
Top Endometriosis Specialist Florida: Your Path to Pain-Free Living
Endometriosis affects approximately 10% of women in Florida, impacting their daily lives and overall well-being. This chronic condition, characterized by the growth of uterine-like tissue outside the uterus, can cause debilitating pain, fertility issues, and a range of other symptoms. For those living in the Sunshine State, an endometriosis specialist is crucial to managing this complex disorder effectively. The persistent pelvic pain, heavy menstrual bleeding, and fatigue associated with the condition can significantly hinder one’s ability to enjoy the state’s beautiful beaches, outdoor activities, and vibrant social scene. Patients can benefit from personalized care plans tailored to their unique needs and lifestyles by choosing an endometriosis specialist in Florida.
As we delve deeper into the world of endometriosis care in Florida, we’ll explore the importance of specialized treatment, highlight top experts in the field, and discuss the various options available to those seeking relief from this challenging condition. Whether you’re newly diagnosed or have been struggling with endometriosis for years, this comprehensive guide will empower you to take control of your health and find your path to pain-free living in the Sunshine State.
Understanding Endometriosis: More Than Just a Sunshine State Struggle
Endometriosis is a complex gynecological condition that affects women worldwide, including those living in Florida. To fully appreciate the importance of seeking specialized care, it’s crucial to understand the intricacies of this disorder and how it impacts the lives of patients.
Decoding the Complexities of Endometriosis
Endometriosis occurs when tissue similar to the lining of the uterus grows outside the uterine cavity. This misplaced tissue can be found on various organs, including the ovaries, fallopian tubes, bladder, and even the intestines. Despite being outside the uterus, this tissue continues to respond to hormonal changes throughout the menstrual cycle, leading to inflammation, pain, and the formation of scar tissue.
The exact cause of endometriosis remains unknown, but several factors may contribute to its development, including:
- Retrograde menstruation
- Genetic predisposition
- Immune system dysfunction
- Environmental factors
Understanding these potential causes is essential for developing effective treatment strategies and managing the condition long-term.
How Endometriosis Affects Floridians’ Active Lifestyles
Florida’s warm climate and abundance of outdoor activities make it an ideal place for an active lifestyle. However, for women with endometriosis, the state’s unique environment can present additional challenges:
- Heat sensitivity: Florida’s hot and humid weather can exacerbate pelvic pain and inflammation associated with endometriosis.
- Beach activities: Swimming and sunbathing, popular pastimes in Florida, may be uncomfortable or even painful for those with severe pelvic pain or bloating.
- Outdoor sports: Engaging in high-impact activities like running or tennis can be challenging due to pelvic discomfort and fatigue.
- Social events: Florida’s vibrant social scene may be difficult to enjoy fully when dealing with unpredictable pain and fatigue.
- Work-life balance: The state’s tourism and service industries often require long hours and physical stamina, which can be taxing for those managing endometriosis symptoms.
Recognizing the Signs of Endometriosis: A Comprehensive Symptom Checklist
Recognizing endometriosis can be difficult due to its wide range of symptoms. To help, here’s a comprehensive checklist of common endometriosis symptoms to watch for:
- Severe menstrual cramps
- Chronic pelvic pain
- Pain during or after sexual intercourse
- Heavy or irregular menstrual bleeding
- Painful bowel movements or urination, especially during menstruation
- Lower back pain
- Abdominal bloating
- Fatigue
- Nausea or vomiting
- Infertility or difficulty conceiving
- Diarrhea or constipation
- Mood swings or depression
- Leg pain
- Painful ovulation
- Chest pain or shortness of breath (in rare cases of thoracic endometriosis)
- Painful urination
It’s important to note that experiencing one or more of these symptoms doesn’t necessarily mean you have endometriosis. However, if you’re concerned about your symptoms, consulting with an endometriosis specialist in Florida can help you receive an accurate diagnosis and appropriate treatment plan.
The Florida Advantage: Cutting-Edge Endo Care Close to Home
Florida offers its residents and visitors a unique advantage regarding endometriosis care. The Sunshine State has become a hub for advanced medical treatments and research, providing women with access to top-tier care without requiring extensive travel. This section explores the benefits of seeking endometriosis treatment in Florida and highlights the state’s commitment to medical excellence in this field.
Access to Top-Tier Treatments and Research
Florida’s medical landscape is characterized by its commitment to innovation and cutting-edge treatments. For women with endometriosis, this translates to:
- Advanced Diagnostic Techniques: Florida’s leading medical centers utilize state-of-the-art imaging technologies, such as high-resolution ultrasounds and MRI scans, to accurately diagnose and stage endometriosis.
- Minimally Invasive Surgical Options: Some Florida specialists are trained in advanced laparoscopic and robotic surgical techniques, offering patients less invasive treatment options with shorter recovery times.
- Participation in Clinical Trials: Several Florida medical institutions actively participate in endometriosis research, allowing patients to access experimental treatments and contribute to scientific advancements.
- Multidisciplinary Approach: Some of Florida’s experts employ a team-based approach, bringing together gynecologists, general surgeons, urologists, pain specialists, fertility experts, and other relevant professionals to provide comprehensive care.
- Fertility Preservation Options: For women concerned about their future fertility, Florida offers advanced reproductive technologies and fertility preservation techniques alongside endometriosis treatment.
Top Endometriosis Specialists in Florida: Experts You Can Trust
Florida is home to some highly skilled and best endometriosis specialists dedicated to providing exceptional care for women struggling with this complex condition. These experts combine their extensive knowledge with cutting-edge techniques to offer personalized treatment plans that address each patient’s unique needs. In this section, we’ll highlight some of the leading endometriosis specialists in Florida and explore their areas of expertise.
Dr. Andrea Vidali is a renowned endometriosis specialist in Miami, Florida, and New York. With over two decades of experience in reproductive endocrinology and infertility, Dr. Vidali has gained international recognition for his expertise in minimally invasive surgical techniques for endometriosis treatment.
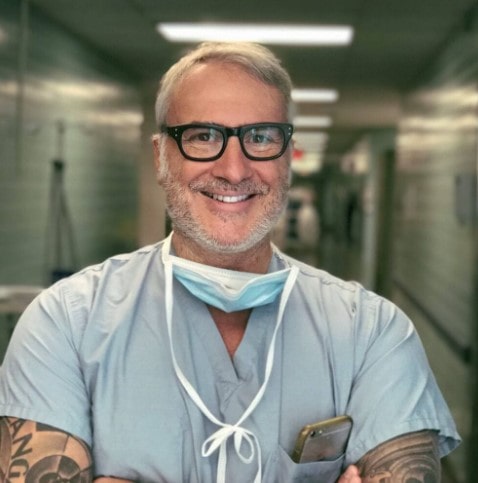
Key areas of expertise:
- Advanced excision surgery
- Fertility preservation in endometriosis patients
- Immunological aspects of endometriosis
- Robotic-assisted endometriosis surgery
Dr. Vidali’s approach focuses on thorough diagnosis and comprehensive treatment plans that address both pain management and fertility concerns. His patients benefit from his extensive experience in complex cases and his commitment to staying at the forefront of endometriosis research and treatment innovations.
Dr. Gaby Moawad is a highly respected gynecologist and endometriosis specialist in Orlando, Florida. Known for his patient-centered approach, he combines surgical expertise with a deep understanding of the holistic needs of women with endometriosis.

Areas of specialization:
- Laparoscopic and robotic excision of endometriosis
- Management of chronic pelvic pain
- Fertility-sparing endometriosis treatments
- Multidisciplinary approach to endometriosis care
Dr. Moawad’s practice emphasizes comprehensive care, addressing not only the physical symptoms of endometriosis but also the emotional and psychological aspects of living with a chronic condition. His patients appreciate his compassionate approach and dedication to improving their quality of life.
Finding the right endometriosis specialist in Florida takes time and research. Consultations offer a chance to discuss your case and assess the fit. Choosing the best specialist is key to managing your condition and improving your quality of life, as these experts understand the unique challenges women with endometriosis face in Florida.
Treatment Options: As Diverse as Florida’s Landscape
Just as Florida boasts a diverse landscape of beaches, swamps, and citrus groves, the treatment options for endometriosis in the state are equally varied and comprehensive. Florida’s endometriosis specialists offer a wide range of advanced surgical techniques, non-invasive therapies, and holistic approaches to address the complex needs of patients with this challenging condition. This section explores the diverse treatment landscape available to women seeking endometriosis care in Florida.
Advanced Surgical Techniques Available in Florida
Surgical intervention remains a cornerstone of endometriosis treatment, especially for severe cases or when conservative measures have failed. Florida’s top endometriosis specialists are skilled in various advanced surgical techniques:
- Laparoscopic Excision Surgery:
- A minimally invasive approach using small incisions
- Allows for thorough removal of endometrial implants
- Reduced scarring and faster recovery compared to open surgery
- Often considered the gold standard for endometriosis treatment
- Robotic-Assisted Surgery:
- Utilizes advanced robotic technology for enhanced precision
- Offers 3D visualization and improved dexterity for complex procedures
- Particularly useful for deep-infiltrating endometriosis
- Fertility-Preserving Surgery:
- Focuses on removing endometriosis while preserving reproductive organs
- Often combined with fertility treatments for women trying to conceive
- Presacral Neurectomy:
- Targets nerve pathways to alleviate chronic pelvic pain
- It can be performed alongside excision surgery for comprehensive treatment
- Hysterectomy with Bilateral Salpingo-Oophorectomy:
- Reserved for severe cases or when other treatments have failed
- Involves the removal of the uterus, fallopian tubes, and ovaries
- Considered a last resort due to its impact on fertility and hormonal balance
Non-Invasive Therapies and Holistic Approaches
Florida’s endometriosis specialists recognize the importance of non-surgical interventions and holistic care in managing the condition. Some common non-invasive therapies include:
- Hormonal Treatments:
- Birth control pills
- Progestin-only medications
- GnRH agonists and antagonists
- Aromatase inhibitors
- Pain Management Techniques:
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Nerve blocks
- Transcutaneous electrical nerve stimulation (TENS)
- Physical Therapy:
- Pelvic floor therapy
- Manual therapy techniques
- Exercise programs tailored for endometriosis patients
- Nutritional Counseling:
- Anti-inflammatory diets
- Elimination diets to identify food sensitivities
- Supplementation strategies
- Complementary Therapies:
- Acupuncture
- Yoga and mindfulness practices
- Herbal medicine under professional guidance
- Psychological Support:
- Cognitive-behavioral therapy
- Support groups
- Stress management techniques
Choosing the Right Treatment Plan
When considering endometriosis treatment options in Florida, working closely with your specialist to develop a personalized plan is essential. Factors to consider include:
- Severity and location of endometriosis lesions
- Primary symptoms and their impact on quality of life
- Fertility goals and reproductive health concerns
- Overall health and any coexisting conditions
- Personal preferences and lifestyle considerations
Florida endometriosis specialists offer comprehensive care through a multimodal approach. They combine surgery with noninvasive therapies to address physical and emotional symptoms. With diverse treatment options—from advanced surgery to holistic therapies—patients can access personalized care for effective management and improved quality of life.
Living with Endometriosis in Florida: Beyond Medical Care
Managing endometriosis extends far beyond the doctor’s office or operating room. For those living with this condition in Florida, finding ways to cope with symptoms and maintain a high quality of life is crucial. The Sunshine State’s unique environment and lifestyle offer challenges and opportunities for those navigating life with endometriosis. This section explores strategies for managing symptoms in Florida’s climate and lifestyle and the supportive therapies and resources available to endometriosis patients in the state.
Adapting to Florida’s Climate and Lifestyle
Florida’s warm, humid climate and active lifestyle can present unique challenges for women with endometriosis. Here are some strategies to help manage symptoms while enjoying all that the state has to offer:
- Heat Management:
- Use cooling products like portable fans or cooling towels when outdoors
- Plan outdoor activities for cooler parts of the day
- Stay hydrated to help regulate body temperature
- Beach-Friendly Strategies:
- Invest in comfortable, supportive swimwear
- Use beach umbrellas or tents for shade and privacy
- Bring a supportive cushion or beach chair for comfort
- Exercise Adaptations:
- Opt for low-impact activities like swimming or yoga
- Try water aerobics or beach walks for gentle exercise
- Listen to your body and pace yourself during physical activities
- Workplace Accommodations:
- Use ergonomic furniture to reduce pelvic strain
- Take regular breaks to stretch and move
- Communicate with employers about flexible work arrangements if needed
- Social Life Adjustments:
- Plan activities with built-in rest periods
- Choose venues with comfortable seating options
- Be open with friends about your needs and limitations
Supportive Therapies for Endometriosis Management
Florida offers many supportive therapies that can complement medical treatments and help manage endometriosis symptoms.
- Acupuncture:
- It may help reduce pain and inflammation
- It can be particularly beneficial for menstrual cramps and chronic pelvic pain
- Massage Therapy:
- It helps relax tense muscles and reduce overall body pain
- It may improve circulation and reduce stress
- Yoga and Pilates:
- Gentle stretching can help alleviate pelvic pain
- Mindfulness aspects can aid in stress reduction
- Nutritional Counseling:
- Guidance on anti-inflammatory diets
- Help in identifying and managing food sensitivities
- Pelvic Floor Physical Therapy:
- Addresses muscle tension and dysfunction in the pelvic area
- Can improve pain during intercourse and bladder/bowel symptoms
- Mindfulness and Meditation:
- Techniques for managing pain and reducing stress
- Can improve overall emotional well-being
Community Resources and Support Groups
Florida offers numerous resources and support groups for women living with endometriosis:
- Endometriosis Association of Florida:
- Provides education and support for patients and families
- Organizes regular meetups and events across the state
- Online Support Communities:
- Florida-specific Facebook groups and forums
- Virtual support meetings for those unable to attend in-person events
- Fertility Support Networks:
- Resources for women dealing with endometriosis-related infertility
- Connections to fertility specialists and treatment options in Florida
- Workplace Advocacy Groups:
- Organizations that help women navigate workplace challenges related to chronic illness
- Resources for understanding employment rights and accommodations
Lifestyle Modifications for Symptom Management
In addition to medical treatments and supportive therapies, certain lifestyle modifications can help manage endometriosis symptoms:
- Stress Reduction Techniques:
- Regular meditation or deep breathing exercises
- Engaging in hobbies or activities that promote relaxation
- Sleep Hygiene:
- Establishing a consistent sleep schedule
- Creating a comfortable sleep environment
- Dietary Adjustments:
- Keeping a food diary to identify trigger foods
- Incorporating anti-inflammatory foods into the diet
- Exercise Routine:
- Finding a balance between rest and gentle activity
- Incorporating low-impact exercises like swimming or cycling
- Emotional Well-being:
- Seeking counseling or therapy to address the emotional impact of living with a chronic condition
- Practicing self-compassion and setting realistic expectations
By using Florida’s resources and strategies, women with endometriosis can manage symptoms and maintain a fulfilling lifestyle. Remember, it’s a journey—be patient and celebrate small victories.
Conclusion: Empowering Your Endo Journey in the Sunshine State
As we conclude our exploration of endometriosis care in Florida, it’s clear that the Sunshine State offers a wealth of resources, expertise, and support for women navigating this challenging condition. From world-class specialists to cutting-edge treatments and supportive communities, Florida provides a comprehensive ecosystem for endometriosis management. We encourage you to take the next step in your endometriosis care journey. Whether that means scheduling a consultation with a specialist, exploring new treatment options, or connecting with a local support group, every action you take is a step towards better health and well-being.
Remember, your health journey is unique, and finding the right care may take time. Be patient with yourself, advocate for your needs, and don’t hesitate to seek second opinions or explore different treatment options. With perseverance and the right support, you can navigate the challenges of endometriosis and embrace all that life in Florida has to offer.
Here’s to your health, well-being, and a brighter, pain-free future in the Sunshine State!
REFERENCES:
https://ufhealth.org/conditions-and-treatments/endometriosis
https://www.medicalnewstoday.com/provider-near-me/condition-or-procedure/endometriosis/fl-florida
https://www.acibademhealthpoint.com/endometriosis-specialist-in-miami-expert-care
https://health.usf.edu/care/obgyn/services-specialties/endometriosis

Endometriosis Pain? Discover the Best OB-GYN Near You for Expert Care
Living with Endometriosis: Why Finding the Right OB-GYN Near You Matters
Living with endometriosis can be an overwhelming and isolating experience. Chronic pain, heavy periods, and potential fertility issues can significantly impact your quality of life. However, you don’t have to face this challenging condition alone. Finding a skilled and compassionate endometriosis OB-GYN near you who can make all the difference in managing your symptoms effectively and regaining control of your health.
In this comprehensive guide, we’ll explore the importance of seeking specialized care for endometriosis, how to identify the right OB-GYN in your area, and what to expect from treatment. Whether you’ve been diagnosed recently or have struggled with endometriosis for years, this article will empower you to take the next step toward finding relief and improving your overall well-being.
What Is Endometriosis and Why Your OB-GYN Matters
Endometriosis is a complex gynecological condition that affects millions of women worldwide. It occurs when tissue similar to the lining of the uterus grows outside the uterine cavity, commonly on the ovaries, fallopian tubes, and pelvic lining. This misplaced tissue responds to hormonal changes during the menstrual cycle, leading to inflammation, pain, and scar tissue formation.
The symptoms of endometriosis can vary widely from person to person but often include:

- Severe menstrual cramps that worsen over time
- Chronic pelvic pain
- Pain during or after sexual intercourse
- Heavy or irregular menstrual bleeding
- Painful bowel movements or urination during menstruation
- Fatigue and gastrointestinal issues
- Difficulty conceiving or infertility
Endometriosis is very complex. There is a general lack of knowledge and expertise among doctors, including OB-GYNs, in diagnosing and treating patients. Therefore, seeking care from an OB-GYN with specialized knowledge and experience in treating endometriosis is crucial. These experts are better equipped to provide accurate diagnoses, develop personalized treatment plans, and offer the latest advancements in endometriosis care.
How to Identify the Best OB-GYN Doctor for Endometriosis Near You
Finding the right OB-GYN doctor specializing in endometriosis requires research and consideration. You should use these strategies to locate the best specialist near you:
Utilize Online Resources and Directories
Several online platforms can help you find experienced endometriosis specialists in your area. One such resource is iCareBetter, a directory designed to connect patients with skilled endometriosis surgeons and specialists. This endometriosis specialist directory provides detailed information about the doctor’s experience, patient reviews, and areas of expertise.
Seek Referrals from Trusted Sources
Don’t hesitate to ask for recommendations from:
- Your primary care physician
- Your physical therapist, dietitian, yoga teacher, counselor, and nurses.
- Friends or family members who have dealt with endometriosis
- Local endometriosis support groups
- Online communities dedicated to endometriosis awareness and support
Research Credentials and Experience
When evaluating potential OB-GYNs, consider the following factors:
- Board certification in obstetrics and gynecology
- Additional fellowship training or specialization in minimally invasive GYN surgery and endometriosis, such as AAGL fellowship
- Years of experience treating endometriosis patients
- Membership in professional organizations focused on endometriosis research and treatment, such as AAGL
- Publications or involvement in clinical trials related to endometriosis
Read Patient Reviews and Testimonials
While individual experiences may vary, patient reviews can provide valuable insights into a doctor’s bedside manner, communication style, and overall patient satisfaction. Look for patterns in feedback and consider both positive and negative reviews to form a balanced perspective. You can read endometriosis-specific patient reviews on doctors’ profiles on iCareBetter.com.
Schedule Consultations
Many OB-GYNs offer initial consultations to discuss your symptoms and concerns. This is an excellent opportunity to assess their approach to endometriosis care and determine if you feel comfortable with their communication style and treatment philosophy.
Comprehensive Treatment Approaches Offered by Endometriosis Specialists
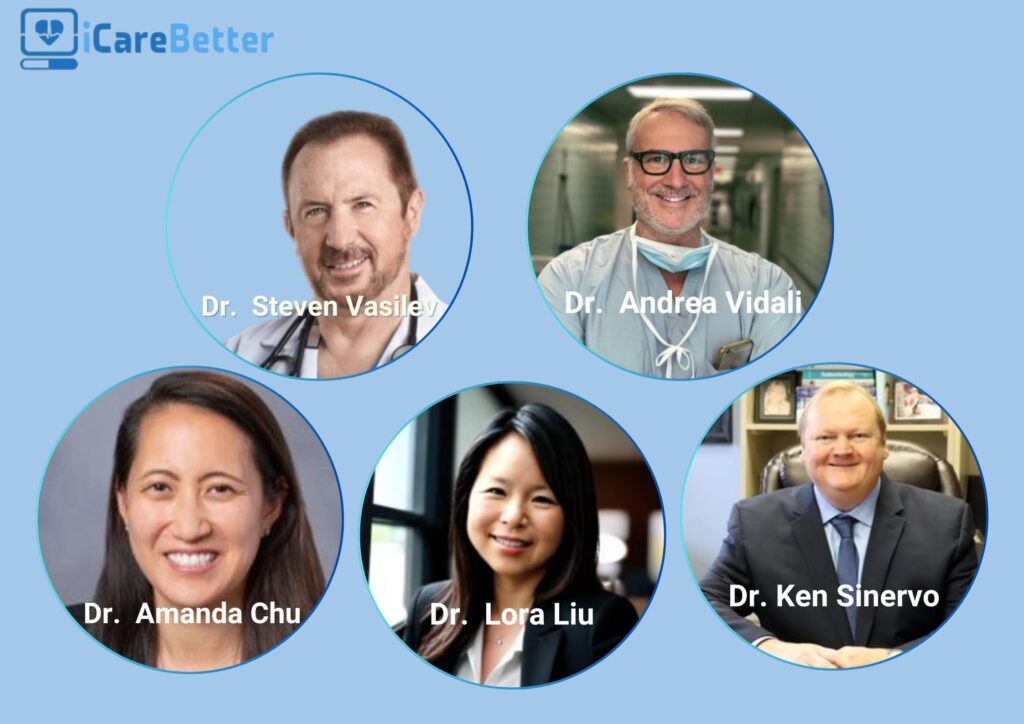
Experienced OB-GYNs specializing in endometriosis recognize that every patient’s journey is unique and requires a personalized treatment approach. Top-tier endometriosis surgeons offer multidisciplinary surgery and care. These experts include Dr. Andrea Vidali, Dr. Steven Vasilev, Dr. Amanda Chu, Dr. Lora Liu, Dr. Ken Sinervo, and many more surgeons who, in total, add up to about one hundred experts in the US. Here are some of the most common approaches used by endometriosis specialists:
Pain Management Strategies
Managing chronic pain is often a top priority for endometriosis patients. Endometriosis surgeons may recommend a combination of:
- Surgery
- Over-the-counter pain relievers (NSAIDs)
- Prescription pain medications
- Physical therapy and pelvic floor exercises
- Alternative therapies such as acupuncture or mindfulness techniques
Hormonal Therapies
Hormonal treatments aim to temporarily manage endometriosis symptoms or regulate your hormones before and after surgery. Options may include:
- Combined oral contraceptives
- Progestin-only medications
- Gonadotropin-releasing hormone (GnRH) agonists or antagonists
- Aromatase inhibitors
Minimal Invasive Surgical Procedures
Surgical intervention may be necessary for more severe cases or when conservative treatments are ineffective. Skilled endometriosis specialists often employ advanced laparoscopic techniques to:
- Remove endometrial implants and scar tissue
- Restore normal pelvic anatomy
- Preserve fertility when possible
Integrative and Holistic Approaches
Many endometriosis specialists recognize the benefits of combining conventional surgical and medical treatments with complementary therapies. These may include:
- Nutritional counseling and anti-inflammatory diets
- Stress reduction techniques
- Pelvic floor physical therapy
- Cognitive-behavioral therapy for pain management
- Pain management by pain specialists or acupuncturists
Fertility Preservation and Treatment
For patients concerned about their fertility, endometriosis specialists work closely with you to develop strategies for preserving and enhancing fertility. This may involve:
- Fertility-sparing surgical techniques
- Ovarian stimulation and egg-freezing
- In vitro fertilization (IVF) when necessary
- Egg preservation before surgery
The Benefits of Early Intervention by a Skilled OB-GYN
Seeking care from an experienced endometriosis specialist near you as early as possible can have numerous benefits for your overall health and quality of life.
- Accurate and timely diagnosis: Endometriosis can be challenging to diagnose, and patients may need about 10 years to receive a firm diagnosis. However, specialists are trained to recognize subtle signs and symptoms that general practitioners may overlook.
- Preventing disease progression: Early intervention can help slow the growth of endometriosis implants and minimize the formation of scar tissue, potentially preserving fertility and reducing long-term complications.
- Tailored treatment plans: Specialists can develop personalized treatment strategies that address your specific symptoms, concerns, and goals.
- Improved pain management: Early intervention can improve pain control and reduce the need for more invasive treatments in the future.
- Enhanced fertility outcomes: For those hoping to conceive, early treatment can help preserve fertility and improve the chances of a successful pregnancy.
- Better overall quality of life: By addressing symptoms early on, you can minimize the impact of endometriosis on your daily activities, relationships, and emotional well-being.
Why Proximity Matters in Choosing an Endometriosis Specialist Near You
When dealing with a chronic condition like endometriosis, having a trusted healthcare provider close to home can make a significant difference in your overall treatment experience and outcomes. Here are some key reasons why proximity matters when choosing an OB-GYN for endometriosis care:
- Convenience and accessibility: Check-ups and follow-up appointments are essential for effectively managing endometriosis. Having a specialist nearby reduces travel time and makes it easier to maintain consistent care.
- Timely intervention: In case of flare-ups or emergencies, being able to quickly reach your OB-GYN can provide peace of mind and ensure prompt medical attention.
- Familiarity with local resources: A local specialist is likely to have established relationships with other healthcare providers in the area, facilitating seamless referrals for additional treatments or support services if needed.
- Community support: Choosing a local OB-GYN may connect you with other patients in your area, fostering a sense of community and shared experiences.
- Continuity of care: Building a long-term relationship with a nearby specialist allows for more personalized and comprehensive care over time.
Start your search today with terms like “endometriosis OB-GYN near me” to find a trusted expert in your area who can provide personalized, timely care. However, because of a significant shortage of skilled endometriosis experts, with an estimated 100 experts in the US, you might end up traveling. In that case, virtual visits will be your best friend.
FAQs About Seeing an Endometriosis OB-GYN Near You
Once you’ve found an OB-GYN specializing in endometriosis, preparing for your initial consultation is important. Here are some tips to help you make the most of your appointment:
- Keep a symptom diary: Record your symptoms, their frequency, and severity in the weeks leading up to your appointment. This information can help your doctor better understand your condition.
- Gather your medical history: Compile a list of any previous diagnoses, treatments, and surgeries related to your pelvic pain and reproductive health.
- Bring relevant medical records: If you’ve had imaging studies or lab tests done previously, bring copies of the results to your appointment.
- Prepare a list of questions: Write down any concerns or questions you have about your symptoms, diagnosis, or treatment options.
- Consider bringing a support person: Having a friend or family member with you can provide emotional support and help you remember important information discussed during the appointment.
Essential Questions to Ask Your Endometriosis Specialist
During your consultation, don’t hesitate to ask questions that will help you better understand your condition and treatment options. Some important endometriosis FAQs to consider:
- What stage of endometriosis do you suspect I have, and how can we confirm the diagnosis?
- What treatment options do you recommend for my specific case, and why?
- What are the potential side effects or risks associated with each treatment option?
- How will the recommended treatments affect my fertility?
- Are there any lifestyle changes or complementary therapies you suggest to help manage my symptoms?
- What is your experience with treating endometriosis, and how many similar cases have you handled?
- How often should I schedule follow-up appointments, and what signs should prompt me to contact you between visits?
- Are there any clinical trials or new treatments for endometriosis that I might be eligible for?
Understanding Insurance Coverage for Endometriosis Treatment
Navigating insurance coverage for endometriosis treatment can be complex. Here are some key points to keep in mind:
- Most health insurance plans cover diagnostic tests and basic treatments for endometriosis.
- Coverage for more advanced treatments, such as laparoscopic surgery or fertility treatments, may vary depending on your specific plan and the specialist you plan to visit.
- Some insurance providers may require a referral from your primary care physician before covering specialist visits.
- Certain treatments, like experimental therapies or some complementary approaches, may not be covered by insurance.
It is essential to review your insurance policy and contact your provider to understand your coverage details. Your chosen OB-GYN’s office may also be able to assist you in determining coverage and obtaining necessary pre-authorizations for treatment.
Taking the Next Step: Finding Relief with the Right OB-GYN
Living with endometriosis can be challenging, but with the right care and support, you can manage your symptoms effectively and improve your quality of life. By seeking out a skilled OB-GYN who specializes in endometriosis, you’re taking a crucial step towards better health and well-being.
Remember, you don’t have to face this journey alone. Reach out to local support groups, connect with online communities, and most importantly, don’t hesitate to seek professional help. With the guidance of an experienced endometriosis specialist, you can develop a personalized treatment plan that addresses your unique needs and goals.
Take action today to find the best endometriosis OB-GYN near you. Use online resources like iCareBetter, ask for referrals and schedule consultations to find the right specialist who can provide the comprehensive care you deserve. Your path to relief and improved health begins with finding the right healthcare partner. Don’t wait—visit iCareBetter to find the best endometriosis OB-GYN near you today and reclaim your health!
References:
https://www.northwell.edu/obstetrics-and-gynecology/conditions/endometriosis
https://www.brighamandwomens.org/obgyn/resources/endometriosis-treatment
https://www.medifind.com/conditions/endometriosis/1797/doctors
https://www.woosterhospital.org/exploring-nearby-endometriosis-treatment-options

How to Become an Endometriosis Expert: Training Path
Table of contents
Due to the condition’s complexity and growing awareness, doctors who can diagnose and treat endometriosis are in high demand. To provide efficient patient care, doctors must complete advanced medical education and develop surgical expertise. These specialists need extensive training to handle this challenging condition.
Becoming an endometriosis specialist requires meeting strict standards. Experts must excel in advanced training courses and perfect their surgical techniques. They also need to keep up with new diagnostic methods and treatment options. This piece outlines the essential steps doctors should take to become recognized experts in endometriosis care.
Educational Requirements for Endometriosis Expertise
To become experts in endometriosis, specialists need extensive training and specialized education beyond standard qualifications. This helps practitioners become skilled at specific techniques and procedures.
Medical degree and gynecology specialization
Endometriosis expertise starts with medical school completion and obstetric gynecology specialization. Doctors need a complete understanding of reproductive medicine and pelvic health conditions. Not all gynecologists have advanced training to work with endometriosis, so specialists need extra intense training to manage it efficiently.
Advanced training in endometriosis diagnosis and treatment
Advanced training helps doctors become skilled in multiple aspects of endometriosis care. The complete training model has the following:
- Diagnostic imaging techniques and interpretation
- Surgical management of the disease
- Hormonal treatment protocols
- Pain management strategies
- Reproductive medicine expertise
- Psychosomatic medicine understanding
- Post-surgical treatment planning
Specialists must complete training at certified endometriosis centers. They work directly with patients and learn different treatment approaches. This specialized training prepares doctors to deliver complete care to their patients.
Surgical skills development
Surgical expertise is crucial for endometriosis specialists. Training programs must help doctors become skilled at laparoscopic or robotic excision of endometriosis. Surgeons need to develop proficiency in several specific techniques.
Advanced Surgical Skills:
- Surgical preparation by imaging studies
- Comprehensive assessment of the pelvic and abdominal organs during the surgery
- Removal of deep infiltrating endometriosis
- Parametrial dissection techniques
- Ureterolysis and ureteral procedures
- Rectal surgery techniques
- Nerve-sparing deep pelvic preparation
- Endometriomas
- Recto-vaginal septum endometriosis
Surgical training combines simulation-based learning with supervised practical experience. Specialists enhance their skills through workshops and specialized courses. At the end of their training, doctors must excel in minimally invasive surgical techniques for removing endometriosis lesions.
Critical Components of Endometriosis Training
Healthcare providers need training in specialized areas to become skilled at endometriosis care. These professionals must build their expertise in diagnostic and treatment approaches that work for better patient outcomes.
Diagnostic techniques (clinical examination, imaging, surgery)
Medical professionals need several examination methods to diagnose accurately. Laparoscopic visualization with histological confirmation remains the gold standard for diagnosis. Healthcare specialists should become skilled at the following:
- Transvaginal ultrasound (TVUS) – This method shows 93% sensitivity and 96% specificity when detecting endometriomas.
- Magnetic Resonance Imaging (MRI): This technique demonstrates 90-92% sensitivity and 91-98% specificity in identifying lesions.
- Laparoscopic examination – This procedure enables direct visualization and allows doctors to perform biopsies.
Medical management approaches
Medical management training emphasizes hormonal therapies and pain management protocols. Endometriosis specialists master several treatment options. Doctors must carefully monitor their patients’ responses and side effects.
Surgical techniques for different types of endometriosis
Surgical expertise includes procedures that doctors customize for each unique case. Doctors need to master both conservative and advanced surgical techniques. They must pay special attention to profoundly infiltrating endometriosis (DIE), which requires specialized surgical approaches.
Fertility preservation and reproductive medicine
Medical specialists need substantial training in fertility preservation because endometriosis affects a woman’s ability to conceive.
Completing required training
Doctors must complete specialized training at certified endometriosis centers to meet certification requirements. This training allows them to work with a variety of cases. The training process helps practitioners:
- Learn comprehensive surgical skills for removal of endometriosis lesions regardless of location and depth
- Become skilled at ultrasound techniques and interpretation
- Develop expertise in MRI interpretation
- Learn pain management protocols
- Study hormonal treatment options
Maintaining proficiency through continuing education
Ongoing Education Requirements: Medical and surgical proficiency just needs continuous professional development. Specialists must participate in educational activities to stay current with advancing medical knowledge. The continuing education process has:
- Participating in specialized workshops and masterclasses
- Attending professional conferences
- Engaging in clinical research
- Completing required continuing medical education (CME) credits
- Tracking certification maintenance through learning portals
Building Expertise Through Clinical Experience
Clinical experience is the lifeblood of expertise in endometriosis treatment. Medical professionals need hands-on practice and must learn continuously from all professional channels.
Working at specialized endometriosis centers
Specialized centers deliver complete care through teams of medical professionals. These teams include gynecologic surgeons, urologists, general surgeons, physical therapists, pain experts, fertility doctors, dietitians, and psychologists. Practitioners get unique opportunities to handle complex cases while working with experienced experts. Research shows that patient outcomes improve and complication rates decrease when surgeons perform endometriosis surgeries with a high volume of cases.
Attending conferences and workshops
Endometriosis experts enhance their expertise by participating in major international conferences. Key events include:
- AAGL annual conference
- World Congress on Endometriosis
- European Endometriosis Congress
- ESHRE Annual Meetings
- ASRM Annual Congress
These scientific gatherings offer insights into molecular fingerprints, complex surgery techniques, and emerging treatment approaches. Experts can find learning opportunities throughout the year at conferences worldwide.
Networking with other endometriosis specialists
Through these connections, specialists can:
- Share clinical experiences
- Work together on research projects
- Mentor younger members
- Promote high standards of ethical investigation
Conclusion
Doctors need thorough education, specialized training, and hands-on experience to become skilled at treating endometriosis. Their path requires expertise in advanced diagnostic techniques, surgical procedures, and medical management strategies. These specialists must show proficiency in multiple disciplines, from reproductive medicine to pain management, and stay updated with emerging treatment approaches.
Specialists can improve their endometriosis care through certification programs, clinical research, and professional networking. Time invested in specialized centers combined with participation in international conferences and professional networks helps doctors become pioneering experts in endometriosis treatment. This dedication benefits patient care through better diagnostic accuracy, improved treatment outcomes, and higher quality care for this complex condition.

Can Ureteral Endometriosis Cause Kidney Shooting Back Pain?
Endometriosis is a common gynecological condition that affects many women during their reproductive years. While it typically manifests in the pelvic region, in some instances, it may invade other organs, including the urinary system. This article explores the question: Can endometriosis on the ureter cause kidney shooting back pain?
Table of contents
About Endometriosis
Endometriosis is a chronic disease characterized by the presence of endometrial-like tissue outside the womb. This could include the ovaries, fallopian tubes, and the lining of the pelvic cavity. In some extreme cases, endometrial tissue may also affect organs outside the pelvic cavity, such as the bladder, bowel, or kidneys.
Read More: Understanding Endometriosis: Unveiling the Common Symptoms and Their Impact
Understanding Ureteral Endometriosis
Ureteral endometriosis is an uncommon manifestation of the disease, accounting for about 1% of all endometriosis cases. It involves the ureters, the tubes that transport urine from the kidneys to the bladder. This condition can lead to urinary tract obstruction, resulting in hydronephrosis, which is the swelling of a kidney due to a build-up of urine.
The Kidney-Endometriosis Connection
The kidneys can be impacted when one or both of the ureters become affected by endometriosis. The section of the ureter that is usually affected sits below the pelvic area.
Symptoms of Kidney Endometriosis
Kidney endometriosis can be asymptomatic for several years. If a person who has undergone surgery to treat endometriosis has ongoing urinary problems such as pain and infections, it may suggest the presence of urinary tract or kidney endometriosis. Symptoms may include:
- Pain in the lower back that gets worse with a monthly menstrual cycle. That pain can also extend down through the legs.
- Blood in the urine that can co-occur with the menstrual cycle
- Difficulty urinating
- Recurrent urinary tract infections
Read More: Understanding How Endometriosis Can Cause
Diagnosis of Ureteral Endometriosis
The diagnosis of ureteral endometriosis relies heavily on clinical suspicion. As a result, they often misdiagnose patients with kidney cancer. This can lead to patients not receiving treatment on time, or receiving the wrong kind of treatment.
Read More: Life After Endometriosis Surgery: A Comprehensive Guide
Treatment Options
Kidney endometriosis can lead to kidney damage and even kidney failure if left untreated. However, the best approach is to treat the condition by removing endometriosis lesions with minimally invasive laparoscopic surgery.
The Silent Threat of Kidney Failure
One of the most concerning aspects of ureteral endometriosis is the silent threat of kidney failure. It is estimated that as many as 25% to 50% of nephrons are lost when there is evidence of ureteral endometriosis, and 30% of patients will have reduced kidney function at the time of diagnosis.
Impact on Kidney Health
The good news is that if one kidney isn’t functioning due to endometriosis, you can survive on the other kidney. So, if you find out you only have one fully-functioning kidney, it’s essential to take care of it.
Conclusion
In conclusion, while endometriosis is typically a pelvic condition, it can venture beyond and affect the urinary system, including the kidneys. This can lead to severe complications, including kidney failure. Therefore, it’s crucial for women with endometriosis to be aware of the potential symptoms and seek medical advice if they experience any signs of kidney problems. The early detection and treatment of ureteral endometriosis are crucial to preserving kidney function and overall health.
References:
https://drseckin.com/kidney-endometriosis/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3535807/
Endometriosis: Perilous impact on kidneys
https://endometriosis.net/clinical/silent-kidney-failure

How to Treat Bowel Endometriosis: A Comprehensive Guide
Bowel endometriosis, a complex and severe variant of endometriosis, is a condition best navigated with a deep understanding of its details. This guide aims to shed light on the various aspects of bowel endometriosis, from its origins to symptoms, diagnostic approaches, and treatment options, to empower those affected.
Table of contents
What is Bowel Endometriosis?
Endometriosis, a chronic health disorder predominantly affecting women in their reproductive years, is characterized by the growth of endometrial-like tissue, which usually lines the uterus in regions outside the uterus. This misplaced tissue prompts an inflammatory reaction, leading to distressing symptoms. When this aberrant tissue growth takes place on or inside the bowels, the condition is referred to as bowel endometriosis.
How Common is Bowel Endometriosis?
While the exact prevalence of bowel endometriosis remains uncertain, it’s estimated to occur in 5-15% of all endometriosis cases. Predominantly, it manifests on the rectum or sigmoid colon but can also affect the appendix or small intestine.
Read More: https://icarebetter.com/endometriosis-and-inflammatory-bowel-disease-distinguishing-the-differences/
Recognizing the Symptoms
Symptoms of bowel endometriosis may not always be apparent, especially in the early stages of the disease. However, as the condition progresses, women may experience discomfort associated with their menstrual cycle, sexual intercourse, bowel movements, and even infertility.
Symptoms commonly associated with bowel endometriosis include:
- Painful Bowel Movements: This is often accompanied by constipation or diarrhea.
- Rectal Bleeding: This symptom, which is more uncommon, usually occurs during menstruation.
- Infertility: Some women may experience difficulty conceiving.
- Pelvic Pain: Chronic pelvic pain is a common symptom associated with endometriosis, often more severe during menstruation or ovulation.
- Painful Intercourse: This is often due to the endometriosis lesion causing a distortion of the pelvic anatomy.
It’s important to note that bowel endometriosis can sometimes mimic symptoms of other gastrointestinal conditions, like irritable bowel syndrome (IBS), making it challenging to diagnose.
Diagnosing Bowel Endometriosis
A comprehensive diagnosis of bowel endometriosis usually involves a combination of physical examination, medical history analysis, and advanced imaging techniques. The diagnostic process may include:
- Physical Examination: This includes a manual check for growths in the rectum or vagina.
- Imaging Tests: These can include ultrasound, MRI, colonoscopy, and barium enema.
- Laparoscopy: This surgical procedure is considered the gold standard for diagnosing endometriosis, as it allows for visual examination of the uterus, ovaries, and other pelvic structures. And surgeons can take samples for histopathology evaluations.
Read More: Understanding Bowel Endometriosis
Treating Bowel Endometriosis: An Overview
Treatment for bowel endometriosis is complex and multifaceted. It requires a personalized approach, taking into account the severity of the disease, the patient’s age, fertility goals, and personal preferences. The primary treatment options include:
- Hormonal Therapy: This involves medications that control estrogen levels, which can influence the progression of endometriosis. These medications can help manage pain and other symptoms.
- Pain Management: Over-the-counter or prescription nonsteroidal anti-inflammatory drugs (NSAIDs) may be recommended to help alleviate pain.
- Surgery: Surgical interventions aim to remove as much endometrial tissue as possible while preserving organ function.
Surgical Treatment Options
Surgery is typically the primary treatment for bowel endometriosis, particularly for severe cases. The goal of surgery is to remove endometrial implants without compromising the functionality of the organs involved. There are three main surgical options:
- Segmental Bowel Resection: This involves removing the section of the bowel affected by endometriosis and reconnecting the healthy portions. This option is often recommended for larger areas of endometriosis.
- Rectal Shaving: This procedure involves shaving off the endometriosis from the top of the bowel without removing any portion of the intestines. It’s often used for smaller areas of endometriosis.
- Disc Resection: In this procedure, a surgeon cuts out a small disk where the endometriosis lesions appear and then closes the remaining hole.
Understanding the Risks of Surgery
Surgery for bowel endometriosis is a complex procedure associated with certain risks. These can include short-term complications such as infection, leakage of bowel content during the postoperative healing phase, peritonitis, and septicaemia. Long-term risks might include bowel dysfunction, characterized by frequency, urgency, and incontinence.
Read More: Finding an Excision Specialist: What you Need to Know
Hormone Treatment Options
Although hormonal treatments cannot halt the progression of endometriosis, they can help manage symptoms. Hormonal treatments for bowel endometriosis can include birth control pills, progestin injections, or, less favorably, gonadotropin-releasing hormone (GnRH) agonists.
Read more: What are the long-term side effects of Lupron?
Managing Symptoms and Quality of Life
Bowel endometriosis can significantly impact the quality of life of those affected. However, with appropriate treatment and management strategies, many women affected by this condition can lead fulfilling lives. Communication with your healthcare team, lifestyle modifications, and psychological support can all contribute to improving the quality of life.
Conclusion
Understanding how to treat bowel endometriosis is crucial for managing this complex and often painful condition. With the right approach, it’s possible to mitigate symptoms, improve fertility outcomes, and enhance the quality of life for those affected. If you suspect you have bowel endometriosis, it’s important to speak with a healthcare provider who can guide you through the diagnostic process and treatment options. With the right knowledge and resources, you can navigate this challenging condition and find a path to improved health and well-being.
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4229526/
https://weillcornell.org/news/what-is-bowel-endometriosis
https://www.webmd.com/women/endometriosis/bowel-endometriosis
https://www.healthline.com/health/womens-health/bowel-endometriosis
Understanding How Endometriosis Can Cause Bowel Problems
Endometriosis, a common health concern among women, can manifest itself in various ways, one of them being bowel problems. But how exactly can endometriosis cause bowel problems? This article will take you through the intricate connection between endometriosis and bowel problems, the symptoms to look out for, diagnostic procedures, and potential treatments.
Table of contents
What is Endometriosis?
Endometriosis is a health condition where the tissue similar to the type that lines the uterus, known as the endometrium, grows outside the uterus. This condition predominantly affects the reproductive organs such as the ovaries, fallopian tubes, and the external part of the uterus. However, it can also extend to other parts of the body including the bowels, rectum, and other pelvic organs.
Understanding Bowel Endometriosis
Bowel endometriosis is a form of endometriosis that affects the gastrointestinal tract, specifically the bowels. It can appear in two forms: superficial (on the surface of the bowel) and deep (penetrating the bowel wall).
Read More: Understanding Bowel Endometriosis
Symptoms of Bowel Endometriosis
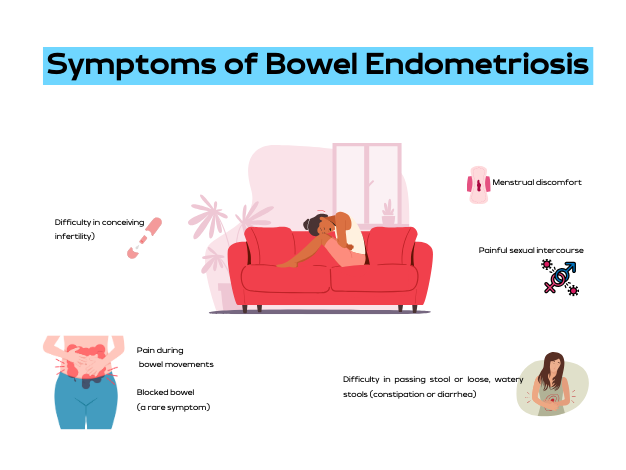
The symptoms of bowel endometriosis can vary widely depending on the location of the lesion, its size, and how deep it is in the bowel wall. Some women may experience no symptoms. However, common symptoms include:
- Difficulty in passing stool or loose, watery stools (constipation or diarrhea)
- Pain during bowel movements
- Menstrual discomfort
- Painful sexual intercourse
- Difficulty in conceiving (infertility)
- Blocked bowel (a rare symptom)
It is noteworthy that these symptoms can often mimic other conditions like irritable bowel syndrome (IBS), but the two conditions are distinct. One distinguishing factor is that with bowel endometriosis, symptoms often worsen before and during the menstrual period.
Read More: Endometriosis and Painful Intercourse: Is it Really Just Endometriosis?
Causes of Bowel Endometriosis
The exact cause of bowel endometriosis is still under study. However, several factors have been linked to its occurrence. These include genetic predisposition, inflammation, and levels of estrogen, a female sex hormone.
The Prevalence of Endometriosis
Endometriosis affects approximately 10%-12% of women of childbearing age. The condition is often diagnosed in women who are in their 30s, although it can occur at any age.
Diagnosing Bowel Endometriosis
The diagnosis of bowel endometriosis starts with the doctor asking about your symptoms and medical history, followed by a physical examination of your pelvic area. The doctor may also recommend imaging tests to get more information on the location and size of any cysts or tissue damage related to endometriosis. These tests include:
- Transvaginal or transrectal ultrasound: This procedure involves the insertion of a wand-like device into your vagina or rectum. This device releases sound waves that create images of your organs.
- Magnetic resonance imaging (MRI): An MRI test provides detailed images of your organs and tissues using a magnetic field and radio waves.
- Laparoscopy: This surgical procedure involves making a small incision near your belly button and inserting a thin viewing tool called a laparoscope.
- Barium enema: This type of X-ray is used to see changes or defects in your large intestine (colon).
- Colonoscopy: They pass a tube with a camera on its tip through the anus into the colon to directly visualize the wall and take samples from inside the colon.
Read More: Colon Chronicles: Delving into Bowel Endometriosis
Treating Bowel Endometriosis
The treatment plan for bowel endometriosis will be personalized, taking into account your symptoms, medical history, age, and reproductive plans. Treatments can include:
- Surgery: The aim of surgery is to remove as many lesions as possible while preserving your organs and overall health.
- Hormone treatments: These medications control estrogen levels which can worsen the symptoms of bowel endometriosis.
- Counseling: Given the ongoing nature of bowel endometriosis and its impact on both physical and mental health, counseling may be recommended to provide emotional support.
The Prognosis for Bowel Endometriosis
There is currently no cure for endometriosis. However, treatments like surgery and hormone therapy can help manage the symptoms. It is also important to note that symptoms could return if treatment is halted, or they could recur on their own, especially in cases with deep lesions.
Endometriosis is a complex condition that can cause bowel problems and other health issues. If you suspect you have endometriosis and are experiencing bowel problems, it’s important to consult with a healthcare provider. Early diagnosis and treatment can help manage symptoms and improve your quality of life.
References:
https://www.webmd.com/women/endometriosis/bowel-endometriosis
https://www.endometriosis-uk.org/endometriosis-and-bowel
https://www.endofound.org/gastrointestinal-distress
ENDOMETRIOSIS AND CONSTIPATION

Through the Looking Glass: Reflecting on 2023
Embarking on the journey of self-reflection is not just a personal endeavor; for us at iCareBetter, it’s a collective celebration of progress, community, and collaboration. As we bid farewell to 2023, a year marked by challenges and triumphs, it’s time to take a look into the past year and reflect on all that has been accomplished. Join us as we navigate through the areas of growth, community involvement, projects, and meaningful collaborations that shaped our year. In this special blog post, we’re excited to share the insights gained from our podcast endeavors and offer a sneak peek into the thrilling developments that await us in 2024. Let’s rewind, recap, and anticipate the exciting narrative that continues to unfold in the ever-evolving story of iCareBetter.
About iCareBetter
iCareBetter is an innovative platform dedicated to helping patients with endometriosis and chronic pelvic pain find compassionate and skilled experts. All experts on iCareBetter have shown knowledge and expertise in the treatment of endometriosis and chronic pelvic pain.
Vision
Our vision is to reduce the symptom-to-effective treatment of endometriosis to less than a year. Studies show that patients with endometriosis spend an average of 7.5 years to have an official diagnosis. Moreover, even after the diagnosis, patients will have to spend several years with multiple failed treatment attempts. After the long delays in diagnosis and treatment, they might be lucky enough to receive effective treatment from an expert.
Mission
Our mission is to improve access to high-quality specialized care for those with endometriosis. iCareBetter wants to combat the issue of patients living in confusion, pain, and isolation. To that end, we hope to connect as many patients to the right experts as early as possible. And we hope that this will ensure timely diagnosis and effective treatment.
To read more about why iCareBetter was built and the inspiration behind it, check out our blog here and listen to episode 1 of the podcast here, where Saeid and Jandra give you a behind the scenes look into what inspired them.
What happened in 2023?
In 2023, iCareBetter grew in many ways, including new avenues to provide education along with collaboration from the community. Here are some of the highlights!
- We started a podcast! iCareBetter: Endometriosis Unplugged is hosted by Jandra Mueller, DPT, MS a pelvic floor physical therapist and endometriosis patient. The podcast is available on Spotify, Apple Podcasts, and Youtube.
- We had 19 weekly episodes in season one
- Listeners joined from all over the world, reaching 22 countries
- We brought on a team to help with new content on social media creating a more visually appealing platform, community engagement, and followers.
- We now have 211 providers on our website available and ready to help those suffering from endometriosis and we are continuing to grow!
- Our blog content is now consistent with twice weekly posts bringing you updates on all things endometriosis.
What To Expect in 2024
While 2023 was a big year for iCareBetter, we hope to continue the growth and expand our providers across the globe. Our hope is to increase our collaboration with medical specialists, researchers, and advocates. There are some exciting things to come in 2024 including a new season of iCareBetter: Endometriosis Unplugged as well as some other projects that will be announced in 2024.
We hope you have found our resources helpful either for yourself or a loved one, and hope you continue to share the love and spread the word about Endometriosis. All of us here at iCareBetter wish you a safe and happy new year.

Cheers to 2024!
Do you or a loved one have Endometriosis? Here are some blogs that may help you get started on your journey.
- Endometriosis Signs and Symptoms: Everything You Need to Know
- Endometriosis Facts & Myths: Dispelling the Misconceptions

Endometriosis Guidelines: A Closer Look at a Potential Source of Confusion in Treatment (Part 2)
Table of contents
Understanding Endometriosis Treatment Confusion
Endometriosis affects millions of women worldwide, presenting with pain, irregular menstruation, and infertility. To shed light on the most effective treatment methods, this article is Part 2 in our series on this topic. It summarizes and comments on the findings from a recent 2021 review which provided a detailed analysis of various endometriosis treatment global guidelines as of September 2020.
There are often some discrepancies between guidelines for any disease. However, for endometriosis, a prior review in 2018 revealed that only about 7% of recommendations were comparable between international guidelines. Up to 28% of the recommendations were not supported by good research evidence at all. This helps explain why there is such a wide variation between doctors’ recommendations in clinical practice.
Key Guidelines reviewed in the most recent publication were:
- American College of Obstetricians and Gynecologists (ACOG)–reviewed in our last post, which you can read HERE
- Society of Obstetricians and Gynaecologists of Canada (SOGC)
- European Society of Human Reproduction and Embryology (ESHRE)
- Australian National Endometriosis Clinical and Scientific Trials (ACCESS)
- Royal College of Obstetricians and Gynaecologists (RCOG)
- French National College of Gynecologists and Obstetricians (CNGOF)
- American Association of Gynecologic Laparoscopists (AAGL)
- German Society for Gynecology and Obstetrics (DGGG)
Summary Review of Treatment Recommendations
- Non-Hormonal Medical Pain Management
- Nonsteroidal anti-inflammatory drugs (NSAIDs): While this is considered by all guidelines to be first-line therapy for dysmenorrhea and acyclic pelvic pain, it is not specific for endometriosis. A diagnosis and targeted therapy is more prudent since a large review showed no difference in effectiveness between NSAIDs and placebo.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): While this is considered by all guidelines to be first-line therapy for dysmenorrhea and acyclic pelvic pain, it is not specific for endometriosis. A diagnosis and targeted therapy is more prudent since a large review showed no difference in effectiveness between NSAIDs and placebo.
- Hormonal Treatment Options:
- Progestins and Combined Oral Contraceptives (COCs): Widely recommended for initial pain management. Specific formulations and dosages vary across guidelines. Of interest, there is little mention of compounded micronized progesterone which is hard to study but may deserve a place in the conversation. The Levonorgestrel Intrauterine System (LNG-IUS) is particularly noted for its localized progestin delivery, reducing systemic side effects and effectively managing pain.
- Megace (Megestrol Acetate): A potent progestin recommended by several guidelines but varies as a first-line vs second-line option. The additional benefit is less bone loss than that seen with GnRH agonist therapy.
- GnRH Agonists: Uniformly recommended in all guidelines for severe symptoms after first-line therapy; potential side effects, which can be long-lasting, include decreased bone density and menopausal-like symptoms. Add-back low-dose estrogen therapy can reduce symptoms. Most guidelines, and the FDA, recommend durations of 6 months or less.
- Emerging Hormonal Therapies: GnRH antagonists are gaining attention for their rapid onset of action and fewer side effects compared to agonists. The evidence is not conclusive.
- Danazol and Gestrinone: Older treatments with androgenic effects, are less commonly used today due to side effects. Gestrinone is not currently available in the United States.
- Selective Estrogen Receptor Modulators (SERMs) and Selective Progesterone Receptor Modulators (SPRMs) are emerging options being explored for their targeted action and potential benefits.
- Aromatase Inhibitors: Considered in some cases, especially for pain unresponsive to other treatments. Most guidelines agree that this is a possible second-line option, but the evidence is not conclusive. A possible niche for effective use may be in post-menopausal patients who have endo.
- Surgical Approaches: Navigating the Complexities
- Laparoscopic Surgery: Endorsed for its efficacy and reduced recovery time, compared to big incision (laparotomy) surgery. However, the extent of surgery (complete vs. partial removal of lesions) varies among guidelines. Studies are likely hampered by different skill sets between participating surgeons.
- Robotic Surgery: AAGL and others highlight its benefits in complex cases, but its cost and accessibility limit widespread use. Specialized training is required.
- Ablation vs. Excision: The choice between these two methods remains a contentious topic, for some reason. Ablation is simpler and requires much less technical skill but is only applicable for treating superficial lesions. It may not be as effective in the long term as excision, which is more comprehensive and accurate in terms of removing all of the visible disease. Again, the skill base of surgeons is critical, and high variability in this regard may be affecting the ability to prove or disprove the effectiveness and safety of each.
- Endometrioma: Cystectomy or excision of endometriomas is superior to drainage in terms of lower recurrence. Excision also provides the opportunity for pathologic confirmation, and this may be important where it is not clear whether or not there is also a tumor present. Where fertility is a major concern, the more atraumatic the approach to surgery, the less ovarian reserve is affected, and this is another area where surgeon expertise is critical.
- Deep Infiltrating Endometriosis: Highly specialized excisional surgeries are recommended because ablation simply does not work with these lesions. There is an even stronger emphasis on the surgeon’s expertise and patient selection. Intuitively, the best outcomes probably rest with selecting the best possible technology in a master surgeon’s hands. Some strongly believe that this means robotic surgery for advanced cases with highly distorted anatomy.
- Hysterectomy: This is considered a “definitive” or last resort surgery but may be helpful for complete excision of endo at any point. It also allows the removal of any co-existing pain-producing adenomyosis, which is embedded in the wall of the uterus.
- LUNA (laparoscopic uterine nerve ablation) and PSN (presacral neurectomy): Guidelines reflect multiple reviews that suggest no benefit to LUNA but a possible benefit for PSN in selected cases. PSN is technically very challenging and treatment should be individualized. As far as LUNA is concerned, studies include a mix of ablation and excision, which means a lack of precision in many of them and, again, surgeon skill level may be a factor. Thus a definitive conclusion may be elusive until a better methodology to accurately study this is employed.
- Complementary and Alternative Therapies: Exploring Additional Avenues
- Acupuncture and Electrotherapy (TENS): Mentioned in some guidelines as adjunct therapies, with some encouraging results. More research is needed to fully validate their effectiveness. However, these are low-risk options.
- Nutritional Supplements: Some guidelines suggest that dietary changes and supplements might play a role in symptom management. This includes microbiome management for optimal estrogen metabolism. There will likely never be large randomized studies for any of these variables because they would have to be huge and thus impractical to conduct. But in today’s emerging world of personalized molecular medicine, other study methodologies are being explored to determine which of these approaches to diet and lifestyle may be more effective than others.
- Infertility and Endometriosis: A Delicate Balance
- Surgical vs. Non-Surgical Approaches: The decision to opt for surgery in infertility cases is complex and depends on individual factors like age, severity of endometriosis, and previous treatments. Reducing inflammation appears to be beneficial to effective intrauterine implantation and gestation.
- Surgical vs. Non-Surgical Approaches: The decision to opt for surgery in infertility cases is complex and depends on individual factors like age, severity of endometriosis, and previous treatments. Reducing inflammation appears to be beneficial to effective intrauterine implantation and gestation.
- Emerging Treatments and Research
- Future Directions: Ongoing research into immunotherapies, new hormonal agents, and gene/molecular therapy offer promising avenues for more personalized treatment strategies.
Endometriosis management is a highly dynamic field with evolving guidelines and currently very discrepant recommendations due to incomplete or low-quality scientific evidence. Understanding current options is crucial for women to make informed decisions about their health. Regular consultations with endometriosis experts, staying informed about new research, and considering a multi-disciplinary holistic approach to treatment can significantly improve quality of life.
Additional Reading:
- The Different Tests Used to Diagnose Endometriosis
- Laparoscopy: A Common Treatment for Endometriosis
References:
- Kalaitzopoulos, D. R., Samartzis, N., Kolovos, G. N., Mareti, E., Samartzis, E. P., Eberhard, M., Dinas, K., & Daniilidis, A. (2021). Treatment of endometriosis: a review with comparison of 8 guidelines. BMC Womens Health, 21(1), 397. https://doi.org/10.1186/s12905-021-01545-5
- Hirsch M, Begum MR, Paniz É, Barker C, Davis CJ, Duffy J. Diagnosis and management of endometriosis: a systematic review of international and national guidelines. BJOG. 2018;125(5):556–64.

Endometriosis Guidelines: A Closer Look at a Potential Source of Confusion in Treatment Debates
Table of contents
Treatment strategies for endometriosis vary widely, with the primary objective being to alleviate pain and enhance fertility where necessary. However, the confusion and inconsistency in recommendations is alarming. This article reviews and comments on some of the key current management strategies supported by the American College of Obstetrics and Gynecologists (ACOG), by way of Bulletin #114 (2010 and reaffirmed in 2022) and Bulletin #760 concerning adolescents (2018 and reaffirmed 2022). In the following posts, we will review other guidelines to give a more in-depth look at these inconsistencies and what you may face as you navigate your journey with endometriosis.
Other internationally recognized bodies have published various guidelines seeking to help clinicians with the diagnosis and treatment of endometriosis. Unfortunately, there is significant discrepancy between some of the recommendations due to the complex nature of the disease and limitations of research to date. Many patients will look to online resources and forums after seeing providers and not seeing results. What they may be surprised to find is that information on sites dedicated to endometriosis are often inconsistent with what is proffered by different guideline resources.
Surgery
Surgery is considered a cornerstone in the management of pain and infertility associated with endometriosis. The timing of surgery and the type of surgery recommended varies between guidelines. However, it is illuminating to note that ACOG guideline Bulletin #114 states that “definitive diagnosis of endometriosis only can be made by histology of lesions removed at surgery.”
Minimally invasive surgery is highly preferred over open surgery (laparotomy) due to less pain, shorter hospital stay, quicker recovery, and better cosmetic results. However, a high level of skill and expertise is required to perform these procedures, whether it be laparoscopic or robotically assisted surgery. Despite better technology inherent in robotic surgery, outcomes research does not clearly show which modality is better overall. However, the skill of the surgeon likely trumps the surgical tools used. Robotic surgery may be better suited for particularly difficult cases involving severely distorted anatomy due to advanced endo or scarring from repeat surgeries.
The excision of endometriosis is widely recommended for patients with endometriosis-associated pain. However, there is ongoing debate on the preferred surgical technique (ablation versus excision) due to lack of conclusive evidence. Currently, the studies that look at excision surgery vs. ablation have significant limitations, potentially due to variation in the skill and training of the surgeons involved in these studies. Meaning, studies to date may not have been done by true excision specialists and resulted in incomplete removal thereby skewing the research results. This variation in surgeon expertise is a common plight affecting surgical procedure outcomes research.
In ovarian endometriosis (endometriomas or chocolate cysts), minimally invasive excision of endometriomas is superior to drainage and ablation in terms of reducing recurrence of dysmenorrhoea, dyspareunia, cyst recurrence, and the need for further surgical interventions.
In cases where women have completed their family planning and failed to respond to conservative treatments, hysterectomy with simultaneous excision of endometriotic lesions is considered the last resort. However, except for cases in which there is coexisting adenomyosis, hysterectomy is not necessarily required for pain relief purposes. Each situation should be highly individualized.
Medical Management of Endometriosis
While surgery is an effective treatment strategy and helps many patients, medical management currently plays a crucial role in managing symptoms and preserving fertility. These treatments primarily focus on pain management, hormonal suppression, and birth control.
Pain management is a critical aspect of endometriosis treatment. Non-steroidal anti-inflammatory drugs (NSAIDs) are widely used for symptomatic treatment of dysmenorrhea and acyclic pelvic pain. In fact, in their article discussing dysmenorrhea and endometriosis in adolescents, without any workup, ACOG believes that the majority of adolescents have primary dysmenorrhea which is defined as painful menstruation in the absence of pelvic pathology and recommends first line-therapies such as NSAIDs and birth control. The question is: without undergoing a definitive workup and assessment (surgery) for endometriosis and knowing that imaging is insufficient for diagnosis – how is it determined they do not have pelvic pathology? Furthermore, ACOG considers those that respond symptomatically to birth control pills and NSAIDs as a confirmation of primary dysmenorrhea, though some people with endometriosis also respond symptomatically to birth control pills and NSAIDs.
Hormonal suppression, through the use of progestins, combined oral contraceptives, micronized progesterone, or Gonadotropin-releasing hormone (GnRH) analogues, is a common treatment strategy. This recommendation assumes that estrogen is responsible for endometriosis, but this is based on an incomplete understanding of endometriosis genesis and progression. Hormones are clearly involved but, based on increasing molecular evidence, this is not the sole factor in promoting growth of endometriosis.
Birth control pills, specifically combined oral contraceptives, are often used as a first-line therapy for endometriosis-associated pain. This works by suppressing ovulation, which may help slow the growth of endometriotic tissue but has not been proven to induce regression or resolution.
GnRH analogues are recommended as second-line treatment options for endometriosis-associated pain. They work by suppressing the production of estrogen, thereby theroretically reducing the growth of endometriotic tissue. Along these lines, ACOG states that “there is no data that support the use of preoperative medical suppressive therapy,” yet in clinical practice, many individuals are offered these medications inconsistently related to consideration or timing of surgery. Additionally, their level B evidence (second level) recommendations state “After an appropriate pretreatment evaluation (to exclude other causes of chronic pelvic pain) and failure of initial treatment with OCs (oral contraceptives) and NSAIDS, empiric therapy with a 3-month course of a GnRH agonist is appropriate.” It can be argued that this is extremely problematic given that there is no conclusive data to support the use of these medications prior to surgery. Finally, there is a significant risk of short and potentially long term side effects and complications.
Complementary Therapies
Complementary therapies such as dietary interventions, acupuncture, and electrotherapy are increasingly being recognized as potential adjunctive treatments for endometriosis. Quite a bit is evidence supported, but more research is needed to fully establish their efficacy and safety. Thus guidelines do not routinely address such options, leaving patients to their own devices and trial and error.
In conclusion, the management of endometriosis requires a multi-faceted approach, incorporating both surgical and medical treatments which will be variable from patient to patient. In the past few years, there have been some improvements in the amount of research as well as advocacy. Finding a knowledgeable specialized surgeon and care team is of utmost importance. The majority of OBGYNs do not focus on endo, have not undergone further specialized training and generally align with the guidelines set forth by ACOG, largely driven by perceived medico-legal concerns related to standard of practice.. Furthermore, other guidelines seem to differ in their opinions and recommendations regarding medical management and surgery, so stay tuned for more information.
Related reading:
- Find an Endometriosis Specialist for Diagnosis, Treatment, & Surgery
- Why was iCareBetter built?
- What You Need to Know About Endometriosis Excision Surgery
References:
- Bulletins–Gynecology, A. C. o. P. (2000). ACOG practice bulletin. Medical management of endometriosis. Number 11, December 1999 (replaces Technical Bulletin Number 184, September 1993). Clinical management guidelines for obstetrician-gynecologists. Int J Gynaecol Obstet, 71(2), 183-196. https://doi.org/10.1016/s0020-7292(00)80034-x
- ACOG Committee Opinion No. 760: Dysmenorrhea and Endometriosis in the Adolescent. (2018). Obstet Gynecol, 132(6), e249-e258. https://doi.org/10.1097/AOG.0000000000002978

Navigating the Path to Your Best Endometriosis Specialist
The journey towards resolving endometriosis involves an important decision – selecting the best endometriosis specialist.
Table of contents
Determining Your Needs in a Surgeon
Being aware of your specific requirements can help you make an informed choice. Here are a few considerations you should keep in mind:
Training and Experience
A surgeon’s training, notably in Minimally Invasive Gynecologic Surgery (MIGS) or Fellowship in Minimally Invasive Gynecologic Surgery (FMIGS) is crucial. Such surgeons have spent more time in operation theaters, honing their skills through extensive practice.
Ensure your surgeon is board-certified and inquire about their experience, including the number of surgeries they’ve performed, complications they’ve encountered, and outcomes.
Surgical Support Team
The surgeon’s team is equally important. Ask about their procedure in case of bowel, bladder, ureter, or diaphragmatic involvement. Inquire if everything can be done during a single procedure.
Approach to Excision
Surgeons may have different opinions on excision versus ablation. Find out their thoughts on the subject and where and when they excise or ablate.
Post-Surgery Care
Ask if the surgeon routinely prescribes suppressive medications pre and post-surgery. Understand their reasons if they do.
Costs
Don’t hesitate to inquire about costs, insurance acceptance, payment policies, and any hidden charges.
Comfort Level
Ensure you feel comfortable conversing with your surgeon and that your queries are answered satisfactorily.
Factors That May Not Influence Your Decision
Certain aspects may not influence the quality of surgical care:
- Gender: The surgeon’s gender does not impact their surgical ability.
- Preferred Tools: The surgical tool used is less important than the surgeon’s skill.
- Bowel Prep: Surgeons may have different preferences for bowel prep before surgery, but it doesn’t seem to influence the outcome.
Factors That Might Influence Your Decision
Some factors might play a role in your decision-making process:
- Reputation: Be cautious while considering a surgeon’s reputation. Some may get media coverage or have excellent bedside manners, but that doesn’t necessarily make them a skilled surgeon.
- Office Management: A well-managed front office can make your experience smoother.
- Location: Depending on your comfort and ability to travel, location might influence your decision.
- Timing: The availability of the surgeon and your urgency might also play a role.
The Most Important Factor
Patients often report being most satisfied with surgeons who actively listen to them. Your surgeon should respect your knowledge and experiences without objection to being recorded or having someone with you during consultations.
Leading Endometriosis Specialists
iCareBetter has a list of endometriosis specialists and surgeons vetted for their surgical skills.
Managing Your Relationship with Your Current Doctor
Dealing with a current doctor who might not be capable of handling your endometriosis can be challenging. Here are some tips:
- Think long-term, maintain a cordial relationship, and educate your doctor about your condition without alienating them.
- Be respectful and considerate of your doctor’s opinions.
- Try to keep your doctor on your side by asking for their support.
- Remain calm and collected during discussions.
- If you choose to seek surgery elsewhere and decide not to return to your current physician, send a copy of the operative and pathology reports with a note of gratitude.
- If your doctor dismisses you as a patient, consider it as a sign that it wasn’t a good fit.
- Routine care can be handled by a GP or Family Doctor, a Nurse Practitioner, or a Physician’s Assistant.

Does Endometriosis Cause Infertility? Covering the Basics
Table of contents
- Learn More About the Connections Between Endometriosis and Infertilit y
- What is Endometriosis
- Endometriosis and Fertility: Exploring the Connection
- What Happens When Endometriosis Does Cause Infertility?
- Other Data on Endometriosis and Reproduction
- Diagnosing Endometriosis: A Multifaceted Approach
- Managing Endometriosis: A Multidisciplinary Approach
- Dietary and Lifestyle Considerations
- Endometriosis and Pregnancy: Potential Complications
- Mental Well-Being and Psychological Impact of Fertility Treatment for Endo Patients
- Endometriosis and Fertility: Navigating the Journey
Learn More About the Connections Between Endometriosis and Infertility
An endometriosis (endo) diagnosis can be a frightening thing. Very frightening. While this inflammatory condition can be binary or non-binary, women of childbearing age are prone to issues with reproduction due to endo. So does endometriosis cause infertility? Keep reading as I break down the basics of this topic. In this comprehensive guide, I will delve into the complex interplay between endometriosis and fertility, exploring the condition’s impact, treatment options, and strategies to overcome potential obstacles on the journey to parenthood. I will also discuss the emotional impact of this condition on patients.
What is Endometriosis
Endometriosis is a chronic inflammatory condition. In this disease, endometrial-like lesions implant on tissues and organs throughout the abdomen and pelvis, even elsewhere in the body! These lesions contain glands and stroma, similar to the endometrium (the tissue that lines the uterine walls), causing chronic inflammatory reactions.
Endometriosis lesions produce many substances and even make their own estrogen, which, as a result, causes a variety of issues locally and systemically. Pain is one of the most common symptoms, though silent endo exists as well. Please continue reading this article to learn more about endometriosis.
Endometriosis and Fertility: Exploring the Connection
While endometriosis does not automatically equate to infertility, there is a well-documented association between the two. Approximately 30% to 50% of individuals with endometriosis experience fertility challenges, though the reasons behind this link are not fully understood. Several potential mechanisms have been proposed:
- Anatomical Distortions: Endometriosis can cause physical distortions in the reproductive anatomy, leading to scarring, adhesions, and obstructions in the fallopian tubes or ovaries, hindering the fertilization process.
- Inflammatory Response: The lesions can trigger an inflammatory response, creating an inhospitable environment for fertilization and implantation.
- Hormonal Imbalances: Endometriosis may disrupt the delicate hormonal balance required for ovulation and implantation, potentially impacting fertility.
- Egg Quality: Some research suggests that endometriosis may adversely affect egg quality, further complicating the conception process.
Despite these potential challenges, it’s important to note that more than 70% of individuals with mild to moderate endometriosis can conceive naturally, offering hope for those seeking to start a family.
What Happens When Endometriosis Does Cause Infertility?
It can. 25 to 50% of women with infertility have endometriosis, and 30 to 50% of women with endometriosis have infertility. However, it is very encouraging to know that most women with endometriosis can become pregnant.
This statistic is significant. Many younger women with this disorder feel psychological effects due to the possibility of not being able to have kids. Not all patients carry this sentiment. Growing numbers of people do not want to have children. However, for those who do, these thoughts and emotions about fertility can be devastating. Then, endometriosis patients who do conceive often worry about the pregnancy and subsequent delivery of the baby.
Other Data on Endometriosis and Reproduction
Studies have also demonstrated that the enzyme aromatase may also play a role in endometriosis and infertility. There is an abnormally high level of this enzyme in the endometrium and endometriosis lesions in patients with endometriosis. In the uterus, this enzyme may affect both natural endometrial development and its receptivity for the implantation of the fetus.
Progesterone is another hormone that may play a role in implantation failure. Resistance to this enzyme can affect reproduction, as it is necessary for a normal pregnancy. In some studies, progesterone receptors displayed abnormalities and caused dysregulation in the endometrial layer of the uterus in patients with endometriosis. Levels of progesterone should increase with pregnancy, but with endometriosis, this process is delayed and can cause an unopposed estrogen state that cannot sustain fertility.
Diagnosing Endometriosis: A Multifaceted Approach
Diagnosing endometriosis can be a complex process, as the symptoms can mimic those of other conditions. The diagnostic journey often begins with a physical examination and an evaluation of the individual’s medical history. If endometriosis is suspected, additional tests may be recommended, such as:
- Ultrasound: An abdominal or transvaginal ultrasound can help identify cysts (endometriomas), possibly endometriosis lesions (this is not common but an up-and-coming area of research), as well as the potential impact on the organs themselves or other abnormalities in the reproductive organs.
- Laparoscopy: Considered the gold standard for diagnosing endometriosis, a laparoscopy involves a minimally invasive surgical procedure where a small camera is inserted into the abdomen, allowing the surgeon to visually inspect the pelvic organs and take tissue samples if necessary.
While the severity of endometriosis is often classified into stages (minimal, mild, moderate, or severe) based on the extent and location of the endometrial growths, it’s important to note that the stage does not necessarily correlate with the intensity of symptoms or the degree of fertility challenges.
Managing Endometriosis: A Multidisciplinary Approach
The management of endometriosis typically involves a multidisciplinary approach, combining medical and surgical interventions tailored to the individual’s unique circumstances and fertility goals. Treatment options may include:
- Pain Management: Over-the-counter or prescription pain medications, such as non-steroidal anti-inflammatory drugs (NSAIDs) or hormonal contraceptives, can help alleviate the discomfort associated with endometriosis.
- Hormone Therapy: Hormonal treatments, such as birth control pills, progestin-only therapy, or gonadotropin-releasing hormone (GnRH) agonists, may have some impact on suppressing the growth of endometriosis and managing symptoms, though these options are only short-term while on the medications and can have some serious side effects.
- Surgery: Laparoscopic or robotic surgery is recommended to remove endometriosis, scar tissue, or cysts, potentially improving fertility outcomes.
- Assisted Reproductive Technologies (ART): In cases where natural conception remains challenging, assisted reproductive technologies like in vitro fertilization (IVF) or intrauterine insemination (IUI) may be recommended.
It’s crucial to work closely with a multidisciplinary team, including reproductive endocrinologists, gynecologists, and fertility specialists, to develop a personalized treatment plan that addresses both the management of endometriosis symptoms and the individual’s fertility goals.
Dietary and Lifestyle Considerations
While there is no definitive evidence that specific dietary or lifestyle changes can cure endometriosis or improve fertility outcomes, maintaining a healthy lifestyle can contribute to overall well-being and potentially alleviate some symptoms. Recommendations may include:
- Balanced Diet: Consuming a diet rich in fresh fruits, and vegetables, minimizing grains, especially gluten, and lean proteins can provide essential nutrients and support overall health.
- Exercise: Regular physical activity, such as low-impact exercises like walking or swimming, can help manage stress and promote overall well-being.
- Stress Management: Engaging in stress-reducing activities like meditation, yoga, or deep breathing exercises can help promote relaxation and reduce the impact of stress on fertility.
- Supplements: While the evidence is limited, some individuals report benefits from taking supplements for pain relief, reducing inflammation, and improving their quality of life.
It’s essential to consult with a healthcare professional before making significant dietary or lifestyle changes, especially if you are undergoing fertility treatments or considering assisted reproductive technologies.
Endometriosis and Pregnancy: Potential Complications
While endometriosis does not necessarily preclude a successful pregnancy, it’s important to be aware of potential complications that may arise. Some of the risks associated with endometriosis during pregnancy include:
- Placenta Previa: Endometriosis may increase the risk of placenta previa, a condition where the placenta partially or completely covers the cervix, potentially leading to bleeding and complications during pregnancy or delivery.
- Miscarriage: Research findings on the link between endometriosis and miscarriage have been mixed, with some studies suggesting an increased risk while others found no significant association.
- Ectopic Pregnancy: Endometriosis may increase the risk of ectopic pregnancy, where the fertilized egg implants outside the uterus, typically in the fallopian tube.
It’s essential to work closely with your healthcare provider to monitor and manage any potential complications that may arise during pregnancy if you have endometriosis.
Mental Well-Being and Psychological Impact of Fertility Treatment for Endo Patients
Living with endometriosis can be a challenging and emotionally taxing experience, particularly for those struggling with fertility issues. The physical pain, emotional distress, and potential financial burdens associated with treatment can take a toll on an individual’s mental well-being. It’s crucial to prioritize self-care and seek support from mental health professionals, support groups, or counseling services if needed.
Furthermore, you and your partner can do these things to help prepare for these possible feelings:
- Prepare and be ready for the emotional journey ahead.
- Cope with grief and loss associated with unsuccessful prior attempts or miscarriages.
- Develop strategies for coping with the news of other people’s births and pregnancies.
- Keep the communication lines between you and your partner open and discuss feelings throughout the entire process.
Endometriosis and Fertility: Navigating the Journey
The path to parenthood for individuals with endometriosis can be challenging, but it’s important to remember that fertility challenges are not insurmountable. By working closely with a multidisciplinary team of healthcare professionals, exploring various treatment options, and maintaining a positive outlook, many individuals with endometriosis can achieve their dream of starting a family.
It’s crucial to be proactive in seeking support and guidance from healthcare providers, as well as accessing resources and support networks specifically designed for those navigating endometriosis and fertility challenges. Organizations like the American Society for Reproductive Medicine (ASRM) and Endometriosis UK offer valuable information, resources, and advocacy support for individuals on this journey.
While endometriosis may present obstacles, embracing a comprehensive approach that addresses both the condition and fertility goals can increase the chances of a successful outcome. With perseverance, the right medical support, and a commitment to self-care, the dream of parenthood can become a reality for many individuals with endometriosis.
REFERENCES
https://www.pennmedicine.org/updates/blogs/fertility-blog/2016/august/endometriosis-and-fertility
https://www.endometriosis-uk.org/endometriosis-fertility-and-pregnanc
Updated: August 9, 2024

Find Endometriosis Specialists for the Best Possible Outcomes
Table of contents
Why You Need an OB-GYN Who Specializes in Endometriosis
Endometriosis is common (affecting nearly 190 million women worldwide) but poorly understood by many medical professionals. It’s hard to find endometriosis specialists who have completed advanced training. With the proper endo specialist, medical treatment or surgery can lessen your pain, improve your quality of life, and manage complications.
Endometriosis is a chronic pain condition that affects 10-15% of women of reproductive age. It causes painful periods, bleeding between periods, pain during sexual intercourse, and discomfort when passing urine or feces. Despite causing chronic pelvic pain, many medical professionals have a poor understanding of the condition.
In this article, we will look into what endometriosis is and explore how to improve diagnosis, treatment, and outcome factors.
What is Endometriosis?
Endometriosis affects menstruating women and girls and some women post-hysterectomy or post-menopause. The condition also can affect transgender men and non-binary individuals. Endometriosis affects roughly 190 million people worldwide, with immune, genetic and hormonal factors all likely to be at play.
To understand Endometriosis, we first need to understand the endometrium or lining of the uterus.
The Endometrium
A large proportion of the endometrium is stromal cells. Stromal cells regulate cell growth and change during the menstrual cycle.
Endometrial glands line the endometrium. During the menstrual cycle, they widen in response to greater blood flow.
Each cycle, stromal cells, and endometrial glands slough off as part of menstruation.
Endometriosis Lesions
The presence of endometrium-like cells found outside the uterus causes the classic endometriosis symptoms. Discourse exists, but scientists have concluded a genetic basis to the cells’ presence, with endometrium-like cells migrating inappropriately during embryogenesis.
Endometriotic lesions can be in the ovaries, uterine ligaments, fallopian tubes, and pouch of Douglas (the space between the uterus and rectum). In some, lesions are present outside the pelvic cavity. Locations include the bowel, urinary tract wall, diaphragm, lungs, abdomen, and pericardium (the sack around the heart).
The endometrial-like tissue responds to the natural cycle of hormones and also produces some hormones by itself. This tissue has cycles of growth and bleeding.
Whereas menstrual blood in the uterus leaves the body via the vagina, the blood and tissues cannot escape from endometriosis lesions. This trapped cells and tissue leads to the painful processes of inflammation, adhesions, and scarring.
What does it feel like to have Endometriosis?
Although pain is the most common complaint, Endometriosis causes a wide range of symptoms, including:
- Painful periods
- Heavy periods (menorrhagia)
- Vaginal bleeding between periods
- Pain on passing urine or feces
- Bowel symptoms include bloating, constipation, diarrhea, or bleeding from the bowel
- Pain during intercourse
- Tiredness
- Depression
- Infertility.
Social and Emotional Effects
Severe pain can interrupt daily life for many patients. This interruption may include missing school, taking days off work, or being unable to socialize. A study in 2020 found that in over half of women, the pain had reduced their professional, physical, and sexual activity.
Endometriosis is associated with low mood. 15% of women are diagnosed with depression, with an average age at diagnosis of 22.
Infertility
Infertility can be the only symptom of Endometriosis for some women. Around 30-50% of patients cannot get pregnant owing to inflammation, pelvic adhesions, blockage of the fallopian tubes, and changes to the pelvic anatomy.
Other Symptoms
Additional symptoms are dependent on the location of endometriosis lesions. For example, an endometriotic lesion in the lung could cause breathlessness or chest pain. A study of over 2000 patients found that endometriotic nodules caused leg and buttock pain, as well as numbness, similar to sciatic pain.
Misdiagnosis and incorrect management are therefore common for women with symptoms that are not classic to pelvic endometriotic lesions.
Endometriosis Myths
The average delay in the diagnosis of Endometriosis is more than seven years, leading to “unnecessary suffering and reduced quality of life.” This delay leads many people to the internet to conduct their own research before and during diagnosis. However, the internet is awash with myths.
The importance of educating yourself via a reputable source such as iCareBetter cannot be understated.
Find Endometriosis Specialists for Appropriate Diagnosis & Treatment
The widespread misunderstanding of Endometriosis hinders its diagnosis and treatment. The inappropriate investigation, treatment with analgesics, or hormonal suppression do little to manage the cause while delaying diagnosis. Women who felt they were not listened to nor understood by doctors have described frustration, anger, annoyance, and sadness.
Reassuringly, appropriate diagnosis and treatment can lead to significant improvements in pain. This is precisely why it is crucial to find an endometriosis specialist. Only highly specialized surgeons with a comprehensive team can perform a thorough excision to remove endometriotic lesions, including extra-pelvic locations. Complete removal can significantly improve overall outcomes, including relief from pain and increased quality of life.
iCareBetter Endometriosis Care
iCareBetter is a platform that connects patients with experts in endometriosis care. At iCareBetter, patients have access to surgeons who have completed advanced training. These professionals have shown expertise in the diagnosis and treatment of complex Endometriosis. iCareBetter utilizes a transparent and unbiased system to ensure that only doctors with proven advanced excision skills and a comprehensive care team can be on their surgeons’ list.
Patients can select their surgeon based on their specific symptoms. This empowers patients to consult a doctor who truly understands the complexity of their condition. Patients can access specialists for endometriosis in the pelvis, bowels, bladder, thorax, heart, or diaphragm. They also can find help with infertility issues.
A highly specialized endo surgeon will take a holistic approach to treatment. This holistic approach includes managing secondary comorbidities such as infertility, even in stage III and IV disease patients.
At iCareBetter, patients can also access expert physical therapists who understand the condition. Working with a physical therapist gives access to myofascial release techniques, visceral mobilization, and the tools to manage a susceptible nervous system for better pain management.
Team-based expert care improves post-operative outcomes. For some iCareBetter doctors, post-treatment reports of satisfactory pain relief could be over 80%, with less than 20% of women requiring subsequent pelvic surgery. Moreover, many patients see reduced pain relief requirements post-recovery.
Standards of excellence, such as those endorsed by iCareBetter, must become a driving force behind treatment protocols for Endometriosis. Women should no longer shoulder the pain and reduced quality of life associated with substandard care.
Conclusion
Endometriosis occurs due to the presence of endometrium-like cells found outside the uterus. The resulting inflammation, adhesions, and scarring can cause severe pain and symptoms related to the location of the lesions. By connecting patients with expert surgeons in endometriosis care, iCareBetter empowers patients to access the care leading to better outcomes. Advanced surgical excision, physical therapy, and an expert team-based approach can reduce pain, as well as skillfully manage secondary complications.
Find endometriosis specialists today.

