
Endometriosis and Fertility: Statistics, Facts, & Fiction
Table of contents
Debunking the Myths Surrounding Endometriosis and Reproduction
Disinformation about endometriosis and how it can impact reproduction is thick. As a matter of fact, not just endometriosis and fertility, the entire disorder is shrouded in junk information, and so it often goes misunderstood and mistreated. To learn more on this topic, read our previous article, titled: “Endometriosis Facts and Myths: Dispelling the Misconceptions.”
Does endometriosis cause infertility? In some cases, yes. However, in most cases, women with endometriosis can and do get pregnant without any medical assistance or intervention of any kind. There is still a myth that if you become pregnant, that can manage the endometriosis (endo) symptoms and even help resolve disease progression.
This statement couldn’t be further from the truth, and it’s an example of a widespread myth about endometriosis and fertility. Furthermore, this school of thought can put additional pressure on women with endometriosis to get pregnant as quickly as possible once they get a diagnosis. As you can imagine, this dangerous misinformation can alter their expectations in terms of treatment for fertility and their outlook on endometriosis in general.
So, Can You Get Pregnant If You Have Endometriosis?
The real truth is that the connection between endometriosis and reproduction is complex. Can you get pregnant if you have endometriosis? Yes, many people can and do. However, having the right endometriosis specialist to help you along the way can make all the difference in your journey. Click here to learn more about finding vetted endo specialists near you. In this article, we will review the disease and lay out the facts regarding endometriosis and fertility.
What is Endometriosis?
Endometriosis is an inflammatory disorder in which tissue similar to the uterus lining grows in places outside the uterus. Often these growths happen on the surface of the uterus, ovaries, fallopian tubes, or other organs within the pelvic cavity – such as the bladder or bowel. In some cases, these endometriosis growths have occurred in distant organs.
Endo growths can cause pain, scarring, and sometimes infertility. Because this tissue is similar to the uterine lining, it also bleeds and sheds once a month during hormonal changes. Typically in the uterus, this period tissue and blood have a means of escaping through the vagina. However, this blood and tissue often accumulate inside the body with endometriosis and causes inflammation and pain. As one can imagine, over time, scar tissue growths with subsequent menstrual cycles develop. Eventually, this scar tissue can fuse organs, immobilize organs, and even damage the fallopian tubes.
Alarming Statistics About Endometriosis & Fertility
- Endometriosis is widespread, affecting between six and ten percent of the general female population. That’s more than 170 million worldwide.
- In patients with pelvic pain, infertility, or both, endometriosis frequency is higher – between 35 percent to 50 percent.
- Between 25 percent to 50 percent of infertile women have endometriosis.
- Between 30 percent to 50 percent of women with endometriosis are infertile.
- Endometriosis affects approximately the same number of women around the world that have diabetes.
- The cost of endometriosis in the US is between $86 Bn – $116 Bn.
- It takes, on average, eight years from the onset of symptoms for a patient to get a diagnosis. This can impact all patients, but especially those of who wish to keep their fertility intact.
Endometriosis Facts About Fertility and Reproduction
- There are ways to get pregnant with endometriosis.
- Hormonal therapy does not cure endo.
- Endometriosis is related to your menstrual cycle and hormonal changes within your body.
- Endometriosis tissue can be removed during laparoscopy. Depending on the location of the growths and the extent of damage, this can sometimes restore fertility.
- There is a type of endometriosis that can cause cancerous lesions, typically dark chocolate brown.
- The causes are uncertain, and there is no “cure” for endometriosis.
- Genes seem to play a role in the occurrence of endo.
Myths About Endometriosis and Fertility
- Pregnancy is not a cure or a way to relieve symptoms of endometriosis. Women should not be pressured or encouraged to get pregnant to help with endometriosis and fertility or alleviate pain or other symptoms. While some women experience less endo pain and symptoms during their period, that does not mean it works the same for all women.
- Do not believe any physician that tells you a hysterectomy is the “gold standard” treatment for endometriosis. As mentioned above, there is no “cure” for endometriosis. Until a specialist is inside the body and can view the number and the placement of the endometriosis lesions, they cannot decide whether a hysterectomy would even solve the problems. Also, some women might make themselves infertile (whether they mind or not, it is an emotional part of this disorder) by having a hysterectomy done that was never needed.
- You do not need to have a major medical procedure to get an endometriosis diagnosis or remove some growths and lesions. With modern equipment, skilled specialists, and advanced technology (often robotic surgical equipment), you can have endometriosis diagnosis and treatment with laparoscopy. This type of procedure is minimally invasive and only leaves behind a few puncture wounds.
- Abortion does not cause endometriosis.
- Endometriosis does not cause ovarian cancer. Although a type of endo involves cancerous tumors, this does not mean that having endometriosis makes you more likely to develop cancer.
- The most important myth to bust is that there is no treatment for endometriosis. Just because there is no “cure” for this pelvic inflammatory disorder does not mean there are no treatment options, even when it comes to endometriosis and infertility.
If you have endometriosis, what is the most common thing you have heard regarding endo and reproduction?
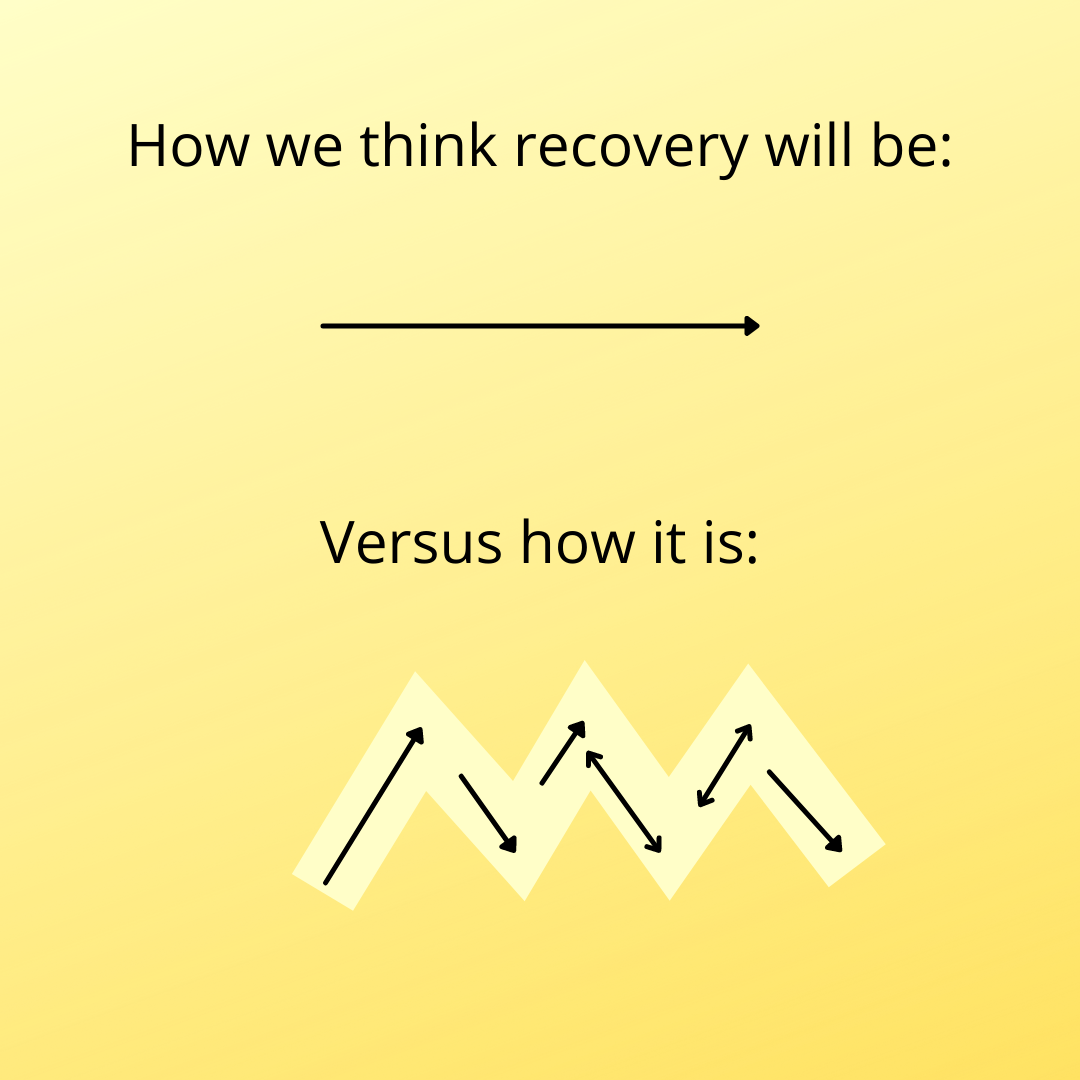
Recovery- not always smooth sailing
We often get questions about how long will it take to recover from surgery and how long does it take to know if it was successful. The aggravating answer is….it depends. There are many different things that play a part of surgery and recovery.
Recovery will be different for everyone. Everyone has their own innate healing (how quickly you heal, how you react to anesthesia and medications, adhesions, how healthy you were beforehand, etc.). Every surgery is different (what was done during surgery, how long was the surgery). Everyone might have other factors to their symptoms that will need to be addressed as well (such as pelvic floor dysfunction). While the incision on the outside may be small, there may be extensive work on the inside that is healing. Some people may notice a difference as soon as waking up from surgery. For others it may be weeks before they can tell a difference.
The success of the surgery can depend on multiple factors as well. One factor is what was your main goal? Some may have a goal of reduced pain while others may be more focused on fertility. With complete excision, there is the less likelihood of recurrence, but some people have ovarian endometriomas that have a higher recurrence rate if they are trying to preserve their ovaries. Some people may have other factors that are contributing symptoms, such as adenomyosis or interstitial cystitis. Sometimes we hear these wonderful stories of people waking up from surgery and feeling so much better, but that is not the case for everyone- but it doesn’t mean your surgery isn’t successful. Susan Pierce-Richards shares her thoughts on managing pre and post op expectations as someone who has been there: https://icarebetter.com/managing-expectations-pre-op-and-post-op/
For more information about healing after surgery, see: https://icarebetter.com/what-to-expect-in-the-weeks-after-skilled-excision-surgery/
*Remember to follow your surgeon’s instructions and call that surgeon if you have any questions or concerns!


Does Endometriosis Cause Infertility? Covering the Basics
Table of contents
- Learn More About the Connections Between Endometriosis and Infertilit y
- What is Endometriosis
- Endometriosis and Fertility: Exploring the Connection
- What Happens When Endometriosis Does Cause Infertility?
- Other Data on Endometriosis and Reproduction
- Diagnosing Endometriosis: A Multifaceted Approach
- Managing Endometriosis: A Multidisciplinary Approach
- Dietary and Lifestyle Considerations
- Endometriosis and Pregnancy: Potential Complications
- Mental Well-Being and Psychological Impact of Fertility Treatment for Endo Patients
- Endometriosis and Fertility: Navigating the Journey
Learn More About the Connections Between Endometriosis and Infertility
An endometriosis (endo) diagnosis can be a frightening thing. Very frightening. While this inflammatory condition can be binary or non-binary, women of childbearing age are prone to issues with reproduction due to endo. So does endometriosis cause infertility? Keep reading as I break down the basics of this topic. In this comprehensive guide, I will delve into the complex interplay between endometriosis and fertility, exploring the condition’s impact, treatment options, and strategies to overcome potential obstacles on the journey to parenthood. I will also discuss the emotional impact of this condition on patients.
What is Endometriosis
Endometriosis is a chronic inflammatory condition. In this disease, endometrial-like lesions implant on tissues and organs throughout the abdomen and pelvis, even elsewhere in the body! These lesions contain glands and stroma, similar to the endometrium (the tissue that lines the uterine walls), causing chronic inflammatory reactions.
Endometriosis lesions produce many substances and even make their own estrogen, which, as a result, causes a variety of issues locally and systemically. Pain is one of the most common symptoms, though silent endo exists as well. Please continue reading this article to learn more about endometriosis.
Endometriosis and Fertility: Exploring the Connection
While endometriosis does not automatically equate to infertility, there is a well-documented association between the two. Approximately 30% to 50% of individuals with endometriosis experience fertility challenges, though the reasons behind this link are not fully understood. Several potential mechanisms have been proposed:
- Anatomical Distortions: Endometriosis can cause physical distortions in the reproductive anatomy, leading to scarring, adhesions, and obstructions in the fallopian tubes or ovaries, hindering the fertilization process.
- Inflammatory Response: The lesions can trigger an inflammatory response, creating an inhospitable environment for fertilization and implantation.
- Hormonal Imbalances: Endometriosis may disrupt the delicate hormonal balance required for ovulation and implantation, potentially impacting fertility.
- Egg Quality: Some research suggests that endometriosis may adversely affect egg quality, further complicating the conception process.
Despite these potential challenges, it’s important to note that more than 70% of individuals with mild to moderate endometriosis can conceive naturally, offering hope for those seeking to start a family.
What Happens When Endometriosis Does Cause Infertility?
It can. 25 to 50% of women with infertility have endometriosis, and 30 to 50% of women with endometriosis have infertility. However, it is very encouraging to know that most women with endometriosis can become pregnant.
This statistic is significant. Many younger women with this disorder feel psychological effects due to the possibility of not being able to have kids. Not all patients carry this sentiment. Growing numbers of people do not want to have children. However, for those who do, these thoughts and emotions about fertility can be devastating. Then, endometriosis patients who do conceive often worry about the pregnancy and subsequent delivery of the baby.
Other Data on Endometriosis and Reproduction
Studies have also demonstrated that the enzyme aromatase may also play a role in endometriosis and infertility. There is an abnormally high level of this enzyme in the endometrium and endometriosis lesions in patients with endometriosis. In the uterus, this enzyme may affect both natural endometrial development and its receptivity for the implantation of the fetus.
Progesterone is another hormone that may play a role in implantation failure. Resistance to this enzyme can affect reproduction, as it is necessary for a normal pregnancy. In some studies, progesterone receptors displayed abnormalities and caused dysregulation in the endometrial layer of the uterus in patients with endometriosis. Levels of progesterone should increase with pregnancy, but with endometriosis, this process is delayed and can cause an unopposed estrogen state that cannot sustain fertility.
Diagnosing Endometriosis: A Multifaceted Approach
Diagnosing endometriosis can be a complex process, as the symptoms can mimic those of other conditions. The diagnostic journey often begins with a physical examination and an evaluation of the individual’s medical history. If endometriosis is suspected, additional tests may be recommended, such as:
- Ultrasound: An abdominal or transvaginal ultrasound can help identify cysts (endometriomas), possibly endometriosis lesions (this is not common but an up-and-coming area of research), as well as the potential impact on the organs themselves or other abnormalities in the reproductive organs.
- Laparoscopy: Considered the gold standard for diagnosing endometriosis, a laparoscopy involves a minimally invasive surgical procedure where a small camera is inserted into the abdomen, allowing the surgeon to visually inspect the pelvic organs and take tissue samples if necessary.
While the severity of endometriosis is often classified into stages (minimal, mild, moderate, or severe) based on the extent and location of the endometrial growths, it’s important to note that the stage does not necessarily correlate with the intensity of symptoms or the degree of fertility challenges.
Managing Endometriosis: A Multidisciplinary Approach
The management of endometriosis typically involves a multidisciplinary approach, combining medical and surgical interventions tailored to the individual’s unique circumstances and fertility goals. Treatment options may include:
- Pain Management: Over-the-counter or prescription pain medications, such as non-steroidal anti-inflammatory drugs (NSAIDs) or hormonal contraceptives, can help alleviate the discomfort associated with endometriosis.
- Hormone Therapy: Hormonal treatments, such as birth control pills, progestin-only therapy, or gonadotropin-releasing hormone (GnRH) agonists, may have some impact on suppressing the growth of endometriosis and managing symptoms, though these options are only short-term while on the medications and can have some serious side effects.
- Surgery: Laparoscopic or robotic surgery is recommended to remove endometriosis, scar tissue, or cysts, potentially improving fertility outcomes.
- Assisted Reproductive Technologies (ART): In cases where natural conception remains challenging, assisted reproductive technologies like in vitro fertilization (IVF) or intrauterine insemination (IUI) may be recommended.
It’s crucial to work closely with a multidisciplinary team, including reproductive endocrinologists, gynecologists, and fertility specialists, to develop a personalized treatment plan that addresses both the management of endometriosis symptoms and the individual’s fertility goals.
Dietary and Lifestyle Considerations
While there is no definitive evidence that specific dietary or lifestyle changes can cure endometriosis or improve fertility outcomes, maintaining a healthy lifestyle can contribute to overall well-being and potentially alleviate some symptoms. Recommendations may include:
- Balanced Diet: Consuming a diet rich in fresh fruits, and vegetables, minimizing grains, especially gluten, and lean proteins can provide essential nutrients and support overall health.
- Exercise: Regular physical activity, such as low-impact exercises like walking or swimming, can help manage stress and promote overall well-being.
- Stress Management: Engaging in stress-reducing activities like meditation, yoga, or deep breathing exercises can help promote relaxation and reduce the impact of stress on fertility.
- Supplements: While the evidence is limited, some individuals report benefits from taking supplements for pain relief, reducing inflammation, and improving their quality of life.
It’s essential to consult with a healthcare professional before making significant dietary or lifestyle changes, especially if you are undergoing fertility treatments or considering assisted reproductive technologies.
Endometriosis and Pregnancy: Potential Complications
While endometriosis does not necessarily preclude a successful pregnancy, it’s important to be aware of potential complications that may arise. Some of the risks associated with endometriosis during pregnancy include:
- Placenta Previa: Endometriosis may increase the risk of placenta previa, a condition where the placenta partially or completely covers the cervix, potentially leading to bleeding and complications during pregnancy or delivery.
- Miscarriage: Research findings on the link between endometriosis and miscarriage have been mixed, with some studies suggesting an increased risk while others found no significant association.
- Ectopic Pregnancy: Endometriosis may increase the risk of ectopic pregnancy, where the fertilized egg implants outside the uterus, typically in the fallopian tube.
It’s essential to work closely with your healthcare provider to monitor and manage any potential complications that may arise during pregnancy if you have endometriosis.
Mental Well-Being and Psychological Impact of Fertility Treatment for Endo Patients
Living with endometriosis can be a challenging and emotionally taxing experience, particularly for those struggling with fertility issues. The physical pain, emotional distress, and potential financial burdens associated with treatment can take a toll on an individual’s mental well-being. It’s crucial to prioritize self-care and seek support from mental health professionals, support groups, or counseling services if needed.
Furthermore, you and your partner can do these things to help prepare for these possible feelings:
- Prepare and be ready for the emotional journey ahead.
- Cope with grief and loss associated with unsuccessful prior attempts or miscarriages.
- Develop strategies for coping with the news of other people’s births and pregnancies.
- Keep the communication lines between you and your partner open and discuss feelings throughout the entire process.
Endometriosis and Fertility: Navigating the Journey
The path to parenthood for individuals with endometriosis can be challenging, but it’s important to remember that fertility challenges are not insurmountable. By working closely with a multidisciplinary team of healthcare professionals, exploring various treatment options, and maintaining a positive outlook, many individuals with endometriosis can achieve their dream of starting a family.
It’s crucial to be proactive in seeking support and guidance from healthcare providers, as well as accessing resources and support networks specifically designed for those navigating endometriosis and fertility challenges. Organizations like the American Society for Reproductive Medicine (ASRM) and Endometriosis UK offer valuable information, resources, and advocacy support for individuals on this journey.
While endometriosis may present obstacles, embracing a comprehensive approach that addresses both the condition and fertility goals can increase the chances of a successful outcome. With perseverance, the right medical support, and a commitment to self-care, the dream of parenthood can become a reality for many individuals with endometriosis.
REFERENCES
https://www.pennmedicine.org/updates/blogs/fertility-blog/2016/august/endometriosis-and-fertility
https://www.endometriosis-uk.org/endometriosis-fertility-and-pregnanc
Updated: August 9, 2024

Blood tests for endometriosis- not yet
We hear more and more about blood tests using DNA, RNA, and microRNA being researched as a possible way to help diagnose endometriosis. While more studies are needed, these tests do show some promise (Zafari et al., 2021). It would be nice to be a able to get a simple blood test and know that you probably have endometriosis and be able to plan accordingly. As Fassbender et al. (2015) states: “The most important goal of the test is that no women with endometriosis or other significant pelvic pathology are missed who might benefit from surgery for endometriosis-associated pain and/or infertility.”
MicroRNA are one specfic type of blood test being investigated. MicroRNA are involved in gene expression. Humans have “over 700 miRNAs” that “have been identified and fully sequenced”; these “miRNAs in humans have a direct influence on at least 30% of the genes in the whole genome” (Meštrović, 2018). Papari et al. (2020) explain that: “microRNAs are present in body fluids, including blood…which makes them more stable than circulating hormone or cytokine concentrations and therefore better candidate markers of disease. One miRNA can target several genes, and one gene can be targeted by different miRNAs. Circulating levels of miRNAs are dysregulated in several different cancers and in endometriosis.”
Papari et al. (2020) further states that “no clinical marker of endometriosis, either alone or in combination, has provided adequate sensitivity or specificity for the diagnosis of endometriosis. Thus, the search for suitable diagnostic markers of endometriosis remains a high but unmet research priority.” They did find in their study that a panel of different microRNA improved the accuracy of the test (Papari et al., 2020). Similar to ultrasounds, MRI’s, and other diagnostics studies, they might be helpful to rule in endometriosis but not necessarily entirely rule it out (see “But All Your Tests Are Negative”). It might be an initial step towards investigating the possibility of endometriosis once tests become available, but further investigation is warranted even if negative.
For more information see “Labwork and Blood Tests“
References
Fassbender, A., Burney, R. O., F O, D., D’Hooghe, T., & Giudice, L. (2015). Update on biomarkers for the detection of endometriosis. BioMed research international, 2015. Retrieved from https://www.hindawi.com/journals/bmri/2015/130854/
Meštrović, T. (2018). What is MicroRNA. Retrieved from https://www.news-medical.net/life-sciences/What-is-MicroRNA.aspx
Papari, E., Noruzinia, M., Kashani, L., & Foster, W. G. (2020). Identification of candidate microRNA markers of endometriosis with the use of next-generation sequencing and quantitative real-time polymerase chain reaction. Fertility and Sterility, 113(6), 1232-1241. Retrieved from https://www.fertstert.org/article/S0015-0282(20)30027-3/fulltext
Zafari, N., Bahramy, A., Majidi Zolbin, M., Emadi Allahyari, S., Farazi, E., Hassannejad, Z., & Yekaninejad, M. S. (2021). MicroRNAs as novel diagnostic biomarkers in endometriosis patients: a systematic review and meta-analysis. Expert Review of Molecular Diagnostics, 1-17. Retrieved from https://www.tandfonline.com/doi/abs/10.1080/14737159.2021.1960508

Find Endometriosis Specialists for the Best Possible Outcomes
Table of contents
Why You Need an OB-GYN Who Specializes in Endometriosis
Endometriosis is common (affecting nearly 190 million women worldwide) but poorly understood by many medical professionals. It’s hard to find endometriosis specialists who have completed advanced training. With the proper endo specialist, medical treatment or surgery can lessen your pain, improve your quality of life, and manage complications.
Endometriosis is a chronic pain condition that affects 10-15% of women of reproductive age. It causes painful periods, bleeding between periods, pain during sexual intercourse, and discomfort when passing urine or feces. Despite causing chronic pelvic pain, many medical professionals have a poor understanding of the condition.
In this article, we will look into what endometriosis is and explore how to improve diagnosis, treatment, and outcome factors.
What is Endometriosis?
Endometriosis affects menstruating women and girls and some women post-hysterectomy or post-menopause. The condition also can affect transgender men and non-binary individuals. Endometriosis affects roughly 190 million people worldwide, with immune, genetic and hormonal factors all likely to be at play.
To understand Endometriosis, we first need to understand the endometrium or lining of the uterus.
The Endometrium
A large proportion of the endometrium is stromal cells. Stromal cells regulate cell growth and change during the menstrual cycle.
Endometrial glands line the endometrium. During the menstrual cycle, they widen in response to greater blood flow.
Each cycle, stromal cells, and endometrial glands slough off as part of menstruation.
Endometriosis Lesions
The presence of endometrium-like cells found outside the uterus causes the classic endometriosis symptoms. Discourse exists, but scientists have concluded a genetic basis to the cells’ presence, with endometrium-like cells migrating inappropriately during embryogenesis.
Endometriotic lesions can be in the ovaries, uterine ligaments, fallopian tubes, and pouch of Douglas (the space between the uterus and rectum). In some, lesions are present outside the pelvic cavity. Locations include the bowel, urinary tract wall, diaphragm, lungs, abdomen, and pericardium (the sack around the heart).
The endometrial-like tissue responds to the natural cycle of hormones and also produces some hormones by itself. This tissue has cycles of growth and bleeding.
Whereas menstrual blood in the uterus leaves the body via the vagina, the blood and tissues cannot escape from endometriosis lesions. This trapped cells and tissue leads to the painful processes of inflammation, adhesions, and scarring.
What does it feel like to have Endometriosis?
Although pain is the most common complaint, Endometriosis causes a wide range of symptoms, including:
- Painful periods
- Heavy periods (menorrhagia)
- Vaginal bleeding between periods
- Pain on passing urine or feces
- Bowel symptoms include bloating, constipation, diarrhea, or bleeding from the bowel
- Pain during intercourse
- Tiredness
- Depression
- Infertility.
Social and Emotional Effects
Severe pain can interrupt daily life for many patients. This interruption may include missing school, taking days off work, or being unable to socialize. A study in 2020 found that in over half of women, the pain had reduced their professional, physical, and sexual activity.
Endometriosis is associated with low mood. 15% of women are diagnosed with depression, with an average age at diagnosis of 22.
Infertility
Infertility can be the only symptom of Endometriosis for some women. Around 30-50% of patients cannot get pregnant owing to inflammation, pelvic adhesions, blockage of the fallopian tubes, and changes to the pelvic anatomy.
Other Symptoms
Additional symptoms are dependent on the location of endometriosis lesions. For example, an endometriotic lesion in the lung could cause breathlessness or chest pain. A study of over 2000 patients found that endometriotic nodules caused leg and buttock pain, as well as numbness, similar to sciatic pain.
Misdiagnosis and incorrect management are therefore common for women with symptoms that are not classic to pelvic endometriotic lesions.
Endometriosis Myths
The average delay in the diagnosis of Endometriosis is more than seven years, leading to “unnecessary suffering and reduced quality of life.” This delay leads many people to the internet to conduct their own research before and during diagnosis. However, the internet is awash with myths.
The importance of educating yourself via a reputable source such as iCareBetter cannot be understated.
Find Endometriosis Specialists for Appropriate Diagnosis & Treatment
The widespread misunderstanding of Endometriosis hinders its diagnosis and treatment. The inappropriate investigation, treatment with analgesics, or hormonal suppression do little to manage the cause while delaying diagnosis. Women who felt they were not listened to nor understood by doctors have described frustration, anger, annoyance, and sadness.
Reassuringly, appropriate diagnosis and treatment can lead to significant improvements in pain. This is precisely why it is crucial to find an endometriosis specialist. Only highly specialized surgeons with a comprehensive team can perform a thorough excision to remove endometriotic lesions, including extra-pelvic locations. Complete removal can significantly improve overall outcomes, including relief from pain and increased quality of life.
iCareBetter Endometriosis Care
iCareBetter is a platform that connects patients with experts in endometriosis care. At iCareBetter, patients have access to surgeons who have completed advanced training. These professionals have shown expertise in the diagnosis and treatment of complex Endometriosis. iCareBetter utilizes a transparent and unbiased system to ensure that only doctors with proven advanced excision skills and a comprehensive care team can be on their surgeons’ list.
Patients can select their surgeon based on their specific symptoms. This empowers patients to consult a doctor who truly understands the complexity of their condition. Patients can access specialists for endometriosis in the pelvis, bowels, bladder, thorax, heart, or diaphragm. They also can find help with infertility issues.
A highly specialized endo surgeon will take a holistic approach to treatment. This holistic approach includes managing secondary comorbidities such as infertility, even in stage III and IV disease patients.
At iCareBetter, patients can also access expert physical therapists who understand the condition. Working with a physical therapist gives access to myofascial release techniques, visceral mobilization, and the tools to manage a susceptible nervous system for better pain management.
Team-based expert care improves post-operative outcomes. For some iCareBetter doctors, post-treatment reports of satisfactory pain relief could be over 80%, with less than 20% of women requiring subsequent pelvic surgery. Moreover, many patients see reduced pain relief requirements post-recovery.
Standards of excellence, such as those endorsed by iCareBetter, must become a driving force behind treatment protocols for Endometriosis. Women should no longer shoulder the pain and reduced quality of life associated with substandard care.
Conclusion
Endometriosis occurs due to the presence of endometrium-like cells found outside the uterus. The resulting inflammation, adhesions, and scarring can cause severe pain and symptoms related to the location of the lesions. By connecting patients with expert surgeons in endometriosis care, iCareBetter empowers patients to access the care leading to better outcomes. Advanced surgical excision, physical therapy, and an expert team-based approach can reduce pain, as well as skillfully manage secondary complications.
Find endometriosis specialists today.

Impact of Living with Endometriosis and Mental Health
(All research studies mentioned in this article about the impact of endometriosis on mental health enrolled people with assigned female gender at birth. However, to be inclusive to all people with endo, we use people throughout the article.)
Being diagnosed with endometriosis (endo) and living with it can bring up a lot of emotions. It can mean making space for changes that you may never have predicted or accounted for. Endometriosis impacts nearly 200 million people worldwide, but there is pernicious misinformation and a lack of awareness and understanding among the medical community and the larger society. This misinformation and lack of awareness stand in the way of receiving a timely diagnosis.
It takes, on average, over seven years for a person who has endometriosis to get a diagnosis. Essentially, this means experiencing intense pain, feeling unheard over and over, and being gaslit at a systemic level for at least seven years.
In most countries, managing the pain and heavy periods remain the first line of treatment for endometriosis. If one is lucky, they can access endometriosis excision surgery. However, the impact of endometriosis goes beyond just the physical. The effect of endometriosis on mental health and the emotional wellbeing of the person is enormous.
Link Between Endometriosis Pain and Mental Health
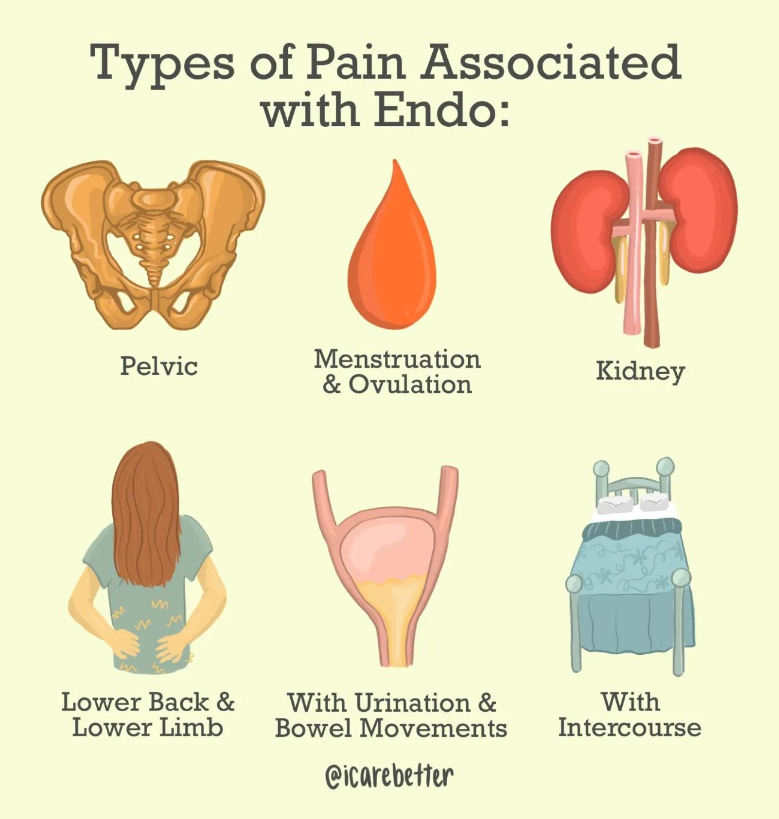
The mental health struggles of living with endometriosis vary from person to person. The debilitating chronic endometriosis pain, one of the most common symptoms, is a critical factor that impacts the quality of life and mental health. Along with the cyclic pelvic pain, one may also experience other types of pain in varying degrees:
- Non-menstrual pelvic pain
- Pain during ovulation, urination, and/or bowel movements
- Pain during sex
- Sciatic pain
- Pain post and during orgasms
- Widespread full-body pain.
Research published in the International Journal of Women’s Health Health looked at the link between common symptoms of endometriosis and mental wellbeing.
It found that a person experiencing chronic pelvic pain (CPP) is likely to feel higher levels of anxiety and depression, which can further amplify the perception and severity of pain, thus placing them in a vicious circle of physical and psychological distress.
Figure 1: The vicious circle of chronic pelvic pain and psychological disease.
Pelvic Pain Causes Further Effects of Endometriosis on Mental Health
A study found that endometriosis patients with pelvic pain had poorer quality of life and mental health than those with asymptomatic endometriosis. It also showed that non-menstrual pelvic pain impacts all the variables of a person’s life. Thus, the study emphasized psychological interventions as an essential aspect of the endometriosis treatment plan and pain management treatments and interventions.
In another meta-analysis of 99,614 people from 24 different studies, researchers found that chronic pelvic pain was a primary factor contributing to the higher rates of depression in patients with endometriosis. This study emphasized that treating this kind of depression with antidepressants without the efforts towards managing the chronic pain would indeed be ineffective.
The Emotional Reality of Endometriosis
Studies have tried to understand the impact and management of endometriosis within the medical healthcare system. But still, the health system has largely overlooked the effect of endometriosis on mental health.
Living with endometriosis can make daily activities a struggle, mainly due to the unpredictability of pain and fatigue. The struggle makes some tasks nearly impossible. These tasks can include planning, working, socializing, exercising, eating, or even basics like cooking, cleaning, and bathing. This inability fuels guilt and anxiety. Furthermore, the debilitating pain being reduced to “just a bad period” or “psychosomatic” often leaves one feeling gaslit, isolated, depressed, and sometimes suicidal.
This distress increases due to the lack of systemic and psychosocial support. When the BBC spoke to 13,500 people (female assigned at birth) with endometriosis, more than 50% of the respondents felt suicidal ideations.
This is a battle
For someone living with chronic pain every day, even a short-lived moment of low pain brings ease, which allows one to hope for a future not controlled by pain. However, grief sets in quickly as fatigue and flare-ups follow. These changes make life with endometriosis incoherent and an inescapable dance between hope and grief. A Swedish study concluded that people living with painful endometriosis underwent a constant struggle for coherence in their lives. It emphasized that healthcare providers should validate this struggle by understanding the disease-related grief.
The anxiety around pain and health, the grief related to the future, the loneliness and isolation often bring up the feeling that chronic pain has monopolized one’s life. Endometriosis becomes the central point around which all decisions revolve. It takes away the body’s ability to be reliable and the capacity to feel safe within it. It often changes the way one views themselves and takes the world in.
One of the ways we feel safe in the world is by feeling safe in our bodies. Then what happens to our sense of safety when the body is a constant source of never-ending pain?
The Trauma of Endometriosis
Experts define trauma as the experience of being left alone with one’s pain. Endometriosis isn’t different. Having to constantly explain one’s pain to medical doctors, families, and friends and still not being believed is an isolating and traumatizing experience. For some, this experience of being gaslit gets stored in the body and pushes the nervous system into a hypervigilant state (Fight, Flight, Freeze).
This experience of trauma can bring up various responses, anger being one of them. The anger can be at the world, the state, the body, the systems, other people, or the pain. It becomes our protective mechanism in response to the powerlessness that one feels while coping with endometriosis.
The Way Forward
In treating endometriosis, it becomes necessary to consider its impact on mental health and provide psychosocial support to people with endometriosis and their families. Unlike the conventional medical belief that solely focuses on the physiological aspects, a multidisciplinary approach integrating the mind and the body is necessary.
A trauma-informed psychotherapist specialized in treating endometriosis, and chronic pain can be helpful. A therapist trained in chronic pain management understands endometriosis, related diagnoses, and its trauma. This understanding is an integral part of the healing process. Seeing the light at the end of the tunnel is complicated and sometimes impossible with pain. Verbalizing the pain, having the hardships validated, acknowledged, and believed can be an empowering experience. Just as people seek medical help for their physical symptoms, seeking help for mental health struggles is an integral part of the endometriosis journey. If therapy is hard to access, support groups for endometriosis can be a step forward. You should know that you are not alone in your experience, and you can have support. The supports that you get can be a lifeline to your mental health.
Author: Anindita Kundu, Trauma Psychotherapist.
How has endometriosis impacted your mental health? Have you considered working with a mental health specialist to help you?

Hysterectomy and endometriosis
A hysterectomy is not a cure for endometriosis; however, many people with endometriosis also experience problems with their uterus or ovaries (such as adenomyosis, fibroids, ovarian cysts, and other conditions that can contribute to chronic pelvic pain) that could benefit from removal of the uterus and/or ovaries. For example, adenomyosis and endometriosis have been found together anywhere from 21.8% to 79% of the time (Antero et al., 2017; Di Donato et al., 2014; Kunz et al., 2005). Both endometriosis and fibroids have been found together in 12-26% of patients, although one small study found both in 86% of the patients studied (Huang et al., 2010; Nezhat et al., 2016; Uimara et al., 2011).
However, the benefits versus the risks of removal of the uterus and especially the ovaries must be weighed carefully. For some of the effects of long term low estrogen see here. Using a hysterectomy to treat endometriosis alone may still leave you susceptible to continued symptoms and other problems from remaining lesions [one example: hydronephrosis from endometriosis left around ureters (Bawin, Troisfontaines, & Nisolle, 2013)]. For more on endometriosis persisting after a hysterectomy see here.
- “The main result of our study is somewhat surprising and contrary to the common notion that hysterectomy, as a last measure, effectively relieves endometriosis-related pain. Nevertheless, the results are in line with two other national register studies on postoperative pain and patient-reported outcomes. Hysterectomy is often considered the last option to treat endometriosis, as the procedure by its very nature ends reproduction. If hysterectomy does not decrease the need for analgesics postoperatively, the effectiveness of the procedure as an integral, albeit final, stage of endometriosis pain management becomes doubtful, however.” (Brunes et al., 2021)
- “Persistent or recurrent endometriosis after a total abdominal hysterectomy and bilateral salpingo-oophorectomy (TAH BSO) has been reported by several investigators.” (Hasty & Murphy, 1995)
- “According to literature, there are no randomized controlled trials for hysterectomy as the treatment for endometriosis.” (Bellelis, 2019)
- “Endometriosis which is not removed at the time of hysterectomy and bilateral salpingo‐oophorectomy may represent after a variable time interval with many or all of the symptoms which prompted the original surgery. This tissue can be highly active and responsive to exogenous hormonal stimulation. In the presence of troublesome symptoms, excision of residual endometriosis may be effective and should be considered.” (Clayton et al., 1999)
- “A high recurrence rate of 62% is reported in advanced stages of endometriosis in which the ovaries were conserved. Ovarian conservation carries a 6 fold risk of recurrent pain and 8 folds risk of reoperation. The decision has to be weighed taking into consideration the patient’s age and the impact of early menopause on her life style. The recurrence of endometriosis symptoms and pelvic pain are directly correlated to the surgical precision and removal of peritoneal and deeply infiltrated disease. Surgical effort should always aim to eradicate the endometriotic lesions completely to keep the risk of recurrence as low as possible.” (Rizk et al., 2014)
- “Studies have showed that the growth and progression of endometriosis continue even in ovariectomized animals.” (Khan et al., 2013)
- Read more here: “Endometriosis persisting after hysterectomy and bilateral salpingo-oophorectomy: Removing the disease, not organs, is key to long-term relief”: http://endopaedia.info/treatment21.html
References
Bellelis, P. (2019). 2607 Hysterectomy in Women with Endometriosis. Journal of Minimally Invasive Gynecology, 26(7), S177. Retrieved from https://www.sciencedirect.com/science/article/pii/S1553465019307393
Brunes, M., Altman, D., Pålsson, M., Söderberg, M. W., & Ek, M. (2021). Impact of hysterectomy on analgesic, psychoactive and neuroactive drug use in women with endometriosis: nationwide cohort study. BJOG: An International Journal of Obstetrics & Gynaecology, 128(5), 846-855. Retrieved from https://obgyn.onlinelibrary.wiley.com/doi/full/10.1111/1471-0528.16469
Clayton, R. D., Hawe, J. A., Love, J. C., Wilkinson, N., & Garry, R. (1999). Recurrent pain after hysterectomy and bilateral salpingo‐oophorectomy for endometriosis: evaluation of laparoscopic excision of residual endometriosis. BJOG: An International Journal of Obstetrics & Gynaecology, 106(7), 740-744. Retrieved from https://obgyn.onlinelibrary.wiley.com/doi/full/10.1111/j.1471-0528.1999.tb08377.x?fbclid=IwAR04aFoLsukqsYutNPNXtJNZpKLNEJbgOOon334NW8D7wvwzZMWaS2YaZts
Hasty, L. A., & Murphy, A. A. (1995). Management of recurrent endometriosis after hysterectomy and bilateral salpingo-oophorectomy. In Endometriosis (pp. 189-192). Springer, New York, NY. Retrieved from https://link.springer.com/chapter/10.1007/978-1-4613-8404-5_18
Khan, K. N., Kitajima, M., Fujishita, A., Nakashima, M., & Masuzaki, H. (2013). Toll‐like receptor system and endometriosis. Journal of Obstetrics and Gynaecology Research, 39(8), 1281-1292. Retrieved from https://obgyn.onlinelibrary.wiley.com/doi/full/10.1111/jog.12117
Rizk, B., Fischer, A. S., Lotfy, H. A., Turki, R., Zahed, H. A., Malik, R., … & Herrera, D. (2014). Recurrence of endometriosis after hysterectomy. Facts, views & vision in ObGyn, 6(4), 219. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4286861/
See https://icarebetter.com/learning-library/related-conditions/

Questions to Ask Your Physical Therapist When You have Endometriosis
Author: Dr. Rebecca Patton, PT, DPT
Table of contents
- Endometriosis Care Process with iCareBetter
- 1. Are you familiar with the disease process and current treatment standards for endometriosis?
- 2. Do they consider the whole body when treating your symptoms?
- 3. Do they practice trauma-informed care specifically related to healthcare trauma?
- 4. How much time will you have for a session?
“I feel like you’re the first physical therapist who understands endo.” It’s a statement I wish I didn’t hear as often as I do. Unfortunately, there has not been a resource specifically made to evaluate pelvic physical therapists’ knowledge about endometriosis before iCareBetter.
Education for physical therapists regarding endometriosis needs more advanced continuing education courses. But it doesn’t typically happen until after completing a doctoral program. For perspective, I self-taught for several years before seeking specific classes related to endometriosis care. Therefore, it wasn’t until years after specializing in pelvic pain treatment that I realized the inefficiency of care for those with endometriosis. We can do better, but we have a long way to go.
Communicating with a pelvic physical therapist before seeking treatment can allow you to ask important questions to ensure you’re finding a provider that is a good fit for you. For achieving this goal, take advantage of time-saving strategies such as a phone consultation before committing to a therapist. Here are a few questions you may want to ask during that phone consultation or the first visit with a pelvic physical therapist for your endometriosis issues.
Endometriosis Care Process with iCareBetter
1- Find an expert based on keyword/ specialty or state
2- choose your doctor from the list
3- Get the contact info
4- First call and consultation.
5- Get info regarding costs and care process
6- Receive care
Top endometriosis physical therapists
Endometriosis Physical Therapy
1. Are you familiar with the disease process and current treatment standards for endometriosis?
It is helpful when your treating therapist is up to date on current treatment standards, as with any diagnosis. Unfortunately, there is no specific physical therapy protocol for treating patients with endometriosis. However, physical therapists should understand who will be involved in your healthcare team and have a multidisciplinary approach (1). I aim to establish what provider, either GYN or expert surgeon, will be a point of contact on that first visit.
2. Do they consider the whole body when treating your symptoms?
Endometriosis is known as a pelvic disease, but we know it is much more than that. Your physical therapist needs to tap into their education to evaluate and treat the whole body. The secondary effect of endo is often an upregulated nervous system. On the initial visit, it is typical that your physical therapist will look at movement patterns from your neck to your feet. Internal pelvic floor assessments are common but certainly do not need to happen on the first visit. Pelvic floor function is only one component in a much larger picture of your overall function. Your individual goals and comfort will dictate how much treatment involves pelvic floor treatment.
Advanced Treatments and education
Treatment involving the abdominal wall fascia, diaphragm, and viscera (organs) require additional advanced coursework compared to treating the pelvic floor. Therefore, you can ask them if they have taken additional coursework to treat the abdomen to get an idea of their experience. There is not one single treatment philosophy for the abdomen, but some courses focus on continuing education in this area. The most common that I am familiar with are The Barral Institute (2), Ramona Horton MPT, DPT (3), and Institute of Physical Art (4). Other courses involve manual nerve techniques such as Lumbar and Sacral Nerve Manual Assessment through the Herman and Wallace Pelvic Rehab Institute (5). These are just a few of the many available resources your physical therapist may use to learn more after graduate school. Some pelvic physical therapists create their treatment tanks to teach one another these skillsets.
Treatment strategies that help regulate an upregulated nervous system may be part of your care. These strategies can look like gentle hands-on treatment, questions to help you process how you relate to your body, and creating mindfulness along with movement. The connection of how our nervous system interprets information from our body is complex. A physical therapist can be a valuable resource to help you better understand the pain response and the nervous system.
3. Do they practice trauma-informed care specifically related to healthcare trauma?
Trauma-informed care in physical therapy does not substitute mental health treatment. A trauma-informed approach concerning physical therapy means understanding the entirety of the patient’s experience and the effects of that experience. Medical trauma can have a lasting response on an individual’s well-being (6). We know that those with endo, on average, have a delayed diagnosis. This delay can lead to a complicated relationship with the medical providers. Many patients with endo are seeking out pelvic PT after years of seeing various specialists. These experiences with the medical system can create barriers to a patient feeling comfortable with a new provider.
For this reason, a trauma-informed approach to treatment is essential. Awareness of how these experiences may have impacted their patient is a critical portion of providing affirming care. You can ask your physical therapist about some processes that they use to create a safe environment. These processes should include consent before any treatment or touching, checking in with your emotions and body reaction during manual therapy, and providing adequate time to provide education throughout the session.
4. How much time will you have for a session?
Asking this question can ensure you have an idea of what to expect when going into your appointment. There is no magic number of minutes that will create a perfect appointment. However, the nature of endo being more complex means I prefer more time to establish a care plan. There are multiple factors to consider during the first evaluation. These factors include sexual health, daily function, bowel and bladder health, and personal goals. Having realistic expectations for each session is helpful to decrease additional medical trauma and find a therapist that fits your needs.
Patient care and human interaction are complex, and sometimes it takes time to establish a level of comfort with your PT. Every session of PT may not equal a breakthrough in pain. Retraining the nervous system takes time, especially when the body has been protecting itself due to chronic pain.
Ultimately, endo care is ideally a multidisciplinary approach. Your physical therapist can work closely with your gynecologist and other healthcare team members to find the best individual plan for you.
If you have more questions about pelvic physical therapy, reach out for more information.
Would you mind sharing with us what pleasant or unpleasant experiences you have had with your PT?
References:
1. Agarwal SK, Foster WG, Groessl EJ. Rethinking endometriosis care: applying the chronic care model via a multidisciplinary program for the care of women with endometriosis. Int J Womens Health. 2019;11:405-410. Published 2019 Jul 23. doi:10.2147/IJWH.S207373
2. Jean-Pierre Barral, DO, MRO(F), RPT. The Barral Institute. Accessed September 1st, 2021. https://www.barralinstitute.com/
3. Ramona Horton, MPT, DPT. Herman and Wallace Pelvic Rehabilitation Institute. Accessed August 27th, 2021. https://hermanwallace.com/faculty/ramona-horton
4. Institute of Physical Art. 2015-2021. Accessed August 19th, 2021. https://instituteofphysicalart.com/
5. Nari Clemmons PT, PRPC. Herman and Wallace Pelvic Rehabilitation Institute. Accessed August 20th, 2021. https://hermanwallace.com/faculty/nari-clemons6. Michelle Flaum Hall and Scott E. Hall. When Treatment Becomes Trauma: Defining, Preventing, and Transforming Medical Trauma. American Counseling Association. March 24th, 2013. Accessed August 19th, 2021. https://www.counseling.org/knowledge-center/vistas/by-year2/vistas-2013/docs/default-source/vistas/when-treatment-becomes-trauma-defining-preventing-

Endometriosis: Impact on Work
We see time and again the impact the symptoms of endometriosis have on daily life. Regarding work and productivity, researchers found that people with endometriosis reported “17.1% of work time missed, 41.8% impaired work ability, 46.5% overall work impairment, and 41.4% activity impairment” with the greatest effect of fatigue and productivity impairment on those in their 30’s (Soliman et al., 2021). Another study reports that persons with endometriosis were “less often able to work in their desired profession than women from the control group…and they had to take health-related limitations into consideration in their career decisions to a significantly higher degree than women in the control group” (Sperschneider et al., 2019). Chronic pain from endometriosis was “was significantly associated with increased sick leave as well as with loss of productivity at work” (Sperschneider et al., 2019). How has endometriosis impacted your ability to work?
References
Sperschneider, M. L., Hengartner, M. P., Kohl-Schwartz, A., Geraedts, K., Rauchfuss, M., Woelfler, M. M., … & Leeners, B. (2019). Does endometriosis affect professional life? A matched case-control study in Switzerland, Germany and Austria. BMJ open, 9(1), e019570. Retrieved from https://bmjopen.bmj.com/content/9/1/e019570
Soliman, A. M., Rahal, Y., Robert, C., Defoy, I., Nisbet, P., Leyland, N., & Singh, S. (2021). Impact of endometriosis on fatigue and productivity impairment in a cross-sectional survey of Canadian Women. Journal of Obstetrics and Gynaecology Canada, 43(1), 10-18. Retrieved from https://doi.org/10.1016/j.jogc.2020.06.022

Endometrioma 101: Understanding Deep Ovarian Endometriosis
Table of contents
- Your Guide to Ovarian Endometrioma: Treatment, Symptoms, Doctors, Etc.
- What is Endometriomas (Deep Ovarian Endometriosis)?
- Recurrence of The Lesions Following Surgery
- Clinical Impact of Endometriomas (in Women of Reproductive Age)
- Major Concerns:
- Treatment and Surgery Options
- Final Thoughts and Question for Readers
Your Guide to Ovarian Endometrioma: Treatment, Symptoms, Doctors, Etc.
Endometrioma (deep ovarian endometriosis) can be difficult to treat due to controversies and challenges surrounding the best approaches, treatment, and diagnosis. Many of these hurdles result from misunderstandings about the condition and underlying disease process – deep ovarian endometriosis.
If you suffer from these ovarian endometriosis lesions, our sincere thoughts go out to you. Often known as “chocolate cysts,” some consider endometriomas as the most severe threat to a woman’s reproductive system (aside from cancerous tumors found in the reproductive tract). Furthermore, these lesions don’t always respond well to medical treatment and can potentially ruin the health of ovarian tissue. This article will help you understand endometrioma, symptoms, and deep ovarian endometriosis treatment.
What is Endometriomas (Deep Ovarian Endometriosis)?
Endometriomas happen when endometrial-like tissue grows inside the ovary or sometimes outside. Endometrioma is very common and affects between 17-44% of endo patients. Endometriomas are typically an advanced form of endometriosis, meaning stage three or four.
Surgery is often necessary to remove the endometriomas. However, eliminating endometrioma cysts and capsules is an advanced procedure and needs excellent skills. This surgery can potentially lead to partial or complete loss of ovarian function, especially if done by less experienced surgeons. These cystic masses can cause extreme challenges for women undergoing fertility treatments, i.e., assisted reproductive technologies (ART).
Endometriomas are dark-fluid-filled cavities, and they can present in a variety of shapes and sizes. An ultrasound can show suspected cases of endometrioma, but confirmation needs surgery and histology. Therefore, getting a diagnosis of endometrioma can be riddled with challenges.
Recurrence of The Lesions Following Surgery
On our social media accounts, we receive many questions about the topic of endometrioma recurrence. We took to Instagram to get the responses from endometriosis specialists about this recurrence. Here are some of their responses:
Dr. Jon Einarsson:
“It depends on several factors including the age of the patient, method of surgery, the experience of the surgeon, etc. In the literature, recurrence rates of over 30% have been reported, although I have personally not seen that high of recurrence risk.”
Dr. Abhishek Mangeshikar
“We’ve had ovarian recurrence rates of less than 10 percent in our two years of follow-ups of about 85 patients with ovarian endometriomas.”
“What’s important is to completely free the ovary and excise the peritoneum or uterosacral ligament it was adherent to, apart from excising the cyst. This will truly help reduce recurrence rates compared to just doing a cyst excision and leaving peritoneal disease behind.”
Dr. Ram Cabrera
“I share the same opinion, in my center, our recurrence rate is less than 8% a good technique and excision of all zone of endometrioma even peritoneal improve outcomes, also as previously said it depends on many factors like endometrioma size, multiple endometriomas, and post-op treatment.”
Dr. Gabriel Mitroi
“We have a very low recurrence rate. This is because often, during surgery, only the visible endometrioma cysts are removed. Anything under 2 cm is out of our visual field.”
Clinical Impact of Endometriomas (in Women of Reproductive Age)
Endometriomas does not cause infertility in all women it affects. However, studies show that between 25% to 50% of women with infertility have endometriosis, and 30% to 50% of women with endometriosis have infertility. However, that does not mean that endometrioma will necessarily cause infertility in women of reproductive age, especially when diagnosed and treated early with the best-practice treatments that have evolved over the years.
One of the leading fertility challenges is that ovarian lesions affect the number of eggs in ovarian tissue. Endometrioma can also impair the maturation of the egg and cause the woman to have a lower antral follicle count (AFC) and Anti-Müllerian hormone (AMH). Also, women with endometriomas often have high follicle-stimulating hormone (FSH) levels.
Major Concerns:
- Intense pelvic pain
- Possible infertility
- Decrease ovarian function
- It can place women of child-bearing age at a higher risk of cancer
Treatment and Surgery Options
Treatment for endometriomas will vary from person to person. The number of lesions and the staging of the disease progress are just a couple of the factors that will influence the right treatment plan for you.
Treatment for Females of Reproductive Ages
Many OB-GYNS and other healthcare providers still practice old treatments for endometriosis that don’t effectively manage the disorder. It’s a complicated condition. Thus, there are many myths and misconceptions about endometriosis.
Women of reproductive ages who wish to maintain fertility should have a fertility specialist in their multidisciplinary endometriosis team. Women with endometriomas may respond to some of the following treatments:
Non-surgical treatments: These treatment options are temporary choices to manage pain and complications in the short term.
- Medication therapy
- Observation
Surgical treatment: this may include:
- Drainage
- Laser ablation
- Capsule excision (the procedure of choice for most top experts)
Final Thoughts and Question for Readers
Have you had to deal with endometrioma? If so, please share how it has impacted your endo journey.

Finding an endometriosis specialist
Endometriosis often requires specialized care. Just as there are specialists such as endocrinologists, oncologists, rheumatologists, cardiovascular surgeons, orthopedic surgeons, and so on, there are specialists for endometriosis. Even within those specialties, there are subspecialties for even more specific disease processes. However, finding those elusive providers can be difficult.
When looking for an endometriosis specialist, it is important for you to understand about the disease yourself- which is why this website is in existence. Start at the beginning and work your way through the site. It is equally important to educate yourself on common diseases that occur with endometriosis and can cause similar symptoms. Treating one disease process (endometriosis) and not treating another (such as interstitial cystitis) can leave you with symptoms and questions as to why.
When looking at a surgeon for endometriosis, we have some resources to help you. Start with this article about Choosing Your Surgeon. Join our Facebook group to find other resources on endometriosis. Take a look at vetted surgeons who have chosen to refine their skills on endometriosis and have subspecialties in endometriosis surgery (bowel, thoracic, etc.) (https://icarebetter.com/).
Endometriosis can cause a lot of problems with our health and healing takes time and effort. It can take addressing multiple pain generators and mental health care. Finding the right specialist/surgeon is an important first step on that journey towards better health.

7 Ways to Prepare For First Endometriosis Specialist Appointment
Table of contents
Diagnosis. Treatment. Surgery. Many Topics May Be Discussed At Your Visit
An endometriosis specialist appointment is not something you do every day (although sometimes it might feel like all day while you’re waiting there). However, the time you get to talk with the doctor may be pretty short. During that moment of consultation with the endometriosis (endo) specialist, you might feel brain fogged or bombarded. Whether it’s the diagnosis, treatment, surgery, pain management, or an endometriosis symptom you want to bring up, it’s easy to forget an essential topic while you’re there.
To make the most out of your initial endometriosis specialist appointment with an endometriosis specialist, we’ve made a list of seven ways you can prepare for the visit. First, we will give a short description of what endometriosis is.
What’s Endometriosis?
Endometriosis is a female medical disorder in which tissue similar to the endometrium (tissue that lines the walls of the uterus) grows outside the uterus. This endometriosis tissue can grow on the surface of the uterus, ovaries, intestines, fallopian tubes, bladder, or other organs in the body.
During menstruation, this tissue releases blood, and it sloughs off. However, this blood and tissue often remain trapped with no way to escape the body. This increased pressure can result in moderate to severe pain, among other symptoms. If you want to learn more about endometriosis and get a general background on the condition, read our article, “Endometriosis 101: Covering the Basics.”
Why You Are Here
People of various ages and demographics are subject to this often debilitating inflammatory pelvic disorder. Whether you have confirmed the diagnosis of endometriosis or if you need surgery to verify its presence and remove lesions – these suggestions can help you prepare for the endometriosis specialist appointment. There are many stages of endometriosis. Whether you’ve got into a specialist early on your journey or later, the important thing is that you are here now – exploring treatment options.
7 Ways to Prepare for Endometriosis Specialist Appointment
Once you have found an experienced endometriosis specialist, it’s essential to prepare yourself for the doctor’s appointment ahead of time. There is no concrete test to diagnose endometriosis (outside of surgery). Therefore, it’s imperative to have a solid understanding of the signs and symptoms of endo and detailed accounts of your own experience ready. Simple things such as medical records or journals that list all your endometriosis symptoms are a vital arsenal that will help you and your doctor determine your treatment plan.
1. Gather Your Records.
Unfortunately, most people with endometriosis have had many doctor appointments before seeing an endometriosis specialist. Therefore, you should have some medical records for them to review during your first appointment with an endo specialist. Gather everything from your regular medical history from your general practitioner to your OB/GYN records, testing, imaging, blood work, etc. Even if you think the particular doctor appointment or medical history is insignificant, you might be surprised by the various conditions linked to endometriosis. Bring it all. This information could play a vital role in your endometriosis treatment.
2. Keep a Journal of Endometriosis Symptoms/Pain.
Write down all the possible endo signs and symptoms you’ve had leading up to the doctor’s appointment. If you get a visit scheduled, and it’s a couple of weeks out, start the journal at that time, but also include the signs and symptoms you’ve experienced leading up to that point. Then, from that date until your appointment, write down all the different types of symptoms you experience. Include everything, even if you don’t think it’s relevant, like colds, headaches, stomach issues, shortness of breath, chest pain, etc. Also, be sure to include your emotions and feelings because endometriosis can significantly impact mental health and can lead to conditions such as depression and anxiety. Emotions and mental health are essential as you might want to include a counselor as part of your holistic endometriosis treatment team.
3. Bring This Printable Guide.
At endometriosis.org, they’ve created a convenient guide that can help you describe your symptoms and know what to ask your endometriosis specialist. Click here for the PDF. Please print it out and answer all the questions. Bring this with you to your doctor’s appointment to help specifically describe your endometriosis pain and other symptoms.
4. Take All Your Medications With You.
The importance of this cannot be understated. Even if you have a medication reconciliation (also known as a “med rec” for short) from your doctor, it’s important to realize those are not always up-to-date with everything you take. This inconsistency is especially true if you are on medications from multiple specialists or take supplements as well. The best way for your endo specialist to have a complete picture of all the medicines you are currently taking is by bringing them with you to the doctor’s appointment. You should include any supplements or over-the-counter medications. Bring in the physical bottles along with any medication history records.
5. Prepare Yourself Mentally.
Go into the appointment with the bold mindset that you will ask every single question you have to gain clarity on your endometriosis diagnosis and treatment options. Endometriosis is an aggressive inflammatory disorder that can have a devastating impact on your quality of life. It would help if you carried an even more aggressive attitude toward trying to stop it dead in its tracks.
6. Bring a List of Questions.
What’s been bothering you the most? Pain? Bowel symptoms? Bring a list of all the important questions that you want answers to. Writing them down will help you not forget during the appointment. Furthermore, when the doctor sees you have a list of questions you want answers to, it makes it harder for them to get up and walk out of the room like the appointment is over. If something like that has ever happened to you, we are sorry you’ve experienced this. That’s why it’s crucial to find a vetted endometriosis expert.
7. Take a Support Person With You.
Finding a good endo expert is no easy task (unless you use iCareBetter to connect you to one). If you are the type of person who is a bit shy or feels intimidated, you should bring your best support person to the appointment with you. Even if you are not nervous about your first endometriosis specialist appointment, having someone you trust by your side can help you process the information and encourage you along your journey. If no one you would like to accompany you, consider bringing a recorder and taping the visit. Because this can help you go back later and make sure you’ve understood all the information. Most doctors will have no qualms about recording your visit.
Endometriosis Care Process with iCareBetter
1- Find an expert based on keyword/ specialty or state
2- choose your doctor from the list
3- Get the contact info
4- First call and consultation.
5- Get info regarding costs and care process
6- Receive care
We Want to Hear From You
Have you been to an endometriosis specialist (OB-GYN experienced in endo)? If so, is there anything you wished you would have done differently? If you’ve not been to an endo specialist yet, what is your biggest concern about the first doctor visit?

