose, a woman suffering from endometriosis and chronic illness, and her journey towards resilience.
Your Endo Shopping List: Comfort Tools for Loved Ones
In case you need to do some last minute shopping and want to show your loved ones you understand, here are some essential items that have proven useful for many. While these tools may not be able to stop this awful disease, they may provide some degree of comfort and relief when things get bad. Whether you are prepping for surgery, or just need some handy tools, here are some of my favorite items.
- Wedge Pillow. This is a must for those preparing for surgery during recovery. I only found this at my 3rd (and hopefully last) surgery and it was a game changer. When your belly is full of air, tender, and you don’t feel like moving (or sitting up at the very least), this helps to provide relief for recovering in bed or on the couch and is great if you are a side or back sleeper.
- Heating pads. This is probably the number one item most endo warriors have – likely at home and work. They are always handy to have wherever you are, and for a more personalized gift, ETSY.COM has some amazing endo swag (including heating pads).
- My Obi Apollo. This is a TENS unit with heat and multiple programs to help with cramps and reduce pain. To learn more about how TENS may be helpful, check out our blog here.
- Squatty Potty. Everyone should have one. This is the gift that no one really wants, but secretly is so happy when they get one. It is essential for optimal toileting for everyone, but especially if you have endometriosis. Constipation and pelvic floor dysfunction are two issues the majority of those with endometriosis suffer from and this tool can make a world of a difference for toileting….
Until recently, endometriosis was not a term most people were familiar with, unless you are suffering. It is amazing how this is shifting and so many more people are familiar with the term, but may not understand how impactful this disease is to one’s life. Finding the right surgeon is key to address the lesions, but having tools to help in the meantime is crucial. More importantly, your loved one will most appreciate the effort you made to educate yourself about their disease, especially during the stress the holidays may bring. Give them the gift of understanding and empathy this year, and maybe something to help their pain in the meantime.
Please note: We do not have financial affiliations with any of these products listed above.
Related Reading:
- Find an Endometriosis Specialist for Diagnosis, Treatment, & Surgery
- Endometriosis Facts & Myths: Dispelling the Misconceptions
- What You Need to Know About Endometriosis Excision Surgery
- Managing Endometriosis: What You Need to Know.

Endometriosis and Painful Intercourse: Is it Really Just Endometriosis?
Table of contents
Those with endometriosis oftentimes will experience pain and discomfort with intercourse, especially pain with deep thrusting, also known as deep dyspareunia. However, many people also experience a different type of pain that extends beyond intercourse – superficial dyspareunia or pain upon entrance. Many people will have been diagnosed with ‘vaginismus’ and oftentimes given dilators, told to “just relax” or “have a glass of wine,” which is terrible advice. While some may have vaginismus, or pelvic floor dysfunction, for many the culprit could be that birth control pill that was given to you and advertised as a treatment for your endometriosis. It is a mixed bag on how many people benefit from the use of oral contraceptive pills (OCPs), and they can be a helpful tool for many. That being said, one thing is certain: medications always have consequences – sometimes good, sometimes not good.
In today’s blog, we will discuss a condition called vestibulodynia, and we will specifically cover hormonally associated vestibulodynia which is a prevalent health concern that results in pain in the vestibule, the tissue within the vulva at the opening of the vagina which also surrounds the urethra. It’s a subcategory of a broader term, vulvodynia, which refers to chronic pain in the vulva. This article aims to provide an in-depth understanding of vestibulodynia, its causes, symptoms, and effective treatment methods.
Vestibulodynia vs Vulvodynia vs Vaginismus?
Vestibulodynia is a general term used to describe discomfort in the vestibule, a part of the vulva that sits at the entrance of the vagina. The vestibule is the transition point between external and internal, similar to the entrance of a building. Vulvodynia is the broader category that includes vestibulodynia but can be pain anywhere in the vulva and typically is present for longer than three months and has specific causes and associated factors. Vaginismus lies within these and often is a misdiagnosis, the term refers to a chronic muscle spasm upon penetration or attempted penetration. This is one of the oldest terms used and while some may have true vaginismus, in the case of endometriosis there are much more likely causes, such as the birth control pill and other hormonal suppressive agents.
Think about it – if you touch a hot stove, the muscles in your shoulder and arm reflexively pull you away. If a penis, speculum, finger, or tampon hit tissue that is painful and irritated, the surrounding muscles will tense reflexively because it is painful. So yes, there is a muscle spasm, but the cause of the spasm is the inflamed and painful vestibule, possibly due to consequences from the birth control pill. There are other causes of pain here, which we will cover in future blogs.
Subtypes of Vestibulodynia
Recent research has led to the identification of a few subtypes of vestibulodynia based on the root cause of the discomfort:
· Neuroproliferative vestibulodynia
· Hormonally-mediated vestibulodynia
· Inflammatory vestibulodynia
The vestibule tissue is fundamentally different from the skin around it, developing from a different part of the embryo. This biological difference is crucial to understanding the causes of pain specifically in the vestibule. In this post, we will be reviewing hormonally mediated vestibulodynia, and in upcoming posts we will discuss neuroproliferative vestibulodynia as there are some interesting new research in the connection between neuroproliferative vestibulodynia and endometriosis.
Causes of Vestibulodynia
The reason why some individuals develop vestibulodynia while others do not, is still under investigation. However, a 2014 study suggests that there may be a genetic risk factor for developing vestibulodynia when taking anti-androgen medication.
Hormonally-mediated vestibulodynia can be caused by several factors, times in life or medications that alter hormones and result in a suboptimal state. This could be during periods of amenorrhea (lack of a period) in young adults, medications including combined oral contraceptive pills, aromatase inhibitors used in breast cancer, and other hormonal suppressive medications as well as acne medications (Accutane and Spironolactone). Periods in life that result in reduced hormones including breastfeeding (lactational amenorrhea) and perimenopause through menopause which we describe as GSM (genitourinary syndrome of menopause). The vestibule tissue is particularly sensitive to a lack of hormone signals, so for those with endometriosis, while your birth control may be helping your painful periods, it maybe causing you to have painful intercourse.
Symptoms of Vestibulodynia
Pain
Individuals with vestibulodynia typically experience discomfort at the entrance of the vagina, known as the vestibule. The pain in the vestibule can be described in many ways. People with hormonally-mediated vestibulodynia may describe their discomfort as burning, stinging, or tearing.
Provoked vestibulodynia refers to vestibular pain that occurs with touch or pressure, while unprovoked pain occurs spontaneously. Sometimes, it can be challenging to distinguish provoked from unprovoked pain before all triggers are recognized, especially when they are seemingly simple things like sitting or wearing tight clothing.
People often feel discomfort any time there is contact or pressure on the vestibule. This includes during vaginal penetration (dyspareunia), tampon use, and speculum exams. Day-to-day activities that put pressure on the vestibule, such as wearing tight clothing, sitting for long periods, or wiping with toilet paper, can also cause discomfort.
Urinary
Because this tissue also impacts the urethra, for some, the primary symptoms are urinary in nature. Urinary urgency, frequency, or UTI-like feelings without an infection are common and some will even receive a diagnosis of interstitial cystitis/painful bladder syndrome, also very common to see in those with endometriosis.
Pelvic Floor Tightness
It is believed that pelvic floor dysfunction may develop in people with vestibulodynia due to a subconscious guarding response against discomfort (remember the stove analogy). However, chronic tightening of the pelvic floor muscles can create more discomfort. The muscles can accumulate knots (trigger points) and become shortened and weak. The weakness is because the muscles are not functioning optimally, please do not go and do kegels!
Additional symptoms of pelvic floor dysfunction can include feeling tension, discomfort, and burning in the hips, legs, lower back, and vulva, especially the vestibule. One can also experience urinary symptoms like frequency, urgency, and leakage, as well as bowel symptoms like constipation or discomfort with bowel movements.
Diagnosis of Vestibulodynia
The first step towards diagnosing vestibulodynia is a thorough history of your story by a knowledgeable provider. Your story holds crucial clues to your diagnosis. People with hormonally-mediated vestibulodynia may have discomfort that developed later in life after any of the associated factors discussed above, including starting a medication, surgery, breastfeeding, or menopause.
Then there should be a very specific examination of the pelvis, vulva, and vagina. In patients with hormonally-mediated vestibulodynia, the vestibule usually appears very red and irritated (erythema), but also pale (mucosal pallor). The provider should manually examine the pelvic floor muscles to determine if there is excess tension in the muscles.
A process called a Q-tip test is essential for mapping discomfort in the vulva. The provider will gently press a cotton swab to each part of the vulva while the patient reports their degree of discomfort at each spot. It is important that the provider touch each region of the vestibule, all the way around the vaginal opening. The physical exam is extremely important prior to using dilators as this may cause more irritation because the cause (or one cause) of the muscle tension is the vestibule and needs attention before dilators come into treatment.
Some specialists will check labs including total testosterone, free testosterone, and SHBG (sex hormone binding globulin), and many with hormonally mediated vestibulodynia show altered levels; though you do not need labs to confirm this diagnosis.
Treatment of Vestibulodynia
Fortunately, in the case of hormonally-mediated vestibulodynia, the standard treatment has a very high success rate. If vestibulodynia developed after starting a medication that is known to affect hormone levels, then patients should stop taking that medication. Stopping the medication is often not enough to help the vestibule tissue heal quickly because hormone levels might stay low for a long time after taking birth control pills.
Providers should prescribe a topical hormone gel to apply directly to the vestibule to restore the hormone signals to the tissue. The standard is 0.01-0.03% estrogen and 0.1% testosterone gel. The hormone gel is usually made by a compounding pharmacy. Custom compounded medications are especially helpful if someone is sensitive to a medication’s base, the inactive ingredients, and needs a different base.
Patients typically use the gel 1 to 2 times daily and start to notice improvement in 6 to 12 weeks. Some patients stop using the hormone gel once the offending medication has been stopped for a while, but many women choose to stay on this therapy.
Support for Vestibulodynia Patients
There are many societies with interests in female sexual dysfunctions in addition to ISSWSH. The National Vulvodynia Association (NVA) is a US-based association founded by patient advocates that focuses specifically on vulvodynia. They provide some educational materials for the public and fund research of vulvodynia. Tight Lipped is also a patient facing, grass-roots, advocacy group helping to change medical education around this condition.
There are many online support groups and communities of patients who support each other on social media. To find fellow patients locally, ask a provider if they know of another patient seeking community or any local groups to join.
Conclusion
Understanding and effectively managing vestibulodynia necessitates a comprehensive understanding of its causes, symptoms, and treatments. The information in this article seeks to bridge the gap between scientific research and the general public, providing evidence-based insights into this prevalent health concern. If you are experiencing symptoms of vestibulodynia, seek advice from a healthcare professional. There is a broad range of treatment options available, and you are not alone in your journey towards healing and managing this condition.
While this article provides a comprehensive overview of vestibulodynia, it is essential to remember that each individual’s experience with the condition can vary. Therefore, it’s crucial to consult with healthcare professionals and consider personal circumstances when making decisions regarding management and treatment.
Find a specialist: www.isswsh.org
Additional reading:
- Managing Endometriosis: What You Need to Know
- Understanding the Relationship between Sex and Endometriosis
- Finding an Endometriosis Specialist: Your Guide to Effective Treatment
References:
- Rubin, R. W. C. (2022). Hormonally mediated vestibulodynia. Accessed from https://www.prosayla.com/articles/hormonally-mediated-vestibulodynia
- Burrows LJ, Goldstein AT. The treatment of vestibulodynia with topical estradiol and testosterone. Sex Med. 2013 Aug;1(1):30-3. doi: 10.1002/sm2.4. PMID: 25356284; PMCID: PMC4184715.

Pelvic Floor Physical Therapy: What you Need to Know
Table of contents
In recent years, pelvic floor physical therapy (PFPT) has increased in popularity, much like endometriosis. More people have at least heard the term, and it has caught the attention of mainstream media recently in FX’s American Horror Story: Delicate. Though I will say the depiction of what we do was a bit horrific if you’ve watched the show, PFPT is a crucial part of one’s endometriosis journey. While there has been a large (and much needed) increase in practitioners and social media reels, there are some things you need to know to find the right physical therapist for you.
In earlier blogs, we’ve posted about the benefits of PFPT before excision surgery as well as the benefits after excision surgery which you can find in the links listed below.
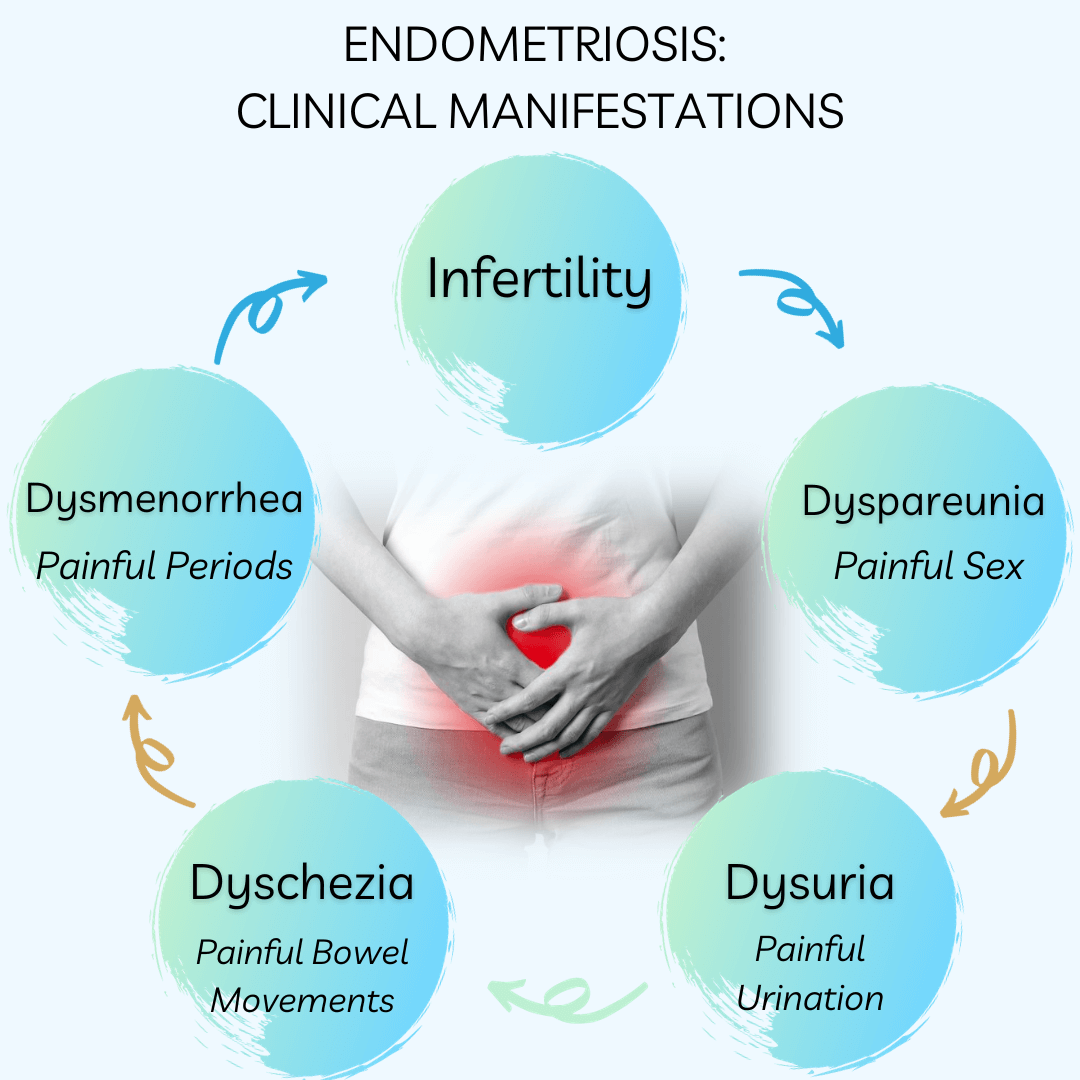
Endometriosis and the Pelvic Floor
Endometriosis is most recognized for its 5 clinical manifestations: infertility, dysmenorrhea (painful periods), dyspareunia (painful intercourse), dyschezia (painful bowel movements), and dysuria (painful urination). It is important to note that many of these manifestations may have alternative causes aside from endometriosis, many of which can stem from pelvic floor dysfunction. When it comes to endometriosis, one of the most frustrating parts is getting a diagnosis, especially because it truly requires surgical intervention for definitive confirmation. Something that we emphasize is that when it comes to endometriosis, it is important to address all of the pain generators in addition to the lesions themselves in order to have the best outcome.
Endometriosis has a 7-10 year delay in diagnosis, providing ample opportunity for additional symptoms to develop either because of progression of the disease, ongoing chronic pain causing physical limitations, or even due to side effects of “treatments” for endometriosis such as hormonal suppression therapies like birth control and GnRH agonists/antagonists.
One of the key aspects of endometriosis that is often underestimated is its association with pelvic floor muscle dysfunction. The pelvic floor muscles (PFMs) play a crucial role in supporting the pelvic organs, providing core stability, controlling bowel and bladder functions, and contributing to sexual arousal and orgasm.
Women with endometriosis often experience PFM dysfunction due to the chronic pain and inflammation caused by the disease. This can lead to a variety of problems, including hypertonia (excessive muscle tone), trigger points (painful knots in the muscles), and myofascial pain (pain in the muscle and its surrounding fascia).
The Role of Pelvic Floor Physical Therapy
PFPT is a specialized form of physical therapy focusing on the pelvic floor’s muscles, ligaments, and connective tissues, addressing issues from the knees to the rib cage and beyond. Contrary to common misconceptions, PFPT goes beyond postpartum care, challenging the notion of a one-size-fits-all solution like Kegel exercises. Those with endometriosis typically fall into the category of “hypertonic” or “high-tone” pelvic floor dysfunction versus weakness or “low-tone” pelvic floor dysfunction, and this needs a vastly different approach than kegels.
Understanding that not all PFPTs are equal, training variations exist, with many PTs needing additional education beyond basic training. PFPTs treating pelvic pain often require a multidisciplinary approach, encompassing interventional pain management and sexual medicine, which is often not taught in the additional courses PFPTs are required to take beyond their basic education in PT school.
The bottom line here is that if your PT only has training in treating “low-tone” pelvic floor dysfunction and is recommending kegels, you may need to see what other options are available. There is also no standardization in what is considered to be adequate pelvic floor PT, though there are some key aspects those specialized in pelvic pain will utilize.
- Manual Therapy including myofascial release and visceral mobilization, involves the use of hands-on techniques to manipulate the body’s tissues. This can help alleviate hypertonia and trigger points in the PFMs, improve circulation, and give different inputs to the nervous system resulting in reduced symptoms.
- Exercises which typically do not involve kegels, at least initially, will focus on exercises that reduce tension in the pelvic floor muscles and will progress to include exercises that optimize your biomechanics and when appropriate, facilitate return to your previous level of function which may include weight lifting, running, yoga, etc.
- Modalities such as TENS unit or e-stim, ultrasound, or biofeedback. Biofeedback may be very helpful for those who are visual learners or may be the only option in your area, but ultimately, these should be adjunct therapies to complement the other techniques vs. the focus of your sessions.
- Education is probably one of the most important pieces of what we do. As the provider that likely spends the most time with patients, we can help answer questions, provide support, and essentially act as your liaison between providers to help streamline care.
- Differential Diagnosis. While PTs cannot make medical diagnoses, we can help in better identifying pain generators and communicating this to your team. For example, if your main complaint is painful sex (dyspareunia), we can help differentiate whether this is due to tight and painful pelvic floor muscles, vestibulodynia (a type of vulvodynia specific to the tissue surrounding the urethra and vagina) which is associated with superficial dyspareunia (or entrance pain) vs. deep dyspareunia which is more associated with endometriosis, or specific palpation techniques that point more towards endometriosis lesions.
Additional Considerations
Finding a PT that fits your needs may be difficult as this is a specialty that needs more practitioners. However, if you are suffering from pain and are not getting the results you expect, the frequency and length of appointments may be a factor. Typically patients with pelvic pain benefit most with at least weekly, sometimes twice per week, appointments for at least 6-8 weeks to begin to see changes. Ideally each appointment is 40-60 min and involves a combination of techniques, especially manual therapy. Because PFPTs are hard to find, sometimes busy schedules do not allow for this treatment frequency, so don’t write off PT altogether if your outcome was less than optimal. Additionally, there is a wide range of techniques we utilize which vary depending on individual training. Most important, not everyone is a good fit for each person and it is really important to find a provider you feel comfortable with.
The Impact of Pelvic Floor Physical Therapy on Endometriosis
Through a combination of these techniques, pelvic floor physical therapy can have a significant impact on the management of endometriosis. Studies have shown that this form of therapy can help reduce pelvic pain, improve PFM function, and enhance overall quality of life for women with endometriosis.
Moreover, pelvic floor physical therapy can also help address some of the underlying issues associated with endometriosis, such as muscular dysfunction and chronic inflammation. By improving the function of the PFMs and reducing inflammation, this form of therapy can help alleviate some of the pain generators present in those with endometriosis, leading to more effective and long-lasting relief and better outcomes along with surgery.
While PFPT is instrumental, it should be part of a broader treatment plan that includes medical treatments, complementary therapies, and lifestyle changes. Integrating PFPT ensures that endometriosis patients receive comprehensive and effective care for the best outcomes.
By integrating pelvic floor physical therapy into the broader treatment plan, healthcare providers can help ensure that endometriosis patients receive the most comprehensive and effective care possible.
Check out our iCareBetter vetted physical therapists here.
Additional reading: Managing Endometriosis: What You Need to Know.
References:
- Wojcik, M., Szczepaniak, R., & Placek, K. (2022). Physiotherapy Management in Endometriosis. Int J Environ Res Public Health, 19(23). https://doi.org/10.3390/ijerph192316148
- Fraga, M. V., Oliveira Brito, L. G., Yela, D. A., de Mira, T. A., & Benetti-Pinto, C. L. (2021). Pelvic floor muscle dysfunctions in women with deep infiltrative endometriosis: An underestimated association. Int J Clin Pract, 75(8), e14350. https://doi.org/10.1111/ijcp.14350

Endometriosis Guidelines: A Closer Look at a Potential Source of Confusion in Treatment (Part 2)
Table of contents
Understanding Endometriosis Treatment Confusion
Endometriosis affects millions of women worldwide, presenting with pain, irregular menstruation, and infertility. To shed light on the most effective treatment methods, this article is Part 2 in our series on this topic. It summarizes and comments on the findings from a recent 2021 review which provided a detailed analysis of various endometriosis treatment global guidelines as of September 2020.
There are often some discrepancies between guidelines for any disease. However, for endometriosis, a prior review in 2018 revealed that only about 7% of recommendations were comparable between international guidelines. Up to 28% of the recommendations were not supported by good research evidence at all. This helps explain why there is such a wide variation between doctors’ recommendations in clinical practice.
Key Guidelines reviewed in the most recent publication were:
- American College of Obstetricians and Gynecologists (ACOG)–reviewed in our last post, which you can read HERE
- Society of Obstetricians and Gynaecologists of Canada (SOGC)
- European Society of Human Reproduction and Embryology (ESHRE)
- Australian National Endometriosis Clinical and Scientific Trials (ACCESS)
- Royal College of Obstetricians and Gynaecologists (RCOG)
- French National College of Gynecologists and Obstetricians (CNGOF)
- American Association of Gynecologic Laparoscopists (AAGL)
- German Society for Gynecology and Obstetrics (DGGG)
Summary Review of Treatment Recommendations
- Non-Hormonal Medical Pain Management
- Nonsteroidal anti-inflammatory drugs (NSAIDs): While this is considered by all guidelines to be first-line therapy for dysmenorrhea and acyclic pelvic pain, it is not specific for endometriosis. A diagnosis and targeted therapy is more prudent since a large review showed no difference in effectiveness between NSAIDs and placebo.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): While this is considered by all guidelines to be first-line therapy for dysmenorrhea and acyclic pelvic pain, it is not specific for endometriosis. A diagnosis and targeted therapy is more prudent since a large review showed no difference in effectiveness between NSAIDs and placebo.
- Hormonal Treatment Options:
- Progestins and Combined Oral Contraceptives (COCs): Widely recommended for initial pain management. Specific formulations and dosages vary across guidelines. Of interest, there is little mention of compounded micronized progesterone which is hard to study but may deserve a place in the conversation. The Levonorgestrel Intrauterine System (LNG-IUS) is particularly noted for its localized progestin delivery, reducing systemic side effects and effectively managing pain.
- Megace (Megestrol Acetate): A potent progestin recommended by several guidelines but varies as a first-line vs second-line option. The additional benefit is less bone loss than that seen with GnRH agonist therapy.
- GnRH Agonists: Uniformly recommended in all guidelines for severe symptoms after first-line therapy; potential side effects, which can be long-lasting, include decreased bone density and menopausal-like symptoms. Add-back low-dose estrogen therapy can reduce symptoms. Most guidelines, and the FDA, recommend durations of 6 months or less.
- Emerging Hormonal Therapies: GnRH antagonists are gaining attention for their rapid onset of action and fewer side effects compared to agonists. The evidence is not conclusive.
- Danazol and Gestrinone: Older treatments with androgenic effects, are less commonly used today due to side effects. Gestrinone is not currently available in the United States.
- Selective Estrogen Receptor Modulators (SERMs) and Selective Progesterone Receptor Modulators (SPRMs) are emerging options being explored for their targeted action and potential benefits.
- Aromatase Inhibitors: Considered in some cases, especially for pain unresponsive to other treatments. Most guidelines agree that this is a possible second-line option, but the evidence is not conclusive. A possible niche for effective use may be in post-menopausal patients who have endo.
- Surgical Approaches: Navigating the Complexities
- Laparoscopic Surgery: Endorsed for its efficacy and reduced recovery time, compared to big incision (laparotomy) surgery. However, the extent of surgery (complete vs. partial removal of lesions) varies among guidelines. Studies are likely hampered by different skill sets between participating surgeons.
- Robotic Surgery: AAGL and others highlight its benefits in complex cases, but its cost and accessibility limit widespread use. Specialized training is required.
- Ablation vs. Excision: The choice between these two methods remains a contentious topic, for some reason. Ablation is simpler and requires much less technical skill but is only applicable for treating superficial lesions. It may not be as effective in the long term as excision, which is more comprehensive and accurate in terms of removing all of the visible disease. Again, the skill base of surgeons is critical, and high variability in this regard may be affecting the ability to prove or disprove the effectiveness and safety of each.
- Endometrioma: Cystectomy or excision of endometriomas is superior to drainage in terms of lower recurrence. Excision also provides the opportunity for pathologic confirmation, and this may be important where it is not clear whether or not there is also a tumor present. Where fertility is a major concern, the more atraumatic the approach to surgery, the less ovarian reserve is affected, and this is another area where surgeon expertise is critical.
- Deep Infiltrating Endometriosis: Highly specialized excisional surgeries are recommended because ablation simply does not work with these lesions. There is an even stronger emphasis on the surgeon’s expertise and patient selection. Intuitively, the best outcomes probably rest with selecting the best possible technology in a master surgeon’s hands. Some strongly believe that this means robotic surgery for advanced cases with highly distorted anatomy.
- Hysterectomy: This is considered a “definitive” or last resort surgery but may be helpful for complete excision of endo at any point. It also allows the removal of any co-existing pain-producing adenomyosis, which is embedded in the wall of the uterus.
- LUNA (laparoscopic uterine nerve ablation) and PSN (presacral neurectomy): Guidelines reflect multiple reviews that suggest no benefit to LUNA but a possible benefit for PSN in selected cases. PSN is technically very challenging and treatment should be individualized. As far as LUNA is concerned, studies include a mix of ablation and excision, which means a lack of precision in many of them and, again, surgeon skill level may be a factor. Thus a definitive conclusion may be elusive until a better methodology to accurately study this is employed.
- Complementary and Alternative Therapies: Exploring Additional Avenues
- Acupuncture and Electrotherapy (TENS): Mentioned in some guidelines as adjunct therapies, with some encouraging results. More research is needed to fully validate their effectiveness. However, these are low-risk options.
- Nutritional Supplements: Some guidelines suggest that dietary changes and supplements might play a role in symptom management. This includes microbiome management for optimal estrogen metabolism. There will likely never be large randomized studies for any of these variables because they would have to be huge and thus impractical to conduct. But in today’s emerging world of personalized molecular medicine, other study methodologies are being explored to determine which of these approaches to diet and lifestyle may be more effective than others.
- Infertility and Endometriosis: A Delicate Balance
- Surgical vs. Non-Surgical Approaches: The decision to opt for surgery in infertility cases is complex and depends on individual factors like age, severity of endometriosis, and previous treatments. Reducing inflammation appears to be beneficial to effective intrauterine implantation and gestation.
- Surgical vs. Non-Surgical Approaches: The decision to opt for surgery in infertility cases is complex and depends on individual factors like age, severity of endometriosis, and previous treatments. Reducing inflammation appears to be beneficial to effective intrauterine implantation and gestation.
- Emerging Treatments and Research
- Future Directions: Ongoing research into immunotherapies, new hormonal agents, and gene/molecular therapy offer promising avenues for more personalized treatment strategies.
Endometriosis management is a highly dynamic field with evolving guidelines and currently very discrepant recommendations due to incomplete or low-quality scientific evidence. Understanding current options is crucial for women to make informed decisions about their health. Regular consultations with endometriosis experts, staying informed about new research, and considering a multi-disciplinary holistic approach to treatment can significantly improve quality of life.
Additional Reading:
- The Different Tests Used to Diagnose Endometriosis
- Laparoscopy: A Common Treatment for Endometriosis
References:
- Kalaitzopoulos, D. R., Samartzis, N., Kolovos, G. N., Mareti, E., Samartzis, E. P., Eberhard, M., Dinas, K., & Daniilidis, A. (2021). Treatment of endometriosis: a review with comparison of 8 guidelines. BMC Womens Health, 21(1), 397. https://doi.org/10.1186/s12905-021-01545-5
- Hirsch M, Begum MR, Paniz É, Barker C, Davis CJ, Duffy J. Diagnosis and management of endometriosis: a systematic review of international and national guidelines. BJOG. 2018;125(5):556–64.

Preparing for the Holidays: Tips for Managing Flares
Table of contents
As the holiday season approaches, individuals grappling with endometriosis or other chronic illnesses are contemplating how to sidestep discomfort and flare-ups. Despite our concerted efforts to prevent or mitigate the frequency and intensity of flares associated with endometriosis, the truth remains that flare-ups are inevitable.
The holiday season holds the promise of joy, connections, and quality time with loved ones for many, but for others, it may bring stress, indulgence, worry, temptation, or even apprehension. The prospect of navigating gatherings, grappling with uncomfortable inquiries, or being compelled to make challenging food choices after diligently avoiding certain items for an extended period can be disheartening. Although flares may be an inherent part of the journey at any given time, holidays are no exception. The good news is that there are strategies available to effectively manage or minimize flares during these festive times!
Managing endometriosis or any chronic illness during the holiday season can present unique challenges, but there are strategies to help minimize flares and make the most of the festive season. Here are some tips:
Plan and Pace Yourself
- Plan your activities and commitments wisely. Don’t overcommit to events or tasks.
- Prioritize what’s most important to you and conserve your energy for those activities.
Communicate Openly
- Communicate with friends and family about your condition. Let them know your limitations and needs.
- Be open about your health concerns, so they can better understand and support you during gatherings.
- Or have a script of what you may want to say to those you do not want to share this information with such as: “Thank you for asking, though I’d prefer not to share those details right now, thank you for understanding.”
For a list of resources for yourself or others, check these out:
Choose Your Events
- Select events that align with your energy levels and health status.
- It’s okay to decline invitations or leave early if you’re not feeling well.
Mindful Eating
- Food is more than just its ingredients and nutrients, food is a major part of many of our cultures, enjoy it!
- Remember, stressing about trigger foods may be just as triggering as enjoying some of your favorite dishes.
- Consider bringing a dish that aligns with your dietary restrictions to ensure there’s something you can comfortably eat.
- Eat prior to going to events to avoid overindulging in foods that may be a trigger for your symptoms.
Rest and Relaxation
- Schedule breaks for rest and relaxation. Give yourself permission to step away from activities and take time for self-care.
- Incorporate relaxation techniques such as deep breathing or meditation to manage stress.
Create a Comfortable Space:
- If attending gatherings, find a comfortable spot to rest if needed.
- Consider bringing a cushion, heating pad, or any other items that provide comfort during flare-ups.
Be Kind to Yourself
- Understand that flares may still happen despite your best efforts. Be kind to yourself and acknowledge that it’s okay to take a step back when needed.
Stay Connected
- Stay connected with supportive friends or online communities. Sharing experiences and tips with others who understand what you’re going through can be comforting.
Use your toolbox!
- For many, you have gathered your individual tools that have worked well for you in the past, don’t forget about these!
- Connect with your providers, if you haven’t seen your providers in a while, it may be helpful to touch base with your mental health therapist, nutritionist, or physical therapist.
- Maybe you opt for that less intense workout to give your body a break.
Remember, everyone’s experience with endometriosis is unique, so tailor these tips to your specific needs and preferences. It’s essential to prioritize your well-being and enjoy the holiday season in a way that works best for you.
For more on this topic, check out our blog Managing Endometriosis: What You Need to Know.

Endometriosis Guidelines: A Closer Look at a Potential Source of Confusion in Treatment Debates
Table of contents
Treatment strategies for endometriosis vary widely, with the primary objective being to alleviate pain and enhance fertility where necessary. However, the confusion and inconsistency in recommendations is alarming. This article reviews and comments on some of the key current management strategies supported by the American College of Obstetrics and Gynecologists (ACOG), by way of Bulletin #114 (2010 and reaffirmed in 2022) and Bulletin #760 concerning adolescents (2018 and reaffirmed 2022). In the following posts, we will review other guidelines to give a more in-depth look at these inconsistencies and what you may face as you navigate your journey with endometriosis.
Other internationally recognized bodies have published various guidelines seeking to help clinicians with the diagnosis and treatment of endometriosis. Unfortunately, there is significant discrepancy between some of the recommendations due to the complex nature of the disease and limitations of research to date. Many patients will look to online resources and forums after seeing providers and not seeing results. What they may be surprised to find is that information on sites dedicated to endometriosis are often inconsistent with what is proffered by different guideline resources.
Surgery
Surgery is considered a cornerstone in the management of pain and infertility associated with endometriosis. The timing of surgery and the type of surgery recommended varies between guidelines. However, it is illuminating to note that ACOG guideline Bulletin #114 states that “definitive diagnosis of endometriosis only can be made by histology of lesions removed at surgery.”
Minimally invasive surgery is highly preferred over open surgery (laparotomy) due to less pain, shorter hospital stay, quicker recovery, and better cosmetic results. However, a high level of skill and expertise is required to perform these procedures, whether it be laparoscopic or robotically assisted surgery. Despite better technology inherent in robotic surgery, outcomes research does not clearly show which modality is better overall. However, the skill of the surgeon likely trumps the surgical tools used. Robotic surgery may be better suited for particularly difficult cases involving severely distorted anatomy due to advanced endo or scarring from repeat surgeries.
The excision of endometriosis is widely recommended for patients with endometriosis-associated pain. However, there is ongoing debate on the preferred surgical technique (ablation versus excision) due to lack of conclusive evidence. Currently, the studies that look at excision surgery vs. ablation have significant limitations, potentially due to variation in the skill and training of the surgeons involved in these studies. Meaning, studies to date may not have been done by true excision specialists and resulted in incomplete removal thereby skewing the research results. This variation in surgeon expertise is a common plight affecting surgical procedure outcomes research.
In ovarian endometriosis (endometriomas or chocolate cysts), minimally invasive excision of endometriomas is superior to drainage and ablation in terms of reducing recurrence of dysmenorrhoea, dyspareunia, cyst recurrence, and the need for further surgical interventions.
In cases where women have completed their family planning and failed to respond to conservative treatments, hysterectomy with simultaneous excision of endometriotic lesions is considered the last resort. However, except for cases in which there is coexisting adenomyosis, hysterectomy is not necessarily required for pain relief purposes. Each situation should be highly individualized.
Medical Management of Endometriosis
While surgery is an effective treatment strategy and helps many patients, medical management currently plays a crucial role in managing symptoms and preserving fertility. These treatments primarily focus on pain management, hormonal suppression, and birth control.
Pain management is a critical aspect of endometriosis treatment. Non-steroidal anti-inflammatory drugs (NSAIDs) are widely used for symptomatic treatment of dysmenorrhea and acyclic pelvic pain. In fact, in their article discussing dysmenorrhea and endometriosis in adolescents, without any workup, ACOG believes that the majority of adolescents have primary dysmenorrhea which is defined as painful menstruation in the absence of pelvic pathology and recommends first line-therapies such as NSAIDs and birth control. The question is: without undergoing a definitive workup and assessment (surgery) for endometriosis and knowing that imaging is insufficient for diagnosis – how is it determined they do not have pelvic pathology? Furthermore, ACOG considers those that respond symptomatically to birth control pills and NSAIDs as a confirmation of primary dysmenorrhea, though some people with endometriosis also respond symptomatically to birth control pills and NSAIDs.
Hormonal suppression, through the use of progestins, combined oral contraceptives, micronized progesterone, or Gonadotropin-releasing hormone (GnRH) analogues, is a common treatment strategy. This recommendation assumes that estrogen is responsible for endometriosis, but this is based on an incomplete understanding of endometriosis genesis and progression. Hormones are clearly involved but, based on increasing molecular evidence, this is not the sole factor in promoting growth of endometriosis.
Birth control pills, specifically combined oral contraceptives, are often used as a first-line therapy for endometriosis-associated pain. This works by suppressing ovulation, which may help slow the growth of endometriotic tissue but has not been proven to induce regression or resolution.
GnRH analogues are recommended as second-line treatment options for endometriosis-associated pain. They work by suppressing the production of estrogen, thereby theroretically reducing the growth of endometriotic tissue. Along these lines, ACOG states that “there is no data that support the use of preoperative medical suppressive therapy,” yet in clinical practice, many individuals are offered these medications inconsistently related to consideration or timing of surgery. Additionally, their level B evidence (second level) recommendations state “After an appropriate pretreatment evaluation (to exclude other causes of chronic pelvic pain) and failure of initial treatment with OCs (oral contraceptives) and NSAIDS, empiric therapy with a 3-month course of a GnRH agonist is appropriate.” It can be argued that this is extremely problematic given that there is no conclusive data to support the use of these medications prior to surgery. Finally, there is a significant risk of short and potentially long term side effects and complications.
Complementary Therapies
Complementary therapies such as dietary interventions, acupuncture, and electrotherapy are increasingly being recognized as potential adjunctive treatments for endometriosis. Quite a bit is evidence supported, but more research is needed to fully establish their efficacy and safety. Thus guidelines do not routinely address such options, leaving patients to their own devices and trial and error.
In conclusion, the management of endometriosis requires a multi-faceted approach, incorporating both surgical and medical treatments which will be variable from patient to patient. In the past few years, there have been some improvements in the amount of research as well as advocacy. Finding a knowledgeable specialized surgeon and care team is of utmost importance. The majority of OBGYNs do not focus on endo, have not undergone further specialized training and generally align with the guidelines set forth by ACOG, largely driven by perceived medico-legal concerns related to standard of practice.. Furthermore, other guidelines seem to differ in their opinions and recommendations regarding medical management and surgery, so stay tuned for more information.
Related reading:
- Find an Endometriosis Specialist for Diagnosis, Treatment, & Surgery
- Why was iCareBetter built?
- What You Need to Know About Endometriosis Excision Surgery
References:
- Bulletins–Gynecology, A. C. o. P. (2000). ACOG practice bulletin. Medical management of endometriosis. Number 11, December 1999 (replaces Technical Bulletin Number 184, September 1993). Clinical management guidelines for obstetrician-gynecologists. Int J Gynaecol Obstet, 71(2), 183-196. https://doi.org/10.1016/s0020-7292(00)80034-x
- ACOG Committee Opinion No. 760: Dysmenorrhea and Endometriosis in the Adolescent. (2018). Obstet Gynecol, 132(6), e249-e258. https://doi.org/10.1097/AOG.0000000000002978
Endometriosis Affects Sexual Function: What You Need to Know
Many people know endometriosis as a “menstrual” disease or associate it with painful periods and/or infertility; however, endometriosis impacts many aspects of one’s life, including sexual function and intimacy.. This article aims to shed light on the complex interplay between endometriosis and sexual dysfunction, highlighting the critical points from recent scientific findings and providing an empathetic and informative perspective for those affected by the condition.
Table of contents
Impact on Sexuality
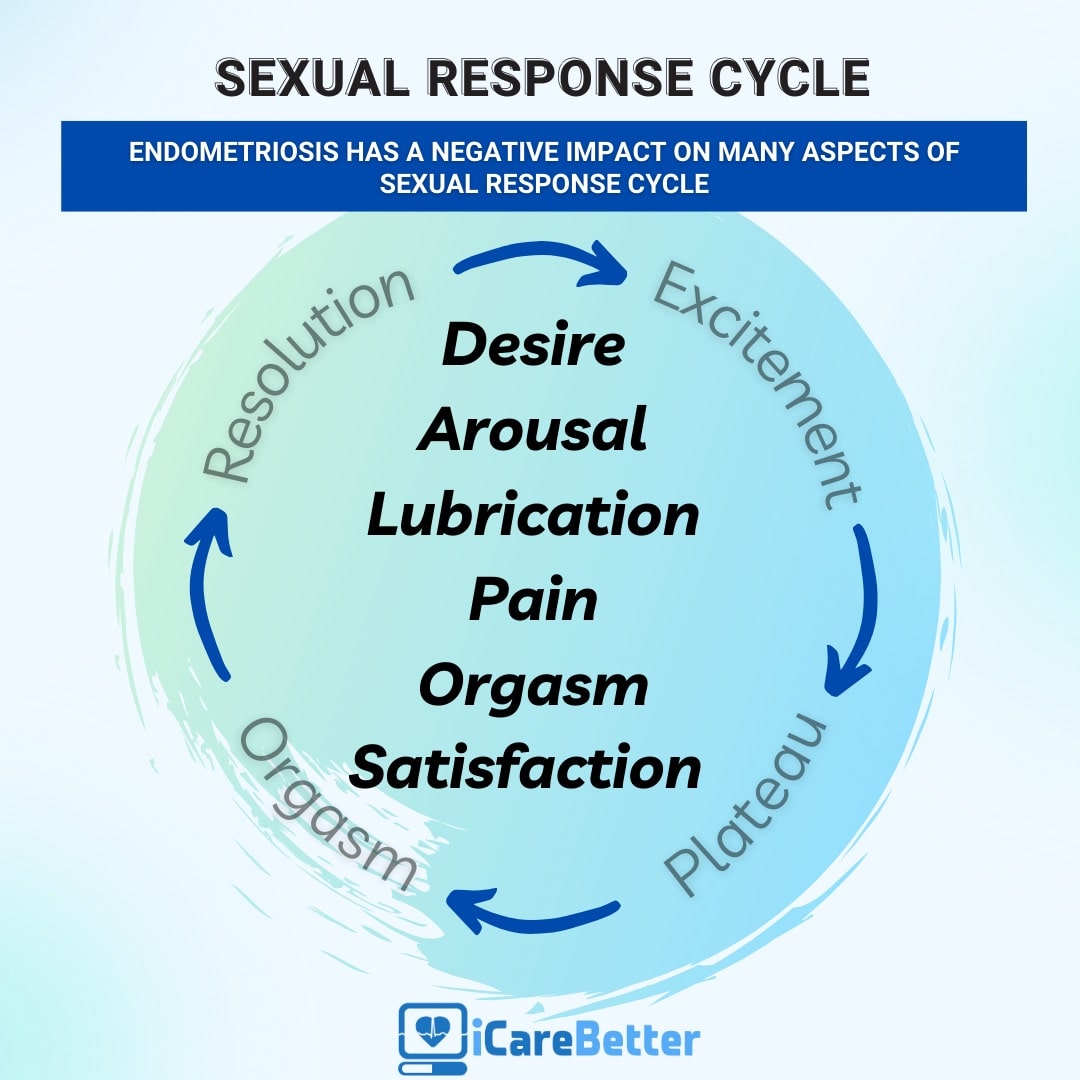
Endometriosis is notorious for causing severe pelvic pain, which is often exacerbated during menstruation. However, its effect extends beyond physical discomfort, with a significant impact on a woman’s sexual function. The correlation between endometriosis and sexual dysfunction is a compelling topic for scientific research, as it profoundly affects the quality of life of those living with this condition. One of the primary clinical manifestations of endometriosis is dyspareunia. What is important to know is that the lesions may directly cause deep dyspareunia (pain with deep thrusting), though the lesions as well as ‘treatments’ for endometriosis may also impact sexual functioning and leads to a decrease in sexual desire or arousal, resulting in a cycle of distress and avoidance of sexual intimacy.
Beyond Pain: Emotional and Psychological Effects
The effects of endometriosis on sexual function aren’t limited to physical symptoms. The condition can also trigger feelings of anxiety, distress, and guilt, affecting a woman’s self-esteem and overall mental health. Furthermore, the chronic nature of endometriosis and its association with infertility can impose additional psychological stress, further exacerbating sexual dysfunction. Over time, one may anticipate the pain, or have anxiety about what the sexual experience may be like, therefore causing reduced desire and arousal, or resulting in avoidance of sex or intimacy altogether.
Understanding the Prevalence of Sexual Dysfunction in Endometriosis
A significant proportion of women living with endometriosis experience some form of sexual dysfunction. However, the severity and type of dysfunction can vary greatly, influenced by factors such as the type and extent of endometriosis, individual pain tolerance, and psychological well being.
Several scientific studies have delved into the intricate relationship between endometriosis and sexual dysfunction. A systematic review of nine studies conducted between 2000 and 2016 found that around two-thirds of women with endometriosis experienced some form of sexual dysfunction. These dysfunctions extended beyond deep dyspareunia, encompassing issues like hypoactive sexual desire, arousal problems, and orgasmic disorders.
The Role of Deep Infiltrating Endometriosis (DIE)
Deep Infiltrating Endometriosis (DIE), a severe form of the disease, is often associated with a higher prevalence of sexual dysfunction. Studies focusing on patients with DIE have found a significant impairment in various aspects of sexual functioning, including satisfaction, frequency of intercourse, and orgasm.
The Multidimensional Nature of Human Sexuality
Human sexuality is a complex phenomenon, influenced by a multitude of physical, psychological, and relational factors. As such, sexual dysfunction in women with endometriosis is not solely a result of physical pain but can also be shaped by the individual’s mental health and the quality of their intimate relationships.
Psychological distress, often associated with chronic pelvic pain, can significantly affect sexual functioning. Women living with endometriosis often experience anxiety and depression, which can act as powerful inhibitors of the sexual response cycle.
The quality of intimate relationships plays a crucial role in shaping sexual function. Marital satisfaction, perceived partner support, and the degree of intimacy can significantly influence the sexual experiences of women living with endometriosis.
Addressing Sexual Dysfunction in Endometriosis: A Multidisciplinary Approach
Given the multifaceted nature of sexual dysfunction in endometriosis, a comprehensive and multidisciplinary approach is crucial for effective management. Such an approach extends beyond medical treatment for painful symptoms, encompassing psychological support and psychosexual therapy.
Your general gynecologist or endometriosis specialist may not necessarily be the person to also address your sexual dysfunction. This is a major area in which many providers are not trained in. ISSWSH, which stands for the International Society for the Study of Women’s Sexual Health, is an international, multidisciplinary organization that focuses on sexual health. Often, these people are the ones you want to see in regards to your sexual dysfunction. They include urologists, gynecologists, mental health professionals, physical therapists, nurse practitioners and more.
Psychological support is crucial in managing the mental health challenges associated with endometriosis. Therapists and psychologists can provide coping strategies for anxiety and depression, addressing feelings of guilt and distress associated with sexual dysfunction.
Empowerment Through Knowledge
Education and awareness are powerful tools in managing endometriosis and its impact on sexual function. By understanding the nature of the disease and its potential effects on their sexual health, women can seek appropriate help and take proactive steps towards improving their quality of life.
Endometriosis and its impact on sexual function is a complex issue, requiring a multifaceted, compassionate, and patient-centric approach. By acknowledging the physical, psychological, and relational aspects of sexual dysfunction, healthcare professionals can provide holistic support to those living with endometriosis, empowering them to navigate the challenges of this chronic condition and enhancing their overall quality of life.
Related reading:
- Endometriosis Pain after Orgasm: What You Need to Know
- Understanding the Relationship between Sex and Endometriosis
- What You Need to Know About Endometriosis and Intimacy
References:Barbara, G., Facchin, F., Buggio, L., Somigliana, E., Berlanda, N., Kustermann, A., & Vercellini, P. (2017). What Is Known and Unknown About the Association Between Endometriosis and Sexual Functioning: A Systematic Review of the Literature. Reprod Sci, 24(12), 1566-1576. https://doi.org/10.1177/1933719117707054
Understanding Endometriosis: Unveiling the Common Symptoms and Their Impact
Table of contents
A recent article from Australia on common symptoms and endometriosis was released recently that followed several thousand women that were both surgically and clinically diagnosed (evaluated separately) with endometriosis and their symptoms to look at associations. There are minimal longitudinal studies available, so this article can be very impactful in raising awareness of the variable, but common, symptoms those with endometriosis experience.
Endometriosis, a chronic gynecologic disorder, is characterized by the presence of endometrium-like tissue outside the uterus. This condition has a profound impact on women’s (XX) lives, often leading to increased hospitalizations, diminished work productivity, and a reduced quality of life. While menstrual symptoms are the most commonly associated with endometriosis, an array of other symptoms can significantly affect the physical and mental wellbeing of women diagnosed with this condition. This article aims to provide an in-depth understanding of the common symptoms associated with endometriosis and their impact on women’s health.
The Prevalence of Endometriosis
Endometriosis is a prevalent health condition affecting approximately 1 in 9 women (11.4%) in Australia by the age of 44 years and in the US the estimation is 1 in 10, though this may be inaccurate due to the significant delay or issues with misdiagnosis. The nonspecific nature and normalization of the symptoms often lead to a significant delay in the diagnosis of endometriosis, with several studies reporting an average delay of 7 to 11 years. This delay in diagnosis results in untreated endometriosis-related symptoms, increased hospitalizations, higher healthcare resource utilization, and potentially reduced success using assisted reproductive technologies. Additionally, some of the overlapping symptoms may be due to the “treatments” offered for symptom management such as hormonal supressive therapies.
Endometriosis and Menstrual Symptoms
Women diagnosed with endometriosis frequently report an array of menstrual symptoms. These may include severe period pain (dysmenorrhea), heavy menstrual bleeding, irregular periods, and premenstrual tension. The association between endometriosis and these symptoms is strong, with the odds ratio for severe period pain being as high as 3.61.
Endometriosis and Mental Health Problems
Apart from physical discomfort, endometriosis can significantly affect a woman’s mental health. Studies reveal a higher incidence of mental health problems, including depression, anxiety, and other mental health disorders, in women with endometriosis. The adjusted odds ratios for depression and anxiety are 1.67 and 1.59, respectively.
Endometriosis and Bowel Symptoms
Bowel symptoms are another common complaint among women with endometriosis. These may include constipation, hemorrhoids or piles, indigestion, or heartburn, bloating, diarrhea, or a combination of these. Additionally, one of the clinical manifestations is dyschezia, or discomfort/pain associated with bowel movements. The adjusted odds ratio for constipation is 1.67, indicating a significant association between endometriosis and bowel symptoms. Additional studies have demonstrated that approximately 90% of those with endometriosis have IBS-like symptoms.
Endometriosis and Urinary Symptoms
Urinary symptoms, such as burning with urination (dysuria) and vaginal discharge or irritation, are also more prevalent in women with endometriosis. The increased odds of urinary symptoms suggest a possible alteration in the pelvic innervation caused by endometriotic lesions.
Endometriosis and Pain Symptoms
Endometriosis is often associated with other forms of pain, including back pain, headaches or migraines, and stiff or painful joints. The adjusted odds ratios for these pain symptoms range from 1.50 to 1.76, further emphasizing the multifaceted impact of endometriosis on women’s health.
Endometriosis and Nonspecific Symptoms
In addition to the symptoms described above, endometriosis is also linked to various nonspecific symptoms. These may include severe tiredness, difficulty sleeping, palpitations, and allergies or hay fever or sinusitis. The association between endometriosis and these symptoms underlines the complex nature of this condition and its wide-ranging effects on women’s health.We need more understanding whether these symptoms are a direct result of the endometriosis, the side effects of treatments, or another related issue.
The Importance of Early Diagnosis
Given the wide array of symptoms associated with endometriosis and their significant impact on a woman’s quality of life, the importance of early diagnosis and treatment cannot be overstated. Early intervention can not only alleviate the physical discomfort associated with the disease but also significantly improve mental health outcomes. Furthermore, it can potentially prevent the development of chronic pain conditions and other long-term health complications.
Conclusion
Endometriosis is a complex condition that affects multiple aspects of a woman’s health. It is associated with a wide range of symptoms, extending beyond menstrual problems to include mental health issues, bowel and urinary symptoms, pain, and other nonspecific symptoms. Understanding these symptoms and their impact on women’s lives is crucial for providing comprehensive care to those diagnosed with this condition. While further research is needed to elucidate the specific mechanisms underlying these associations, the current evidence underscores the importance of early diagnosis and intervention in improving health outcomes for women with endometriosis.
Related reading:
- Understanding fatigue and endometriosis: A Practical No-Nonsense Guide
- Interstitial Cystitis and Endometriosis: Unraveling the “Evil Twins” Syndrome of Chronic Pelvic Pain
- Endometriosis Signs and Symptoms: Everything You Need to Know
References:
- Gete DG, Doust J, Mortlock S, et al. Associations between endometriosis and common symptoms: findings from the Australian Longitudinal Study on Women’s Health. Am J Obstet Gynecol 2023;229:536.e1-20.
Choosing Your Battle Against Endometriosis: Understanding Excision, Ablation, and Robotic Techniques
Table of contents
The gold standard for diagnosis of endometriosis, a chronic, debilitating condition impacting millions of women (XX), is minimally invasive surgery with histological confirmation. Due to advancements and understanding of the disease, we now recommend that surgical treatment of the lesions be performed at the same time as a diagnostic surgery. It is well understood and agreed upon that in order to obtain a biopsy, the tissue must be removed and excised for analysis but the type of surgical approach to address the lesions is not consistent among all practitioners.
If you were to ask someone well versed in endometriosis such as an endometriosis excision surgeon or even a patient advocate who is well up to date on their understanding and research, you’d likely hear that excision surgery is the gold standard for treatment and the preferred approach is minimally invasive. However, there are still those who would provide a counterargument stating that there is a place for ablation, especially, according to some guidelines, in the pediatric and adolescent age group. Those who proffer minimally invasive excision surgery differ in opinion about the adequacy of older technology laparoscopy vs. the technical benefits of robotically assisted enhancements.
This article aims to provide some insight as to the understanding and nuances behind these arguments, and the limitations in the current research, as well as provide a comprehensive guide on the different treatment approaches for endometriosis, including excision surgery, robotic surgery, and the role of ablation.
Understanding Endometriosis
Endometriosis is a heterogeneous, inflammatory condition where endometrial-like tissue is found throughout the body, typically in the abdominopelvic cavity. While some patients with endometriosis can remain asymptomatic, an estimated 35-50% experience severe pelvic pain, infertility, and other symptoms related to the location of the endometriosis lesions or implants. Endo is intensely inflammatory and fibrogenic, which often creates huge anatomic distortion, causing infertility and pain. Tackling endo surgically requires advanced skills for these reasons.
Current and Future Treatment Approaches for Endometriosis
Today’s treatment options are largely limited to hormonal manipulation and surgery. According to various medical advisory organizations, medical therapies should be offered as first-line therapies to alleviate endometriosis symptoms and potentially treat the endo, and then surgical intervention becomes an option. Sometimes surgery is only offered when pain is not alleviated, potentially allowing the endometriosis and resulting fibrosis to grow.
There is a strong counterargument to starting with medical/hormonal therapy, which is often initiated based on clinical symptoms and findings that suggest endometriosis may be present. Leading with medical treatment, which can have significant and lasting side effects, means potentially injurious and ineffective treatment can be prescribed when in fact there is no endometriosis present. In addition, due to relative progesterone resistance, symptoms may be ameliorated but the aberrant endometriotic tissue is not usually eradicated. Meanwhile, fibrosis from your body’s healing efforts continues to accumulate. Therefore, excision may be considered a cornerstone initial step to remove the macroscopically evident bulk of disease followed by potential preventive strategies to suppress any residual microscopic disease after the diagnosis is pathologically established.
Excising all visible lesions, associated adhesions, and scarring or fibrosis, is thought to reduce disease recurrence, relieve pain, and enhance fertility rates. However, while this can provide long-term relief, it is not usually curative. In complex endometriosis cases (stage III or IV according to the revised American Society for Reproductive Medicine classification), achieving the goal of safe and complete excision of visible lesions, especially using conventional laparoscopy can be technically challenging, and requires specialized training.
While this article is not focused on other treatment options, keep in mind that holistic, nutritional, Eastern and natural approaches have a role in alleviating symptoms and, to a degree, can influence the course of endo as well.
Future treatments on the horizon will go far beyond surgery and hormonal manipulation. We already know that there are other molecular pathways that drive endo growth and these will eventually be effectively harnessed for diagnostics, monitoring, and treatment. Some of these pathways can already be influenced by nutritional and other holistic methods.
Excision Surgery for Endometriosis
Excision surgery, most often performed via laparoscopy or robotics, has largely replaced ablation and big incision surgery. There is general agreement that minimally invasive surgery is superior to big incision (laparotomy) type of surgery. However, ablation is still commonly performed, partly because it is simply easier and requires far less skill.
During excisional surgery, visible endometriosis lesions are removed, which studies have shown significantly reduces the rate of disease recurrence and associated pelvic pain. However, not all studies clearly support excision over ablation. Additional research is required to settle this question and this is very difficult to do because of the extremely wide variance of surgeon skill. Suffice it to say that publications by experts in excisional surgery seem to clearly support this technique over ablation.
The technical aspects of laparoscopy and robotics, as well as the surgeon’s expertise, dexterity, surgical precision, coordination, and visualization limitations, can cause complications during surgical dissection to vary widely, particularly in severe endometriosis cases. For this reason, it is prudent that a surgeon trained in specialized excision techniques perform these surgeries to minimize complications as well as to ensure adequate removal of all visible lesions.
Robotic Surgery for Endometriosis
Over the past fifteen years, robotically enhanced surgery has emerged as an additional tool that can help circumvent the technical challenges of conventional laparoscopy. It offers several advanced features, including 3-D and magnified visualization, wristed instruments, motion scaling, and ergonomic positioning for the surgeon. But what does this mean in terms of benefits to you as the patient?
First, 3-D technology and magnified view mean that the surgeon can see every little detail which conventional 2-dimensional laparoscopy may not allow the surgeon to discriminate, even using so-called “near contact laparoscopy.” This is because magnified 3-D allows depth perception so that even sub-millimeter irregularities on the peritoneal surface can be identified. Also, in a difficult case with distorted anatomy, it allows the surgeon to better avoid damaging adjacent organs, like the bowel and ureters.
Second, the instruments at the tips are “wristed”, meaning they behave like tiny human hands. Conventional laparoscopic instruments are straight sticks with scissors or graspers at the end, which can limit options in tight spaces to cut, push, pull and tear. Robotic wristed instruments can result in more precise motions to excise endo in difficult places and avoid bleeding and other complications.
Third, the fulcrum of activity during conventional laparoscopy is the abdominal wall. When the surgeon moves the instruments, because of their straight nature, the abdominal wall is constantly being tweaked and traumatized. In contradistinction, since the surgical activity fulcrum is at the instrument tips during robotic surgery, there is less ongoing trauma to the abdominal wall. This results in less abdominal wall pain over the first hours and days after surgery.
Fourth, the risk of needing to convert to a big incision because the surgery is not going well using minimally invasive surgery is higher for laparoscopy compared to robotics. So, you have twice the risk of waking up with a much bigger incision during a planned conventional laparoscopy. Big incisions are prone to hernia and infection, not to mention more painful during recovery. Generally, the more difficult the surgery the higher the conversion risk. Unfortunately, it is not possible with endometriosis (due to its intensely inflammatory and scarring nature) to accurately predict what is going to be an easy vs difficult surgery. This is truly a case of an ounce of prevention (optimal preparedness) being worth a pound of cure (getting caught with inadequate instruments for the job and then trying to scramble and fix it).
Research Comparing Robotic Surgery with Conventional Laparoscopy
Several studies have been conducted to compare the efficacy of robotic surgery and conventional laparoscopy in treating endometriosis. A meta-analysis by Chen et al. evaluated the safety and efficacy of robotic surgery for treating advanced-stage endometriosis. The study concluded that while robotic surgery was safe and efficient, it was also time-consuming and incurred higher costs compared to conventional laparoscopy. Studies like this are hard to interpret because it is not possible to know the real skill base of the surgeons involved, which means conclusions about costs and efficiencies are suspect. Also, it’s important to keep in mind that from the patient’s perspective, this cost is irrelevant. The costs are almost all absorbed by the hospital or surgery center and not directly passed on to the patient.
The bottom line is that an experienced laparoscopic excision surgeon will likely be able to get the right surgery done safely in straightforward and moderately complicated cases. A robotic surgeon should be vested enough in the newer technology (i.e., does a lot of robotic surgery, if not all robotics) to realize a difference. In other words, in most cases, the surgeon is the most important part. However, due to the superior technology, a highly skilled robotic surgeon will likely complete a complicated case safely (e.g., Stage III or IV with multiple prior surgeries), without conversion to a big incision, more often than a highly skilled laparoscopic surgeon, due to the limitations of inferior technology.
From a practical perspective, you can experience/simulate the difference yourself between 2-D and 3-D vision or between straight stick laparoscopic surgery vs wristed robotics technology. Wear a patch or tape one eye closed and immobilize your elbows and wrists with splints and tape, leaving only two fingers to grasp things with, and go about your daily business (NOTE: please don’t do this without someone assisting you because you will find that you misjudge distances and are unable to carry out tasks safely). Can you adjust to this handicap over time? Of course, as can a surgeon. However, it is certainly not optimal to avoid using your wrists and both eyes if you have a choice.
Robotic Surgery for Deep Infiltrating Endometriosis (DIE) and Extragential Endometriosis
DIE is a severe form of endometriosis characterized by endometrial tissue growth more than 5mm deep into the peritoneum. Approximately 40% of patients with endometriosis suffer from DIE. DIE can cause dense adhesions and fibrosis, distorting pelvic structures, including genital organs, the bowel, and the urinary tract, causing severe pelvic pain. There is also an overlap of molecular abnormality markers (primarily ARID1A mutations) between DIE and clear cell cancer arising from endometriosis. This has led researchers to suggest that the DIE type of endo is pre-malignant. Removing DIE requires an even higher skill base, and robotics can facilitate far safer and complete surgery for the reasons noted above.
Ablation for Endometriosis
Let’s consider the technique of ablation, as opposed to excision, in a little more detail. This procedure involves destroying endometrial lesions using heat or laser energy rather than removing them. This method was introduced in the 70’s but has significant limitations. The issue with ablation is that while it may be adequate for very superficial disease, it does not remove the lesion, and more importantly, you cannot determine how deep the lesion goes by burning the surface and not carefully excising the lesion. Ultimately this can leave behind endometriosis which can continue to wreak havoc on the body. In addition, the more trauma to your body (ablation via thermal damage is more traumatic than precise excision), the more your body resorts to scarring and fibrosis for healing. This fibrosis can continue to cause pain and lead to complications like urinary system obstruction. Finally, the ureters ( tubes that connect your kidneys to your bladder) and bowel are often right underneath endo lesions. These are thin, delicate structures that are in danger of damage by thermal spread. If they leak due to damage this can lead to emergency surgery, colostomy (wearing a bag for stool on your belly), urinary reconstruction and even death. Therefore, it should only be done in circumstances where the risk is low, such as the eradication of tiny endo superficial ovarian lesions when all else (including endometriomas) has been excised.
Conclusion
Regardless of the approach to excision – robotic or conventional laparoscopy, the need for better research utilizing highly skilled surgeons performing wide-excision is needed to definitively demonstrate the superior overall benefits compared to ablation surgeries. As of now, research is relatively sparse due to flaws in the research process discussed in this article and many more statistical reasons. Again, we are burdened by a lack of superlative surgeons and this is not a surgery for less skilled surgeons to dabble in, whether it be in research study participation or patient care. As a result, the lack of absolute positive outcome superiority currently impacts the availability and insurance reimbursement for those seeking a safe and effective excision surgery. At this time, since everyone’s situation is different, the best course of action is to get an expert opinion from the best endometriosis specialist you can find.
Looking for a specialist? Check out our related blogs:
- Finding an Endometriosis Specialist: Your Guide to Effective Treatment
- Find an Endometriosis Specialist for Diagnosis, Treatment, & Surgery
N.B. The above is based on a combination of published data and the author-surgeon’s personal experience, spanning over three decades, using both laparoscopy and robotic surgery for advanced excisional surgery, inclusive of advanced endometriosis and radical cancer excision.
References
- Pundir, J., Omanwa, K., Kovoor, E., Pundir, V., Lancaster, G., & Barton-Smith, P. (2017). Laparoscopic Excision Versus Ablation for Endometriosis-associated Pain: An Updated Systematic Review and Meta-analysis. J Minim Invasive Gynecol, 24(5), 747-756. https://doi.org/10.1016/j.jmig.2017.04.008
- Kang, J.-H., & Kim, T.-J. (2020). The role of robotic surgery for endometriosis. Gynecologic Robotic Surgery, 1(2), 36-49. https://doi.org/10.36637/grs.2020.00045
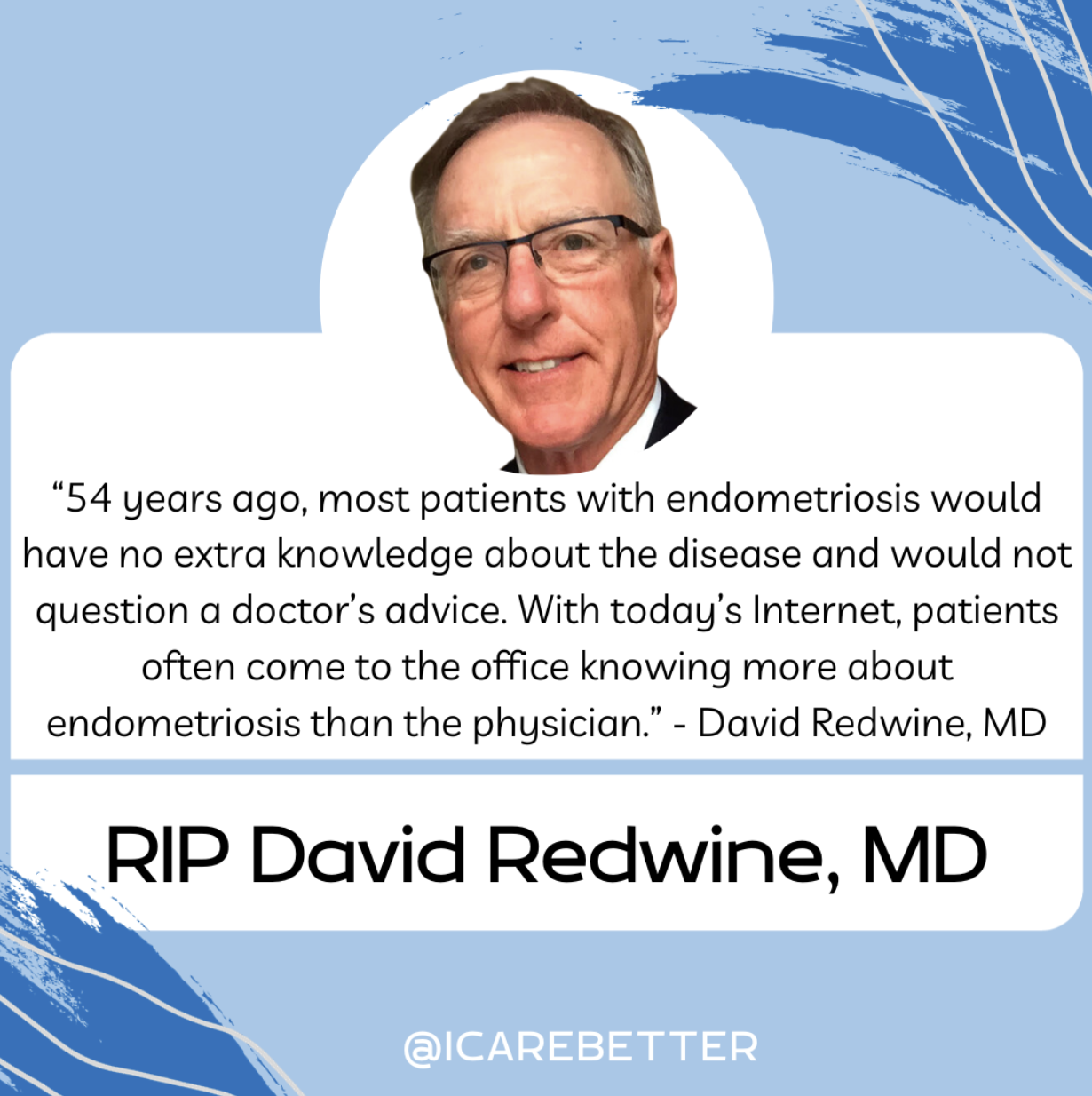
Dr. David Redwine Obituary : A Modern Hero in Endometriosis Research and Excision Surgery
The recent death of David Redwine has undoubtedly left many with sadness and devastation. Our thoughts are with his friends, family, colleagues, and the endometriosis community as a whole. The world of gynecology has been significantly influenced and transformed by the groundbreaking work of Dr. David Redwine, a significant contributor to those suffering from this disease. A modern hero in this community in his contributions to endometriosis research, excision surgery, and fighting alongside patients and advocating for better answers and better care. His innovative approaches and relentless pursuit of knowledge have positioned him as a leading advocate for patients with endometriosis, a debilitating condition that affects millions of women worldwide.
Table of contents
Who is David Redwine?
A formidable figure in the medical community, Dr. David Redwine has devoted his career to understanding and treating endometriosis. His profound commitment to research and patient care has made him a renowned authority in the field.
Redwine’s Contribution to the Understanding of Endometriosis
Endometriosis is a complex and often misunderstood condition. Dr. Redwine’s research has been instrumental in challenging established theories and introducing new perspectives on the origins and treatment of the disease.
Challenging Sampson’s Theory
One of the most significant contributions of Dr. Redwine has been his challenge to the widely accepted Sampson’s Theory of endometriosis. The theory, proposed by Dr. John Sampson in the 1920s, suggests that endometriosis is caused by retrograde menstruation, where menstrual blood containing endometrial cells flows back through the fallopian tubes and into the pelvic cavity. Redwine questioned the validity of this theory, arguing that if retrograde menstruation were indeed the cause of endometriosis, there should be ample microscopic evidence of refluxed endometrial cells attaching to the pelvic lining and subsequently proliferating. Yet, such evidence is conspicuously lacking. While modern day understanding by experts support alternative theories and are moving toward more plausible explanations, Dr. Redwine is largely to thank for this movement.
Proposing an Embryonic Origin
In place of Sampson’s Theory, Redwine proposed that endometriosis originates from an embryonic source. He argued that endometriosis is derived from mesoderm, the middle layer of the three embryonic layers, and is a result of abnormal differentiation and migration of cells during embryonic formation of the female reproductive tract. This theory suggests that endometriosis is a congenital condition that can manifest later in life under the influence of hormones and other factors.
The Concept of Mulleriosis
To further elucidate the embryonic origin of endometriosis, Redwine introduced the concept of ‘Mulleriosis.’ This term embraces a wider perspective, encompassing all pathologies associated with abnormal development of the Mullerian ducts, the precursor structures to the female reproductive organs.
Redwine’s Innovations in Endometriosis Surgery
Dr. Redwine has not only helped reshape our understanding of endometriosis but also revolutionized its treatment. He is a staunch advocate for excision surgery, a procedure that aims to completely remove endometriosis lesions. While early surgeries also focused on excision surgery, though lacking the precision and advanced technology we have today, the introduction of ablation surgery in the 70’s has complicated research findings, surgical outcomes, and the overall role of surgery in the treatment of this disease resulting in a further push towards hormonal suppression and the fight against Big Pharma.
The Importance of Excision Surgery
Whereas traditional first-line therapies often rely on hormonal therapy or less thorough surgical methods, Redwine emphasizes the importance of excision surgery in effectively treating endometriosis. Through extensive research and practice, he has demonstrated that excision surgery can significantly alleviate symptoms and improve the quality of life for patients with endometriosis.
The Concept of Cure
Contrary to the prevalent belief that endometriosis is incurable, Redwine insists that the disease can be effectively treated through excision surgery. He defines ‘cure’ as the complete absence of the disease, as proven by follow-up laparoscopy. While this topic may be nuanced to a degree and there are cases of regrowth, those of who have undergone a true excision surgery, and those that perform skilled excision surgery understand the difference of persistent pain vs. incomplete technique.
Redwine’s Advocacy for Patients with Endometriosis
In addition to his clinical and research work, Dr. David Redwine is a passionate advocate for patients with endometriosis. He strongly believes in empowering patients with knowledge about their condition and available treatment options.
Redwine is committed to educating both the medical community and the public about endometriosis. He regularly delivers lectures and presentations, sharing his insights and the latest research findings. His dedication to education aims to foster a more informed and empathetic understanding of endometriosis.
As a fervent advocate for patient-centered care, Redwine emphasizes the need to listen to patients’ experiences and concerns. He argues that an effective treatment approach should consider not only the physical manifestations of the disease but also its impact on a patient’s mental and emotional well-being.
You Will Be Missed!
Dr. David Redwine’s pioneering work in endometriosis research, excision surgery, and patient advocacy has had a profound impact on the understanding and treatment of the disease. His unwavering dedication to advancing knowledge and improving patient care serves as an inspiration for both medical professionals and patients alike. Dr. Redwine’s contributions will undoubtedly continue to shape the future of endometriosis care and research, despite his recent passing. His name will always be known in this community for the significant contributions he has made and the patients whom he has helped whether directly, or indirectly.
Rest in peace Dr. Redwine, you will be missed.

