
Chronic fatigue syndrome and endometriosis
While no strong studies have been performed on endometriosis and chronic fatigue syndrome (also called myalgic encephalomyelitis)(CFS/ME), CFS/ME has been found with some frequency in those with endometriosis. This doesn’t mean that one causes the other. Rather it indicates that they can often be found present together, like we see with migraines and endometriosis. It is good to consider that there may be some overlapping symptoms and that more than one etiology may be present.
Boneva et al. (2019) reports that:
“Chronic fatigue syndrome (CFS), also referred to as myalgic encephalomyelitis (ME) or ME/CFS, is a serious chronic condition characterized by significant impairment in activity levels due to profound fatigue, worsening symptoms after seemingly minimal physical, or mental exertion, sleep problems, as well as difficulties with memory and concentration or orthostatic intolerance (1). Patients with ME/CFS also frequently experience chronic joint and muscle pain. Conditions with chronic pain as a major symptom, such as ME/CFS, endometriosis (EM), fibromyalgia, interstitial cystitis/bladder pain, irritable bowel syndrome, temporomandibular joint syndrome, and chronic migraines, have been termed chronic overlapping pain conditions. There is evidence that persons with one of these conditions are more likely to have another one as a co-morbidity…. We found more than a third of women with CFS reported endometriosis as a comorbid condition.”
(Boneva et al., 2019)
This comorbidity, as well as other chronic pain conditions (interstitial cystitis, irritable bowel syndrome, chronic headaches, chronic low back pain, vulvodynia, fibromyalgia, temporomandibular joint disease, and chronic fatigue syndrome) has been noted in adolescents as well (Smorgick et al., 2013).
References
Boneva, R. S., Lin, J. M. S., Wieser, F., Nater, U. M., Ditzen, B., Taylor, R. N., & Unger, E. R. (2019). Endometriosis as a comorbid condition in chronic fatigue syndrome (CFS): secondary analysis of data from a CFS case-control study. Frontiers in pediatrics, 7, 195. Retrieved from https://doi.org/10.3389/fped.2019.00195
Smorgick, N., Marsh, C. A., As-Sanie, S., Smith, Y. R., & Quint, E. H. (2013). Prevalence of pain syndromes, mood conditions, and asthma in adolescents and young women with endometriosis. Journal of pediatric and adolescent gynecology, 26(3), 171-175. Retrieved from https://www.sciencedirect.com/science/article/abs/pii/S1083318813000028

Endometriosis Fertility Treatment: Natural, Medical, & Surgical Options
Table of contents
Natural, Medical & Surgical Treatment of Endometriosis Infertility
Endometriosis (endo) is a common condition that affects up to 10% of all women globally. But most people do not realize this condition’s impact on a significant proportion of women. Endometriosis and pregnancy complications are a common coincidence. Up to 50% of women with infertility have endo.
Endometriosis and pregnancy can be problematic for patients. And sometimes, endometriosis treatments are needed to conceive. Keep reading to learn more about fertility options for women with endo.
Read More: How Does Endometriosis Cause Infertility?
Lack of Evidence-Based Research Stalls Treatment Options
Endometriosis is sometimes like the elephant in the room that no one wants to discuss or do enough research. However, that needs to change because endometriosis is often a disabling condition, and people should know about it. Not only does this condition impact the patient’s quality of life, but it also affects the potential for some of these patients to have a family. This situation can affect a marriage, other family members, a partner, etc.
Options for treating women with endometriosis and pregnancy issues can be natural, medical, surgical, or surgery-assisted. Let’s review the latest fertility treatments and courses of action for women affected by endometriosis. First, we will briefly discuss how endometriosis and pregnancy are related.
Can You Get Pregnant with Endometriosis?
Natural
Getting pregnant with endometriosis is not always easy, but it’s a reality for most patients who have the condition and want to conceive. It’s important to emphasize that the body can and still does get pregnant. There are things such as an endometriosis diet that might help. Let’s look at the good numbers. Up to 70%, according to some studies, of women with mild to moderate endometriosis will become pregnant without medical intervention.
Medically-Assisted
Statistics show that about 75% of women with severe endometriosis (stage III/IV) will conceive if they desire. Two-thirds of those pregnancies occurred naturally, and one-third with the help of the endometriosis fertility treatment.
If you have endometriosis and are having troubles getting or maintaining a pregnancy, and you wish to carry full-term, here are some medical options that may interest you:
- Freeze some eggs: Your ovarian reserve of eggs can decline due to endometriosis. Therefore, some endo specialists recommend preserving your eggs in case you wish to conceive later. Just note that this can be an expensive option.
- Superovulation and intrauterine insemination (SO-IUI): If you have normal fallopian tubes, mild endometriosis, and a partner with healthy sperm, this might be the best choice for you.
- Fertility medications: Doctors can prescribe medications to produce up to two or three mature eggs. There are also progestin injections that are often used to help fertility issues.
- Frequent ultrasounds: If a person is trying to get pregnant, they may go in for frequent ultrasounds to identify when the eggs are most mature. At that time, a doctor can insert the partner’s collected sperm.
- In-Vitro Fertilization (IVF): This treatment involves the extraction of the egg and sperm. The egg is fertilized outside the body and then implanted into the uterus.
Endometriosis Surgery For Infertility
Many women with endometriosis do become pregnant without medical assistance. However, studies suggest that endometriosis surgery does help a woman to become pregnant without difficulty.
- Removal of endometriosis tissue: Evidence shows that pregnancy rates improve if the endometriosis tissues are removed surgically.
- Removal of tissue or large endometriosis cysts: Large cysts and tissue accumulation can contribute to infertility. Removing these can help the patient conceive.
- Routine follow-up: Women with endometriosis often have cysts that relapse after treatment. It is crucial to complete follow-up visits and possibly have complementary surgeries down the road.
How Your Stage of Endometriosis Impacts Fertility
A diagnosis of endometriosis is a heavy thing to take in, primarily since it’s known to impact a woman’s reproductive organs. Studies have shown that the extent of endometriosis present during laparoscopy correlates with fertility.
Do You Have Concerns About Endometriosis and Fertility?
We want to hear from you. What is your biggest concern about the fertility impact of endometriosis? Or does it concern you at all? Leave your answers in the comments below. If you need medical attention that is not emergent, be sure to find a vetted endometriosis specialist who is familiar with the disease and modern treatments.

Killer cramps
What’s behind those killer cramps in endometriosis? A mixture of nociceptive, inflammatory, and neuropathic factors that combine to create pain and other symptoms. Endometriosis is more than killer cramps. The factors associated with inflammation and nerves, such as prostaglandins, can cause other symptoms as well (Koike et al., 1992). For example, prostaglandins, such as seen in endometriosis, can also contribute to pain associated with irritable bowel syndrome (Grabauskas et al., 2020). Or chronic inflammation can cause a reduction in energy on the cellular level leading to fatigue (Lacourt et al., 2018). Morotti et al. (2014) notes that “endometriosis-associated pain is as complex as the disease itself” and that “no correlation exists between the extent of endometriosis seen at laparoscopy and the degree of pain symptoms.” There have been several studies demonstrating an increase in sensory nerve fibers in endometriotic lesions as well as inflammatory factors that contribute to pain (Morotti et al., 2014).
Understanding and Finding Relief from Endometriosis Cramps
Find out more about pain and endometriosis here: https://icarebetter.com/what-influences-pain-levels/
References
Grabauskas, G., Wu, X., Gao, J., Li, J. Y., Turgeon, D. K., & Owyang, C. (2020). Prostaglandin E2, produced by mast cells in colon tissues from patients with irritable bowel syndrome, contributes to visceral hypersensitivity in mice. Gastroenterology, 158(8), 2195-2207. Retrieved from https://www.sciencedirect.com/science/article/pii/S0016508520302328
Koike, H., Egawa, H., Ohtsuka, T., Yamaguchi, M., Ikenoue, T., & Mori, N. (1992). Correlation between dysmenorrheic severity and prostaglandin production in women with endometriosis. Prostaglandins, leukotrienes and essential fatty acids, 46(2), 133-137. Retrieved from https://doi.org/10.1016/0952-3278(92)90219-9
Lacourt, T. E., Vichaya, E. G., Chiu, G. S., Dantzer, R., & Heijnen, C. J. (2018). The high costs of low-grade inflammation: persistent fatigue as a consequence of reduced cellular-energy availability and non-adaptive energy expenditure. Frontiers in behavioral neuroscience, 12, 78. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5932180/#:~:text=We%20propose%20that%20chronic%20low,rapid%20generation%20of%20cellular%20energy.
Morotti, M., Vincent, K., Brawn, J., Zondervan, K. T., & Becker, C. M. (2014). Peripheral changes in endometriosis-associated pain. Human reproduction update, 20(5), 717-736. Retrieved from https://academic.oup.com/humupd/article/20/5/717/2952641?login=true

Thankful for resources on endometriosis
It was Thanksgiving week in the USA- a time to take a moment to focus our attention on what we are grateful to have. While there is much to be learned about endometriosis and the best treatment, I am grateful for the researchers, healthcare providers, and advocates who are working to better the understanding and care of endometriosis. There are researchers out there trying to decipher the way endometriosis originates, functions, and affects people in order to lead to better treatment. There are healthcare professionals out there such as surgeons refining their skill in removing endometriosis as well as teaching others how to do so, therapists who help with the effects that endometriosis has on our bodies and minds, and advocates who are working to bring attention to this disease. There are too many to list them all but visit our Articles and Website links page as well as the links on Podcasts and Videos to see just a small sampling of those out there working to better endometriosis care.

Social gatherings and food choices
As we approach a season of many different holidays, our thoughts often turn to food. There is usually food at most any holiday gathering- which can be both a pleasure and a grief for those dealing with a chronic illness. Those with a history of endometriosis can often have gastrointestinal symptoms that are exacerbated by certain foods or patterns of eating. Those with endometriosis may also have other conditions with specific dietary guidelines (such as interstitial cystitis or migraines).
We have noted before that while there is no specific diet overall for endometriosis, nutrition can improve symptoms as well as overall health and well-being. Nutrition should be individualized to your specific needs. As we approach the holidays, you really have to know your body. For example, one person may tolerate gluten in small portions, while another cannot tolerate even an occasional cheat. Knowing your body and practicing mindful eating can lessen the stress and enable you to more fully enjoy gatherings. Because food is not only essential to our basic survival, it is often at the center of community gatherings and part of the pleasure of living.
Some preplanning to accommodate dietary choices can minimize the interference of enjoying social gatherings. It may be bringing a dish that you know you can eat, having a small meal beforehand so you won’t be as tempted to indulge in things that don’t agree with you, or having an artful dodge if someone comments on what you are or are not eating (or better yet- as Toby Amidor put it- “don’t be afraid to politely say, ‘no, thank you’ without giving a long explanation…you don’t owe an explanation to anyone — so don’t feel obligated”). Sometimes dietary choices can feel like a punishment- a series of avoiding things. Focus on what you CAN have and enjoy. From time to time we have to Jedi mind trick ourselves by knowing that we can eat whatever we want, but we are choosing something better for ourselves (because you are worth it!). And if you throw caution to the wind and indulge, then don’t beat yourself up over it. Next time you eat, you’ll eat something better for yourself. If you are still in the process of finding what food choices work best for your body, then here are a few things to consider:
Diet and Nutrition: https://icarebetter.com/diet-and/
Is There an Endo Diet?: https://icarebetter.com/fast-facts-is-there-an-endo-diet/
Curcumin: https://icarebetter.com/curcumins-effect-on-endometriosis/
Mediterranean and FODMAP: https://icarebetter.com/endo-diet-mediterranean-or-fodmap-for-the-win/
Celiac Disease and Endometriosis: https://icarebetter.com/celiac-disease-and-endometriosis/
Interstitial cystitis: https://www.ichelp.org/living-with-ic/interstitial-cystitis-and-diet/
Reference
Amidor, T. (2018). How to Navigate a Holiday Party With Dietary Restrictions. Retrieved from https://www.foodnetwork.com/healthyeats/holidays/2018/12/how-to-navigate-a-holiday-party-with-dietary-restrictions
Wait a minute- is that true?
We frequently get questions about information that is assumed to be true in most cases of endometriosis. When evaluating information about endometriosis, it is good to keep in mind that long accepted beliefs may not necessarily be absolute. Here are a few often touted beliefs about endometriosis and why they may not necessarily be accurate:
- “Hysterectomy is the definitive treatment for endometriosis.” Or variations of this theme: “Removing your uterus and/or ovaries will cure you”. Many people with endometriosis also experience problems with their uterus or ovaries (such as adenomyosis, fibroids, and other conditions that can contribute to chronic pelvic pain) that could benefit from a hysterectomy. However, using a hysterectomy to treat endometriosis alone may still leave you susceptible to continued symptoms and other problems from remaining lesions [one example: hydronephrosis from endometriosis left around ureters (Bawin, Troisfontaines, & Nisolle, 2013)].
- “Persistent or recurrent endometriosis after a total abdominal hysterectomy and bilateral salpingo-oophorectomy (TAH BSO) has been reported by several investigators.” (Hasty & Murphy, 1995)
- “According to literature, there are no randomized controlled trials for hysterectomy as the treatment for endometriosis.” (Bellelis, 2019)
- “Endometriosis which is not removed at the time of hysterectomy and bilateral salpingo‐oophorectomy may represent after a variable time interval with many or all of the symptoms which prompted the original surgery. This tissue can be highly active and responsive to exogenous hormonal stimulation. In the presence of troublesome symptoms, excision of residual endometriosis may be effective and should be considered.” (Clayton et al., 1999)
- “A high recurrence rate of 62% is reported in advanced stages of endometriosis in which the ovaries were conserved. Ovarian conservation carries a 6 fold risk of recurrent pain and 8 folds risk of reoperation. The decision has to be weighed taking into consideration the patient’s age and the impact of early menopause on her life style. The recurrence of endometriosis symptoms and pelvic pain are directly correlated to the surgical precision and removal of peritoneal and deeply infiltrated disease. Surgical effort should always aim to eradicate the endometriotic lesions completely to keep the risk of recurrence as low as possible.” (Rizk et al., 2014)
- “We found that among women undergoing hysterectomy, endometriosis was associated with a higher degree of prescription of analgesics. In the endometriosis group the prescription of analgesic, psychoactive and neuroactive drugs did not decrease significantly after surgery. In fact, the prescription of psychoactive and neuroactive drugs increased.” (Brunes et al., 2020)
- “Studies have showed that the growth and progression of endometriosis continue even in ovariectomized animals.” (Khan et al., 2013)
- Read more here: “Endometriosis persisting after hysterectomy and bilateral salpingo-oophorectomy: Removing the disease, not organs, is key to long-term relief”: http://endopaedia.info/treatment21.html
- “All of your endo will die off in menopause.” Whether natural, surgically induced, or medically induced, there are cases of endometriosis continuing after menopause. Endometriosis lesions are capable of producing their own estrogen (Huhtinen, Ståhle, Perheentupa, & Poutanen, 2012). Another spin off is that “you are too old to have endometriosis”. Inceboz (2015) reports cases of endometriosis in the 8th and 9th decade of life. While some people’s symptoms do improve, it is not a sure thing.
- “As an estrogen-dependent disease, endometriosis was thought to become less active or regress with the onset of the menopause. However, based on some new data, we are discovering that this pathology can emerge or reappear at this period of life.” (Marie-Scemama, Even, De La Joliniere, & Ayoubi, 2019)
- “Endometriotic lesions remained biologically active, with proliferative activity and preserved hormonal responsiveness, even in the lower estrogenic environment in the postmenopause.” (Inceboz, 2015)
- “True prevalence of postmenopausal endometriosis is unknown. There have been some reports in the literature on the prevalence of endometriosis in postmenopausal women [5–8]. According to these studies, the prevalence of postmenopausal endometriosis is 2–5%…. Interestingly, nine of the cases were at the upper extreme of the age groups (eight were in 80–85 years and a case in 90–95 years).” (Inceboz, 2015)
- “Occurrence or progression of postmenopausal endometriosis lesions could be related to extra-ovarian production of estrogen by endometriosis lesions and adipose tissue, which becomes the major estrogen-producing tissue after menopause. Postmenopausal women with symptomatic endometriosis should be managed surgically…” (Streuli, Gaitzsch, Wenger, & Petignat, 2017)
- “Getting pregnant will help.” However, endometriosis can cause infertility…..
- “Although gynaecologists often advise women that pregnancy has a beneficial effect on endometriosis, few studies confirm this association. Owing to the paucity and limited quality of the data, we can conclude that the behaviour of endometriotic lesions during pregnancy seems to be variable, ranging from complete disappearance to increased growth. Despite some of the early authors questioning a positive effect (McArthur and Ulfelder, 1965; Schenken et al., 1987), the idea to recommend pregnancy as part of the treatment strategy for endometriosis persists to this day (Rubegni et al., 2003; Coccia et al., 2012; Benaglia et al., 2013). The few favourable early observations and very limited options to treat endometriosis seem to have generated the myth of a beneficial effect of pregnancy and initiation of the so-called ‘pseudopregnancy’ therapy. Endometriosis is associated with infertility, and a lower prevalence of endometriosis in pregnant than in non-pregnant women may have led clinicians and scientists to the view that pregnancy has a positive effect against the disease.” (Leeners, Damaso, Ochsenbein-Kölble, & Farquhar, 2018)
- “Mild endometriosis won’t affect fertility.” So-called “mild” or “minimal” endometriosis can affect the ability to conceive (Carvalho et al., 2012). Also, “mild” or “minimal” endometriosis can still produce significant symptoms (see Pain with Minimal Endometriosis).
- “The purpose of this systematic review is to present studies regarding the association between pregnancy rates and the presence of early stages of endometriosis. Studies regarding infertility, minimal (stage I, American Society of Reproductive Medicine [ASRM]) and mild (stage II, ASRM) endometriosis were identified…Earlier stages of endometriosis play a critical role in infertility, and most likely negatively impact pregnancy outcomes.” (Carvalho, Below, Abrão, & Agarwal, 2012)
- “Hormonal suppressants will clean up the rest of the endometriosis.” Hormonal medications may be useful for other problems but cannot be relied upon to “clean up” or prevent recurrence of endometriosis. Surgeons who perform endometriosis surgery exclusively (excision) versus a general gynecological/obstetric practice have more chance to develop skill in being able to identify and being able to remove ALL endometriosis lesions (Khazali, 2020) (see Why Excision is Recommended).
- “Endometriotic stromal cells resist the antiproliferative effect of GnRH agonists and antagonists.” (Taniguchi et al., 2013)
- “This case demonstrates the obvious progression of deep rectal endometriosis despite 4 years of continuous hormonal therapy.” (Millochau et al., 2016)
- “Few studies of medical therapies for endometriosis report outcomes that are relevant to patients, and many women gain only limited or intermittent benefit from treatment.” (Becker et al., 2017)
- “There is currently no evidence to support any treatment being recommended to prevent the recurrence of endometriosis following conservative surgery.” (Sanghera et al., 2016)
- “A systematic review found that post-surgical hormonal treatment of endometriosis compared with surgery alone has no benefit for the outcomes of pain or pregnancy rates, but a significant improvement in disease recurrence in terms of decrease in rAFS score (mean = −2.30; 95% CI = −4.02 to −0.58) (Yap et al., 2004). Overall, however, it found that there is insufficient evidence to conclude that hormonal suppression in association with surgery for endometriosis is associated with a significant benefit with regard to any of the outcomes identified….Moreover, even if post-operation medication proves to be effective in reducing recurrence risk, it is questionable that ‘all’ patients would require such medication in order to reduce the risk of recurrence.” (Guo, 2009)
- “Many studies have investigated factors determining the recurrence of endometrioma and pain after surgery [16, 19, 20]…. Regardless of the mechanism, the present and previous studies suggest that postoperative medical treatment is known to delay but not completely prevent recurrence…. In our study, we also failed to observe a benefit for postoperative medication in preventing endometrioma and/or endometriosis-related pain recurrence.” (Li et al., 2019)
- “Furthermore, all currently approved drugs are suppressive and not curative. For example, creating a hormonal balance in patients by taking oral contraceptives, such as progestins and gonadotropin‐releasing hormone agonists, may only relieve the associated inflammatory status and pain symptoms.” (Che et al., 2015)
- “If I respond to hormonal therapy then that means I have endometriosis.” Response to hormonal treatment, whether positive or negative, does NOT diagnose endometriosis or exclude it.
- “Relief of chronic pelvic pain symptoms, or lack of response, with preoperative hormonal therapy is not an accurate predictor of presence or absence of histologically confirmed endometriosis at laparoscopy.” (Jenkins, Liu, & White, 2008)
- “The definitive diagnosis of endometriosis can only be made by histopathology showing endometrial glands and stroma with varying degree of inflammation and fibrosis.” (Rafique & Decherney, 2017)
- “My scans didn’t show anything so I was told I didn’t have endometriosis.” Transvaginal ultrasounds and magnetic resonance imaging are becoming more sensitive in the hands of those with experience and can rule in instances of endometriosis (especially deep infiltrating endometriosis and endometriomas). However, it cannot rule out endometriosis. (See But All Your Tests Are Negative)
- “Currently, there are no non‐invasive tests available in clinical practice to accurately diagnose endometriosis…. Laparoscopy remains the gold standard for the diagnosis of endometriosis and using any non‐invasive tests should only be undertaken in a research setting.” (Nisenblat et al., 2016)
- “Ultrasonography and magnetic resonance imaging can be used to diagnose ovarian endometriotic cysts and deep infiltrating endometriosis; but their performance is poor in the diagnosis of initial stages of endometriosis.” (Ferrero, 2019)
- “None of my tests showed I had endometriosis.” Other tests, in addition to scans, cannot adequately rule out endometriosis with consistency or certainty.
- “Currently, there are no non‐invasive tests available in clinical practice to accurately diagnose endometriosis…. Laparoscopy remains the gold standard for the diagnosis of endometriosis and using any non‐invasive tests should only be undertaken in a research setting.” (Nisenblat et al., 2016)
- “CA‐125 and other serum markers (such as CA 19‐9, serum protein PP14, interleukins, and angiogenetic factors) have been measured in women with endometriosis but they are not reliable for the diagnosis of the disease.” (Ferrero, 2019)
- “The majority of studies focused on a panel of biomarkers, rather than a single biomarker and were unable to identify a single biomolecule or a panel of biomarkers with sufficient specificity and sensitivity in endometriosis. Conclusion: Noninvasive biomarkers, proteomics, genomics, and miRNA microarray may aid the diagnosis, but further research on larger datasets along with a better understanding of the pathophysiologic mechanisms are needed.” (Anastasiu et al., 2020)
- “I was told it was IBS.”
- “Endometriosis can be commonly misdiagnosed as IBS [22] due to overlap in common symptoms and perhaps mechanisms of disease progression involving aberrant activation of inflammatory cascades.” (Torres-Reverón, Rivera-Lopez, Flores, & Appleyard, 2018)
- “You are too young to have endometriosis.” Or “you are too young to have adenomyosis or DIE.” In those adolescents with chronic pelvic pain, endometriosis is a common discovery. Deep infiltrating endometriosis (DIE) can be found in teens.
- “Endometriosis is a common finding in adolescents who have a history of chronic pelvic pain or dysmenorrhoea resistant to medical treatment, however the exact prevalence is unknown. Both early/superficial and advanced forms of endometriosis are found in adolescents, including ovarian endometriomas and deep endometriotic lesions. Whilst spontaneous resolution is possible, recent reports suggest that adolescent endometriosis can be a progressive condition, at least in a significant proportion of cases. It is also claimed that deep endometriosis has its roots in adolescence.” (Sarıdoğan, 2017)
- “The majority of adolescent girls with chronic pelvic pain not responding to conventional medical therapy have endometriosis (up to 80%). Laparoscopy with biopsy is the only way to diagnose endometriosis in the adolescent population, and depends on recognition of atypical manifestations of the disease.” (Yeung Jr, Gupta, & Gieg, 2017)
- “Adolescent endometriosis is not a rare condition.” (Audebert et al., 2015)
- “An increasing body of literature suggests that advanced-stage endometriosis (revised scoring system of the American Society for Reproductive Medicine Stage III or IV) and deeply invasive endometriosis are relatively common in adolescents.” (Dowlut-McElroy & Strickland, 2017)
- “In all, 648 of 1011 (64%) adolescents undergoing laparoscopy were found to have endometriosis. The prevalence ranged from 25% to 100%, with a mean prevalence of 64%. Thirteen studies including 381 participants categorized disease severity using the revised American Society of Reproductive Medicine classification. Among these, 53% of participants (201/381) had stage I, 28% (105/381) had stage II, 20% (76/381) had stage III, and 13% (49/381) had stage IV disease. Conclusions: The prevalence of endometriosis among adolescents with pelvic pain symptoms is high. Endometriosis is treatable, and prompt recognition will help to ensure that adolescents are signposted earlier to appropriate specialists. The management of adolescents with suspected endometriosis should be consistent with best practice guidance. Despite recommendations to increase the awareness and knowledge of endometriosis in adolescence, minimal research has followed.” (Hirsch et al., 2020)
- “My endo keeps coming back so there’s nothing I can do.” It can be difficult to ascertain if endometriosis truly reappeared or was all of it not removed previously (See Is There Microscopic or Occult Endometriosis). With repetitive surgeries or with endometriosis in certain locations (such as ureters, bowel, diaphragm, etc.), seeking someone who exclusively does surgery for endometriosis and its related conditions can be beneficial (Khazali, 2020). Often a team approach, utilizing other specialties as dictated by the individual’s case, is valuable (Khazali, 2020). (See Why Excision is Recommended) Recurrence can happen, more often in ovarian endometriosis, stage III and IV, and in those who were younger (Selçuk & Bozdağ, 2013). When looking at recurrence rates, it ranges from 6% to 67% (Selçuk & Bozdağ, 2013)! This wide range is due to many factors when evaluating studies- most studies do not differentiate the type of surgery, the type of surgeon (specialty center versus general gynecological practice), or the criteria for recurrence (was it reemergence of symptoms or repeat surgery) (Selçuk & Bozdağ, 2013). There are many related conditions that appear with endometriosis that can cause similar symptoms that should also be addressed (See Related Conditions).
- “A multidisciplinary team approach (eg, gynecologic endoscopist, colorectal surgeon, urologist) can reduce risk and facilitate effective treatment.19 Likewise, advanced surgical skills and anatomical knowledge are required for deep resection and should be performed primarily in tertiary referral centers. Careful preoperative planning, informed consent, and meticulous adherence to “best practice” technique is requisite to reduce morbidity and ensure effective management of potential complications.90Although excisional biopsy and resection offers a higher success rate in treating the disease, surgical excision also requires a higher level of surgical skill. As a result, many patients receive incomplete treatment, which in turn may lead to persistent symptoms and recurrent disease. It should be noted that many women who have undergone repeated surgeries and had a hysterectomy still suffer.86 The need to improve surgical approach and/or engage in timely referrals is unquestionable. Surgery to debulk and excise endometriosis may be “more difficult than for cancer”. Complete removal of implants may be difficult due to variation in appearance and visibility. True surgical resection and treatment poses formidable challenges, even the hands of experienced clinicians. In particular, deep disease is often difficult to treat due to close proximity of and common infiltration in and around bowel, ureters, and uterine artery.18 Potential adenomyosis should also be included in the preoperative workup, as it can influence postoperative improvement patterns of pain and symptoms associated with endometriosis.” (Fishcer et al., 2013)
- “All of the studies were conducted by expert laparoscopic surgeons, whose results are unlikely to be reproduced by the generalist surgeon…. Based on the studies performed to date, it is the author’s opinion that laparoscopic excision of endometriosis, when technically feasible, should be the standard of care. First, whereas visual diagnosis of endometriosis is correct in only 57% to 72% of cases, excisional surgery yields specimens for histologic confirmation—and identifies endometriosis in 25% of “atypical” pelvic lesions as well.18 The availability of such specimens would prevent unnecessary treatment and ensure more reproducible research findings. Excision should also reduce the incidence of persistent disease secondary to inadequate “tip of the iceberg” destruction, removing both invasive and microscopic endometriosis to provide the best possible symptom relief.” (Jenkins, 2009)
- “Laparoscopic identification of superficial endometriosis implants represents a challenge for the gynecologic surgeon. Endometriosis lesions may present in a wide spectrum of appearance according to a “lifecycle” of the implants. The lesions can be flat or vesicular. They can have any combination of color typically red, back/brown and white. Active “red” lesions, large endometriomas, deep infiltrating nodules, and typical “powder-burn” lesions are easier to identify than “white” old fibrotic lesions. The endometriotic implants are hypervascular. The diagnostic accuracy at laparoscopy is also affected by the experience of the surgeon and the laparoscopic equipment [16].” (Jose, Fausto, & Antonio, 2018)
- “It’s all in your head.” When no visible cause is identified or usual treatments fail, the blame often gets shifted to the individual- that they are exaggerating or are not strong enough to deal with it or that they should be able to just live it. Sadly, one study (Rowe & Quinlivan, 2020) found that often a women’s fertility rather than quality of life was the driver for getting further care.
- “Women’s symptoms are frequently trivialized or disbelieved, consequently attributing pathology to the woman rather than the disease, which is deeply distressing [11]. These responses are underpinned by essentialist notions that pain is just part of being a woman. Lack of legitimation results in victim blaming, reinforces gendered stereotypes about feminine weakness, intensifies women’s distress and averts prompt action [10]. Similar essentialist ideas underlie observations that framing endometriosis as a fertility problem is more likely to result in health care intervention than when it is framed as symptom management. In one qualitative study, women described fertility as the entry point for discussion about endometriosis, despite having sought health care for symptoms over many years [12].” (Rowe & Quinlivan, 2020)
- “Endometriosis impairs the quality of life due to chronic and severe acyclic pelvic pain with associated dysmenorrhea, dyspareunia, gastrointestinal problems, fatigue and headaches….women with endometriosis are often surrounded by taboos, myths, scourge of subfertility, pain of disease and missed diagnosis and treatment [22]. Delays in the diagnosis and initiation of treatment for the disease in fact occur due to these counterproductive factors operative both at the individual patient level and at the medical level resulting in frustration and loss of valuable time in the prime phase of life of the patient….Delays also occur at the medical level due to the delay in referral from primary to secondary care, pain normalized by clinicians, intermittent hormonal suppression of symptoms, use of non-discriminating investigations and insufficiency in awareness and lack of constructive support among a subset of healthcare providers [23,24,25,37,38]. In this connection, it is noteworthy that delay in diagnosis is longer for women reporting with pelvic pain compared with those reporting with infertility, which is suggestive of the fact that there is a higher level of reluctance surrounding endometriosis-associated pain symptoms….” (Ghosh et al., 2020)
- “Women had to ‘battle’ for an accurate diagnosis, and had limited faith in health professionals…. Conclusions: Implications for health professionals are discussed, including the need for earlier diagnosis and taking women’s symptoms more seriously at referral…” (Grogan, Turley, & Cole, 2018)
- “Despite its high prevalence and cost, endometriosis remains underfunded and underresearched, greatly limiting our understanding of the disease and slowing much-needed innovation in diagnostic and treatment options. Due in part to the societal normalization of women’s pain and stigma around menstrual issues…” (As-Sanie et al., 2019)
References
Anastasiu, C. V., Moga, M. A., Elena Neculau, A., Bălan, A., Scârneciu, I., Dragomir, R. M., … & Chicea, L. M. (2020). Biomarkers for the Noninvasive Diagnosis of Endometriosis: State of the Art and Future Perspectives. International Journal of Molecular Sciences, 21(5), 1750. Retrieved from https://www.mdpi.com/1422-0067/21/5/1750
As-Sanie, S., Black, R., Giudice, L. C., Valbrun, T. G., Gupta, J., Jones, B., … & Taylor, R. N. (2019). Assessing research gaps and unmet needs in endometriosis. American Journal of Obstetrics and Gynecology, 221(2), 86-94. Retrieved from https://www.sciencedirect.com/science/article/abs/pii/S0002937819303850
Audebert, A., Lecointre, L., Afors, K., Koch, A., Wattiez, A., & Akladios, C. (2015). Adolescent endometriosis: report of a series of 55 cases with a focus on clinical presentation and long-term issues. Journal of minimally invasive gynecology, 22(5), 834-840. Retrieved from https://pubmed.ncbi.nlm.nih.gov/25850071/
Bawin, I., Troisfontaines, E., & Nisolle, M. (2013). Clinical case of the month. Rare case of ureteral endometriosis nine years after hysterectomy. Revue medicale de Liege, 68(7-8), 378-381. Retrieved from https://europepmc.org/article/med/24053093
Becker, C. M., Gattrell, W. T., Gude, K., & Singh, S. S. (2017). Reevaluating response and failure of medical treatment of endometriosis: a systematic review. Fertility and sterility, 108(1), 125-136. Retrieved from https://www.sciencedirect.com/science/article/abs/pii/S0015028217303606
Bellelis, P. (2019). 2607 Hysterectomy in Women with Endometriosis. Journal of Minimally Invasive Gynecology, 26(7), S177. Retrieved from https://www.sciencedirect.com/science/article/pii/S1553465019307393
Brunes, M., Altman, D., Pålsson, M., Söderberg, M. W., & Ek, M. (2020). Impact of hysterectomy on analgesic, psychoactive and neuroactive drug use in women with endometriosis: Nationwide cohort study. BJOG: An International Journal of Obstetrics & Gynaecology. Retreived from https://obgyn.onlinelibrary.wiley.com/doi/full/10.1111/1471-0528.16469
Carvalho, L. F. P., Below, A., Abrão, M. S., & Agarwal, A. (2012). Minimal and mild endometriosis negatively impact on pregnancy outcome. Revista da Associação Médica Brasileira, 58(5), 607-614. Retrieved from https://www.sciencedirect.com/science/article/pii/S0104423012702579
Che, X. H., Chen, Y. C., Chen, C. L., Ye, X. L., & Zhu, H. (2015). Non‐hormonal targets underlying endometriosis: A focus on molecular mechanisms. Molecular Reproduction and Development, 82(6), 410-431. Retrieved from https://onlinelibrary.wiley.com/doi/full/10.1002/mrd.22493
Clayton, R. D., Hawe, J. A., Love, J. C., Wilkinson, N., & Garry, R. (1999). Recurrent pain after hysterectomy and bilateral salpingo‐oophorectomy for endometriosis: evaluation of laparoscopic excision of residual endometriosis. BJOG: An International Journal of Obstetrics & Gynaecology, 106(7), 740-744. Retrieved from https://obgyn.onlinelibrary.wiley.com/doi/full/10.1111/j.1471-0528.1999.tb08377.x?fbclid=IwAR04aFoLsukqsYutNPNXtJNZpKLNEJbgOOon334NW8D7wvwzZMWaS2YaZts
Dowlut-McElroy, T., & Strickland, J. L. (2017). Endometriosis in adolescents. Current Opinion in Obstetrics and Gynecology, 29(5), 306-309. Retrieved from https://journals.lww.com/co-obgyn/Abstract/2017/10000/Endometriosis_in_adolescents.6.aspx
Ferrero, S. (2019). Proteomics in the diagnosis of endometriosis: opportunities and challenges. PROTEOMICS–Clinical Applications, 13(3), 1800183. Retrieved from https://onlinelibrary.wiley.com/doi/abs/10.1002/prca.201800183
Fischer, J., Giudice, L. C., Milad, M., Mosbrucker, C., & Sinervo, K. R. (2013). Diagnosis & management of endometriosis: pathophysiology to practice. APGO Educational Series on Women’s Health Issues. Retrieved from https://www.ed.ac.uk/files/atoms/files/diagnosis_and_management_of_endometriosis_booklet.pdf
Ghosh, D., Filaretova, L., Bharti, J., Roy, K. K., Sharma, J. B., & Sengupta, J. (2020). Pathophysiological Basis of Endometriosis-Linked Stress Associated with Pain and Infertility: A Conceptual Review. Reproductive Medicine, 1(1), 32-61. Retrieved from https://www.mdpi.com/2673-3897/1/1/4/htm
Grogan, S., Turley, E., & Cole, J. (2018). ‘So many women suffer in silence’: a thematic analysis of women’s written accounts of coping with endometriosis. Psychology & health, 33(11), 1364-1378. Retrieved from https://www.tandfonline.com/doi/abs/10.1080/08870446.2018.1496252
Guo, S. W. (2009). Recurrence of endometriosis and its control. Human reproduction update, 15(4), 441-461. Retrieved from http://humupd.oxfordjournals.org/content/15/4/441.full
Hasty, L. A., & Murphy, A. A. (1995). Management of recurrent endometriosis after hysterectomy and bilateral salpingo-oophorectomy. In Endometriosis (pp. 189-192). Springer, New York, NY. Retrieved from https://link.springer.com/chapter/10.1007/978-1-4613-8404-5_18
Hirsch, M., Dhillon-Smith, R., Cutner, A., Yap, M., & Creighton, S. M. (2020). The prevalence of endometriosis in adolescents with pelvic pain: a systematic review. Journal of Pediatric and Adolescent Gynecology. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32736134/
Huhtinen, K., Ståhle, M., Perheentupa, A., & Poutanen, M. (2012). Estrogen biosynthesis and signaling in endometriosis. Molecular and cellular endocrinology, 358(2), 146-154. Retrieved from https://www.sciencedirect.com/science/article/abs/pii/S0303720711005041
Inceboz, U. (2015). Endometriosis after menopause. Women’s Health, 11(5), 711-715. Retreived from https://journals.sagepub.com/doi/full/10.2217/whe.15.59
Jenkins, T. (2009). Endometriosis: The case for surgical excision. The Cutting Edge. Vol. 34, 19-23. Retrieved from https://www.yumpu.com/en/document/read/37376957/endometriosis-the-case-for-surgical-excision-skin-allergy-news
Jenkins, T. R., Liu, C. Y., & White, J. (2008). Does response to hormonal therapy predict presence or absence of endometriosis?. Journal of minimally invasive gynecology, 15(1), 82-86. Retrieved from https://pubmed.ncbi.nlm.nih.gov/18262150/
Jose, C., Fausto, A., & Antonio, L. (2018). Laparoscopic Enhanced Imaging Modalities for the Identification of Endometriosis Implants a Review of the Current Status. MOJ Womens Health, 7(1), 00160. Retrieved from https://www.researchgate.net/profile/Jose_Carugno/publication/323777470_Laparoscopic_Enhanced_Imaging_Modalities_for_the_Identification_of_Endometriosis_Implants_a_Review_of_the_Current_Status/links/5b54617345851507a7bcd5c3/Laparoscopic-Enhanced-Imaging-Modalities-for-the-Identification-of-Endometriosis-Implants-a-Review-of-the-Current-Status.pdf
Khan, K. N., Kitajima, M., Fujishita, A., Nakashima, M., & Masuzaki, H. (2013). Toll‐like receptor system and endometriosis. Journal of Obstetrics and Gynaecology Research, 39(8), 1281-1292. Retrieved from https://obgyn.onlinelibrary.wiley.com/doi/full/10.1111/jog.12117
Leeners, B., Damaso, F., Ochsenbein-Kölble, N., & Farquhar, C. (2018). The effect of pregnancy on endometriosis—facts or fiction?. Human reproduction update, 24(3), 290-299. Retrieved from https://academic.oup.com/humupd/article/24/3/290/4859612
Li, X. Y., Chao, X. P., Leng, J. H., Zhang, W., Zhang, J. J., Dai, Y., … & Wu, Y. S. (2019). Risk factors for postoperative recurrence of ovarian endometriosis: long-term follow-up of 358 women. Journal of Ovarian Research, 12(1), 79. Retrieved from https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-019-0552-y
Marie-Scemama, L., Even, M., De La Joliniere, J. B., & Ayoubi, J. M. (2019). Endometriosis and the menopause: Why the question merits our full attention. Hormone Molecular Biology and Clinical Investigation, 37(2). Retrieved from https://www.degruyter.com/view/journals/hmbci/37/2/article-20180071.xml
Millochau, J. C., Abo, C., Darwish, B., Huet, E., Dietrich, G., & Roman, H. (2016). Continuous amenorrhea may be insufficient to stop the progression of colorectal endometriosis. Journal of minimally invasive gynecology, 23(5), 839-842. Retrieved from https://www.sciencedirect.com/science/article/pii/S1553465016300474
Nisenblat, V., Prentice, L., Bossuyt, P. M., Farquhar, C., Hull, M. L., & Johnson, N. (2016). Combination of the non‐invasive tests for the diagnosis of endometriosis. Cochrane Database of Systematic Reviews, (7). Retrieved from https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD012281/full
Rafique, S., & Decherney, A. H. (2017). Medical management of endometriosis. Clinical obstetrics and gynecology, 60(3), 485. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5794019/
Rizk, B., Fischer, A. S., Lotfy, H. A., Turki, R., Zahed, H. A., Malik, R., … & Herrera, D. (2014). Recurrence of endometriosis after hysterectomy. Facts, views & vision in ObGyn, 6(4), 219. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4286861/
Rowe, H., & Quinlivan, J. (2020). Let’s not forget endometriosis and infertility amid the covid-19 crisis. Retrieved from https://www.tandfonline.com/doi/full/10.1080/0167482X.2020.1757200
Sanghera, S., Barton, P., Bhattacharya, S., Horne, A. W., & Roberts, T. E. (2016). Pharmaceutical treatments to prevent recurrence of endometriosis following surgery: a model-based economic evaluation. BMJ open, 6(4), e010580. Retrieved from http://bmjopen.bmj.com/content/6/4/e010580.long
Sarıdoğan, E. (2017). Adolescent endometriosis. European Journal of Obstetrics & Gynecology and Reproductive Biology, 209, 46-49. Retrieved from https://www.sciencedirect.com/science/article/abs/pii/S0301211516302330
Streuli, I., Gaitzsch, H., Wenger, J. M., & Petignat, P. (2017). Endometriosis after menopause: physiopathology and management of an uncommon condition. Climacteric, 20(2), 138-143. Retrieved from https://www.tandfonline.com/doi/abs/10.1080/13697137.2017.1284781
Taniguchi, F., Higaki, H., Azuma, Y., Deura, I., Iwabe, T., Harada, T., & Terakawa, N. (2013). Gonadotropin-releasing hormone analogues reduce the proliferation of endometrial stromal cells but not endometriotic cells. Gynecologic and obstetric investigation, 75(1), 9-15. Retrieved from https://www.karger.com/Article/Abstract/343748
Torres-Reverón, A., Rivera-Lopez, L. L., Flores, I., & Appleyard, C. B. (2018). Antagonizing the corticotropin releasing hormone receptor 1 with antalarmin reduces the progression of endometriosis. PLoS One, 13(11), e0197698. Retrieved from https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0197698
Yeung Jr, P., Gupta, S., & Gieg, S. (2017). Endometriosis in adolescents: a systematic review. Journal of Endometriosis and Pelvic Pain Disorders, 9(1), 17-29. Retrieved from https://journals.sagepub.com/doi/abs/10.5301/je.5000264

Endometriosis and Fertility: Statistics, Facts, & Fiction
Table of contents
Debunking the Myths Surrounding Endometriosis and Reproduction
Disinformation about endometriosis and how it can impact reproduction is thick. As a matter of fact, not just endometriosis and fertility, the entire disorder is shrouded in junk information, and so it often goes misunderstood and mistreated. To learn more on this topic, read our previous article, titled: “Endometriosis Facts and Myths: Dispelling the Misconceptions.”
Does endometriosis cause infertility? In some cases, yes. However, in most cases, women with endometriosis can and do get pregnant without any medical assistance or intervention of any kind. There is still a myth that if you become pregnant, that can manage the endometriosis (endo) symptoms and even help resolve disease progression.
This statement couldn’t be further from the truth, and it’s an example of a widespread myth about endometriosis and fertility. Furthermore, this school of thought can put additional pressure on women with endometriosis to get pregnant as quickly as possible once they get a diagnosis. As you can imagine, this dangerous misinformation can alter their expectations in terms of treatment for fertility and their outlook on endometriosis in general.
So, Can You Get Pregnant If You Have Endometriosis?
The real truth is that the connection between endometriosis and reproduction is complex. Can you get pregnant if you have endometriosis? Yes, many people can and do. However, having the right endometriosis specialist to help you along the way can make all the difference in your journey. Click here to learn more about finding vetted endo specialists near you. In this article, we will review the disease and lay out the facts regarding endometriosis and fertility.
What is Endometriosis?
Endometriosis is an inflammatory disorder in which tissue similar to the uterus lining grows in places outside the uterus. Often these growths happen on the surface of the uterus, ovaries, fallopian tubes, or other organs within the pelvic cavity – such as the bladder or bowel. In some cases, these endometriosis growths have occurred in distant organs.
Endo growths can cause pain, scarring, and sometimes infertility. Because this tissue is similar to the uterine lining, it also bleeds and sheds once a month during hormonal changes. Typically in the uterus, this period tissue and blood have a means of escaping through the vagina. However, this blood and tissue often accumulate inside the body with endometriosis and causes inflammation and pain. As one can imagine, over time, scar tissue growths with subsequent menstrual cycles develop. Eventually, this scar tissue can fuse organs, immobilize organs, and even damage the fallopian tubes.
Alarming Statistics About Endometriosis & Fertility
- Endometriosis is widespread, affecting between six and ten percent of the general female population. That’s more than 170 million worldwide.
- In patients with pelvic pain, infertility, or both, endometriosis frequency is higher – between 35 percent to 50 percent.
- Between 25 percent to 50 percent of infertile women have endometriosis.
- Between 30 percent to 50 percent of women with endometriosis are infertile.
- Endometriosis affects approximately the same number of women around the world that have diabetes.
- The cost of endometriosis in the US is between $86 Bn – $116 Bn.
- It takes, on average, eight years from the onset of symptoms for a patient to get a diagnosis. This can impact all patients, but especially those of who wish to keep their fertility intact.
Endometriosis Facts About Fertility and Reproduction
- There are ways to get pregnant with endometriosis.
- Hormonal therapy does not cure endo.
- Endometriosis is related to your menstrual cycle and hormonal changes within your body.
- Endometriosis tissue can be removed during laparoscopy. Depending on the location of the growths and the extent of damage, this can sometimes restore fertility.
- There is a type of endometriosis that can cause cancerous lesions, typically dark chocolate brown.
- The causes are uncertain, and there is no “cure” for endometriosis.
- Genes seem to play a role in the occurrence of endo.
Myths About Endometriosis and Fertility
- Pregnancy is not a cure or a way to relieve symptoms of endometriosis. Women should not be pressured or encouraged to get pregnant to help with endometriosis and fertility or alleviate pain or other symptoms. While some women experience less endo pain and symptoms during their period, that does not mean it works the same for all women.
- Do not believe any physician that tells you a hysterectomy is the “gold standard” treatment for endometriosis. As mentioned above, there is no “cure” for endometriosis. Until a specialist is inside the body and can view the number and the placement of the endometriosis lesions, they cannot decide whether a hysterectomy would even solve the problems. Also, some women might make themselves infertile (whether they mind or not, it is an emotional part of this disorder) by having a hysterectomy done that was never needed.
- You do not need to have a major medical procedure to get an endometriosis diagnosis or remove some growths and lesions. With modern equipment, skilled specialists, and advanced technology (often robotic surgical equipment), you can have endometriosis diagnosis and treatment with laparoscopy. This type of procedure is minimally invasive and only leaves behind a few puncture wounds.
- Abortion does not cause endometriosis.
- Endometriosis does not cause ovarian cancer. Although a type of endo involves cancerous tumors, this does not mean that having endometriosis makes you more likely to develop cancer.
- The most important myth to bust is that there is no treatment for endometriosis. Just because there is no “cure” for this pelvic inflammatory disorder does not mean there are no treatment options, even when it comes to endometriosis and infertility.
If you have endometriosis, what is the most common thing you have heard regarding endo and reproduction?
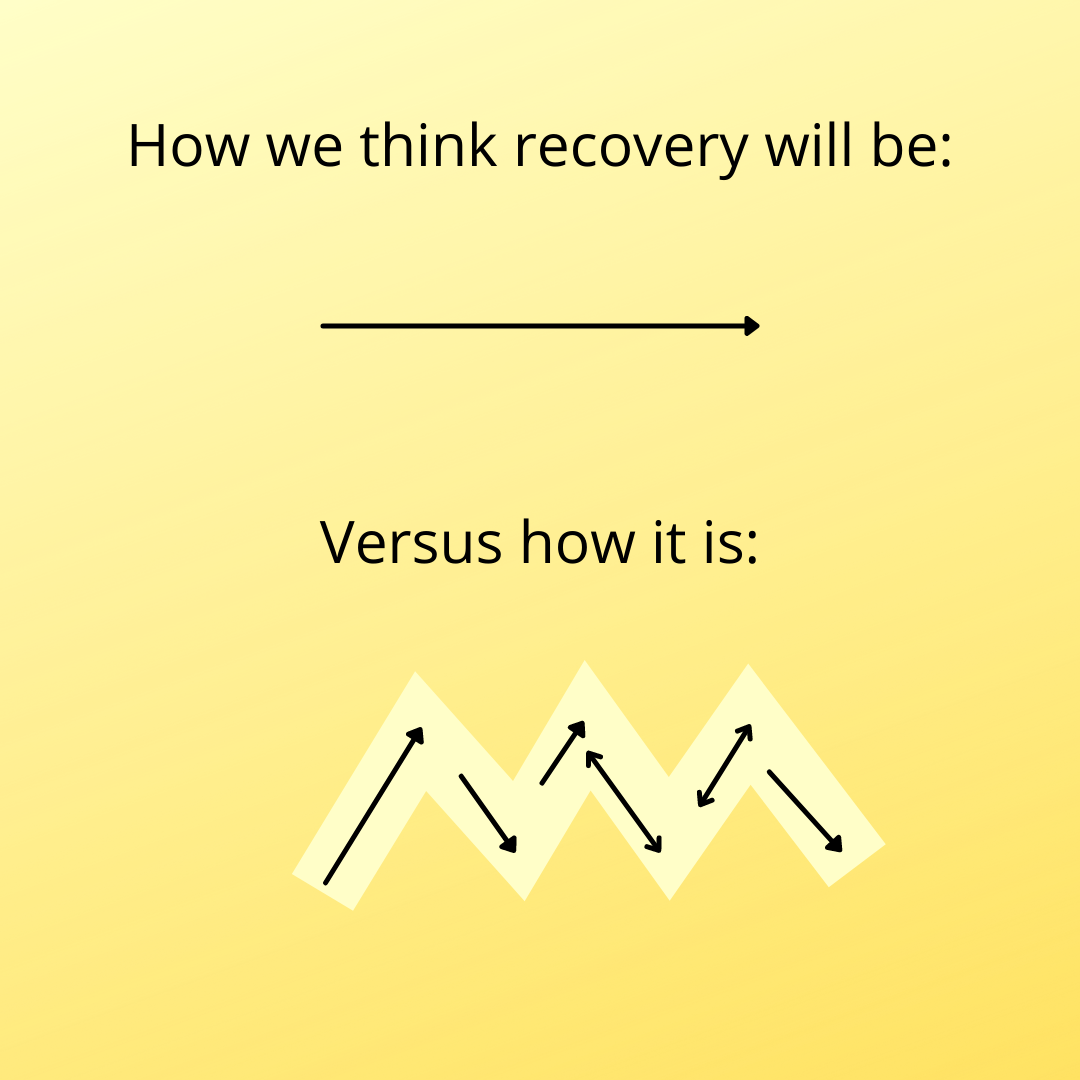
Recovery- not always smooth sailing
We often get questions about how long will it take to recover from surgery and how long does it take to know if it was successful. The aggravating answer is….it depends. There are many different things that play a part of surgery and recovery.
Recovery will be different for everyone. Everyone has their own innate healing (how quickly you heal, how you react to anesthesia and medications, adhesions, how healthy you were beforehand, etc.). Every surgery is different (what was done during surgery, how long was the surgery). Everyone might have other factors to their symptoms that will need to be addressed as well (such as pelvic floor dysfunction). While the incision on the outside may be small, there may be extensive work on the inside that is healing. Some people may notice a difference as soon as waking up from surgery. For others it may be weeks before they can tell a difference.
The success of the surgery can depend on multiple factors as well. One factor is what was your main goal? Some may have a goal of reduced pain while others may be more focused on fertility. With complete excision, there is the less likelihood of recurrence, but some people have ovarian endometriomas that have a higher recurrence rate if they are trying to preserve their ovaries. Some people may have other factors that are contributing symptoms, such as adenomyosis or interstitial cystitis. Sometimes we hear these wonderful stories of people waking up from surgery and feeling so much better, but that is not the case for everyone- but it doesn’t mean your surgery isn’t successful. Susan Pierce-Richards shares her thoughts on managing pre and post op expectations as someone who has been there: https://icarebetter.com/managing-expectations-pre-op-and-post-op/
For more information about healing after surgery, see: https://icarebetter.com/what-to-expect-in-the-weeks-after-skilled-excision-surgery/
*Remember to follow your surgeon’s instructions and call that surgeon if you have any questions or concerns!


Does Endometriosis Cause Infertility? Covering the Basics
Table of contents
- Learn More About the Connections Between Endometriosis and Infertilit y
- What is Endometriosis
- Endometriosis and Fertility: Exploring the Connection
- What Happens When Endometriosis Does Cause Infertility?
- Other Data on Endometriosis and Reproduction
- Diagnosing Endometriosis: A Multifaceted Approach
- Managing Endometriosis: A Multidisciplinary Approach
- Dietary and Lifestyle Considerations
- Endometriosis and Pregnancy: Potential Complications
- Mental Well-Being and Psychological Impact of Fertility Treatment for Endo Patients
- Endometriosis and Fertility: Navigating the Journey
Learn More About the Connections Between Endometriosis and Infertility
An endometriosis (endo) diagnosis can be a frightening thing. Very frightening. While this inflammatory condition can be binary or non-binary, women of childbearing age are prone to issues with reproduction due to endo. So does endometriosis cause infertility? Keep reading as I break down the basics of this topic. In this comprehensive guide, I will delve into the complex interplay between endometriosis and fertility, exploring the condition’s impact, treatment options, and strategies to overcome potential obstacles on the journey to parenthood. I will also discuss the emotional impact of this condition on patients.
What is Endometriosis
Endometriosis is a chronic inflammatory condition. In this disease, endometrial-like lesions implant on tissues and organs throughout the abdomen and pelvis, even elsewhere in the body! These lesions contain glands and stroma, similar to the endometrium (the tissue that lines the uterine walls), causing chronic inflammatory reactions.
Endometriosis lesions produce many substances and even make their own estrogen, which, as a result, causes a variety of issues locally and systemically. Pain is one of the most common symptoms, though silent endo exists as well. Please continue reading this article to learn more about endometriosis.
Endometriosis and Fertility: Exploring the Connection
While endometriosis does not automatically equate to infertility, there is a well-documented association between the two. Approximately 30% to 50% of individuals with endometriosis experience fertility challenges, though the reasons behind this link are not fully understood. Several potential mechanisms have been proposed:
- Anatomical Distortions: Endometriosis can cause physical distortions in the reproductive anatomy, leading to scarring, adhesions, and obstructions in the fallopian tubes or ovaries, hindering the fertilization process.
- Inflammatory Response: The lesions can trigger an inflammatory response, creating an inhospitable environment for fertilization and implantation.
- Hormonal Imbalances: Endometriosis may disrupt the delicate hormonal balance required for ovulation and implantation, potentially impacting fertility.
- Egg Quality: Some research suggests that endometriosis may adversely affect egg quality, further complicating the conception process.
Despite these potential challenges, it’s important to note that more than 70% of individuals with mild to moderate endometriosis can conceive naturally, offering hope for those seeking to start a family.
What Happens When Endometriosis Does Cause Infertility?
It can. 25 to 50% of women with infertility have endometriosis, and 30 to 50% of women with endometriosis have infertility. However, it is very encouraging to know that most women with endometriosis can become pregnant.
This statistic is significant. Many younger women with this disorder feel psychological effects due to the possibility of not being able to have kids. Not all patients carry this sentiment. Growing numbers of people do not want to have children. However, for those who do, these thoughts and emotions about fertility can be devastating. Then, endometriosis patients who do conceive often worry about the pregnancy and subsequent delivery of the baby.
Other Data on Endometriosis and Reproduction
Studies have also demonstrated that the enzyme aromatase may also play a role in endometriosis and infertility. There is an abnormally high level of this enzyme in the endometrium and endometriosis lesions in patients with endometriosis. In the uterus, this enzyme may affect both natural endometrial development and its receptivity for the implantation of the fetus.
Progesterone is another hormone that may play a role in implantation failure. Resistance to this enzyme can affect reproduction, as it is necessary for a normal pregnancy. In some studies, progesterone receptors displayed abnormalities and caused dysregulation in the endometrial layer of the uterus in patients with endometriosis. Levels of progesterone should increase with pregnancy, but with endometriosis, this process is delayed and can cause an unopposed estrogen state that cannot sustain fertility.
Diagnosing Endometriosis: A Multifaceted Approach
Diagnosing endometriosis can be a complex process, as the symptoms can mimic those of other conditions. The diagnostic journey often begins with a physical examination and an evaluation of the individual’s medical history. If endometriosis is suspected, additional tests may be recommended, such as:
- Ultrasound: An abdominal or transvaginal ultrasound can help identify cysts (endometriomas), possibly endometriosis lesions (this is not common but an up-and-coming area of research), as well as the potential impact on the organs themselves or other abnormalities in the reproductive organs.
- Laparoscopy: Considered the gold standard for diagnosing endometriosis, a laparoscopy involves a minimally invasive surgical procedure where a small camera is inserted into the abdomen, allowing the surgeon to visually inspect the pelvic organs and take tissue samples if necessary.
While the severity of endometriosis is often classified into stages (minimal, mild, moderate, or severe) based on the extent and location of the endometrial growths, it’s important to note that the stage does not necessarily correlate with the intensity of symptoms or the degree of fertility challenges.
Managing Endometriosis: A Multidisciplinary Approach
The management of endometriosis typically involves a multidisciplinary approach, combining medical and surgical interventions tailored to the individual’s unique circumstances and fertility goals. Treatment options may include:
- Pain Management: Over-the-counter or prescription pain medications, such as non-steroidal anti-inflammatory drugs (NSAIDs) or hormonal contraceptives, can help alleviate the discomfort associated with endometriosis.
- Hormone Therapy: Hormonal treatments, such as birth control pills, progestin-only therapy, or gonadotropin-releasing hormone (GnRH) agonists, may have some impact on suppressing the growth of endometriosis and managing symptoms, though these options are only short-term while on the medications and can have some serious side effects.
- Surgery: Laparoscopic or robotic surgery is recommended to remove endometriosis, scar tissue, or cysts, potentially improving fertility outcomes.
- Assisted Reproductive Technologies (ART): In cases where natural conception remains challenging, assisted reproductive technologies like in vitro fertilization (IVF) or intrauterine insemination (IUI) may be recommended.
It’s crucial to work closely with a multidisciplinary team, including reproductive endocrinologists, gynecologists, and fertility specialists, to develop a personalized treatment plan that addresses both the management of endometriosis symptoms and the individual’s fertility goals.
Dietary and Lifestyle Considerations
While there is no definitive evidence that specific dietary or lifestyle changes can cure endometriosis or improve fertility outcomes, maintaining a healthy lifestyle can contribute to overall well-being and potentially alleviate some symptoms. Recommendations may include:
- Balanced Diet: Consuming a diet rich in fresh fruits, and vegetables, minimizing grains, especially gluten, and lean proteins can provide essential nutrients and support overall health.
- Exercise: Regular physical activity, such as low-impact exercises like walking or swimming, can help manage stress and promote overall well-being.
- Stress Management: Engaging in stress-reducing activities like meditation, yoga, or deep breathing exercises can help promote relaxation and reduce the impact of stress on fertility.
- Supplements: While the evidence is limited, some individuals report benefits from taking supplements for pain relief, reducing inflammation, and improving their quality of life.
It’s essential to consult with a healthcare professional before making significant dietary or lifestyle changes, especially if you are undergoing fertility treatments or considering assisted reproductive technologies.
Endometriosis and Pregnancy: Potential Complications
While endometriosis does not necessarily preclude a successful pregnancy, it’s important to be aware of potential complications that may arise. Some of the risks associated with endometriosis during pregnancy include:
- Placenta Previa: Endometriosis may increase the risk of placenta previa, a condition where the placenta partially or completely covers the cervix, potentially leading to bleeding and complications during pregnancy or delivery.
- Miscarriage: Research findings on the link between endometriosis and miscarriage have been mixed, with some studies suggesting an increased risk while others found no significant association.
- Ectopic Pregnancy: Endometriosis may increase the risk of ectopic pregnancy, where the fertilized egg implants outside the uterus, typically in the fallopian tube.
It’s essential to work closely with your healthcare provider to monitor and manage any potential complications that may arise during pregnancy if you have endometriosis.
Mental Well-Being and Psychological Impact of Fertility Treatment for Endo Patients
Living with endometriosis can be a challenging and emotionally taxing experience, particularly for those struggling with fertility issues. The physical pain, emotional distress, and potential financial burdens associated with treatment can take a toll on an individual’s mental well-being. It’s crucial to prioritize self-care and seek support from mental health professionals, support groups, or counseling services if needed.
Furthermore, you and your partner can do these things to help prepare for these possible feelings:
- Prepare and be ready for the emotional journey ahead.
- Cope with grief and loss associated with unsuccessful prior attempts or miscarriages.
- Develop strategies for coping with the news of other people’s births and pregnancies.
- Keep the communication lines between you and your partner open and discuss feelings throughout the entire process.
Endometriosis and Fertility: Navigating the Journey
The path to parenthood for individuals with endometriosis can be challenging, but it’s important to remember that fertility challenges are not insurmountable. By working closely with a multidisciplinary team of healthcare professionals, exploring various treatment options, and maintaining a positive outlook, many individuals with endometriosis can achieve their dream of starting a family.
It’s crucial to be proactive in seeking support and guidance from healthcare providers, as well as accessing resources and support networks specifically designed for those navigating endometriosis and fertility challenges. Organizations like the American Society for Reproductive Medicine (ASRM) and Endometriosis UK offer valuable information, resources, and advocacy support for individuals on this journey.
While endometriosis may present obstacles, embracing a comprehensive approach that addresses both the condition and fertility goals can increase the chances of a successful outcome. With perseverance, the right medical support, and a commitment to self-care, the dream of parenthood can become a reality for many individuals with endometriosis.
REFERENCES
https://www.pennmedicine.org/updates/blogs/fertility-blog/2016/august/endometriosis-and-fertility
https://www.endometriosis-uk.org/endometriosis-fertility-and-pregnanc
Updated: August 9, 2024

Endo in adolescents
Adolescents can be affected by endometriosis. In fact, according to American College of Obstetricians and Gynecologists:
“Endometriosis is the leading cause of secondary dysmenorrhea in adolescents. Endometriosis should be considered in patients with persistent, clinically significant dysmenorrhea despite treatment with hormonal agents and NSAIDs, particularly if no other etiology for chronic pelvic pain or secondary dysmenorrhea has been identified based on history, physical examination, and pelvic ultrasonography. Family history of endometriosis also should raise suspicion because patients with an affected first-degree relative have a 7-fold to 10-fold increased risk of developing endometriosis.”
Adolescents experience significant symptoms and delays in diagnosis. DiVasta et al. (2018) found that their study’s participants “experienced moderate-severe menstrual pain” and that “3 doctors were seen before diagnosis, regardless of age at presentation.” It took an average of 2 years for adolescents to receive a diagnosis (DiVasta et al., 2018). According to the study, they found that participants reported:
“More adolescents (50%) than adults (33%) reported pain starting at menarche and nausea accompanying pain. Noncyclic, general pelvic pain was prevalent. One-half of the participants reported relief of their general pelvic pain after a bowel movement. Pain interfered with work/school, daily activities, exercise, and sleep to a moderate-extreme degree; difficulties were similar by age at diagnosis.”
Find more information here: https://icarebetter.com/teens-and-endometriosis/
References
American College of Obstetricians and Gynecologists. (2018). Dysmenorrhea and endometriosis in the adolescent. Retrieved from https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/12/dysmenorrhea-and-endometriosis-in-the-adolescent
DiVasta, A. D., Vitonis, A. F., Laufer, M. R., & Missmer, S. A. (2018). Spectrum of symptoms in women diagnosed with endometriosis during adolescence vs adulthood. American journal of obstetrics and gynecology, 218(3), 324-e1. Retrieved from https://www.sciencedirect.com/science/article/abs/pii/S0002937817324821

Blood tests for endometriosis- not yet
We hear more and more about blood tests using DNA, RNA, and microRNA being researched as a possible way to help diagnose endometriosis. While more studies are needed, these tests do show some promise (Zafari et al., 2021). It would be nice to be a able to get a simple blood test and know that you probably have endometriosis and be able to plan accordingly. As Fassbender et al. (2015) states: “The most important goal of the test is that no women with endometriosis or other significant pelvic pathology are missed who might benefit from surgery for endometriosis-associated pain and/or infertility.”
MicroRNA are one specfic type of blood test being investigated. MicroRNA are involved in gene expression. Humans have “over 700 miRNAs” that “have been identified and fully sequenced”; these “miRNAs in humans have a direct influence on at least 30% of the genes in the whole genome” (Meštrović, 2018). Papari et al. (2020) explain that: “microRNAs are present in body fluids, including blood…which makes them more stable than circulating hormone or cytokine concentrations and therefore better candidate markers of disease. One miRNA can target several genes, and one gene can be targeted by different miRNAs. Circulating levels of miRNAs are dysregulated in several different cancers and in endometriosis.”
Papari et al. (2020) further states that “no clinical marker of endometriosis, either alone or in combination, has provided adequate sensitivity or specificity for the diagnosis of endometriosis. Thus, the search for suitable diagnostic markers of endometriosis remains a high but unmet research priority.” They did find in their study that a panel of different microRNA improved the accuracy of the test (Papari et al., 2020). Similar to ultrasounds, MRI’s, and other diagnostics studies, they might be helpful to rule in endometriosis but not necessarily entirely rule it out (see “But All Your Tests Are Negative”). It might be an initial step towards investigating the possibility of endometriosis once tests become available, but further investigation is warranted even if negative.
For more information see “Labwork and Blood Tests“
References
Fassbender, A., Burney, R. O., F O, D., D’Hooghe, T., & Giudice, L. (2015). Update on biomarkers for the detection of endometriosis. BioMed research international, 2015. Retrieved from https://www.hindawi.com/journals/bmri/2015/130854/
Meštrović, T. (2018). What is MicroRNA. Retrieved from https://www.news-medical.net/life-sciences/What-is-MicroRNA.aspx
Papari, E., Noruzinia, M., Kashani, L., & Foster, W. G. (2020). Identification of candidate microRNA markers of endometriosis with the use of next-generation sequencing and quantitative real-time polymerase chain reaction. Fertility and Sterility, 113(6), 1232-1241. Retrieved from https://www.fertstert.org/article/S0015-0282(20)30027-3/fulltext
Zafari, N., Bahramy, A., Majidi Zolbin, M., Emadi Allahyari, S., Farazi, E., Hassannejad, Z., & Yekaninejad, M. S. (2021). MicroRNAs as novel diagnostic biomarkers in endometriosis patients: a systematic review and meta-analysis. Expert Review of Molecular Diagnostics, 1-17. Retrieved from https://www.tandfonline.com/doi/abs/10.1080/14737159.2021.1960508

Find Endometriosis Specialists for the Best Possible Outcomes
Table of contents
Why You Need an OB-GYN Who Specializes in Endometriosis
Endometriosis is common (affecting nearly 190 million women worldwide) but poorly understood by many medical professionals. It’s hard to find endometriosis specialists who have completed advanced training. With the proper endo specialist, medical treatment or surgery can lessen your pain, improve your quality of life, and manage complications.
Endometriosis is a chronic pain condition that affects 10-15% of women of reproductive age. It causes painful periods, bleeding between periods, pain during sexual intercourse, and discomfort when passing urine or feces. Despite causing chronic pelvic pain, many medical professionals have a poor understanding of the condition.
In this article, we will look into what endometriosis is and explore how to improve diagnosis, treatment, and outcome factors.
What is Endometriosis?
Endometriosis affects menstruating women and girls and some women post-hysterectomy or post-menopause. The condition also can affect transgender men and non-binary individuals. Endometriosis affects roughly 190 million people worldwide, with immune, genetic and hormonal factors all likely to be at play.
To understand Endometriosis, we first need to understand the endometrium or lining of the uterus.
The Endometrium
A large proportion of the endometrium is stromal cells. Stromal cells regulate cell growth and change during the menstrual cycle.
Endometrial glands line the endometrium. During the menstrual cycle, they widen in response to greater blood flow.
Each cycle, stromal cells, and endometrial glands slough off as part of menstruation.
Endometriosis Lesions
The presence of endometrium-like cells found outside the uterus causes the classic endometriosis symptoms. Discourse exists, but scientists have concluded a genetic basis to the cells’ presence, with endometrium-like cells migrating inappropriately during embryogenesis.
Endometriotic lesions can be in the ovaries, uterine ligaments, fallopian tubes, and pouch of Douglas (the space between the uterus and rectum). In some, lesions are present outside the pelvic cavity. Locations include the bowel, urinary tract wall, diaphragm, lungs, abdomen, and pericardium (the sack around the heart).
The endometrial-like tissue responds to the natural cycle of hormones and also produces some hormones by itself. This tissue has cycles of growth and bleeding.
Whereas menstrual blood in the uterus leaves the body via the vagina, the blood and tissues cannot escape from endometriosis lesions. This trapped cells and tissue leads to the painful processes of inflammation, adhesions, and scarring.
What does it feel like to have Endometriosis?
Although pain is the most common complaint, Endometriosis causes a wide range of symptoms, including:
- Painful periods
- Heavy periods (menorrhagia)
- Vaginal bleeding between periods
- Pain on passing urine or feces
- Bowel symptoms include bloating, constipation, diarrhea, or bleeding from the bowel
- Pain during intercourse
- Tiredness
- Depression
- Infertility.
Social and Emotional Effects
Severe pain can interrupt daily life for many patients. This interruption may include missing school, taking days off work, or being unable to socialize. A study in 2020 found that in over half of women, the pain had reduced their professional, physical, and sexual activity.
Endometriosis is associated with low mood. 15% of women are diagnosed with depression, with an average age at diagnosis of 22.
Infertility
Infertility can be the only symptom of Endometriosis for some women. Around 30-50% of patients cannot get pregnant owing to inflammation, pelvic adhesions, blockage of the fallopian tubes, and changes to the pelvic anatomy.
Other Symptoms
Additional symptoms are dependent on the location of endometriosis lesions. For example, an endometriotic lesion in the lung could cause breathlessness or chest pain. A study of over 2000 patients found that endometriotic nodules caused leg and buttock pain, as well as numbness, similar to sciatic pain.
Misdiagnosis and incorrect management are therefore common for women with symptoms that are not classic to pelvic endometriotic lesions.
Endometriosis Myths
The average delay in the diagnosis of Endometriosis is more than seven years, leading to “unnecessary suffering and reduced quality of life.” This delay leads many people to the internet to conduct their own research before and during diagnosis. However, the internet is awash with myths.
The importance of educating yourself via a reputable source such as iCareBetter cannot be understated.
Find Endometriosis Specialists for Appropriate Diagnosis & Treatment
The widespread misunderstanding of Endometriosis hinders its diagnosis and treatment. The inappropriate investigation, treatment with analgesics, or hormonal suppression do little to manage the cause while delaying diagnosis. Women who felt they were not listened to nor understood by doctors have described frustration, anger, annoyance, and sadness.
Reassuringly, appropriate diagnosis and treatment can lead to significant improvements in pain. This is precisely why it is crucial to find an endometriosis specialist. Only highly specialized surgeons with a comprehensive team can perform a thorough excision to remove endometriotic lesions, including extra-pelvic locations. Complete removal can significantly improve overall outcomes, including relief from pain and increased quality of life.
iCareBetter Endometriosis Care
iCareBetter is a platform that connects patients with experts in endometriosis care. At iCareBetter, patients have access to surgeons who have completed advanced training. These professionals have shown expertise in the diagnosis and treatment of complex Endometriosis. iCareBetter utilizes a transparent and unbiased system to ensure that only doctors with proven advanced excision skills and a comprehensive care team can be on their surgeons’ list.
Patients can select their surgeon based on their specific symptoms. This empowers patients to consult a doctor who truly understands the complexity of their condition. Patients can access specialists for endometriosis in the pelvis, bowels, bladder, thorax, heart, or diaphragm. They also can find help with infertility issues.
A highly specialized endo surgeon will take a holistic approach to treatment. This holistic approach includes managing secondary comorbidities such as infertility, even in stage III and IV disease patients.
At iCareBetter, patients can also access expert physical therapists who understand the condition. Working with a physical therapist gives access to myofascial release techniques, visceral mobilization, and the tools to manage a susceptible nervous system for better pain management.
Team-based expert care improves post-operative outcomes. For some iCareBetter doctors, post-treatment reports of satisfactory pain relief could be over 80%, with less than 20% of women requiring subsequent pelvic surgery. Moreover, many patients see reduced pain relief requirements post-recovery.
Standards of excellence, such as those endorsed by iCareBetter, must become a driving force behind treatment protocols for Endometriosis. Women should no longer shoulder the pain and reduced quality of life associated with substandard care.
Conclusion
Endometriosis occurs due to the presence of endometrium-like cells found outside the uterus. The resulting inflammation, adhesions, and scarring can cause severe pain and symptoms related to the location of the lesions. By connecting patients with expert surgeons in endometriosis care, iCareBetter empowers patients to access the care leading to better outcomes. Advanced surgical excision, physical therapy, and an expert team-based approach can reduce pain, as well as skillfully manage secondary complications.
Find endometriosis specialists today.

