
Top Endometriosis Specialist Florida: Your Path to Pain-Free Living
Endometriosis affects approximately 10% of women in Florida, impacting their daily lives and overall well-being. This chronic condition, characterized by the growth of uterine-like tissue outside the uterus, can cause debilitating pain, fertility issues, and a range of other symptoms. For those living in the Sunshine State, an endometriosis specialist is crucial to managing this complex disorder effectively. The persistent pelvic pain, heavy menstrual bleeding, and fatigue associated with the condition can significantly hinder one’s ability to enjoy the state’s beautiful beaches, outdoor activities, and vibrant social scene. Patients can benefit from personalized care plans tailored to their unique needs and lifestyles by choosing an endometriosis specialist in Florida.
As we delve deeper into the world of endometriosis care in Florida, we’ll explore the importance of specialized treatment, highlight top experts in the field, and discuss the various options available to those seeking relief from this challenging condition. Whether you’re newly diagnosed or have been struggling with endometriosis for years, this comprehensive guide will empower you to take control of your health and find your path to pain-free living in the Sunshine State.
Understanding Endometriosis: More Than Just a Sunshine State Struggle
Endometriosis is a complex gynecological condition that affects women worldwide, including those living in Florida. To fully appreciate the importance of seeking specialized care, it’s crucial to understand the intricacies of this disorder and how it impacts the lives of patients.
Decoding the Complexities of Endometriosis
Endometriosis occurs when tissue similar to the lining of the uterus grows outside the uterine cavity. This misplaced tissue can be found on various organs, including the ovaries, fallopian tubes, bladder, and even the intestines. Despite being outside the uterus, this tissue continues to respond to hormonal changes throughout the menstrual cycle, leading to inflammation, pain, and the formation of scar tissue.
The exact cause of endometriosis remains unknown, but several factors may contribute to its development, including:
- Retrograde menstruation
- Genetic predisposition
- Immune system dysfunction
- Environmental factors
Understanding these potential causes is essential for developing effective treatment strategies and managing the condition long-term.
How Endometriosis Affects Floridians’ Active Lifestyles
Florida’s warm climate and abundance of outdoor activities make it an ideal place for an active lifestyle. However, for women with endometriosis, the state’s unique environment can present additional challenges:
- Heat sensitivity: Florida’s hot and humid weather can exacerbate pelvic pain and inflammation associated with endometriosis.
- Beach activities: Swimming and sunbathing, popular pastimes in Florida, may be uncomfortable or even painful for those with severe pelvic pain or bloating.
- Outdoor sports: Engaging in high-impact activities like running or tennis can be challenging due to pelvic discomfort and fatigue.
- Social events: Florida’s vibrant social scene may be difficult to enjoy fully when dealing with unpredictable pain and fatigue.
- Work-life balance: The state’s tourism and service industries often require long hours and physical stamina, which can be taxing for those managing endometriosis symptoms.
Recognizing the Signs of Endometriosis: A Comprehensive Symptom Checklist
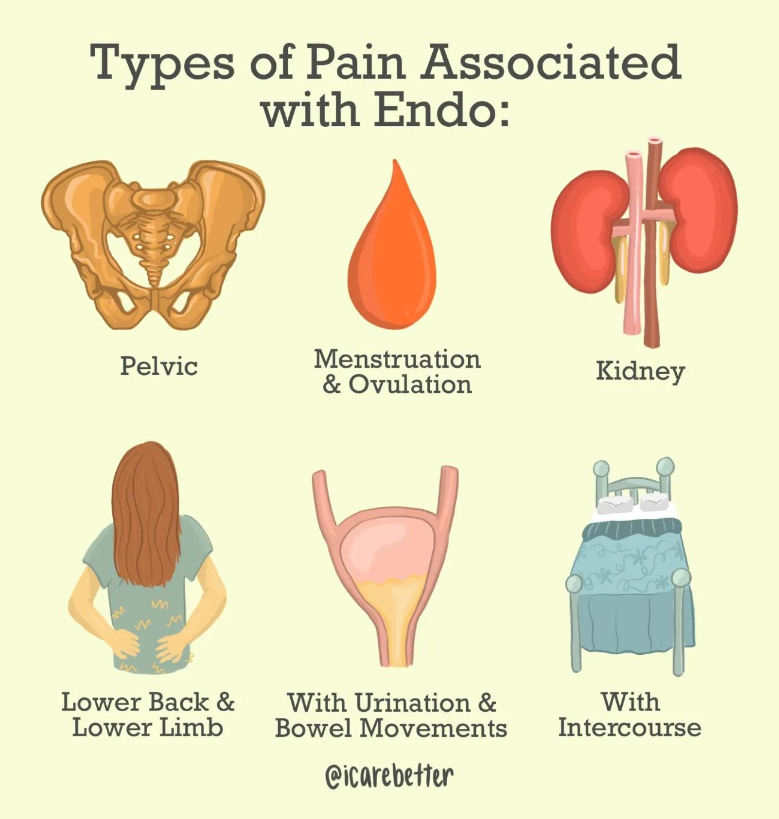
Recognizing endometriosis can be difficult due to its wide range of symptoms. To help, here’s a comprehensive checklist of common endometriosis symptoms to watch for:
- Severe menstrual cramps
- Chronic pelvic pain
- Pain during or after sexual intercourse
- Heavy or irregular menstrual bleeding
- Painful bowel movements or urination, especially during menstruation
- Lower back pain
- Abdominal bloating
- Fatigue
- Nausea or vomiting
- Infertility or difficulty conceiving
- Diarrhea or constipation
- Mood swings or depression
- Leg pain
- Painful ovulation
- Chest pain or shortness of breath (in rare cases of thoracic endometriosis)
- Painful urination
It’s important to note that experiencing one or more of these symptoms doesn’t necessarily mean you have endometriosis. However, if you’re concerned about your symptoms, consulting with an endometriosis specialist in Florida can help you receive an accurate diagnosis and appropriate treatment plan.
The Florida Advantage: Cutting-Edge Endo Care Close to Home
Florida offers its residents and visitors a unique advantage regarding endometriosis care. The Sunshine State has become a hub for advanced medical treatments and research, providing women with access to top-tier care without requiring extensive travel. This section explores the benefits of seeking endometriosis treatment in Florida and highlights the state’s commitment to medical excellence in this field.
Access to Top-Tier Treatments and Research
Florida’s medical landscape is characterized by its commitment to innovation and cutting-edge treatments. For women with endometriosis, this translates to:
- Advanced Diagnostic Techniques: Florida’s leading medical centers utilize state-of-the-art imaging technologies, such as high-resolution ultrasounds and MRI scans, to accurately diagnose and stage endometriosis.
- Minimally Invasive Surgical Options: Some Florida specialists are trained in advanced laparoscopic and robotic surgical techniques, offering patients less invasive treatment options with shorter recovery times.
- Participation in Clinical Trials: Several Florida medical institutions actively participate in endometriosis research, allowing patients to access experimental treatments and contribute to scientific advancements.
- Multidisciplinary Approach: Some of Florida’s experts employ a team-based approach, bringing together gynecologists, general surgeons, urologists, pain specialists, fertility experts, and other relevant professionals to provide comprehensive care.
- Fertility Preservation Options: For women concerned about their future fertility, Florida offers advanced reproductive technologies and fertility preservation techniques alongside endometriosis treatment.
Top Endometriosis Specialists in Florida: Experts You Can Trust
Florida is home to some highly skilled and best endometriosis specialists dedicated to providing exceptional care for women struggling with this complex condition. These experts combine their extensive knowledge with cutting-edge techniques to offer personalized treatment plans that address each patient’s unique needs. In this section, we’ll highlight some of the leading endometriosis specialists in Florida and explore their areas of expertise.
Dr. Andrea Vidali is a renowned endometriosis specialist in Miami, Florida, and New York. With over two decades of experience in reproductive endocrinology and infertility, Dr. Vidali has gained international recognition for his expertise in minimally invasive surgical techniques for endometriosis treatment.

Key areas of expertise:
- Advanced excision surgery
- Fertility preservation in endometriosis patients
- Immunological aspects of endometriosis
- Robotic-assisted endometriosis surgery
Dr. Vidali’s approach focuses on thorough diagnosis and comprehensive treatment plans that address both pain management and fertility concerns. His patients benefit from his extensive experience in complex cases and his commitment to staying at the forefront of endometriosis research and treatment innovations.
Dr. Gaby Moawad is a highly respected gynecologist and endometriosis specialist in Orlando, Florida. Known for his patient-centered approach, he combines surgical expertise with a deep understanding of the holistic needs of women with endometriosis.

Areas of specialization:
- Laparoscopic and robotic excision of endometriosis
- Management of chronic pelvic pain
- Fertility-sparing endometriosis treatments
- Multidisciplinary approach to endometriosis care
Dr. Moawad’s practice emphasizes comprehensive care, addressing not only the physical symptoms of endometriosis but also the emotional and psychological aspects of living with a chronic condition. His patients appreciate his compassionate approach and dedication to improving their quality of life.
Finding the right endometriosis specialist in Florida takes time and research. Consultations offer a chance to discuss your case and assess the fit. Choosing the best specialist is key to managing your condition and improving your quality of life, as these experts understand the unique challenges women with endometriosis face in Florida.
Treatment Options: As Diverse as Florida’s Landscape
Just as Florida boasts a diverse landscape of beaches, swamps, and citrus groves, the treatment options for endometriosis in the state are equally varied and comprehensive. Florida’s endometriosis specialists offer a wide range of advanced surgical techniques, non-invasive therapies, and holistic approaches to address the complex needs of patients with this challenging condition. This section explores the diverse treatment landscape available to women seeking endometriosis care in Florida.
Advanced Surgical Techniques Available in Florida
Surgical intervention remains a cornerstone of endometriosis treatment, especially for severe cases or when conservative measures have failed. Florida’s top endometriosis specialists are skilled in various advanced surgical techniques:
- Laparoscopic Excision Surgery:
- A minimally invasive approach using small incisions
- Allows for thorough removal of endometrial implants
- Reduced scarring and faster recovery compared to open surgery
- Often considered the gold standard for endometriosis treatment
- Robotic-Assisted Surgery:
- Utilizes advanced robotic technology for enhanced precision
- Offers 3D visualization and improved dexterity for complex procedures
- Particularly useful for deep-infiltrating endometriosis
- Fertility-Preserving Surgery:
- Focuses on removing endometriosis while preserving reproductive organs
- Often combined with fertility treatments for women trying to conceive
- Presacral Neurectomy:
- Targets nerve pathways to alleviate chronic pelvic pain
- It can be performed alongside excision surgery for comprehensive treatment
- Hysterectomy with Bilateral Salpingo-Oophorectomy:
- Reserved for severe cases or when other treatments have failed
- Involves the removal of the uterus, fallopian tubes, and ovaries
- Considered a last resort due to its impact on fertility and hormonal balance
Non-Invasive Therapies and Holistic Approaches
Florida’s endometriosis specialists recognize the importance of non-surgical interventions and holistic care in managing the condition. Some common non-invasive therapies include:
- Hormonal Treatments:
- Birth control pills
- Progestin-only medications
- GnRH agonists and antagonists
- Aromatase inhibitors
- Pain Management Techniques:
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Nerve blocks
- Transcutaneous electrical nerve stimulation (TENS)
- Physical Therapy:
- Pelvic floor therapy
- Manual therapy techniques
- Exercise programs tailored for endometriosis patients
- Nutritional Counseling:
- Anti-inflammatory diets
- Elimination diets to identify food sensitivities
- Supplementation strategies
- Complementary Therapies:
- Acupuncture
- Yoga and mindfulness practices
- Herbal medicine under professional guidance
- Psychological Support:
- Cognitive-behavioral therapy
- Support groups
- Stress management techniques
Choosing the Right Treatment Plan
When considering endometriosis treatment options in Florida, working closely with your specialist to develop a personalized plan is essential. Factors to consider include:
- Severity and location of endometriosis lesions
- Primary symptoms and their impact on quality of life
- Fertility goals and reproductive health concerns
- Overall health and any coexisting conditions
- Personal preferences and lifestyle considerations
Florida endometriosis specialists offer comprehensive care through a multimodal approach. They combine surgery with noninvasive therapies to address physical and emotional symptoms. With diverse treatment options—from advanced surgery to holistic therapies—patients can access personalized care for effective management and improved quality of life.
Living with Endometriosis in Florida: Beyond Medical Care
Managing endometriosis extends far beyond the doctor’s office or operating room. For those living with this condition in Florida, finding ways to cope with symptoms and maintain a high quality of life is crucial. The Sunshine State’s unique environment and lifestyle offer challenges and opportunities for those navigating life with endometriosis. This section explores strategies for managing symptoms in Florida’s climate and lifestyle and the supportive therapies and resources available to endometriosis patients in the state.
Adapting to Florida’s Climate and Lifestyle
Florida’s warm, humid climate and active lifestyle can present unique challenges for women with endometriosis. Here are some strategies to help manage symptoms while enjoying all that the state has to offer:
- Heat Management:
- Use cooling products like portable fans or cooling towels when outdoors
- Plan outdoor activities for cooler parts of the day
- Stay hydrated to help regulate body temperature
- Beach-Friendly Strategies:
- Invest in comfortable, supportive swimwear
- Use beach umbrellas or tents for shade and privacy
- Bring a supportive cushion or beach chair for comfort
- Exercise Adaptations:
- Opt for low-impact activities like swimming or yoga
- Try water aerobics or beach walks for gentle exercise
- Listen to your body and pace yourself during physical activities
- Workplace Accommodations:
- Use ergonomic furniture to reduce pelvic strain
- Take regular breaks to stretch and move
- Communicate with employers about flexible work arrangements if needed
- Social Life Adjustments:
- Plan activities with built-in rest periods
- Choose venues with comfortable seating options
- Be open with friends about your needs and limitations
Supportive Therapies for Endometriosis Management
Florida offers many supportive therapies that can complement medical treatments and help manage endometriosis symptoms.
- Acupuncture:
- It may help reduce pain and inflammation
- It can be particularly beneficial for menstrual cramps and chronic pelvic pain
- Massage Therapy:
- It helps relax tense muscles and reduce overall body pain
- It may improve circulation and reduce stress
- Yoga and Pilates:
- Gentle stretching can help alleviate pelvic pain
- Mindfulness aspects can aid in stress reduction
- Nutritional Counseling:
- Guidance on anti-inflammatory diets
- Help in identifying and managing food sensitivities
- Pelvic Floor Physical Therapy:
- Addresses muscle tension and dysfunction in the pelvic area
- Can improve pain during intercourse and bladder/bowel symptoms
- Mindfulness and Meditation:
- Techniques for managing pain and reducing stress
- Can improve overall emotional well-being
Community Resources and Support Groups
Florida offers numerous resources and support groups for women living with endometriosis:
- Endometriosis Association of Florida:
- Provides education and support for patients and families
- Organizes regular meetups and events across the state
- Online Support Communities:
- Florida-specific Facebook groups and forums
- Virtual support meetings for those unable to attend in-person events
- Fertility Support Networks:
- Resources for women dealing with endometriosis-related infertility
- Connections to fertility specialists and treatment options in Florida
- Workplace Advocacy Groups:
- Organizations that help women navigate workplace challenges related to chronic illness
- Resources for understanding employment rights and accommodations
Lifestyle Modifications for Symptom Management
In addition to medical treatments and supportive therapies, certain lifestyle modifications can help manage endometriosis symptoms:
- Stress Reduction Techniques:
- Regular meditation or deep breathing exercises
- Engaging in hobbies or activities that promote relaxation
- Sleep Hygiene:
- Establishing a consistent sleep schedule
- Creating a comfortable sleep environment
- Dietary Adjustments:
- Keeping a food diary to identify trigger foods
- Incorporating anti-inflammatory foods into the diet
- Exercise Routine:
- Finding a balance between rest and gentle activity
- Incorporating low-impact exercises like swimming or cycling
- Emotional Well-being:
- Seeking counseling or therapy to address the emotional impact of living with a chronic condition
- Practicing self-compassion and setting realistic expectations
By using Florida’s resources and strategies, women with endometriosis can manage symptoms and maintain a fulfilling lifestyle. Remember, it’s a journey—be patient and celebrate small victories.
Conclusion: Empowering Your Endo Journey in the Sunshine State
As we conclude our exploration of endometriosis care in Florida, it’s clear that the Sunshine State offers a wealth of resources, expertise, and support for women navigating this challenging condition. From world-class specialists to cutting-edge treatments and supportive communities, Florida provides a comprehensive ecosystem for endometriosis management. We encourage you to take the next step in your endometriosis care journey. Whether that means scheduling a consultation with a specialist, exploring new treatment options, or connecting with a local support group, every action you take is a step towards better health and well-being.
Remember, your health journey is unique, and finding the right care may take time. Be patient with yourself, advocate for your needs, and don’t hesitate to seek second opinions or explore different treatment options. With perseverance and the right support, you can navigate the challenges of endometriosis and embrace all that life in Florida has to offer.
Here’s to your health, well-being, and a brighter, pain-free future in the Sunshine State!
REFERENCES:
https://ufhealth.org/conditions-and-treatments/endometriosis
https://www.medicalnewstoday.com/provider-near-me/condition-or-procedure/endometriosis/fl-florida
https://www.acibademhealthpoint.com/endometriosis-specialist-in-miami-expert-care
https://health.usf.edu/care/obgyn/services-specialties/endometriosis

Does Endometriosis Cause Infertility? Covering the Basics
Table of contents
- Learn More About the Connections Between Endometriosis and Infertilit y
- What is Endometriosis
- Endometriosis and Fertility: Exploring the Connection
- What Happens When Endometriosis Does Cause Infertility?
- Other Data on Endometriosis and Reproduction
- Diagnosing Endometriosis: A Multifaceted Approach
- Managing Endometriosis: A Multidisciplinary Approach
- Dietary and Lifestyle Considerations
- Endometriosis and Pregnancy: Potential Complications
- Mental Well-Being and Psychological Impact of Fertility Treatment for Endo Patients
- Endometriosis and Fertility: Navigating the Journey
Learn More About the Connections Between Endometriosis and Infertility
An endometriosis (endo) diagnosis can be a frightening thing. Very frightening. While this inflammatory condition can be binary or non-binary, women of childbearing age are prone to issues with reproduction due to endo. So does endometriosis cause infertility? Keep reading as I break down the basics of this topic. In this comprehensive guide, I will delve into the complex interplay between endometriosis and fertility, exploring the condition’s impact, treatment options, and strategies to overcome potential obstacles on the journey to parenthood. I will also discuss the emotional impact of this condition on patients.
What is Endometriosis
Endometriosis is a chronic inflammatory condition. In this disease, endometrial-like lesions implant on tissues and organs throughout the abdomen and pelvis, even elsewhere in the body! These lesions contain glands and stroma, similar to the endometrium (the tissue that lines the uterine walls), causing chronic inflammatory reactions.
Endometriosis lesions produce many substances and even make their own estrogen, which, as a result, causes a variety of issues locally and systemically. Pain is one of the most common symptoms, though silent endo exists as well. Please continue reading this article to learn more about endometriosis.
Endometriosis and Fertility: Exploring the Connection
While endometriosis does not automatically equate to infertility, there is a well-documented association between the two. Approximately 30% to 50% of individuals with endometriosis experience fertility challenges, though the reasons behind this link are not fully understood. Several potential mechanisms have been proposed:
- Anatomical Distortions: Endometriosis can cause physical distortions in the reproductive anatomy, leading to scarring, adhesions, and obstructions in the fallopian tubes or ovaries, hindering the fertilization process.
- Inflammatory Response: The lesions can trigger an inflammatory response, creating an inhospitable environment for fertilization and implantation.
- Hormonal Imbalances: Endometriosis may disrupt the delicate hormonal balance required for ovulation and implantation, potentially impacting fertility.
- Egg Quality: Some research suggests that endometriosis may adversely affect egg quality, further complicating the conception process.
Despite these potential challenges, it’s important to note that more than 70% of individuals with mild to moderate endometriosis can conceive naturally, offering hope for those seeking to start a family.
What Happens When Endometriosis Does Cause Infertility?
It can. 25 to 50% of women with infertility have endometriosis, and 30 to 50% of women with endometriosis have infertility. However, it is very encouraging to know that most women with endometriosis can become pregnant.
This statistic is significant. Many younger women with this disorder feel psychological effects due to the possibility of not being able to have kids. Not all patients carry this sentiment. Growing numbers of people do not want to have children. However, for those who do, these thoughts and emotions about fertility can be devastating. Then, endometriosis patients who do conceive often worry about the pregnancy and subsequent delivery of the baby.
Other Data on Endometriosis and Reproduction
Studies have also demonstrated that the enzyme aromatase may also play a role in endometriosis and infertility. There is an abnormally high level of this enzyme in the endometrium and endometriosis lesions in patients with endometriosis. In the uterus, this enzyme may affect both natural endometrial development and its receptivity for the implantation of the fetus.
Progesterone is another hormone that may play a role in implantation failure. Resistance to this enzyme can affect reproduction, as it is necessary for a normal pregnancy. In some studies, progesterone receptors displayed abnormalities and caused dysregulation in the endometrial layer of the uterus in patients with endometriosis. Levels of progesterone should increase with pregnancy, but with endometriosis, this process is delayed and can cause an unopposed estrogen state that cannot sustain fertility.
Diagnosing Endometriosis: A Multifaceted Approach
Diagnosing endometriosis can be a complex process, as the symptoms can mimic those of other conditions. The diagnostic journey often begins with a physical examination and an evaluation of the individual’s medical history. If endometriosis is suspected, additional tests may be recommended, such as:
- Ultrasound: An abdominal or transvaginal ultrasound can help identify cysts (endometriomas), possibly endometriosis lesions (this is not common but an up-and-coming area of research), as well as the potential impact on the organs themselves or other abnormalities in the reproductive organs.
- Laparoscopy: Considered the gold standard for diagnosing endometriosis, a laparoscopy involves a minimally invasive surgical procedure where a small camera is inserted into the abdomen, allowing the surgeon to visually inspect the pelvic organs and take tissue samples if necessary.
While the severity of endometriosis is often classified into stages (minimal, mild, moderate, or severe) based on the extent and location of the endometrial growths, it’s important to note that the stage does not necessarily correlate with the intensity of symptoms or the degree of fertility challenges.
Managing Endometriosis: A Multidisciplinary Approach
The management of endometriosis typically involves a multidisciplinary approach, combining medical and surgical interventions tailored to the individual’s unique circumstances and fertility goals. Treatment options may include:
- Pain Management: Over-the-counter or prescription pain medications, such as non-steroidal anti-inflammatory drugs (NSAIDs) or hormonal contraceptives, can help alleviate the discomfort associated with endometriosis.
- Hormone Therapy: Hormonal treatments, such as birth control pills, progestin-only therapy, or gonadotropin-releasing hormone (GnRH) agonists, may have some impact on suppressing the growth of endometriosis and managing symptoms, though these options are only short-term while on the medications and can have some serious side effects.
- Surgery: Laparoscopic or robotic surgery is recommended to remove endometriosis, scar tissue, or cysts, potentially improving fertility outcomes.
- Assisted Reproductive Technologies (ART): In cases where natural conception remains challenging, assisted reproductive technologies like in vitro fertilization (IVF) or intrauterine insemination (IUI) may be recommended.
It’s crucial to work closely with a multidisciplinary team, including reproductive endocrinologists, gynecologists, and fertility specialists, to develop a personalized treatment plan that addresses both the management of endometriosis symptoms and the individual’s fertility goals.
Dietary and Lifestyle Considerations
While there is no definitive evidence that specific dietary or lifestyle changes can cure endometriosis or improve fertility outcomes, maintaining a healthy lifestyle can contribute to overall well-being and potentially alleviate some symptoms. Recommendations may include:
- Balanced Diet: Consuming a diet rich in fresh fruits, and vegetables, minimizing grains, especially gluten, and lean proteins can provide essential nutrients and support overall health.
- Exercise: Regular physical activity, such as low-impact exercises like walking or swimming, can help manage stress and promote overall well-being.
- Stress Management: Engaging in stress-reducing activities like meditation, yoga, or deep breathing exercises can help promote relaxation and reduce the impact of stress on fertility.
- Supplements: While the evidence is limited, some individuals report benefits from taking supplements for pain relief, reducing inflammation, and improving their quality of life.
It’s essential to consult with a healthcare professional before making significant dietary or lifestyle changes, especially if you are undergoing fertility treatments or considering assisted reproductive technologies.
Endometriosis and Pregnancy: Potential Complications
While endometriosis does not necessarily preclude a successful pregnancy, it’s important to be aware of potential complications that may arise. Some of the risks associated with endometriosis during pregnancy include:
- Placenta Previa: Endometriosis may increase the risk of placenta previa, a condition where the placenta partially or completely covers the cervix, potentially leading to bleeding and complications during pregnancy or delivery.
- Miscarriage: Research findings on the link between endometriosis and miscarriage have been mixed, with some studies suggesting an increased risk while others found no significant association.
- Ectopic Pregnancy: Endometriosis may increase the risk of ectopic pregnancy, where the fertilized egg implants outside the uterus, typically in the fallopian tube.
It’s essential to work closely with your healthcare provider to monitor and manage any potential complications that may arise during pregnancy if you have endometriosis.
Mental Well-Being and Psychological Impact of Fertility Treatment for Endo Patients
Living with endometriosis can be a challenging and emotionally taxing experience, particularly for those struggling with fertility issues. The physical pain, emotional distress, and potential financial burdens associated with treatment can take a toll on an individual’s mental well-being. It’s crucial to prioritize self-care and seek support from mental health professionals, support groups, or counseling services if needed.
Furthermore, you and your partner can do these things to help prepare for these possible feelings:
- Prepare and be ready for the emotional journey ahead.
- Cope with grief and loss associated with unsuccessful prior attempts or miscarriages.
- Develop strategies for coping with the news of other people’s births and pregnancies.
- Keep the communication lines between you and your partner open and discuss feelings throughout the entire process.
Endometriosis and Fertility: Navigating the Journey
The path to parenthood for individuals with endometriosis can be challenging, but it’s important to remember that fertility challenges are not insurmountable. By working closely with a multidisciplinary team of healthcare professionals, exploring various treatment options, and maintaining a positive outlook, many individuals with endometriosis can achieve their dream of starting a family.
It’s crucial to be proactive in seeking support and guidance from healthcare providers, as well as accessing resources and support networks specifically designed for those navigating endometriosis and fertility challenges. Organizations like the American Society for Reproductive Medicine (ASRM) and Endometriosis UK offer valuable information, resources, and advocacy support for individuals on this journey.
While endometriosis may present obstacles, embracing a comprehensive approach that addresses both the condition and fertility goals can increase the chances of a successful outcome. With perseverance, the right medical support, and a commitment to self-care, the dream of parenthood can become a reality for many individuals with endometriosis.
REFERENCES
https://www.pennmedicine.org/updates/blogs/fertility-blog/2016/august/endometriosis-and-fertility
https://www.endometriosis-uk.org/endometriosis-fertility-and-pregnanc
Updated: August 9, 2024

7 Ways to Prepare For First Endometriosis Specialist Appointment
Table of contents
Diagnosis. Treatment. Surgery. Many Topics May Be Discussed At Your Visit
An endometriosis specialist appointment is not something you do every day (although sometimes it might feel like all day while you’re waiting there). However, the time you get to talk with the doctor may be pretty short. During that moment of consultation with the endometriosis (endo) specialist, you might feel brain fogged or bombarded. Whether it’s the diagnosis, treatment, surgery, pain management, or an endometriosis symptom you want to bring up, it’s easy to forget an essential topic while you’re there.
To make the most out of your initial endometriosis specialist appointment with an endometriosis specialist, we’ve made a list of seven ways you can prepare for the visit. First, we will give a short description of what endometriosis is.
What’s Endometriosis?
Endometriosis is a female medical disorder in which tissue similar to the endometrium (tissue that lines the walls of the uterus) grows outside the uterus. This endometriosis tissue can grow on the surface of the uterus, ovaries, intestines, fallopian tubes, bladder, or other organs in the body.
During menstruation, this tissue releases blood, and it sloughs off. However, this blood and tissue often remain trapped with no way to escape the body. This increased pressure can result in moderate to severe pain, among other symptoms. If you want to learn more about endometriosis and get a general background on the condition, read our article, “Endometriosis 101: Covering the Basics.”
Why You Are Here
People of various ages and demographics are subject to this often debilitating inflammatory pelvic disorder. Whether you have confirmed the diagnosis of endometriosis or if you need surgery to verify its presence and remove lesions – these suggestions can help you prepare for the endometriosis specialist appointment. There are many stages of endometriosis. Whether you’ve got into a specialist early on your journey or later, the important thing is that you are here now – exploring treatment options.
7 Ways to Prepare for Endometriosis Specialist Appointment
Once you have found an experienced endometriosis specialist, it’s essential to prepare yourself for the doctor’s appointment ahead of time. There is no concrete test to diagnose endometriosis (outside of surgery). Therefore, it’s imperative to have a solid understanding of the signs and symptoms of endo and detailed accounts of your own experience ready. Simple things such as medical records or journals that list all your endometriosis symptoms are a vital arsenal that will help you and your doctor determine your treatment plan.
1. Gather Your Records.
Unfortunately, most people with endometriosis have had many doctor appointments before seeing an endometriosis specialist. Therefore, you should have some medical records for them to review during your first appointment with an endo specialist. Gather everything from your regular medical history from your general practitioner to your OB/GYN records, testing, imaging, blood work, etc. Even if you think the particular doctor appointment or medical history is insignificant, you might be surprised by the various conditions linked to endometriosis. Bring it all. This information could play a vital role in your endometriosis treatment.
2. Keep a Journal of Endometriosis Symptoms/Pain.
Write down all the possible endo signs and symptoms you’ve had leading up to the doctor’s appointment. If you get a visit scheduled, and it’s a couple of weeks out, start the journal at that time, but also include the signs and symptoms you’ve experienced leading up to that point. Then, from that date until your appointment, write down all the different types of symptoms you experience. Include everything, even if you don’t think it’s relevant, like colds, headaches, stomach issues, shortness of breath, chest pain, etc. Also, be sure to include your emotions and feelings because endometriosis can significantly impact mental health and can lead to conditions such as depression and anxiety. Emotions and mental health are essential as you might want to include a counselor as part of your holistic endometriosis treatment team.
3. Bring This Printable Guide.
At endometriosis.org, they’ve created a convenient guide that can help you describe your symptoms and know what to ask your endometriosis specialist. Click here for the PDF. Please print it out and answer all the questions. Bring this with you to your doctor’s appointment to help specifically describe your endometriosis pain and other symptoms.
4. Take All Your Medications With You.
The importance of this cannot be understated. Even if you have a medication reconciliation (also known as a “med rec” for short) from your doctor, it’s important to realize those are not always up-to-date with everything you take. This inconsistency is especially true if you are on medications from multiple specialists or take supplements as well. The best way for your endo specialist to have a complete picture of all the medicines you are currently taking is by bringing them with you to the doctor’s appointment. You should include any supplements or over-the-counter medications. Bring in the physical bottles along with any medication history records.
5. Prepare Yourself Mentally.
Go into the appointment with the bold mindset that you will ask every single question you have to gain clarity on your endometriosis diagnosis and treatment options. Endometriosis is an aggressive inflammatory disorder that can have a devastating impact on your quality of life. It would help if you carried an even more aggressive attitude toward trying to stop it dead in its tracks.
6. Bring a List of Questions.
What’s been bothering you the most? Pain? Bowel symptoms? Bring a list of all the important questions that you want answers to. Writing them down will help you not forget during the appointment. Furthermore, when the doctor sees you have a list of questions you want answers to, it makes it harder for them to get up and walk out of the room like the appointment is over. If something like that has ever happened to you, we are sorry you’ve experienced this. That’s why it’s crucial to find a vetted endometriosis expert.
7. Take a Support Person With You.
Finding a good endo expert is no easy task (unless you use iCareBetter to connect you to one). If you are the type of person who is a bit shy or feels intimidated, you should bring your best support person to the appointment with you. Even if you are not nervous about your first endometriosis specialist appointment, having someone you trust by your side can help you process the information and encourage you along your journey. If no one you would like to accompany you, consider bringing a recorder and taping the visit. Because this can help you go back later and make sure you’ve understood all the information. Most doctors will have no qualms about recording your visit.
Endometriosis Care Process with iCareBetter
1- Find an expert based on keyword/ specialty or state
2- choose your doctor from the list
3- Get the contact info
4- First call and consultation.
5- Get info regarding costs and care process
6- Receive care
We Want to Hear From You
Have you been to an endometriosis specialist (OB-GYN experienced in endo)? If so, is there anything you wished you would have done differently? If you’ve not been to an endo specialist yet, what is your biggest concern about the first doctor visit?

