
Can Endometriosis on Ureter Cause Kidney Shooting Back Pain?
Endometriosis is a common gynecological condition that affects many women during their reproductive years. While it typically manifests in the pelvic region, in some instances, it may invade other organs, including the urinary system. This article explores the question: Can endometriosis on the ureter cause kidney shooting back pain?
About Endometriosis
Endometriosis is a chronic disease characterized by the presence of endometrial-like tissue outside the womb. This could include the ovaries, fallopian tubes, and the lining of the pelvic cavity. In some extreme cases, endometrial tissue may also affect organs outside the pelvic cavity, such as the bladder, bowel, or kidneys.
Read More: Understanding Endometriosis: Unveiling the Common Symptoms and Their Impact
Understanding Ureteral Endometriosis
Ureteral endometriosis is an uncommon manifestation of the disease, accounting for about 1% of all endometriosis cases. It involves the ureters, the tubes that transport urine from the kidneys to the bladder. This condition can lead to urinary tract obstruction, resulting in hydronephrosis, which is the swelling of a kidney due to a build-up of urine.
The Kidney-Endometriosis Connection
The kidneys can be impacted when one or both of the ureters become affected by endometriosis. The section of the ureter that is usually affected sits below the pelvic area.
Symptoms of Kidney Endometriosis
Kidney endometriosis can be asymptomatic for several years. If a person who has undergone surgery to treat endometriosis has ongoing urinary problems such as pain and infections, it may suggest the presence of urinary tract or kidney endometriosis. Symptoms may include:
- Pain in the lower back that gets worse with a monthly menstrual cycle. That pain can also extend down through the legs.
- Blood in the urine that can co-occur with the menstrual cycle
- Difficulty urinating
- Recurrent urinary tract infections
Read More: Understanding How Endometriosis Can Cause
Diagnosis of Kidney Endometriosis
The diagnosis of ureteral endometriosis relies heavily on clinical suspicion. As a result, they often misdiagnose patients with kidney cancer. This can lead to patients not receiving treatment on time, or receiving the wrong kind of treatment.
Read More: Life After Endometriosis Surgery: A Comprehensive Guide
Treatment Options
Kidney endometriosis can lead to kidney damage and even kidney failure if left untreated. However, the best approach is to treat the condition by removing endometriosis lesions with minimally invasive laparoscopic surgery.
The Silent Threat of Kidney Failure
One of the most concerning aspects of ureteral endometriosis is the silent threat of kidney failure. It is estimated that as many as 25% to 50% of nephrons are lost when there is evidence of ureteral endometriosis, and 30% of patients will have reduced kidney function at the time of diagnosis.
Impact on Kidney Health
The good news is that if one kidney isn’t functioning due to endometriosis, you can survive on the other kidney. So, if you find out you only have one fully-functioning kidney, it’s essential to take care of it.
Conclusion
In conclusion, while endometriosis is typically a pelvic condition, it can venture beyond and affect the urinary system, including the kidneys. This can lead to severe complications, including kidney failure. Therefore, it’s crucial for women with endometriosis to be aware of the potential symptoms and seek medical advice if they experience any signs of kidney problems. The early detection and treatment of ureteral endometriosis are crucial to preserving kidney function and overall health.
References:
https://drseckin.com/kidney-endometriosis/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3535807/
Endometriosis: Perilous impact on kidneys
https://endometriosis.net/clinical/silent-kidney-failure

How to Treat Bowel Endometriosis: A Comprehensive Guide
Bowel endometriosis, a complex and severe variant of endometriosis, is a condition best navigated with a deep understanding of its details. This guide aims to shed light on the various aspects of bowel endometriosis, from its origins to symptoms, diagnostic approaches, and treatment options, to empower those affected.
What is Bowel Endometriosis?
Endometriosis, a chronic health disorder predominantly affecting women in their reproductive years, is characterized by the growth of endometrial-like tissue, which usually lines the uterus in regions outside the uterus. This misplaced tissue prompts an inflammatory reaction, leading to distressing symptoms. When this aberrant tissue growth takes place on or inside the bowels, the condition is referred to as bowel endometriosis.
How Common is Bowel Endometriosis?
While the exact prevalence of bowel endometriosis remains uncertain, it’s estimated to occur in 5-15% of all endometriosis cases. Predominantly, it manifests on the rectum or sigmoid colon but can also affect the appendix or small intestine.
Read More: https://icarebetter.com/endometriosis-and-inflammatory-bowel-disease-distinguishing-the-differences/
Recognizing the Symptoms
Symptoms of bowel endometriosis may not always be apparent, especially in the early stages of the disease. However, as the condition progresses, women may experience discomfort associated with their menstrual cycle, sexual intercourse, bowel movements, and even infertility.
Symptoms commonly associated with bowel endometriosis include:
- Painful Bowel Movements: This is often accompanied by constipation or diarrhea.
- Rectal Bleeding: This symptom, which is more uncommon, usually occurs during menstruation.
- Infertility: Some women may experience difficulty conceiving.
- Pelvic Pain: Chronic pelvic pain is a common symptom associated with endometriosis, often more severe during menstruation or ovulation.
- Painful Intercourse: This is often due to the endometriosis lesion causing a distortion of the pelvic anatomy.
It’s important to note that bowel endometriosis can sometimes mimic symptoms of other gastrointestinal conditions, like irritable bowel syndrome (IBS), making it challenging to diagnose.
Diagnosing Bowel Endometriosis
A comprehensive diagnosis of bowel endometriosis usually involves a combination of physical examination, medical history analysis, and advanced imaging techniques. The diagnostic process may include:
- Physical Examination: This includes a manual check for growths in the rectum or vagina.
- Imaging Tests: These can include ultrasound, MRI, colonoscopy, and barium enema.
- Laparoscopy: This surgical procedure is considered the gold standard for diagnosing endometriosis, as it allows for visual examination of the uterus, ovaries, and other pelvic structures. And surgeons can take samples for histopathology evaluations.
Read More: Understanding Bowel Endometriosis
Treating Bowel Endometriosis: An Overview
Treatment for bowel endometriosis is complex and multifaceted. It requires a personalized approach, taking into account the severity of the disease, the patient’s age, fertility goals, and personal preferences. The primary treatment options include:
- Hormonal Therapy: This involves medications that control estrogen levels, which can influence the progression of endometriosis. These medications can help manage pain and other symptoms.
- Pain Management: Over-the-counter or prescription nonsteroidal anti-inflammatory drugs (NSAIDs) may be recommended to help alleviate pain.
- Surgery: Surgical interventions aim to remove as much endometrial tissue as possible while preserving organ function.
Surgical Treatment Options
Surgery is typically the primary treatment for bowel endometriosis, particularly for severe cases. The goal of surgery is to remove endometrial implants without compromising the functionality of the organs involved. There are three main surgical options:
- Segmental Bowel Resection: This involves removing the section of the bowel affected by endometriosis and reconnecting the healthy portions. This option is often recommended for larger areas of endometriosis.
- Rectal Shaving: This procedure involves shaving off the endometriosis from the top of the bowel without removing any portion of the intestines. It’s often used for smaller areas of endometriosis.
- Disc Resection: In this procedure, a surgeon cuts out a small disk where the endometriosis lesions appear and then closes the remaining hole.
Understanding the Risks of Surgery
Surgery for bowel endometriosis is a complex procedure associated with certain risks. These can include short-term complications such as infection, leakage of bowel content during the postoperative healing phase, peritonitis, and septicaemia. Long-term risks might include bowel dysfunction, characterized by frequency, urgency, and incontinence.
Read More: Finding an Excision Specialist: What you Need to Know
Hormone Treatment Options
Although hormonal treatments cannot halt the progression of endometriosis, they can help manage symptoms. Hormonal treatments for bowel endometriosis can include birth control pills, progestin injections, or, less favorably, gonadotropin-releasing hormone (GnRH) agonists.
Read more: What are the long-term side effects of Lupron?
Managing Symptoms and Quality of Life
Bowel endometriosis can significantly impact the quality of life of those affected. However, with appropriate treatment and management strategies, many women affected by this condition can lead fulfilling lives. Communication with your healthcare team, lifestyle modifications, and psychological support can all contribute to improving the quality of life.
Conclusion
Understanding how to treat bowel endometriosis is crucial for managing this complex and often painful condition. With the right approach, it’s possible to mitigate symptoms, improve fertility outcomes, and enhance the quality of life for those affected. If you suspect you have bowel endometriosis, it’s important to speak with a healthcare provider who can guide you through the diagnostic process and treatment options. With the right knowledge and resources, you can navigate this challenging condition and find a path to improved health and well-being.
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4229526/
https://weillcornell.org/news/what-is-bowel-endometriosis
https://www.webmd.com/women/endometriosis/bowel-endometriosis
https://www.healthline.com/health/womens-health/bowel-endometriosis
Understanding How Endometriosis Can Cause
Bowel Problems
Endometriosis, a common health concern among women, can manifest itself in various ways, one of them being bowel problems. But how exactly can endometriosis cause bowel problems? This article will take you through the intricate connection between endometriosis and bowel problems, the symptoms to look out for, diagnostic procedures, and potential treatments.
What is Endometriosis?
Endometriosis is a health condition where the tissue similar to the type that lines the uterus, known as the endometrium, grows outside the uterus. This condition predominantly affects the reproductive organs such as the ovaries, fallopian tubes, and the external part of the uterus. However, it can also extend to other parts of the body including the bowels, rectum, and other pelvic organs.
Understanding Bowel Endometriosis
Bowel endometriosis is a form of endometriosis that affects the gastrointestinal tract, specifically the bowels. It can appear in two forms: superficial (on the surface of the bowel) and deep (penetrating the bowel wall).
Read More: Understanding Bowel Endometriosis
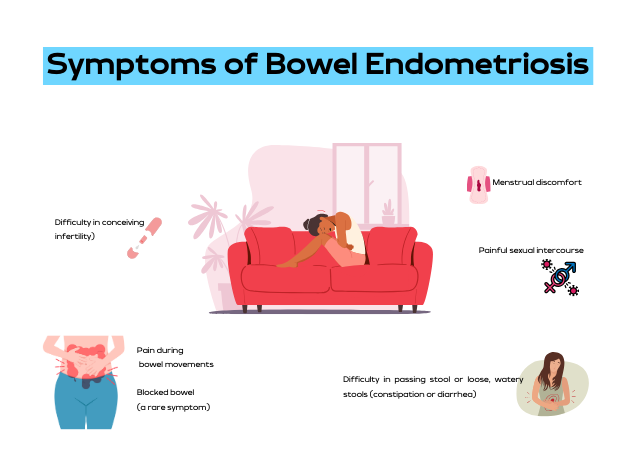
Symptoms of Bowel Endometriosis
The symptoms of bowel endometriosis can vary widely depending on the location of the lesion, its size, and how deep it is in the bowel wall. Some women may experience no symptoms. However, common symptoms include:
- Difficulty in passing stool or loose, watery stools (constipation or diarrhea)
- Pain during bowel movements
- Menstrual discomfort
- Painful sexual intercourse
- Difficulty in conceiving (infertility)
- Blocked bowel (a rare symptom)
It is noteworthy that these symptoms can often mimic other conditions like irritable bowel syndrome (IBS), but the two conditions are distinct. One distinguishing factor is that with bowel endometriosis, symptoms often worsen before and during the menstrual period.
Read More: Endometriosis and Painful Intercourse: Is it Really Just Endometriosis?
Causes of Bowel Endometriosis
The exact cause of bowel endometriosis is still under study. However, several factors have been linked to its occurrence. These include genetic predisposition, inflammation, and levels of estrogen, a female sex hormone.
The Prevalence of Endometriosis
Endometriosis affects approximately 10%-12% of women of childbearing age. The condition is often diagnosed in women who are in their 30s, although it can occur at any age.
Diagnosing Bowel Endometriosis
The diagnosis of bowel endometriosis starts with the doctor asking about your symptoms and medical history, followed by a physical examination of your pelvic area. The doctor may also recommend imaging tests to get more information on the location and size of any cysts or tissue damage related to endometriosis. These tests include:
- Transvaginal or transrectal ultrasound: This procedure involves the insertion of a wand-like device into your vagina or rectum. This device releases sound waves that create images of your organs.
- Magnetic resonance imaging (MRI): An MRI test provides detailed images of your organs and tissues using a magnetic field and radio waves.
- Laparoscopy: This surgical procedure involves making a small incision near your belly button and inserting a thin viewing tool called a laparoscope.
- Barium enema: This type of X-ray is used to see changes or defects in your large intestine (colon).
- Colonoscopy: They pass a tube with a camera on its tip through the anus into the colon to directly visualize the wall and take samples from inside the colon.
Read More: Colon Chronicles: Delving into Bowel Endometriosis
Treating Bowel Endometriosis
The treatment plan for bowel endometriosis will be personalized, taking into account your symptoms, medical history, age, and reproductive plans. Treatments can include:
- Surgery: The aim of surgery is to remove as many lesions as possible while preserving your organs and overall health.
- Hormone treatments: These medications control estrogen levels which can worsen the symptoms of bowel endometriosis.
- Counseling: Given the ongoing nature of bowel endometriosis and its impact on both physical and mental health, counseling may be recommended to provide emotional support.
The Prognosis for Bowel Endometriosis
There is currently no cure for endometriosis. However, treatments like surgery and hormone therapy can help manage the symptoms. It is also important to note that symptoms could return if treatment is halted, or they could recur on their own, especially in cases with deep lesions.
Endometriosis is a complex condition that can cause bowel problems and other health issues. If you suspect you have endometriosis and are experiencing bowel problems, it’s important to consult with a healthcare provider. Early diagnosis and treatment can help manage symptoms and improve your quality of life.
References:
https://www.webmd.com/women/endometriosis/bowel-endometriosis
https://www.endometriosis-uk.org/endometriosis-and-bowel
https://www.endofound.org/gastrointestinal-distress
ENDOMETRIOSIS AND CONSTIPATION

Through the Looking Glass: Reflecting on 2023
Embarking on the journey of self-reflection is not just a personal endeavor; for us at iCareBetter, it’s a collective celebration of progress, community, and collaboration. As we bid farewell to 2023, a year marked by challenges and triumphs, it’s time to take a look into the past year and reflect on all that has been accomplished. Join us as we navigate through the areas of growth, community involvement, projects, and meaningful collaborations that shaped our year. In this special blog post, we’re excited to share the insights gained from our podcast endeavors and offer a sneak peek into the thrilling developments that await us in 2024. Let’s rewind, recap, and anticipate the exciting narrative that continues to unfold in the ever-evolving story of iCareBetter.
About iCareBetter
iCareBetter is an innovative platform dedicated to helping patients with endometriosis and chronic pelvic pain find compassionate and skilled experts. All experts on iCareBetter have shown knowledge and expertise in the treatment of endometriosis and chronic pelvic pain.
Vision
Our vision is to reduce the symptom-to-effective treatment of endometriosis to less than a year. Studies show that patients with endometriosis spend an average of 7.5 years to have an official diagnosis. Moreover, even after the diagnosis, patients will have to spend several years with multiple failed treatment attempts. After the long delays in diagnosis and treatment, they might be lucky enough to receive effective treatment from an expert.
Mission
Our mission is to improve access to high-quality specialized care for those with endometriosis. iCareBetter wants to combat the issue of patients living in confusion, pain, and isolation. To that end, we hope to connect as many patients to the right experts as early as possible. And we hope that this will ensure timely diagnosis and effective treatment.
To read more about why iCareBetter was built and the inspiration behind it, check out our blog here and listen to episode 1 of the podcast here, where Saeid and Jandra give you a behind the scenes look into what inspired them.
What happened in 2023?
In 2023, iCareBetter grew in many ways, including new avenues to provide education along with collaboration from the community. Here are some of the highlights!
- We started a podcast! iCareBetter: Endometriosis Unplugged is hosted by Jandra Mueller, DPT, MS a pelvic floor physical therapist and endometriosis patient. The podcast is available on Spotify, Apple Podcasts, and Youtube.
- We had 19 weekly episodes in season one
- Listeners joined from all over the world, reaching 22 countries
- We brought on a team to help with new content on social media creating a more visually appealing platform, community engagement, and followers.
- We now have 211 providers on our website available and ready to help those suffering from endometriosis and we are continuing to grow!
- Our blog content is now consistent with twice weekly posts bringing you updates on all things endometriosis.
What To Expect in 2024
While 2023 was a big year for iCareBetter, we hope to continue the growth and expand our providers across the globe. Our hope is to increase our collaboration with medical specialists, researchers, and advocates. There are some exciting things to come in 2024 including a new season of iCareBetter: Endometriosis Unplugged as well as some other projects that will be announced in 2024.
We hope you have found our resources helpful either for yourself or a loved one, and hope you continue to share the love and spread the word about Endometriosis. All of us here at iCareBetter wish you a safe and happy new year.

Cheers to 2024!
Do you or a loved one have Endometriosis? Here are some blogs that may help you get started on your journey.
- Endometriosis Signs and Symptoms: Everything You Need to Know
- Endometriosis Facts & Myths: Dispelling the Misconceptions

Endometriosis Guidelines: A Closer Look at a Potential Source of Confusion in Treatment (Part 2)
Understanding Endometriosis Treatment Confusion
Endometriosis affects millions of women worldwide, presenting with pain, irregular menstruation, and infertility. To shed light on the most effective treatment methods, this article is Part 2 in our series on this topic. It summarizes and comments on the findings from a recent 2021 review which provided a detailed analysis of various endometriosis treatment global guidelines as of September 2020.
There are often some discrepancies between guidelines for any disease. However, for endometriosis, a prior review in 2018 revealed that only about 7% of recommendations were comparable between international guidelines. Up to 28% of the recommendations were not supported by good research evidence at all. This helps explain why there is such a wide variation between doctors’ recommendations in clinical practice.
Key Guidelines reviewed in the most recent publication were:
- American College of Obstetricians and Gynecologists (ACOG)–reviewed in our last post, which you can read HERE
- Society of Obstetricians and Gynaecologists of Canada (SOGC)
- European Society of Human Reproduction and Embryology (ESHRE)
- Australian National Endometriosis Clinical and Scientific Trials (ACCESS)
- Royal College of Obstetricians and Gynaecologists (RCOG)
- French National College of Gynecologists and Obstetricians (CNGOF)
- American Association of Gynecologic Laparoscopists (AAGL)
- German Society for Gynecology and Obstetrics (DGGG)
Summary Review of Treatment Recommendations
- Non-Hormonal Medical Pain Management
- Nonsteroidal anti-inflammatory drugs (NSAIDs): While this is considered by all guidelines to be first-line therapy for dysmenorrhea and acyclic pelvic pain, it is not specific for endometriosis. A diagnosis and targeted therapy is more prudent since a large review showed no difference in effectiveness between NSAIDs and placebo.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): While this is considered by all guidelines to be first-line therapy for dysmenorrhea and acyclic pelvic pain, it is not specific for endometriosis. A diagnosis and targeted therapy is more prudent since a large review showed no difference in effectiveness between NSAIDs and placebo.
- Hormonal Treatment Options:
- Progestins and Combined Oral Contraceptives (COCs): Widely recommended for initial pain management. Specific formulations and dosages vary across guidelines. Of interest, there is little mention of compounded micronized progesterone which is hard to study but may deserve a place in the conversation. The Levonorgestrel Intrauterine System (LNG-IUS) is particularly noted for its localized progestin delivery, reducing systemic side effects and effectively managing pain.
- Megace (Megestrol Acetate): A potent progestin recommended by several guidelines but varies as a first-line vs second-line option. The additional benefit is less bone loss than that seen with GnRH agonist therapy.
- GnRH Agonists: Uniformly recommended in all guidelines for severe symptoms after first-line therapy; potential side effects, which can be long-lasting, include decreased bone density and menopausal-like symptoms. Add-back low-dose estrogen therapy can reduce symptoms. Most guidelines, and the FDA, recommend durations of 6 months or less.
- Emerging Hormonal Therapies: GnRH antagonists are gaining attention for their rapid onset of action and fewer side effects compared to agonists. The evidence is not conclusive.
- Danazol and Gestrinone: Older treatments with androgenic effects, are less commonly used today due to side effects. Gestrinone is not currently available in the United States.
- Selective Estrogen Receptor Modulators (SERMs) and Selective Progesterone Receptor Modulators (SPRMs) are emerging options being explored for their targeted action and potential benefits.
- Aromatase Inhibitors: Considered in some cases, especially for pain unresponsive to other treatments. Most guidelines agree that this is a possible second-line option, but the evidence is not conclusive. A possible niche for effective use may be in post-menopausal patients who have endo.
- Surgical Approaches: Navigating the Complexities
- Laparoscopic Surgery: Endorsed for its efficacy and reduced recovery time, compared to big incision (laparotomy) surgery. However, the extent of surgery (complete vs. partial removal of lesions) varies among guidelines. Studies are likely hampered by different skill sets between participating surgeons.
- Robotic Surgery: AAGL and others highlight its benefits in complex cases, but its cost and accessibility limit widespread use. Specialized training is required.
- Ablation vs. Excision: The choice between these two methods remains a contentious topic, for some reason. Ablation is simpler and requires much less technical skill but is only applicable for treating superficial lesions. It may not be as effective in the long term as excision, which is more comprehensive and accurate in terms of removing all of the visible disease. Again, the skill base of surgeons is critical, and high variability in this regard may be affecting the ability to prove or disprove the effectiveness and safety of each.
- Endometrioma: Cystectomy or excision of endometriomas is superior to drainage in terms of lower recurrence. Excision also provides the opportunity for pathologic confirmation, and this may be important where it is not clear whether or not there is also a tumor present. Where fertility is a major concern, the more atraumatic the approach to surgery, the less ovarian reserve is affected, and this is another area where surgeon expertise is critical.
- Deep Infiltrating Endometriosis: Highly specialized excisional surgeries are recommended because ablation simply does not work with these lesions. There is an even stronger emphasis on the surgeon’s expertise and patient selection. Intuitively, the best outcomes probably rest with selecting the best possible technology in a master surgeon’s hands. Some strongly believe that this means robotic surgery for advanced cases with highly distorted anatomy.
- Hysterectomy: This is considered a “definitive” or last resort surgery but may be helpful for complete excision of endo at any point. It also allows the removal of any co-existing pain-producing adenomyosis, which is embedded in the wall of the uterus.
- LUNA (laparoscopic uterine nerve ablation) and PSN (presacral neurectomy): Guidelines reflect multiple reviews that suggest no benefit to LUNA but a possible benefit for PSN in selected cases. PSN is technically very challenging and treatment should be individualized. As far as LUNA is concerned, studies include a mix of ablation and excision, which means a lack of precision in many of them and, again, surgeon skill level may be a factor. Thus a definitive conclusion may be elusive until a better methodology to accurately study this is employed.
- Complementary and Alternative Therapies: Exploring Additional Avenues
- Acupuncture and Electrotherapy (TENS): Mentioned in some guidelines as adjunct therapies, with some encouraging results. More research is needed to fully validate their effectiveness. However, these are low-risk options.
- Nutritional Supplements: Some guidelines suggest that dietary changes and supplements might play a role in symptom management. This includes microbiome management for optimal estrogen metabolism. There will likely never be large randomized studies for any of these variables because they would have to be huge and thus impractical to conduct. But in today’s emerging world of personalized molecular medicine, other study methodologies are being explored to determine which of these approaches to diet and lifestyle may be more effective than others.
- Infertility and Endometriosis: A Delicate Balance
- Surgical vs. Non-Surgical Approaches: The decision to opt for surgery in infertility cases is complex and depends on individual factors like age, severity of endometriosis, and previous treatments. Reducing inflammation appears to be beneficial to effective intrauterine implantation and gestation.
- Surgical vs. Non-Surgical Approaches: The decision to opt for surgery in infertility cases is complex and depends on individual factors like age, severity of endometriosis, and previous treatments. Reducing inflammation appears to be beneficial to effective intrauterine implantation and gestation.
- Emerging Treatments and Research
- Future Directions: Ongoing research into immunotherapies, new hormonal agents, and gene/molecular therapy offer promising avenues for more personalized treatment strategies.
Endometriosis management is a highly dynamic field with evolving guidelines and currently very discrepant recommendations due to incomplete or low-quality scientific evidence. Understanding current options is crucial for women to make informed decisions about their health. Regular consultations with endometriosis experts, staying informed about new research, and considering a multi-disciplinary holistic approach to treatment can significantly improve quality of life.
Additional Reading:
- The Different Tests Used to Diagnose Endometriosis
- Laparoscopy: A Common Treatment for Endometriosis
References:
- Kalaitzopoulos, D. R., Samartzis, N., Kolovos, G. N., Mareti, E., Samartzis, E. P., Eberhard, M., Dinas, K., & Daniilidis, A. (2021). Treatment of endometriosis: a review with comparison of 8 guidelines. BMC Womens Health, 21(1), 397. https://doi.org/10.1186/s12905-021-01545-5
- Hirsch M, Begum MR, Paniz É, Barker C, Davis CJ, Duffy J. Diagnosis and management of endometriosis: a systematic review of international and national guidelines. BJOG. 2018;125(5):556–64.

Endometriosis Guidelines: A Closer Look at a Potential Source of Confusion in Treatment Debates
Treatment strategies for endometriosis vary widely, with the primary objective being to alleviate pain and enhance fertility where necessary. However, the confusion and inconsistency in recommendations is alarming. This article reviews and comments on some of the key current management strategies supported by the American College of Obstetrics and Gynecologists (ACOG), by way of Bulletin #114 (2010 and reaffirmed in 2022) and Bulletin #760 concerning adolescents (2018 and reaffirmed 2022). In the following posts, we will review other guidelines to give a more in-depth look at these inconsistencies and what you may face as you navigate your journey with endometriosis.
Other internationally recognized bodies have published various guidelines seeking to help clinicians with the diagnosis and treatment of endometriosis. Unfortunately, there is significant discrepancy between some of the recommendations due to the complex nature of the disease and limitations of research to date. Many patients will look to online resources and forums after seeing providers and not seeing results. What they may be surprised to find is that information on sites dedicated to endometriosis are often inconsistent with what is proffered by different guideline resources.
Surgery
Surgery is considered a cornerstone in the management of pain and infertility associated with endometriosis. The timing of surgery and the type of surgery recommended varies between guidelines. However, it is illuminating to note that ACOG guideline Bulletin #114 states that “definitive diagnosis of endometriosis only can be made by histology of lesions removed at surgery.”
Minimally invasive surgery is highly preferred over open surgery (laparotomy) due to less pain, shorter hospital stay, quicker recovery, and better cosmetic results. However, a high level of skill and expertise is required to perform these procedures, whether it be laparoscopic or robotically assisted surgery. Despite better technology inherent in robotic surgery, outcomes research does not clearly show which modality is better overall. However, the skill of the surgeon likely trumps the surgical tools used. Robotic surgery may be better suited for particularly difficult cases involving severely distorted anatomy due to advanced endo or scarring from repeat surgeries.
The excision of endometriosis is widely recommended for patients with endometriosis-associated pain. However, there is ongoing debate on the preferred surgical technique (ablation versus excision) due to lack of conclusive evidence. Currently, the studies that look at excision surgery vs. ablation have significant limitations, potentially due to variation in the skill and training of the surgeons involved in these studies. Meaning, studies to date may not have been done by true excision specialists and resulted in incomplete removal thereby skewing the research results. This variation in surgeon expertise is a common plight affecting surgical procedure outcomes research.
In ovarian endometriosis (endometriomas or chocolate cysts), minimally invasive excision of endometriomas is superior to drainage and ablation in terms of reducing recurrence of dysmenorrhoea, dyspareunia, cyst recurrence, and the need for further surgical interventions.
In cases where women have completed their family planning and failed to respond to conservative treatments, hysterectomy with simultaneous excision of endometriotic lesions is considered the last resort. However, except for cases in which there is coexisting adenomyosis, hysterectomy is not necessarily required for pain relief purposes. Each situation should be highly individualized.
Medical Management of Endometriosis
While surgery is an effective treatment strategy and helps many patients, medical management currently plays a crucial role in managing symptoms and preserving fertility. These treatments primarily focus on pain management, hormonal suppression, and birth control.
Pain management is a critical aspect of endometriosis treatment. Non-steroidal anti-inflammatory drugs (NSAIDs) are widely used for symptomatic treatment of dysmenorrhea and acyclic pelvic pain. In fact, in their article discussing dysmenorrhea and endometriosis in adolescents, without any workup, ACOG believes that the majority of adolescents have primary dysmenorrhea which is defined as painful menstruation in the absence of pelvic pathology and recommends first line-therapies such as NSAIDs and birth control. The question is: without undergoing a definitive workup and assessment (surgery) for endometriosis and knowing that imaging is insufficient for diagnosis – how is it determined they do not have pelvic pathology? Furthermore, ACOG considers those that respond symptomatically to birth control pills and NSAIDs as a confirmation of primary dysmenorrhea, though some people with endometriosis also respond symptomatically to birth control pills and NSAIDs.
Hormonal suppression, through the use of progestins, combined oral contraceptives, micronized progesterone, or Gonadotropin-releasing hormone (GnRH) analogues, is a common treatment strategy. This recommendation assumes that estrogen is responsible for endometriosis, but this is based on an incomplete understanding of endometriosis genesis and progression. Hormones are clearly involved but, based on increasing molecular evidence, this is not the sole factor in promoting growth of endometriosis.
Birth control pills, specifically combined oral contraceptives, are often used as a first-line therapy for endometriosis-associated pain. This works by suppressing ovulation, which may help slow the growth of endometriotic tissue but has not been proven to induce regression or resolution.
GnRH analogues are recommended as second-line treatment options for endometriosis-associated pain. They work by suppressing the production of estrogen, thereby theroretically reducing the growth of endometriotic tissue. Along these lines, ACOG states that “there is no data that support the use of preoperative medical suppressive therapy,” yet in clinical practice, many individuals are offered these medications inconsistently related to consideration or timing of surgery. Additionally, their level B evidence (second level) recommendations state “After an appropriate pretreatment evaluation (to exclude other causes of chronic pelvic pain) and failure of initial treatment with OCs (oral contraceptives) and NSAIDS, empiric therapy with a 3-month course of a GnRH agonist is appropriate.” It can be argued that this is extremely problematic given that there is no conclusive data to support the use of these medications prior to surgery. Finally, there is a significant risk of short and potentially long term side effects and complications.
Complementary Therapies
Complementary therapies such as dietary interventions, acupuncture, and electrotherapy are increasingly being recognized as potential adjunctive treatments for endometriosis. Quite a bit is evidence supported, but more research is needed to fully establish their efficacy and safety. Thus guidelines do not routinely address such options, leaving patients to their own devices and trial and error.
In conclusion, the management of endometriosis requires a multi-faceted approach, incorporating both surgical and medical treatments which will be variable from patient to patient. In the past few years, there have been some improvements in the amount of research as well as advocacy. Finding a knowledgeable specialized surgeon and care team is of utmost importance. The majority of OBGYNs do not focus on endo, have not undergone further specialized training and generally align with the guidelines set forth by ACOG, largely driven by perceived medico-legal concerns related to standard of practice.. Furthermore, other guidelines seem to differ in their opinions and recommendations regarding medical management and surgery, so stay tuned for more information.
Related reading:
- Find an Endometriosis Specialist for Diagnosis, Treatment, & Surgery
- Why was iCareBetter built?
- What You Need to Know About Endometriosis Excision Surgery
References:
- Bulletins–Gynecology, A. C. o. P. (2000). ACOG practice bulletin. Medical management of endometriosis. Number 11, December 1999 (replaces Technical Bulletin Number 184, September 1993). Clinical management guidelines for obstetrician-gynecologists. Int J Gynaecol Obstet, 71(2), 183-196. https://doi.org/10.1016/s0020-7292(00)80034-x
- ACOG Committee Opinion No. 760: Dysmenorrhea and Endometriosis in the Adolescent. (2018). Obstet Gynecol, 132(6), e249-e258. https://doi.org/10.1097/AOG.0000000000002978







